Abstract
Objective
The aim of this randomized controlled trial for patients with advanced cancer receiving radiation therapy was to determine the effect of a multidisciplinary intervention on spiritual quality of life (QOL) at the end of the intervention (week 4) and at two follow-up time points (weeks 26 and 52).
Methods
One hundred thirty-one persons were randomized to either the intervention or control (forms only) groups. The intervention included six 90-min in-person sessions based on the physical, emotion, social, and spiritual domains of QOL. Three sessions included the spiritual component. Caregivers were present for four sessions, one which included a spiritual component. Ten follow-up phone calls were made to the patients in the intervention group during the 6-month follow-up period. Patients completed the Functional Assessment of Cancer Therapy: General Scale, the Linear Analog Self-Assessment which includes an assessment of spiritual QOL, and the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) at enrollment, and weeks 4, 27, and 52.
Results
Following the intervention, the intervention group demonstrated improved spiritual QOL on the FACIT-Sp, whereas the spiritual QOL of the control group decreased, resulting in significant mean changes between groups (total score: 1.7 vs. −2.9; p <0.01; meaning/peace subscale: 1.0 vs. −3.5; p <0.01; faith subscale: 3.1 vs. −1.7; p = 0.04).
Conclusions
The results indicate that a multidisciplinary intervention which includes a spiritual component can maintain the spiritual QOL of patients with advanced cancer during radiation therapy.
Introduction
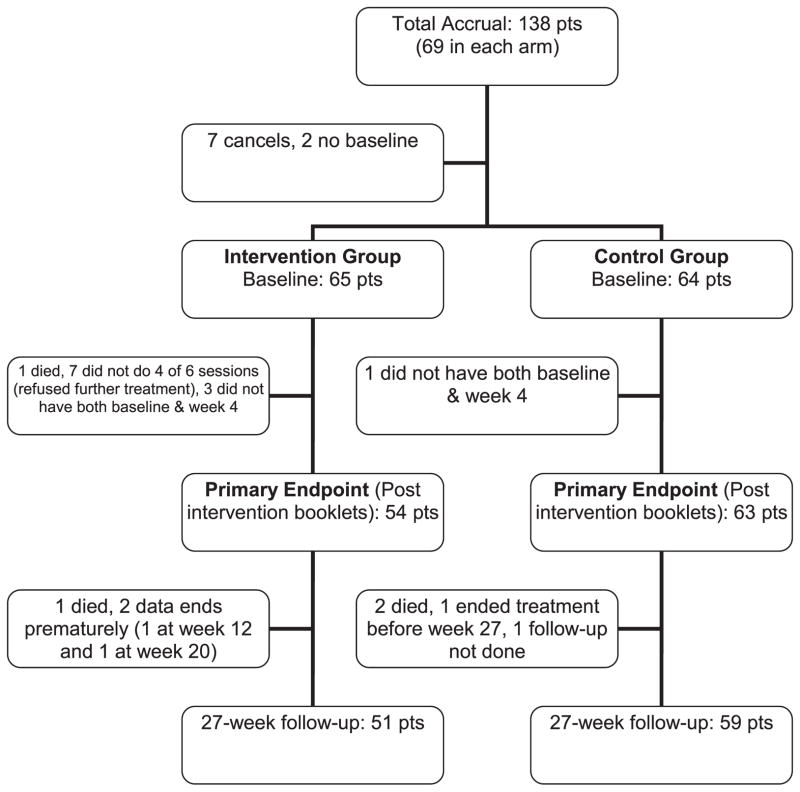
Spirituality is one of the most salient domains of quality of life (QOL) for those with life-limiting medical illnesses including advanced cancers. The poor prognosis associated with advanced cancers and the symptom burden resulting from cancer treatments often bring patients’ spiritual concerns to the forefront [1–5]. Although some patients may seek and receive spiritual care from chaplains, pastors, or other providers [6], opportunities to address and impact the spiritual QOL of patients with advanced cancer may be unrecognized and underutilized [7,8]. There is some research that examines the benefit of a structured intervention on spiritual QOL for patients with advanced stage cancer [1,9], but more is needed (Figure 1).
Figure 1.
Patient enrollment and follow-up
This study was designed following the successful outcome of a randomized, controlled, multidisciplinary QOL trial that included a spiritual component for patients with advanced cancer receiving radiation therapy (Study 1) [9]. In this previous study (Study 1), the overall QOL of the intervention group was maintained during radiation, whereas the QOL of the control group (who received questionnaires only) decreased. Additionally, the spiritual QOL was higher in those who received the intervention when compared with the spiritual QOL of the controls, directly following the intervention [9].
Based on feedback from Study 1 participants, this subsequent study (Study 2) reduced the number of intervention sessions from eight to six. Additionally, caregivers were included in four of the six intervention sessions, and ten follow-up phone calls over 6 months were added.
The primary endpoint of Study 2 was to determine whether the augmented structured multidisciplinary intervention maintained patient QOL, as measured by the Functional Assessment of Cancer Therapy: General Scale (FACT-G), at the end of intervention (week 4) and at the follow-up time points (weeks 27 and 52). The aim of this secondary analysis was to determine the effect of this augmented intervention on spiritual QOL, following the intervention and at the follow-up time points.
Methods
Design
This institutional review board-approved study was a randomized controlled trial designed to maintain or improve the QOL of patients with advanced cancer receiving radiation therapy. Patients were stratified by type of primary malignant disease (brain vs. head/neck vs. lung vs. ovarian vs. gastro--intestinal vs. other), Eastern Cooperative Oncology Group (ECOG) performance status (0 vs. 1 vs. 2), age (<50 vs. ≥50), and planned treatment (radiation therapy vs. chemotherapy vs. both).
Participants
Enrollment began following the approval of the Mayo Clinic Institutional Review Board. The primary participants were patients who had been diagnosed with advanced stage cancer within the past year and were receiving radiation therapy. Inclusion criteria required patients to have a projected life expectancy of greater than 6 months but less than 5 years (i.e., estimated 5 year survival of 0–50%). We selected this group because they have significant physical and psychosocial needs associated with the advanced stage of their cancer and their limited life expectancy, and because others have documented that the psychosocial needs of patients with cancer are often unmet [10,11].
Excluded were patients with ECOG performance status of greater than 2, which indicates severe medical decompensation. Also excluded were those determined by a psychologist or psychiatrist to be actively suicidal or too cognitively impaired to participate in the study, based on the Beck Depression Inventory-II and the mini-mental state examination scores, respectively. Secondary participants were patients’ designated caregivers, one per patient. After enrollment, patient–caregiver pairs were randomly assigned to receive the structured multidisciplinary intervention or standard medical care. To be eligible for inclusion in the analysis, patients in the intervention group must have supplied baseline data and attended at least four of the six sessions.
Intervention
The multidisciplinary intervention included six 90-min scheduled in-person sessions for the patient-participants. The topics of each session were based on the physical, emotion, social, and spiritual domains of QOL. Sessions started with 15 min of physical therapy and ended with a 15 min relaxation exercise. Each session was led by a psychologist or a psychiatrist and co-facilitated by an advanced practice nurse, a licensed social worker, or a board-certified chaplain. Non-professional caregivers, generally family members or close friends, participated with the patient-participants in four of the six sessions. A complete description of the intervention has been reported elsewhere [12].
The spiritual component of the intervention was led by board-certified chaplains and was included in three of the six sessions. Key spiritual themes relevant in facing life-threatening illness framed these sessions, i.e., life review, meaning and purpose, and grief and acceptance (presented in sessions 2, 3, and 5, respectively) [5,9,12]. Structured prompts were developed by the multidisciplinary team based on a thorough review of the literature and their clinical experiences to facilitate participants’ reflection on these themes and to encourage discussion with the other participants and the chaplain [13–16] (Table 1).
Table 1.
Sample prompts from spiritual intervention
Life review (session 2)
|
Meaning and purpose (session 3 - caregiver present)
|
Grief, loss, acceptance, and integration (session 5)
|
The caregivers were present for the session on meaning and purpose, but they were not included in the sessions that dealt with life review or grief and acceptance. Based upon participant feedback on the previous study, it had been hypothesized that the presence of the caregivers may inhibit candid communication by the patient-participants regarding these more sensitive issues.
Ten follow-up phone calls were made to the patients during the 6-month follow-up period. Eight of the phone calls were made by a psychologist, and two were made by a physical therapist. The content of the phone calls was related to the content in the intervention sessions. Structured questions were asked related to the patient’s use of the material provided in the intervention, and suggestions for compliance were given. The expectation was that both caregiver involvement and the follow-up phone calls would reinforce the material presented in the invention and increase its efficacy for the patient-participants.
Measures
Patients completed QOL assessments, including the FACT-G, the Linear Analog Self-Assessment (LASA), and the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) at enrollment, at 4 weeks (or end of face-to-face intervention) and 27 and 52 weeks after enrollment.
The FACT-G (version 4) is a well-validated 28-item general patient-rated QOL life measure for cancer patients with any tumor type. It has been used widely in clinical trials and has demonstrated sensitivity according to performance status and extent of disease. The FACT-G has four subscales: functional well-being (WB), physical WB, social/family WB, and emotional WB [17,18].
The LASA consists of 12 items and is a general measure of QOL that was constructed at Mayo Clinic for use in cancer patients [19]. Other studies have validated LASA items as measures of global and dimensional QOL constructs in numerous settings [20]. The current study focused on the spiritual QOL item which asked, ‘How is your spiritual well-being over the past week?’ using a scale from 0 (as bad as it can be) to 10 (as good as it can be).
The 12-item FACIT-Sp was used to measure overall spiritual QOL. It has been found to be a reliable and valid for measurement of spiritual QOL for people with cancer and other chronic illnesses. We also used the two author-identified subscales which differentiate between meaning and peace (items 1–8) and faith (items 9–12) [21–23].
Statistical analysis
Each assessment was scored according to its specific scoring algorithm and scores were converted to a 0- to 100-point scale for comparability, with 100 being QOL as good as it can be. Changes from baseline values were calculated. Comparison of scores between arms was conducted using chi-square or Wilcoxon tests as appropriate. Relationships between QOL scores were characterized using Pearson correlation coefficients. The study was designed to evaluate the multidisciplinary intervention as a whole, and therefore, no analysis of the specific components of the intervention was attempted.
Results
One hundred thirty-one eligible patients were randomized (65 to the intervention group and 64 to the control group). Of these, 117 (54 intervention and 63 control) were evaluable for the primary endpoint. Reasons for the patients being non-evaluable for the primary endpoint were not attending at least four of the six intervention sessions (one died and seven were absent due to illness) and not completing both baseline assessments and week 4 assessments (three intervention participants and one control participant). Fourteen patients left the study and were non-evaluable (11 from the intervention arm and three from the standard care arm). None of them completed week 4 evaluations, so we had no endpoint data available. There was no difference in the demographic variables or admission spiritual QOL between those evaluable and those non-evaluable for analysis.
The distribution of patient baseline characteristics was balanced between arms (Table 2). The mean age of patients was 59.3 years. The majority of patients were male (66%), married (87%), and employed (59%). Almost all were Caucasian (97%). Over half reported their religious affiliation as Protestant (57%) and over one third as Catholic (35%). Patients with a variety of tumor types participated (37% gastrointestinal, 22% brain, 16% head/neck, 13% lung, and 12% other). Almost all had had surgery (95%), and 86% were receiving chemotherapy, in addition to radiation.
Table 2.
Baseline patient characteristics
| Characteristics | Intervention group (n = 65) | Control group (n = 66) | p-value |
|---|---|---|---|
| Age, years: mean (SD) | 58.7 (10.6) | 59.9 (10.9) | 0.61a |
| Sex | 0.54b | ||
| Female | 24 (37%) | 21 (32%) | |
| Male | 41 (63%) | 45 (68%) | |
| Race | 0.26b | ||
| Caucasian | 63 (97%) | 64 (97%) | |
| Currently employed | 0.67b | ||
| Yes | 37 (57%) | 40 (61%) | |
| Marital status | 0.07b | ||
| Divorced | 0 | 6 (9%) | |
| Married | 59 (91%) | 56 (85%) | |
| Single | 1 (2%) | 2 (3%) | |
| Widowed | 5 (7%) | 2 (3%) | |
| Religious affiliation | 0.23b | ||
| Catholic | 18 (28%) | 28 (42%) | |
| Protestant | 39 (60%) | 35 (53%) | |
| None | 5 (8%) | 2 (3%) | |
| Other | 3 (4%) | 1 (2%) | |
| Attend religious services | 50 (76.8%) | 58 (87.9%) | 0.10b |
| Tumor type | 0.47b | ||
| Brain | 11 (17%) | 18 (27%) | |
| Gastrointestinal | 25 (39%) | 24 (36%) | |
| Head and neck | 10 (15%) | 11 (17%) | |
| Lung | 10 (15%) | 7 (11%) | |
| Other | 9 (14%) | 6 (9%) |
SD, standard deviation.
Wilcoxon signed-rank test.
Chi-square test.
Overall QOL, assessed by FACT-G, at week 4 was significantly higher in the intervention group compared with the control group (mean of 74.2 vs. 68.7; p = 0.02) [10]. The change from the baseline scores showed that the intervention group maintained their overall QOL, whereas the control group experienced a reduction in their overall QOL (mean change of −1.4 vs. −6.2; p = 0.01). There were no differences between groups at week 27 or 52.
At week 4, the intervention participants demonstrated improved spiritual QOL on the FACIT-Sp (total score and both subscales), whereas the spiritual QOL of the control participants decreased, resulting in significant mean changes between groups (mean change in total score: 1.7 vs. −2.9; p <0.01; mean change in meaning/ peace subscale: 1.0 vs. −3.5; p <0.01; mean change in faith subscale: 3.1 vs. −1.7; p = 0.04). Spiritual QOL as measured with the spiritual well-being item (SWB) on the LASA showed no statistically significant differences between groups at week 4. No differences in spiritual QOL were detected between groups at week 27 or 52 on either the FACIT-Sp or SWB LASA (Table 3).
Table 3.
Mean (standard deviation) spirituality scores from Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) and the Linear Analog Assessment spiritual well-being item (LASA spiritual WB)
| Week | Scale | Intervention | Control | p-valuea |
|---|---|---|---|---|
| 0 | FACIT-Sp meaning/peace subscale | 80.4 (15.6) | 82.8 (16.2) | 0.27 |
| FACIT-Sp faith subscale | 70.2 (28.4) | 80.2 (22.0) | 0.052 | |
| FACIT-Sp total score | 77.0 (17.0) | 81.9 (15.4) | 0.07 | |
| LASA spiritual WB | 77.2 (21.8) | 83.2 (12.8) | 0.27 | |
| 4 | FACIT-Sp meaning/peace subscale | 81.4 (16.01) | 79.3 (17.75) | 0.61 |
| FACIT-Sp meaning/peace subscale change from baseline | 1.0 (11.58) | −3.5 (10.89) | <0.01 | |
| FACIT-Sp faith subscale | 73.3 (22.26) | 78.5 (20.10) | 0.18 | |
| FACIT-Sp faith subscale change from baseline | 3.1 (16.23) | −1.7 (13.10) | 0.04 | |
| FACIT-Sp total score | 78.7 (15.31) | 79.0 (16.45) | 0.72 | |
| FACIT-Sp total score change from baseline | 1.7 (10.42) | −2.9 (8.93) | <0.01 | |
| LASA spiritual WB | 74.3 (19.48) | 78.4 (18.07) | 0.23 | |
| LASA spiritual WB change from baseline | −3.0 (16.33) | −4.8 (13.78) | 0.58 | |
| 27 | FACIT-Sp meaning/peace subscale | 78.1 (15.24) | 80.8 (16.46) | 0.24 |
| FACIT-Sp meaning/peace subscale change from baseline | −2.4 (14.87) | −2.8 (13.49) | 0.59 | |
| FACIT-Sp faith subscale | 70.5 (25.68) | 76.4 (23.60) | 0.27 | |
| FACIT-Sp faith subscale change from baseline | 0.4 (21.86) | −3.1 (17.86) | 0.52 | |
| FACIT-Sp total score | 75.5 (16.12) | 79.3 (16.27) | 0.20 | |
| FACIT-Sp total score change from baseline | −1.5 (15.05) | −2.9 (12.36) | 0.45 | |
| LASA spiritual WB | 78.5 (16.11) | 80.4 (18.18) | 0.37 | |
| LASA spiritual WB change from baseline | 0.4 (18.10) | −2.6 (18.10) | 0.58 | |
| 52 | FACIT-Sp meaning/peace subscale | 80.0 (15.92) | 78.7 (14.85) | 0.71 |
| FACIT-Sp meaning/peace subscale change from baseline | −1.0 (14.57) | −4.7 (15.66) | 0.12 | |
| FACIT-Sp faith subscale | 73.0 (23.40) | 78.4 (22.58) | 0.20 | |
| FACIT-Sp faith subscale change from baseline | 5.2 (19.76) | −1.7 (15.32) | 0.11 | |
| FACIT-Sp total score | 77.7 (15.9) | 78.6 (13.8) | 0.87 | |
| FACIT-Sp total change from baseline | 1.1 (14.30) | −3.7 (12.74) | 0.07 | |
| LASA spiritual WB | 75.6 (18.03) | 83.4 (14.13) | 0.05 | |
| LASA spiritual WB change from baseline | −1.8 (19.85) | 1.1 (15.28) | 0.40 |
Wilcoxon signed-rank test.
To characterize associations between spiritual QOL as measured by the FACIT-Sp and the SWB LASA, correlation statistics were calculated. The correlations of the FACIT-Sp total score and the SWB LASA score were moderate in value at each time point (baseline, r = 0.64; week 4, r = 0.49; week 27, r = 0.67; week 52, r = 0.58). Correlations between the subscales of the FACIT-Sp and the SWB LASA were also consistently moderate over time (FACIT-Sp faith subscale and the SWB LASA: baseline, r = 0.56; week 4, r = 0.44; week 27, r = 0.63; week 52, r = 0.47).; FACIT-Sp Meaning/Peace subscale and the SWB LASA: baseline, r = 0.53; week 4, r = 0.41; week 27, r = 0.53; week 52, r = 0.49).
Discussion
This randomized controlled trial demonstrated that a multidisciplinary intervention with a spiritual component maintained overall QOL and spiritual QOL in advanced cancer patients receiving radiation. This finding supports the growing literature that structured interventions can impact the spiritual QOL of patients with advanced cancer and provides further suggestions for a structured process of spiritual care designed to benefit patients with advanced cancer dealing with the additional challenges of radiation therapy. Because spiritual distress has been associated with declines in physical and mental health in various populations, an intervention that has a positive impact on spiritual QOL is very advantageous [24–26] and warrants further exploration.
From a clinical and patient care perspective, the board-certified chaplains involved in this study were impressed with the depth and richness of the discussions that occurred during the intervention sessions. The themes and the prompts used in the spiritual intervention could easily be incorporated into spiritual conversation with individual cancer patients and their caregivers by chaplains. The resulting discussions may lead to important life review and integration that inevitably leads to patient and caregiver well-being [13].
In the development of subsequent QOL interventions for patients with advanced cancer, it will be important to identify strategies to promote and enhance long term-spiritual QOL. Given their poor prognosis, spiritual issues may continue to be important to them, and they may benefit from conversation with a chaplain following an in-person intervention [27]. Perhaps, follow-up phone calls from a chaplain to reinforce the spiritual aspects of the intervention and provide spiritual dialogue about spiritual concerns or questions would be beneficial. Another strategy would be to incorporate the patients’ local spiritual providers and resources into follow-up care to foster long-term spiritual QOL.
The limitations of our study include the fact that most of our study population contains very minimal religious diversity. Most are Protestant or Catholic, and most attend religious services. Additionally, almost all participants were Caucasian. Thus, the generalizability of our findings is limited. Future studies should attempt to enroll a more religiously and ethnically diverse group of participants.
Another limitation of this project is the restrictedness of the spiritual data collected. In addition to very brief demographic information, spirituality was assessed only through two instruments both focused on SWB. Despite moderate correlations between them, only one of these, the FACIT-Sp, demonstrated a difference between groups. Questionnaires assessing other aspects of spirituality may have shed light on the reason for this finding. Additionally, future research could involve a qualitative analysis of transcripts of the spirituality sessions and qualitative interviews assessing key components of the spiritual intervention to obtain more personalized information regarding changes in spirituality. The results would make an important contribution to the understanding of spiritual QOL and spiritual struggle in patients with advanced cancer. The results would make an important contribution to the understanding of spiritual QOL and spiritual struggle in patients with advanced cancer. Current spiritual constructs are considered ‘fuzzy’ [28–30], and a qualitative investigation into the material discussed may lead to more precise definitions, and consequently, add to the efficacy of interventions and measurement.
Conclusion
The results of this study support previous findings indicating that a multidisciplinary intervention which includes a chaplain-led spiritual component has a significant impact on overall QOL and spiritual QOL in patients with advanced cancer during the challenging experience of active radiation therapy. These results offer important information for researchers and clinicians seeking to develop best practice clinical interventions for patients with advanced cancer. They also suggest the importance of investigating further the meaning of spiritual QOL for these patients and the trajectory of their spiritual QOL over time.
Acknowledgments
This study was supported by the Linse Bock Foundation and the Saint Mary’s Hospital Sponsorship Board Inc., Rochester, MN.
References
- 1.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-Oncology. 2010;19:21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delgado-Guay MO, Hui D, Parsons HA, et al. Spirituality, religiosity, and spiritual pain in advanced cancer patients. J Pain Symptom Manage. 2011;41:986–994. doi: 10.1016/j.jpainsymman.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Puchalski C, Ferrell BR. Making Health Care Whole: Integrating Spirituality into Patient Care. Templeton Press; West Conshohocken, PA: 2010. [Google Scholar]
- 4.Puchalski CM. A Time for Listening and Caring: Spirituality and the Care of the Chronically Ill and Dying. Oxford University Press; New York, NY: 2006. [Google Scholar]
- 5.Winkelman WD, Lauderdale K, Balboni MJ, et al. The relationship of spiritual concerns to the quality of life of advanced cancer patients: preliminary findings. J Palliat Med. 2011;14:1022–1028. doi: 10.1089/jpm.2010.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piderman KM, Marek DV, Jenkins S, et al. Predicting Patients’ Expectations of Hospital Chaplains: A Multisite Survey. Mayo Clin Proc. 2010;85:1002–1010. doi: 10.4065/mcp.2010.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balboni MJ, Sullivan A, Amobi A, et al. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. J Clin Oncol. 2013;31:461–467. doi: 10.1200/JCO.2012.44.6443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vallurupalli M, Lauderdale K, Balboni MJ, et al. The role of spirituality and religious coping in the quality of life of patients with advanced cancer receiving palliative radiation therapy. J Supportive Oncol. 2012;10:81–87. doi: 10.1016/j.suponc.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rummans T, Clark M, Sloan J, et al. Impacting quality of life for patients with advanced cancer with a structure multidisciplinary intervention: a randomized controlled trial. J Clin Oncol. 2006;24:635–642. doi: 10.1200/JCO.2006.06.209. [DOI] [PubMed] [Google Scholar]
- 10.Cwikel JG, Behar LC. Organizing social work services with adult cancer patients: integrating empirical research. Soc Work Health Care. 1999;28:55–76. doi: 10.1300/J010v28n03_04. [DOI] [PubMed] [Google Scholar]
- 11.Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012;30:1178–1186. doi: 10.1200/JCO.2011.39.7398. [DOI] [PubMed] [Google Scholar]
- 12.Clark MM, Rumans TA, Atherton PJ, et al. Randomized controlled trial of maintaining quality of life during radiation therapy for advanced cancer. Cancer. 2013;119:880–887. doi: 10.1002/cncr.27776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011;12:753–762. doi: 10.1016/S1470-2045(11)70153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson ME, Piderman KM, Sloan JA, et al. Measuring spiritual quality of life in patients with cancer. J Support Oncol. 2007;5:437–442. [PubMed] [Google Scholar]
- 15.Piderman KM, Johnson ME. Hospital chaplains’ involvement in a randomized controlled multidisciplinary trial: implications for spiritual care and research. J Pastoral Care and Counseling. 2009;63:1–6. [PubMed] [Google Scholar]
- 16.Wilson KG, Chochinov HM, McPherson CJ, et al. Suffering with advanced cancer. J Clin Oncol. 2007;25:1691–1697. doi: 10.1200/JCO.2006.08.6801. [DOI] [PubMed] [Google Scholar]
- 17.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 18.Janda M, Gebski V, Brand A, et al. Quality of life after total laparoscopic hysterectomy versus total abdominal hysterectomy for stage I endometrial cancer (LACE): a randomised trial. Lancet Oncol. 2010;11:772–780. doi: 10.1016/S1470-2045(10)70145-5. [DOI] [PubMed] [Google Scholar]
- 19.Bretscher M, Rummans TA, Sloan J, et al. Quality of life in hospice patients: a pilot study. Psychosomatics. 1999;40:309–313. doi: 10.1016/S0033-3182(99)71224-7. [DOI] [PubMed] [Google Scholar]
- 20.Locke DEC, Decker PA, Sloan JA, et al. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. J Pain Symptom Manage. 2007;34:628–638. doi: 10.1016/j.jpainsymman.2007.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brady MJ, Peterman AH, Fitchett G, Cella D. The expanded version of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp-Ex): Initial report of psychometric properties. Ann Behav Med. 1999;21:129. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 22.Cella D, Nowinski CJ. Measuring quality of life in chronic illness: the functional assessment of chronic illness therapy measurement system. Archives Phys Med Rehabilitation. 2002;83(12 Suppl 2):S10–17. doi: 10.1053/apmr.2002.36959. [DOI] [PubMed] [Google Scholar]
- 23.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 24.Hui D, de la Cruz M, Thorney S, Parsons HA, Delgado-Guay M, Bruera E. The frequency and correlates of spiritual distress among patients with advanced cancer admitted to an acute palliative care unit. Am J Hospice & Palliative Med. 2011;28:264–270. doi: 10.1177/1049909110385917. [DOI] [PubMed] [Google Scholar]
- 25.Pargament KI, Ano GG. Spiritual resources and struggles in coping with medical illness. South Med J. 2006;99:1161–1162. doi: 10.1097/01.smj.0000242847.40214.b6. [DOI] [PubMed] [Google Scholar]
- 26.Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: a two-year longitudinal study. J Health Psychol. 2004;9:713–730. doi: 10.1177/1359105304045366. [DOI] [PubMed] [Google Scholar]
- 27.Phelps AC, Lauderdale KE, Alcorn S, et al. Addressing spirituality within the care of patients at the end of life: perspectives of patients with advanced cancer, oncologists, and oncology nurses. J Clin Oncol. 2012;30:2538–2544. doi: 10.1200/JCO.2011.40.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Jager Meezenbroek E, Garssen B, van den Berg M, van Dierendonck D, Visser A, Schaufeli WB. Measuring spirituality as a universal human experience: a review of spirituality questionnaires. J Relig Health. 2012;51:336–354. doi: 10.1007/s10943-010-9376-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hill P, Pargament K. Advances in the conceptualization and measurement of religion and spirituality: implications for physical and mental health research. Am Psychol. 2003;58:64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- 30.Zinnbauer B, Pargament K, Cole B, et al. Religion and spirituality: unfuzzying the fuzzy. J Sci Study Religion. 1997;36:549–564. [Google Scholar]