Abstract
Objective
To estimate the association of age of viral suppression and central nervous system penetration effectiveness (CPE) score with neurocognitive functioning among school-age children with perinatally-acquired HIV infection (PHIV+).
Design
We analyzed data from two U.S.-based multisite prospective cohort studies.
Methods
Multivariable general linear regression models were used to evaluate associations of age at viral suppression and CPE scores [of initial ART regimen and weighted average] with WISC-III or WISC-IV neurocognitive assessments [full scale IQ (FSIQ); performance IQ/ perceptual reasoning index (PIQ/PRI); and verbal IQ/ verbal comprehension index (VIQ/VCI)], adjusted for demographic and clinical covariates. Sensitivity analyses were stratified by birth cohort (before vs after 1996).
Results
396 PHIV+ children were included. Estimated differences in mean FSIQ (comparing virally suppressed vs. unsuppressed children) by each age cutoff were 3.7, 2.2, 3.2, 4.4, and 3.9 points at ages 1, 2, 3, 4, and 5, respectively. For PIQ/PRI, estimated mean differences were 3.7, 2.4, 2.2, 4.6, and 4.5 at ages 1 through 5 respectively. In both cases, these differences were significant only at the age 4 and 5 thresholds. After stratifying by birth cohort the association between age at suppression and cognitive function persisted only among those born after 1996. Age at viral suppression was not associated with VIQ/VCI; CPE score was not associated with FSIQ, verbal comprehension or perceptual reasoning indices.
Conclusions
Virologic suppression during infancy or early childhood is associated with improved neurocognitive outcomes in school-aged PHIV+ children. In contrast, CPE scores showed no association with neurocognitive outcomes.
Keywords: Paediatrics, HIV, cognition, antiretroviral therapy, viral load, central nervous system
Introduction
Children and adolescents with perinatally-acquired HIV infection (PHIV+) are vulnerable to subtle to severe neurocognitive problems during development. Introduction of combination antiretroviral therapy (cART) has resulted in a dramatic decrease in incidence of severe neurocognitive impairments; however, HIV-infected children on suppressive cART regimens may still experience neurocognitive deficits.[1-4] HIV-associated neurocognitive disorders are thought to be due to virus-specific effects via direct infection of brain macrophages and microglia, and indirectly via virus-induced immune activation and inflammatory responses.[5-7] cART improves immunologic status and produces viral suppression in the peripheral blood; however, it remains unclear what impact cART has on the development of HIV-associated neurocognitive disorders in children as they age through adolescence and young adulthood.[8]
Recent data have shown that initiation of cART early in infancy results in significantly better neurodevelopmental scores at one year of age.[9] Initiating cART during the pre-school years (<6 years) also appears to positively affect neurodevelopment, since PHIV+ children ages 18-71 months with lower neurodevelopmental function relative to their HIV-exposed uninfected peers demonstrated developmental gains after one year of cART.[10] In contrast, children who initiated early cART (i.e, without clinical and/or immunological progression) later in childhood (median age 6.4 years) did not experience greater cognitive improvement compared to children who initiated cART when such progression had occurred, highlighting the importance of early cART initiation in infancy.[11] Despite the recent evidence for the benefit of early cART on neurodevelopment in early childhood, it remains unclear if this positive effect will persist through school-age years and adolescence.
Antiretroviral (ARV) medications penetrate the central nervous system (CNS) to differing extents. Despite viral-suppressing levels in the blood there may be low drug concentrations in the CNS, potentially allowing replication of the virus in that system. Studies in adults of the effect of the CNS penetration-effectiveness (CPE) score [12, 13] of a patient's cART regimen on neurocognitive outcomes have been conflicting [14-21] and pediatric data have been limited.[22, 23] Our study aimed to clarify this question by directly evaluating the impact of CPE score on neurocognitive outcomes.
As we move towards diagnosis and initiation of cART in infancy, it is important to determine whether early initiation of effective therapy benefits neurocognitive functioning beyond the immediate early childhood period. The main purpose of our study was to determine the effect of age at viral suppression on school-age neurocognitive outcomes. As a secondary objective, we investigated the association between CPE score and school-age neurocognitive functioning.
Methods
Study population
Study participants were from two U.S.-based multi-site prospective cohort studies, the Adolescent Master Protocol (AMP) of the Pediatric HIV/AIDS Cohort Study (PHACS) network and the Pediatric AIDS Clinical Trials Group (PACTG) 219C cohort. Both studies enrolled children, whether infected or uninfected, who were born to an HIV-infected mother. The PHACS AMP study enrolled children ages 7 to 16 years from 15 sites from March 2007 through November 2009, to evaluate the impact of HIV infection and antiretroviral therapy (ART) on pre-adolescents and adolescents with perinatal HIV infection. Eligibility criteria for PHACS AMP included complete documentation of ART history either from medical records or from participation in other cohort studies. Follow-up is ongoing. PACTG 219C enrolled individuals from 89 sites who were younger than 21 years of age from January 2000 through May 2007, to study the long-term effects of ART and HIV disease progression. Many of the children enrolled in AMP had previously participated in PACTG 219C. Only perinatally HIV-infected children were included in the present analysis. Eligible participants for this analysis were also required to complete a neurocognitive assessment at 6 years of age or older, and have at least two viral load measurements with one of the measurements either prior to or within 6 months after ART initiation. Viral load measurements performed prior to entry into either PHACS AMP or PACTG 219C were retrospectively obtained through medical chart abstraction as dictated by the original study protocol.
Institutional Review Boards (IRB) at participating sites and the Harvard School of Public Health approved both studies. Parents or legal guardians provided written informed consent for minor youth, and youth provided assent per local IRB guidelines or consent if older than 18 years.
Cognitive outcome measures
Neurocognitive functioning was measured using the Wechsler Intelligence Scale for Children, Third or Fourth Edition (WISC-III or WISC-IV).[24-26] All children in AMP were assessed using the WISC-IV; children in 219C were assessed using either the WISC-III or the WISC-IV, following the revision of the WISC-III in 2003. If a child completed multiple tests, the earliest valid test results were used in these analyses. Both the WISC-III and WISC-IV provide a Full Scale IQ (FSIQ) to represent overall cognitive ability. In addition, verbal comprehension [verbal IQ (VIQ) for WISC-III and verbal comprehension index (VCI) for WISC-IV] and perceptual reasoning [performance IQ (PIQ) for WISC-III and perceptual reasoning index (PRI) for WISC-IV] are evaluated using combinations of subtests of the WISC-III and WISC-IV, yielding composite scores for each domain. The corrected correlation coefficients of composites for the WISC-III and WISC-IV indicate that the WISC-III and WISC-IV measure similar constructs, with coefficients of 0.74 (WISC-III PIQ/WISC-IV PRI), 0.87 (WISC-III VIQ/WISC-IV VCI), and 0.89 (WISC-III FSIQ/WISC-IV FSIQ).[26] The primary outcome of the analysis was FSIQ; PIQ/PRI and VIQ/VCI were also examined as secondary outcomes. Validity of test results was reviewed by neuropsychologists and all test scores determined to be invalid were excluded from the analyses.
Exposure measures
Earliest age at viral suppression
Five age cutoffs, at 1, 2, 3, 4, and 5 years old, were used to classify viral suppression status. Viral suppression was considered achieved when two consecutive HIV-1 RNA viral load measures ≤400 copies/mL were obtained 1-6 months apart, with at least the first measurement obtained prior to the age cutoff (e.g. an infant who achieved viral suppression at 8 months of age but whose consecutive suppression was not obtained until after 1 year of age would be considered virally suppressed before age 1).
CPE score of initial ART regimen
The initial ART regimen was defined as the first regimen received before age 5 with duration > 2 weeks. The CPE score of a specific ART regimen was calculated as the sum of the individual CPE scores of each drug within the regimen. The CPE score for each ARV drug was obtained using a previously validated ranking system that assigns a score of 1 to 4 to each ARV (1 = lowest CNS penetration; 4 = highest CNS penetration).[12]
Weighted average CPE score by each age cutoff
To calculate the weighted average CPE score at each age cutoff, the CPE score of each regimen was first multiplied by the duration of the regimen, and then the sum of all CPE scores was divided by the duration of each time period of interest.
Demographic and clinical covariates
The following child and caregiver socio-demographic variables were evaluated as potential confounders of the associations between the exposure and outcome measures: child age, sex, race, ethnicity, primary language (English vs other), low birth weight (<2500 g), birth cohort (1984-1995 vs. 1996-2002), primary caregiver type (biological parent vs. other), and caregiver education level (less than high school vs higher). Clinical information, including child's pre-treatment nadir CD4% and peak viral load, CDC disease classification, diagnosis of HIV-related encephalopathy, maternal ARV exposure, and version of Wechsler assessment (WISC-III or WISC-IV), were also evaluated.
Statistical analyses
Summary statistics for background characteristics, exposures and outcome measures were provided. General linear regression models were used to evaluate associations between each exposure and outcome. Univariable analyses were first conducted to estimate the associations of each covariate of interest with each outcome. A multiple regression model was then built to evaluate the adjusted association between each exposure and outcome, including all potential confounders identified with p-value <0.1 from univariable analyses. Child's age at the time of Wechsler assessment, version of the Wechsler assessment, and birth cohort were included in multivariable models as an a priori decision. For covariates with > 5% missing data, a missing value indicator was created and included in multivariable models. Covariates with more than 20% missing data (nadir CD4%, peak viral load, maternal ARV) were excluded from multivariable analyses. Sensitivity analyses were also conducted which (a) stratified analyses by birth cohort and (b) excluded children with HIV encephalopathy diagnosis.
Analyses were based on the data collected as of October 1, 2012. SAS Version 9.2 (SAS Institute Inc., Cary, NC) was used to conduct all statistical analyses. Two-sided p-values < 0.05 were considered statistically significant.
Results
A total of 2210 HIV-infected children from PHACS AMP (n = 225) and PACTG 219C (n = 1985) completed at least one WISC-III or WISC-IV assessment. Of these, 410 children (AMP: 183; 219C: 128; co-enrolled: 99) had at least one viral load measurement either prior to or within 6 months after ART initiation. [Note that viral load measures were not routinely obtained prior to 1998 and were thus more likely unavailable for 219C children]. Fourteen (3%) children with confirmed invalid WISC test results were excluded. As a result, 396 HIV-infected children were included in the analyses. (Table 1) The mean age at time of WISC evaluation was 9.6 years (IQR: 7.3, 11.4); 54% were female, 73% Black, 27% Hispanic, and 83% spoke English as their primary language. Overall, 42% of children achieved viral suppression by 5 years of age, with 12% by age 1; 8% between age 1-2; 6% between ages 2-3; 8% between ages 3-4 and 8% between ages 4-5.
Table 1.
Baseline characteristics of PHIV+ Children (N=396) in the PHACS AMP and P219C Studies with Cognitive Functioning Assessments and Virologic Data Prior to ART Initiation
| Characteristics | N (%) |
|---|---|
| Female | 213 (54%) |
| Study | |
| AMP | 176 (44%) |
| 219C | 220 (55%) |
| Co-enrolled | 99 (25%) |
| Age at ART initiation (years): Mean (SD) | 2.8 (3.5) |
| Age at WISC evaluation (years): Mean (SD) | 9.6 (2.6) |
| Black race | 262 (73%) |
| Hispanic ethnicity | 108 (27%) |
| Primary language of child is English | 328 (83%) |
| Birth weight < 2500g | 83 (25%) |
| Baseline CDC classification: C | 87 (22%) |
| HIV encephalopathy diagnosis at entry | 24 (6%) |
| Any PMTCT ARV exposure | 83 (25%) |
| Baseline primary caregiver identity: biological parent | 201 (51%) |
| Primary caregiver education at baseline < high school | 93 (25%) |
| Nadir CD4% prior to ART initiation, mean (SD) | 23.6 (13.2) |
| Peak logRNA prior to ART initiation, mean (SD) | 5.2 (0.8) |
| Birth cohort | |
| 1984-1995 | 165 (42%) |
| 1996-2005 | 231 (58%) |
Participants with missing data were excluded from the calculations in table: race (38); Ethnicity (2); birth weight (62); PMTCT ARV exposure (62); baseline primary caregiver identity (1); caregiver education (29); nadir CD4% (140); peak logRNA (148)
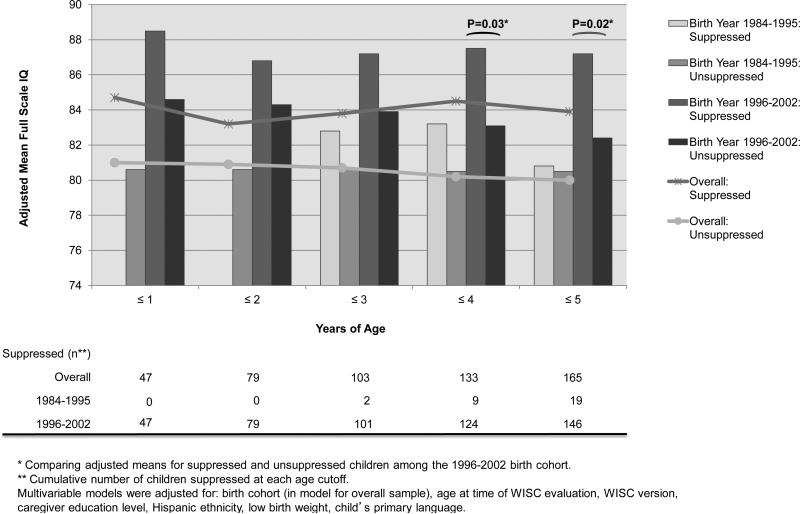
There was no difference in FSIQ or composite scores between children who took WISC-IV versus WISC-III tests: FSIQ 86.1 versus 86.7 (p = 0.69), PIQ/PRI 89.7 versus 89.6 (p = 0.94), VIQ/VCI 86.3 versus 88.5 (p = 0.17). In addition, there was no difference in FSIQ between WISC-III and WISC-IV in the 68 children who were evaluated with both versions. After adjusting for birth cohort, age at the time of WISC evaluation, WISC version, Hispanic ethnicity, primary language of the child, low birth weight and caregiver's education at study entry, the estimated difference in mean FSIQ (comparing children who were virally suppressed versus unsuppressed) by each age cutoff was 3.7 points at age 1 (p = 0.13), 2.2 at age 2 (p = 0.29), 3.2 at age 3 (p = 0.11), 4.4 at age 4 (p = 0.02), and 3.9 at age 5 (p = 0.03), with higher FSIQ in children who were virally suppressed. After stratifying by birth cohort, viral suppression and higher FSIQ remained associated only in the later birth cohort (Figure 1) and mean FSIQ was higher in the later birth cohort (data not shown). Restricting the analysis to children without a diagnosis of HIV encephalopathy at study entry did not affect the results (data not shown).
Figure 1.
Adjusted Mean Full Scale IQ Score by Viral Suppression at each Age Cutoff, Overall and by Birth Cohort. Children who achieved viral suppression at ≤4 and ≤5 years had significantly higher school-age FSIQ scores compared to children who did not achieve viral suppression by those age cutoffs. Multivariable models were adjusted for: birth cohort (in model for overall sample), age at time of WISC evaluation, WISC version, caregiver education level, Hispanic ethnicity, low birth weight, child's primary language.
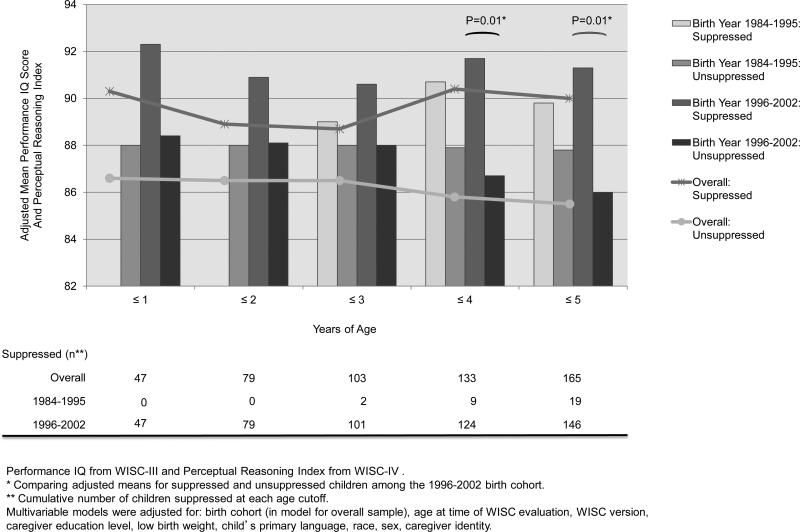
The estimated difference in adjusted mean PIQ/PRI score (comparing children who were virally suppressed versus unsuppressed) by each age cutoff was 3.7 at age 1 (p = 0.13), 2.4 at age 2 (p = 0.25), 2.2 at age 3 (p=0.27), 4.6 at age 4 (p = 0.01) and 4.5 at age 5 (p=0.01). After stratifying by birth cohort, viral suppression and higher PIQ/PRI score remained associated only in the later birth cohort. (Figure 2) No significant associations were found between age of viral suppression and VIQ/VCI.
Figure 2.
Adjusted Mean PIQ/PRI Score by Viral Suppression at each Age Cutoff, Overall and by Birth Cohort. Performance IQ from WISC-III and Perceptual Reasoning Index from WISC-IV. Children who achieved viral suppression at ≤4 and ≤5 years had significantly higher school-age PIQ/PRI scores compared to children who did not achieve viral suppression by those age cutoffs. Multivariable models were adjusted for: birth cohort (in model for overall sample), age at time of WISC evaluation, WISC version, caregiver education level, low birth weight, child's primary language, race, sex, caregiver identity.
CPE score of initial regimen and weighted average CPE score were negatively associated with higher FSIQ, PIQ/PRI and VIQ/VCI but did not reach statistical significance (Table 2). Stratifying by birth cohort and restricting the analysis to children who were virally suppressed did not change the results (data not shown).
Table 2.
Adjusted Associations Between Full Scale IQ (FSIQ), Performance IQ/Perceptual Reasoning Index Scores (PIQ/PRI), Verbal IQ/Verbal Comprehension Index Scores (VIQ/VCI) and Continuous CNS Penetration Effectiveness (CPE) Score
| Overall (n=396) |
||||||
|---|---|---|---|---|---|---|
| FSIQ1 | PIQ/PRI2 | VIQ/VCI3 | ||||
| Estimated Difference* (95% CI) | P-value | Estimated Difference* (95% CI) | P-value | Estimated Difference* (95% CI) | P-value | |
| CPE score of first ART regimen (with duration >2 weeks) before age 5 | 0.0 (−0.5, 0.6) | 0.88 | 0.1 (−0.5, 0.7) | 0.74 | 0.1 (−0.5, 0.6) | 0.79 |
| Weighted average CPE score by age 1 | −0.6 (−1.2, 0.1) | 0.10 | −0.5 (−1.2, 0.2) | 0.14 | −0.6 (−1.2, 0.1) | 0.09 |
| Weighted average CPE score by age 2 | −0.5 (−1.2, 0.1) | 0.10 | −0.6 (−1.3, 0.0) | 0.06 | −0.5 (−1.1, 0.2) | 0.14 |
| Weighted average CPE score by age 3 | −0.3 (−1.0, 0.3) | 0.31 | −0.5 (−1.1, 0.2) | 0.17 | −0.3 (−0.9, 0.4) | 0.39 |
| Weighted average CPE score by age 4 | −0.2 (−0.9, 0.5) | 0.52 | −0.3 (−1.0, 0.4) | 0.37 | −0.2 (−0.9, 0.5) | 0.52 |
| Weighted average CPE score by age 5 | −0.2 (−0.9, 0.5) | 0.58 | −0.3 (−1.0, 0.4) | 0.45 | −0.2 (−0.9, 0.5) | 0.61 |
Estimated difference in adjusted mean FSIQ, PIQ/PRI, VIQ/VCI for each one unit increase in CPE score.
Multivariable models were adjusted for: birth cohort, age at time of WISC evaluation, WISC version, caregiver education level, Hispanic ethnicity, low birth weight, child's primary language.
Multivariable models were adjusted for: birth cohort, age at time of WISC evaluation, WISC version, caregiver education level, low birth weight, primary caregiver identity, child's primary language, race, sex.
Multivariable models were adjusted for: birth cohort, age at time of WISC evaluation, WISC version, caregiver education level, Hispanic ethnicity, child's primary language.
Discussion
Our findings demonstrate that early viral suppression is associated with positive impact on cognitive functioning during childhood; children with early viral suppression demonstrated 2.2-4.4 point higher global cognitive scores and 2.2-4.6 point higher perceptual reasoning scores on Wechsler intelligence scales (WISC-III and WISC-IV). Although this association reached statistical significance only for ages 4 and 5, the effect size was consistent across all age groups and our analysis controlled for factors potentially associated with cognitive development during childhood.
In a study nested within a large randomized controlled trial of early versus deferred cART, Laughton et al found that infants randomized to cART at <3 months of age had significantly better short-term neurodevelopmental outcomes at a median age of 11 months compared to those for whom cART was deferred until immunological or clinical progression (median 31.4 weeks).[9] Our study extends this observation by showing that achievement of viral suppression at any age up to five years had positive albeit modest cognitive benefits, as measured by school- age Wechsler scores. However, the number of children who achieved viral suppression at <1 year of age in our study was small (n = 47) and we may not have had sufficient power to detect a difference at this age cutoff. These results are nonetheless encouraging in that children were evaluated at ≥6 years of age when intelligence can be more reliably measured and when the FSIQ is an adequate predictor of school achievement. Although our results did not change after excluding children with a diagnosis of HIV encephalopathy at study entry, it is possible that we missed this diagnosis particularly in the <1 year of age category. This would have biased our results towards the null in the younger age categories as a history of a prior CDC class C diagnosis, in particular HIV encephalopathy, has been shown to be independently associated with later neurocognitive impairment.[27-29]
Our findings of cognitive benefit of cART are in contrast to those of Puthanakit et al who examined cognitive outcomes of youth with early and deferred cART after 3 years of follow-up.[11] Children with moderate immunosuppression (CD4 15-24%) and no AIDS-defining illness randomized to early cART when ≥1 year of age did not differ from PHIV+ children for whom cART was deferred until immunological or clinical progression. The median age of their cohort at time of ART initiation was older than our study (6.4 years), thus very few achieved viral suppression before age 5,[30] which may have precluded detection of an effect of suppressive cART in early childhood.
It is important to note that although early viral suppression was associated with higher school-age neurocognitive scores in our study, both the suppressed and unsuppressed children scored within the low average/average range of cognitive functioning. In a study conducted by Lowick et al, ART treated HIV-infected children ages 5-6 had significantly lower general quotient (GQ) scores by Griffiths Mental Development Scales compared to healthy controls of similar socioeconomic status (mean overall GQ 70 versus 78, p = 0.001).[31] The HIV-infected children in their study were virologically suppressed at the time of enrollment; however, the median age of ART initiation was 24 months and 16.67% of their cohort was diagnosed with HIV encephalopathy. These results highlight the fact that some ART treated HIV-infected children may perform less adequately than their HIV-uninfected peers, particularly if they have a history of AIDS defining complications. This finding is in keeping with prior studies of cognitive outcomes among youth with HIV and suggests that early CNS effects and/or neuroinflammation that occurs or persists despite effective cART may have subtle or notable negative effects on cognitive development in some children.[29]
We also found that within each age category of viral suppression, mean FSIQ was higher in the later birth cohort. In addition, the association between age of viral suppression and FSIQ was limited to PHIV+ children in the later birth cohort, when use of cART was more common, suggesting that cART may be associated with improved neurocognitive outcomes independent of viral suppression. This is in contrast to prior studies that showed only limited neurodevelopmental improvement after the introduction of protease inhibitor-based cART.[32, 33]
There have been limited studies of the effect of high CNS penetrating ARV regimens on neurocognitive outcomes in HIV-infected children, and studies in adults have produced conflicting results.[14, 16, 17, 20] Patel et al demonstrated a survival benefit and a decrease in HIV-encephalopathy incidence in children associated with high CNS-penetrating regimens.[23] In contrast, Shanbag et al found no association between number of CNS-penetrating ARV agents and school-aged neurocognitive scores.[22] While it was suggested that the CPE score represents CNS penetration, the drug levels used for the calculations were derived from the cerebrospinal fluid (CSF) which may not represent levels in the brain parenchyma, the more relevant site for the antiviral effect. Furthermore, published CPE values are based on studies conducted in adults and may not accurately reflect CNS penetration in children. Although studies in adults have shown that higher CPE scoring regimens are associated with viral suppression in the CSF, this has not been confirmed in children due to the difficulties associated with obtaining CSF in children for research purposes.[34] We attempted to address this problem by restricting our analyses to only those with viral suppression in the periphery and did not see a change in our results. It is not surprising that by using a published scoring system for CNS-penetration effectiveness of ARV regimens based on adults, we found no association between CPE score of the initial ART regimen and the weighted average CPE score with FSIQ, PIQ/PRI or VIQ/VCI. Our findings suggest that CNS-directed cART in early childhood does not have a positive effect on school-age neurocognitive scores. The possibility that the observed nonsignificant negative relationships between CPE and neurocognitive outcomes reflect potential neuro-toxicities of high CPE scoring regimens on the developing brain merits further research.[35]
Our study has several limitations. The number of children achieving viral suppression prior to one year of age was low and may have precluded detection of a difference at this age cutoff. Despite this limitation, the effect size was consistent across all age groups. The two study cohorts included in our analyses were significantly different in many aspects. PACTG 219C was an earlier cohort of children who were diagnosed prior to the availability of cART. Our outcome (WISC-III or WISC-IV) was measured at ≥6 years of age and may have introduced an element of survivor bias as children in PACTG 219C surviving to ≥6 years of age would most likely have been children with less severe disease. We explored the extent of this bias by stratifying analyses by birth cohort (separate analyses for those born prior to and after the wider availability of cART from 1996) and did, in fact, detect the presence of effect modification, such that the association between age at suppression and cognitive function was present only among those born in the later cohort. Finally, it is important to note that although the association between age at viral suppression and school-age neurocognitive scores was statistically significant at ages 4 and 5, the effect sizes are unlikely to be clinically significant.
Conclusion
Virologic suppression during infancy or early childhood is associated with improved school-age neurocognitive outcomes in PHIV+ children. Despite this association, the difference in neurocognitive scores associated with viral suppression is unlikely to be clinically significant and additional interventions to positively impact neurodevelopment in PHIV+ children are needed. CNS penetration effectiveness (CPE) scores showed no association with later neurocognitive outcomes. As FSIQ is a composite score that may mask important differences among domains of function, future studies are needed to explore the relationships between virologic suppression and specific neurocognitive domains other than verbal comprehension and perceptual reasoning, including language, executive function, memory, learning and processing speed, especially in perinatally-infected youth surviving to adolescence and young adulthood.
Acknowledgements
YH and KT performed the data analysis. All authors contributed to writing the draft.
PACTG 219C
We thank the children and families for their participation in PACTG 219C, and the individuals and institutions involved in the conduct of 219C as well as the leadership and participants of the P219/219C protocol team. We are grateful for the contributions of Joyce Kraimer, Barbara Heckman, Shirley Traite, and Nathan Tryon. We also thank the sites which participated in the conduct of this study, as provided in Appendix I.
Protocol Team Members: Russell Van Dyke MD, Chair; James M Oleske MD MPH, Founding Chair; Mark Abzug MD and John Farley MD, Vice-Chairs; Mary Glen Fowler MD MPH, Michael Brady MD and Wayne Dankner MD, Past Vice-Chairs; Elizabeth Smith MD, Anne Fresia, Gregory Ciupak, Michelle Eagle PA, Dorothy R Smith MS CPNP, Paul Palumbo MD, John Sleasman MD, James Connor MD, Michael Hughes PhD, Rebecca Oyomopita MSc, George Johnson MD, Andrew Wiznia MD, Nancy Hutton MD, Andrea Kovacs MD, Mary Sawyer MD, Martin Anderson MD, Audrey Rogers PhD MPH, William Borkowsky MD, Jane Lindsey ScD, Jack Moye MD, Myron Levin MD, Marilyn Crain MD MPH, Paul Britto MS, Ruth Toumala MD, Joseph Cervia MD, Eileen Monagham, Kenneth Dominguez MD, Melody Higgins RN MS, George Seage DSc MPH, Denise Gaughan MPH, Phil Gona PhD, William Shearer MD PhD, Lois Howland DPH MS RN, Deborah Storm PhD RN, Kathleen Malee PhD, Wendy Mitchell MD, Carol Gore, Eve Powell, Michelle McConnell MD, Newana Beatty, Susan Brogly PhD, Jennifer Bryant CRA, Miriam Chernoff PhD, Barbara Heckman BS, Dawn English, Edward Handelsman MD, Patrick Jean-Philippe MD, Kathleen Kaiser, Joyce Kraimer MS, Linda Millar, Shirley Traite MSW, Paige Williams PhD, Elizabeth Woods MD MPH, Carol Worrell MD.
PHACS
We thank the children and families for their participation in PHACS, and the individuals and institutions involved in the conduct of PHACS. The following institutions, clinical site investigators and staff participated in conducting PHACS AMP in 2013, in alphabetical order: Ann & Robert H. Lurie Children's Hospital of Chicago: Ram Yogev, Margaret Ann Sanders, Kathleen Malee, Scott Hunter; Baylor College of Medicine: William Shearer, Mary Paul, Norma Cooper, Lynnette Harris; Bronx Lebanon Hospital Center: Murli Purswani, Mahboobullah Baig, Anna Cintron; Children's Diagnostic & Treatment Center: Ana Puga, Sandra Navarro, Patricia Garvie, James Blood; Children's Hospital, Boston: Sandra Burchett, Nancy Karthas, Betsy Kammerer; Jacobi Medical Center: Andrew Wiznia, Marlene Burey, Molly Nozyce; Rutgers - New Jersey Medical School: Arry Dieudonne, Linda Bettica, Susan Adubato; St. Christopher's Hospital for Children: Janet Chen, Maria Garcia Bulkley, Latreaca Ivey, Mitzie Grant; St. Jude Children's Research Hospital: Katherine Knapp, Kim Allison, Megan Wilkins; San Juan Hospital/Department of Pediatrics: Midnela Acevedo-Flores, Heida Rios, Vivian Olivera; Tulane University Health Sciences Center: Margarita Silio, Medea Jones, Patricia Sirois; University of California, San Diego: Stephen Spector, Kim Norris, Sharon Nichols; University of Colorado Denver Health Sciences Center: Elizabeth McFarland, Alisa Katai, Jennifer Dunn, Suzanne Paul; University of Miami: Gwendolyn Scott, Patricia Bryan, Elizabeth Willen.
Sources of funding
PACTG 219C
Overall support for the International Maternal Pediatric Adolescent AIDS Clinical Trials Group (IMPAACT) was provided by the National Institute of Allergy and Infectious Diseases [U01 AI068632] and the NICHD International and Domestic Pediatric and Maternal HIV Clinical Trials Network supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development [contract N01-3-3345 and HHSN267200800001C]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health. This work was supported by the Statistical and Data Analysis Center at Harvard School of Public Health, under the National Institute of Allergy and Infectious Diseases cooperative agreement #5 U01 AI41110 with the Pediatric AIDS Clinical Trials Group (PACTG) and #1 U01 AI068616 with the IMPAACT Group.
PHACS
The Pediatric HIV/AIDS Cohort Study (PHACS) was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development with co-funding from the National Institute on Drug Abuse, the National Institute of Allergy and Infectious Diseases, the Office of AIDS Research, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Institute on Deafness and Other Communication Disorders, the National Heart Lung and Blood Institute, the National Institute of Dental and Craniofacial Research, and the National Institute on Alcohol Abuse and Alcoholism, through cooperative agreements with the Harvard University School of Public Health (HD052102) and the Tulane University School of Medicine (HD052104).
APPENDIX I. Participating institutions in the U.S.-based multisite cohort study, PACTG 219/219C, between 1993-2007
The following institutions and clinical site investigators participated in PACTG 219/219C:
University of New Jersey Medical and Dental School - Department of Pediatrics, Division of Allergy, Immunology & Infectious Diseases, Boston Medical Center, Division of Pediatric Infectious Diseases, Med, Children’s Hospital LA - Department of Pediatrics, Division of Clinical Immunology & Allergy, Long Beach Memorial Medical Center, Miller Children's Hospital, Harbor - UCLA Medical Center - Department of Pediatrics, Division of Infectious Diseases, Johns Hopkins Hospital & Health System - Department of Pediatrics, Division of Infectious Diseases, University of Maryland Medical Center, Division of Pediatric Immunology & Rheumatology, Texas Children's Hospital, Allergy & Immunology Clinic, Cook County Hospital, Children's Hospital of Columbus, Ohio, University of Miami Miller School of Medicine, Division of Pediatric Immunology & Infectious Disease, University of California San Francisco School of Medicine, Department of Pediatrics, Children's Hospital & Research Center Oakland, Pediatric Clinical Research Center & Research Lab, University of California San Diego Mother, Child & Adolescent HIV Program, Duke University School of Medicine - Department of Pediatrics, Children's Health Center, University of North Carolina at Chapel Hill School of Medicine - Department of Pediatrics, Division of Immunology and Infectious Diseases, Schneider Children’s Hospital, Harlem Hospital Center, New York University School of Medicine, Division of Pediatric Infectious Diseases, Children's National Medical Center, ACT, University of Washington School of Medicine - Children's Hospital and Regional Medical Center, University of Illinois College of Medicine at Chicago, Department of Pediatrics, Yale University School of Medicine - Department of Pediatrics, Division of Infectious Disease, SUNY at Stony Brook School of Medicine, Division of Pediatric Infectious Diseases, Howard University Hospital, Department of Pediatrics & Child Health, LA County/University of Southern California Medical Center, University of Florida Health Science Center Jacksonville, Division of Pediatric Infectious Disease & Immunology, North Broward Hospital District, Children's Diagnostic & Treatment Center, University of Rochester Medical Center, Golisano Children's Hospital, Medical College of Virginia, St. Jude Children's Research Hospital, Department of Infectious Diseases, University of Puerto Rico, U. Children’s Hospital AIDS, Children's Hospital of Philadelphia, Center for Pediatric & Adolescent AIDS, St. Christopher’s Hospital for Children/Drexel University College of Medicine, Bronx-Lebanon Hospital Center, Infectious Diseases, New York Medical College/Metropolitan Hospital Center, University of Massachusetts Memorial Children's Medical School, Department of Pediatrics, Baystate Health, Baystate Medical Center, Connecticut Children's Medical Center, Medical College of Georgia School of Medicine, Department of Pediatrics, Division of Infectious Disease, University of South Alabama College of Medicine, Southeast Pediatric ACTU, LSU Health Sciences Center, Tulane University Health Sciences Center, St. Josephs Hospital and Medical Center, Cooper University Hospital - Children's Hospital Boston, Division of Infectious Diseases, David Geffen School of Medicine at UCLA - Department of Pediatrics, Division of Infectious Diseases, Children's Hospital of Orange County, Children's Memorial Hospital - Department of Pediatrics, Division of Infectious Disease, University of Chicago - Department of Pediatrics, Division of Infectious Disease, Mt. Sinai Hospital Medical Center - Chicago, Women’s & Children’s HIV Program, Columbia University Medical Center, Pediatric ACTU, Incarnation Children’s Center, Cornell University, Division of Pediatric Infectious Diseases & Immunology, University of Miami Miller School of Medicine - Jackson Memorial Hospital, Bellevue Hospital (Pediatric), San Francisco General (Pediatric), Phoenix Children's Hospital, Metropolitan Hospital Center (N.Y.), University of Cincinnati, SUNY Downstate Medical Center, Children's Hospital at Downstate, North Shore University Hospital, Jacobi Medical Center, University of South Florida - Department of Pediatrics, Division of Infectious Diseases, Cornell University, Oregon Health & Science University - Department of Pediatrics, Division of Infectious Diseases, Children's Hospital of the King's Daughters, Infectious Disease, Lincoln Medical & Mental Health Center, Mt. Sinai School of Medicine, Division of Pediatric Infectious Diseases, Emory University Hospital, San Juan City Hospital, UMDNJ - Robert Wood Johnson, Ramon Ruiz Arnau University Hospital, Medical University of South Carolina, SUNY Upstate Medical University, Department of Pediatrics, Wayne State University School of Medicine, Children's Hospital of Michigan, Children’s Hospital at Albany Medical Center, Children’s Medical Center of Dallas, Children's Hospital - University of Colorado at Denver and Health Sciences, Center, Pediatric Infectious Diseases, Columbus Children’s Hospital, University of Florida College of Medicine - Department of Pediatrics, Division of Immunology, Infectious Diseases & Allergy, University of Mississippi Medical Center, Palm Beach County Health Department, Children’s Hospital LA - Department of Pediatrics, Division of Adolescent Medicine, Vanderbilt University Medical Center, Division of Pediatric Infectious Diseases, Washington University School of Medicine at St. Louis, St. Louis Children's Hospital, Children’s Hospital & Medical Center, Seattle ACTU, Oregon Health Sciences University, St. Luke's-Roosevelt Hospital Center, Montefiore Medical Center - Albert Einstein College of Medicine, Children's Hospital, Washington, D.C., Children’s Hospital of the King's Daughters, University of Alabama at Birmingham, Department of Pediatrics, Division of Infectious Diseases, Columbus Regional HealthCare System, The Medical Center, Sacred Heart Children’s Hospital/CMS of Florida, Bronx Municipal Hospital Center/Jacobi Medical Center.
Footnotes
Conflicts of interest: All authors had none to declare.
The conclusions and opinions expressed in this article are those of the authors and do not necessarily reflect those of the National Institutes of Health or U.S. Department of Health and Human Services.
References
- 1.Tamula MA, Wolters PL, Walsek C, Zeichner S, Civitello L. Cognitive decline with immunologic and virologic stability in four children with human immunodeficiency virus disease. Pediatrics. 2003;112:679–684. doi: 10.1542/peds.112.3.679. [DOI] [PubMed] [Google Scholar]
- 2.Koekkoek S, de Sonneville LM, Wolfs TF, Licht R, Geelen SP. Neurocognitive function profile in HIV-infected school-age children. Eur J Paediatr Neurol. 2008;12:290–297. doi: 10.1016/j.ejpn.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Paramesparan Y, Garvey LJ, Ashby J, Foster CJ, Fidler S, Winston A. High rates of asymptomatic neurocognitive impairment in vertically acquired HIV-1-infected adolescents surviving to adulthood. J Acquir Immune Defic Syndr. 2010;55:134–136. doi: 10.1097/QAI.0b013e3181d90e8c. [DOI] [PubMed] [Google Scholar]
- 4.Crowell CS, Malee KM, Yogev R, Muller WJ. Neurologic disease in HIV-infected children and the impact of combination antiretroviral therapy. Rev Med Virol. 2014 doi: 10.1002/rmv.1793. [DOI] [PubMed] [Google Scholar]
- 5.Zink WE, Zheng J, Persidsky Y, Poluektova L, Gendelman HE. The neuropathogenesis of HIV-1 infection. FEMS Immunol Med Microbiol. 1999;26:233–241. doi: 10.1111/j.1574-695X.1999.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 6.Willen EJ. Neurocognitive outcomes in pediatric HIV. Ment Retard Dev Disabil Res Rev. 2006;12:223–228. doi: 10.1002/mrdd.20112. [DOI] [PubMed] [Google Scholar]
- 7.Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17:3–16. doi: 10.1007/s13365-010-0006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laughton B, Cornell M, Boivin M, Van Rie A. Neurodevelopment in perinatally HIV-infected children: a concern for adolescence. J Int AIDS Soc. 2013;16:18603. doi: 10.7448/IAS.16.1.18603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laughton B, Cornell M, Grove D, Kidd M, Springer PE, Dobbels E, et al. Early antiretroviral therapy improves neurodevelopmental outcomes in infants. AIDS. 2012;26:1685–1690. doi: 10.1097/QAD.0b013e328355d0ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Rie A, Dow A, Mupuala A, Stewart P. Neurodevelopmental trajectory of HIV-infected children accessing care in Kinshasa, Democratic Republic of Congo. J Acquir Immune Defic Syndr. 2009;52:636–642. doi: 10.1097/QAI.0b013e3181b32646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puthanakit T, Ananworanich J, Vonthanak S, Kosalaraksa P, Hansudewechakul R, van der Lugt J, et al. Cognitive function and neurodevelopmental outcomes in HIV-infected Children older than 1 year of age randomized to early versus deferred antiretroviral therapy: the PREDICT neurodevelopmental study. Pediatr Infect Dis J. 2013;32:501–508. doi: 10.1097/INF.0b013e31827fb19d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Letendre S, Marquie-Beck J, Capparelli E, Best B, Clifford D, Collier AC, et al. Validation of the CNS Penetration-Effectiveness rank for quantifying antiretroviral penetration into the central nervous system. Arch Neurol. 2008;65:65–70. doi: 10.1001/archneurol.2007.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Letendre S. Central nervous system complications in HIV disease: HIV-associated neurocognitive disorder. Top Antivir Med. 2011;19:137–142. [PMC free article] [PubMed] [Google Scholar]
- 14.Cysique LA, Vaida F, Letendre S, Gibson S, Cherner M, Woods SP, et al. Dynamics of cognitive change in impaired HIV-positive patients initiating antiretroviral therapy. Neurology. 2009;73:342–348. doi: 10.1212/WNL.0b013e3181ab2b3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cysique LA, Waters EK, Brew BJ. Central nervous system antiretroviral efficacy in HIV infection: a qualitative and quantitative review and implications for future research. BMC Neurol. 2011;11:148. doi: 10.1186/1471-2377-11-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marra CM, Zhao Y, Clifford DB, Letendre S, Evans S, Henry K, et al. Impact of combination antiretroviral therapy on cerebrospinal fluid HIV RNA and neurocognitive performance. AIDS. 2009;23:1359–1366. doi: 10.1097/QAD.0b013e32832c4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smurzynski M, Wu K, Letendre S, Robertson K, Bosch RJ, Clifford DB, et al. Effects of central nervous system antiretroviral penetration on cognitive functioning in the ALLRT cohort. AIDS. 2011;25:357–365. doi: 10.1097/QAD.0b013e32834171f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garvey L, Surendrakumar V, Winston A. Low rates of neurocognitive impairment are observed in neuro-asymptomatic HIV-infected subjects on effective antiretroviral therapy. HIV Clin Trials. 2011;12:333–338. doi: 10.1310/hct1206-333. [DOI] [PubMed] [Google Scholar]
- 19.Ellis RJ, Letendre S, Vaida F, Haubrich R, Heaton RK, Sacktor N, et al. Randomized Trial of Central Nervous System-Targeted Antiretrovirals for HIV-Associated Neurocognitive Disorder. Clin Infect Dis. 2014;58:1015–1022. doi: 10.1093/cid/cit921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caniglia EC, Cain LE, Justice A, Tate J, Logan R, Sabin C, et al. Antiretroviral penetration into the CNS and incidence of AIDS-defining neurologic conditions. Neurology. 2014;83:134–141. doi: 10.1212/WNL.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berger JR, Clifford DB. The relationship of CPE to HIV dementia: slain by an ugly fact? Neurology. 2014;83:109–110. doi: 10.1212/WNL.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 22.Shanbhag MC, Rutstein RM, Zaoutis T, Zhao H, Chao D, Radcliffe J. Neurocognitive functioning in pediatric human immunodeficiency virus infection: effects of combined therapy. Arch Pediatr Adolesc Med. 2005;159:651–656. doi: 10.1001/archpedi.159.7.651. [DOI] [PubMed] [Google Scholar]
- 23.Patel K, Ming X, Williams PL, Robertson KR, Oleske JM, Seage GR., 3rd Impact of HAART and CNS-penetrating antiretroviral regimens on HIV encephalopathy among perinatally infected children and adolescents. AIDS. 2009;23:1893–1901. doi: 10.1097/QAD.0b013e32832dc041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wechsler D. The Wechsler Intelligence Scale for Children-Third Edition. The Psychological Corporation; San Antonio, TX: 1991. [Google Scholar]
- 25.Wechsler D. The Wechsler Intelligence Scale for Children-Fourth Edition. The Psychological Corporation; San Antonio, TX: 2003. [Google Scholar]
- 26.Wechsler D. The Wechsler Intelligence Scale for Children-Fourth Edition, Technical and Interpretive Manual. The Psychological Corporation; San Antonio, TX: 2003. [Google Scholar]
- 27.Wood SM, Shah SS, Steenhoff AP, Rutstein RM. The impact of AIDS diagnoses on long-term neurocognitive and psychiatric outcomes of surviving adolescents with perinatally acquired HIV. AIDS. 2009;23:1859–1865. doi: 10.1097/QAD.0b013e32832d924f. [DOI] [PubMed] [Google Scholar]
- 28.Smith R, Malee K, Leighty R, Brouwers P, Mellins C, Hittelman J, et al. Effects of perinatal HIV infection and associated risk factors on cognitive development among young children. Pediatrics. 2006;117:851–862. doi: 10.1542/peds.2005-0804. [DOI] [PubMed] [Google Scholar]
- 29.Smith R, Chernoff M, Williams PL, Malee KM, Sirois PA, Kammerer B, et al. Impact of HIV severity on cognitive and adaptive functioning during childhood and adolescence. Pediatr Infect Dis J. 2012;31:592–598. doi: 10.1097/INF.0b013e318253844b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puthanakit T, Saphonn V, Ananworanich J, Kosalaraksa P, Hansudewechakul R, Vibol U, et al. Early versus deferred antiretroviral therapy for children older than 1 year infected with HIV (PREDICT): a multicentre, randomised, open-label trial. Lancet Infect Dis. 2012;12:933–941. doi: 10.1016/S1473-3099(12)70242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lowick S, Sawry S, Meyers T. Neurodevelopmental delay among HIV-infected preschool children receiving antiretroviral therapy and healthy preschool children in Soweto, South Africa. Psychol Health Med. 2012;17:599–610. doi: 10.1080/13548506.2011.648201. [DOI] [PubMed] [Google Scholar]
- 32.Jeremy RJ, Kim S, Nozyce M, Nachman S, McIntosh K, Pelton SI, et al. Neuropsychological functioning and viral load in stable antiretroviral therapy-experienced HIV-infected children. Pediatrics. 2005;115:380–387. doi: 10.1542/peds.2004-1108. [DOI] [PubMed] [Google Scholar]
- 33.Lindsey JC, Malee KM, Brouwers P, Hughes MD. Neurodevelopmental functioning in HIV-infected infants and young children before and after the introduction of protease inhibitor-based highly active antiretroviral therapy. Pediatrics. 2007;119:e681–693. doi: 10.1542/peds.2006-1145. [DOI] [PubMed] [Google Scholar]
- 34.Cusini A, Vernazza PL, Yerly S, Decosterd LA, Ledergerber B, Fux CA, et al. Higher CNS Penetration-Effectiveness of Long-term Combination Antiretroviral Therapy Is Associated With Better HIV-1 Viral Suppression in Cerebrospinal Fluid. J Acquir Immune Defic Syndr. 2013;62:28–35. doi: 10.1097/QAI.0b013e318274e2b0. [DOI] [PubMed] [Google Scholar]
- 35.Robertson KR, Su Z, Margolis DM, Krambrink A, Havlir DV, Evans S, et al. Neurocognitive effects of treatment interruption in stable HIV-positive patients in an observational cohort. Neurology. 2010;74:1260–1266. doi: 10.1212/WNL.0b013e3181d9ed09. [DOI] [PMC free article] [PubMed] [Google Scholar]