Abstract
Background
Tai Chi may be efficient for healthy adults to improve the cardiorespiratory fitness, but there is no systematic evaluation for its effectiveness.
Objective
To systematically assess the effectiveness of Tai Chi on cardiorespiratory fitness in healthy adults.
Methods
Seven electronic databases were searched from their inception to October 2013. The controlled trails including randomized controlled trial (RCT), non-randomized controlled trial (NRCT), self-controlled trial (SCT), and cohort study (CS) testing Tai Chi exercise against non-intervention control conditions in healthy adults that assessed any type cardiorespiratory fitness outcome measures were considered. Two reviewers independently performed the selection of the studies according to predefined criteria. The risk of bias was assessed using Cochrane criteria. RevMan 5.2 software was applied for data analysis.
Results
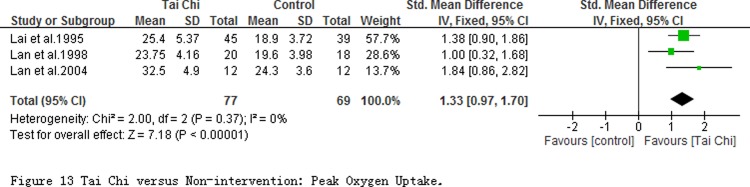
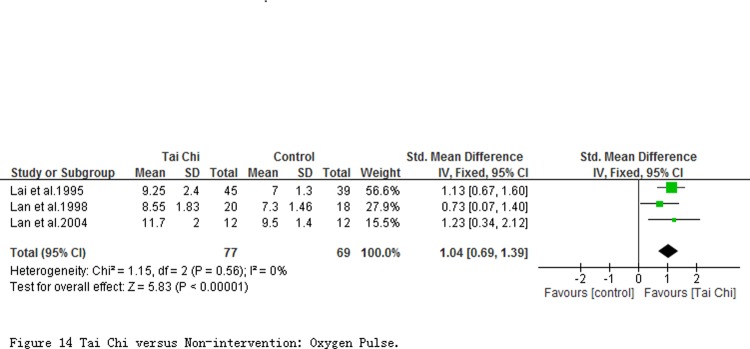
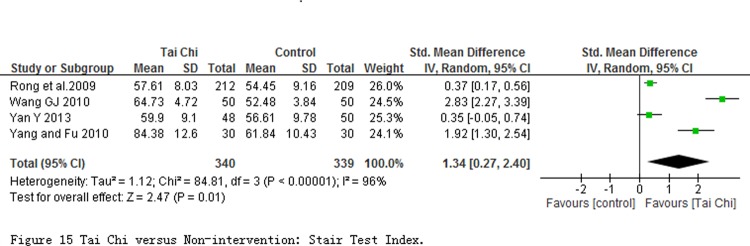
Twenty studies (2 RCTs, 8 NRCTs, 3 SCTs, and 7 CSs) with 1868 participants were included, but most of them belonged to low methodological quality. The results of systematic review showed that Tai Chi exercise had positive effect on majority outcomes of cardio function (Blood pressure: n = 536, SPB SMD = -0.93, 95% CI -1.30 to -0.56, P < 0.00001; DBP SMD = -0.54, 95% CI -0.90 to -0.18, P < 0.00001; heart rate at quiet condition: n = 986, SMD = -0.72, 95% CI -1.27 to -0.18, P = 0.010; stroke volume: n = 583, SMD = 0.44, 95% CI 0.28 to 0.61, P < 0.00001; cardio output: n = 583, MD = 0.32 L/min, 95% CI 0.08 to 0.56, P = 0.009), lung capacity (FVC at quiet condition: n = 1272, MD = 359.16 mL, 95% CI 19.57 to 698.75, P = 0.04 for less than one year intervention, and MD = 442.46 mL, 95% CI 271.24 to 613.68, P<0.0001 for more than one year intervention; V·O2peak: n = 246, SMD = 1.33, 95% CI 0.97 to 1.70, P < 0.00001), and cardiorespiratory endurance (O2 pulse at quiet condition: n = 146, SMD = 1.04; 95% CI 0.69 to 1.39; P < 0.00001; stair test index at quiet condition: n = 679, SMD = 1.34, 95% CI 0.27 to 2.40, p = 0.01). No adverse events were reported.
Conclusions
The results are encouraging and suggest that Tai Chi may be effective in improving cardiorespiratory fitness in healthy adults. However, concerning the low methodological quality in the included studies, more larger-scale well-designed trails are needed till the specific and accurate conclusions can be perorated.
Introduction
Cardiorespiratory fitness (CRF) is a measure of the capacity of the cardiovascular system to transport oxygen and the ability of the muscles to use it. Furthermore CRF indicates the ability of the circulatory, respiratory, and muscular systems to supply oxygen to skeletal muscles during sustained physical activity [1]. It therefore is strongly associated with various health outcomes. Substantial data have demonstrated that CRF is associated with morbidity and mortality in general population independently of other risk factors [2–4]. Compared with the individuals with the low level CRF, those with high level CRF had 53% lower risk for all-cause mortality for women and 43% for men [5]. Moreover, the efficient CRF has benefit to reduce the risk of heart disease, lung cancer, type 2 diabetes, stroke, and other chronic diseases [6–7]. However, with increasing of age in the general population, cardiorespiratory system generates certain changes in shape and functionality, which shows the angiosclerosis of arterial vascular walls, the decline of blood vessel compliance, enlargement of peripheral resistance, increase of blood pressure, decline of respiratory muscle function and low-efficiency work of breathing [8]. Thus low CRF is an important risk factor for the development of cardiovascular disease. CRF also is an independent predictor of mortality, and provides significantly more accurate prognostic information [9].
Although CRF has a genetic contribution, physical activity habits are its primary determinant in adults, and changes in physical activity levels result in changes in CRF [10–12]. Furthermore intensity and duration of physical activity may emerge as the best independent predictor of CRF [13–14]. A number of published studies have demonstrated that regular physical activity can significantly increase aerobic capacity as well as lung capacity and decreased heart rate [15–17]. Previous studies also testified that physical activity and exercise training resulted in significant cardiorespiratory fitness improvements not only in healthy populations [18] but also in patients of traumatic brain injury [19].
Tai Chi (TC), also known as Tai Chi Chuan, developed originally as a martial art from the 17th century, and has been practiced for centuries in China as a no-contact, low-impact, soft body and mindfulness exercise for health promotion in general population [20–21]. The basic action of TC is “a series of individual movements linked together a continuous manner that flow smoothly from one movement to another” [22]. The practitioners were required to keep deep diaphragmatic and rhythmic breathing, and integrate into body motions to harmonize the body balance and mental concentration when TC is practiced [23]. It’s also principled upon breathing and neuromuscular active relaxation with slow and gentle movement meanwhile maintaining stable postures [24]. Studies have been performed to examine the effect of TC exercise on the physical condition of a wide age range [25–26] particularly in the elder people [27–28]. Beneficial improvement has been reported on blood pressure, immune capacity, mental control, flexibility, and balance control [29–30]. Currently, the increasing data from clinical trials and exercise intervention studies found that TC exercise associated with the improvement of CRF in both healthy people and patients with chronic diseases. For example, some studies indicated that TC training with low to moderate intensity is of great positive importance on outcomes of CRF including the oxygen uptake (Vo2), O2 pulse [31], ventilatory efficiency [32], lung function [33–35], blood pressure [36], aerobic endurance [37] and exercise capacity [38]. The results from a meta-analysis and its update suggested that Tai Chi might be effective in improving the aerobic capacity of CRF outcomes among sedentary adults with over 55 years old [39–40], whereas another previous systematic review found no significant differences [41]. Furthermore those previous review or meta-analysis did not involve in other outcomes of CRF. Therefore the convincing evidence of Tai Chi on improving CRF in the general healthy population or patients with chronic diseases was yet unclear. To our knowledge, no systematic reviews have evaluated the effect of Tai Chi exercise on the outcomes of CRF in healthy adults. We therefore designed this systematic review to investigate the effectiveness and safety of Tai Chi exercise on the outcomes of CRF in healthy adults.
Methods
Eligibility Criteria
Available human clinical or community studies with a randomized controlled, non-randomized controlled, self-control trials and cohort design published in English or Chinese were included in this review. The participants were defined to healthy adults. The included studies should focus on the effect of TC exercise for CRF comparing with non-intervention, which those comparing TC with other exercise intervention were excluded. Outcomes measures for CRF assessment should cover at least one of essential outcomes such as heart rate, stroke volume, cardiac output, myocardial oxygen consumption, left heart energy effective utilization, left ventricular effective pump power, gas exchange rate, forced vital capacity, forced vital capacity in the first second, maximal minute ventilation, peak oxygen uptake, myocardial oxygen consumption, oxygen pulse, expansion coefficient of elasticity of blood vessels.
Data Sources and Searches
The original research articles were searched from 7 electronic English and Chinese databases which covered PubMed, Science Citation Index (SCI), EMBASE, Cochrane library, Chinese Scientific Journal Database (VIP), China National Knowledge Information database (CNKI) and Wan Fang from their inception to October 2013. We used the following search strategy ((Taiji OR Tai Chi OR Chi, Tai OR Tai Ji Quan OR Ji Quan, Tai OR Quan, Tai Ji OR Tai-ji OR Taijiquan OR T’ai Chi OR Tai Chi Chuan) AND (cardiorespiratory function OR maximal oxygen OR FVC OR Forced Vital Capacity OR gas exchange rate OR stroke volume OR VE OR minute ventilation OR minute respiratory volume OR EWK OR myocardial oxygen consumption OR HOV OR MOCI OR HOI OR maximal oxygen consumption OR FEK OR expansion coefficient of elasticity of blood vessels OR heart rate OR blood pressure OR oxygen pulse) AND (control OR comparison OR controlled trial)) in the English databases and (Taiji AND cardiorespiratory function AND comparison) in the Chinese databases. The detail of search strategies can be found in S1 File. The reference lists of identified articles were also searched.
Study Identification and Quality Assessment
Two reviewers (LSZ and HMM) independently screened the title and abstract of the searched studies. Full text of the studies that potentially met the eligibility criteria were obtained, and the potentially relevant references were retrieved according to predefined eligibility criteria. Data was extracted by one reviewer (LSZ) using the prepared forms and checked for accuracy by the second (HMM). The extracted details from eligible literatures included the language of publication, age of participants, methodological information, demographics of participants, sample size, experimental and control interventions, duration, frequency and style of TC exercise, outcomes, and adverse effects. Disagreements were resolved through discussion, and the original author was contacted with if the results could not come to an agreement.
Quality of studies was assessed independently by two reviewers (LSZ and LFW) using the Cochrane Collaboration’s tool for assessing the risk of bias [42]. The following recommended domains were considered: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting) and other bias, each of which was rated according to the level of bias and categorized into either low, high, or unclear.
Data Analysis
Statistical heterogeneity among studies was assessed using a Chi-square test, or by calculating Higgins I 2 values [43]. The results were pooled using a fixed effect model when the I 2 value was less than 40%. Otherwise, a random effect model was applied. However if the I 2 value among studies was more than 75%, the heterogeneity was considered substantive and the overall meta-analysis was not appropriate to conducted but subgroup analysis was considered to measure the pooled effect. Sensitivity analysis was used to explore the source of heterogeneity. The mean difference (MD) or standard mean difference (SMD) with corresponding 95% confidence interval (CI) was calculated for the continuous outcomes. Review Manager 5.2 software of The Cochrane Collaboration was applied for data analysis and all P values were two sided [44].
Results
Description of Studies
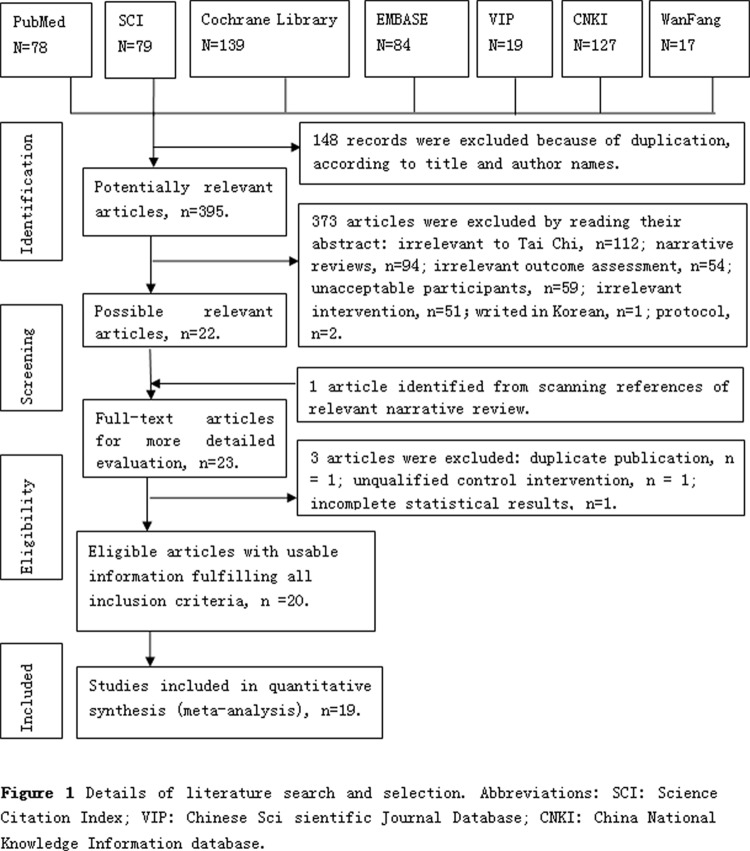
The detail screening flow about the generating of eligible articles was presented in the Fig. 1. A total of 532 records were identified through database searches. After removing duplicates, 395 remained to be screened for eligibility, and 23 were selected for a full-text evaluation. Of these, 3 studies were excluded, and reasons included: duplicate publication (n = 1) [45]; unqualified control intervention (n = 1) [46], and incomplete statistical results (n = 1) [47] (S2 File). Consequently, 20 literatures met with the inclusion criteria and 19 studies were included into meta-analysis.
Fig 1. Details of literature search and selection.
Abbreviations: SCI: Science Citation Index; VIP: Chinese Sci sientific Journal Database; CNKI: China National Knowledge Information database.
Table 1 illustrated the characteristics of the sample, intervention and outcomes. This review involved a total of 1783 healthy community-dwellers (age from 45 to 75 years old). And the design type of those included studies covered 2 randomized controlled trials (RCTs) [48–49], 8 non- randomized controlled trials (NRCTs) [50–57], 7 Cohort studies (CSs) [58–64] and 3 Self-controlled trials (SCTs) [65–67]. Few studies [49, 54, 56, 57, 63, 64] definitely described the type of Tai Chi used in their studies. Apart from the 3 Self-controlled trials, the remaining 17 trials compared TC with non-intervention. Moreover, all the measurement of outcomes utilized acknowledged apparatus and method. Additionally, TC has not been reported to be associated with adverse events during the intervention.
Table 1. Characteristics of the included studies.
| Author, year | Study design | Place of study | No.of participants (T/C) | Age (year) | Intervention | Frequency and Duration of Tai Chi exercise | Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|
| Tai Chi | Control | Tai Chi | Control | ||||||
| Nguyen et al. 2012 (48) | RCT | Vinh, Vietnam | 96(48/48) | 69.23±5.3 | 68.73 ±4.95 | Tai Chi | Non-intervention | 60 minutes per time and twice per week for 6 months | HR,SBP,DBP |
| Lu et al.2012(49) | RCT | Taiwan, China | 50(25/25) | 50–67 | 47–59 | Yang’s Tai Chi Chung | Non-intervention | 40 minutes per time and 7 times per week for 3 months | FVC,FEV1,SBP,DBP |
| Tu HL 2005 (50) | NRCT | Hubei, China | 32(16/16) | 61.64±4.21 | 63.25±6.05 | Taijiquan | Non-intervention | 12 minutes per time and 3 times per week for 10 weeks | SV,CO,VPE,EWK,HOV,SBP,DBP |
| Xu and Wen 1997 (51) | NRCT | Sichuan, China | 34(18/16) | 66.7±7.4 | 64.6±3.9 | Taijiquan | Non-intervention | for 10.5±8.7 years. | HR.SBP,DBP,MMV,FVC |
| Liu and Jin 2010(52) | NRCT | Jiangsu, China | 20(10/10) | 61.2±3.0 | 62.5±2.4 | Taijiquan | Non-intervention | 60 minutes per time and 4 times per week for 8 weeks. | HR.SBP,DBP,MMV,FVC,FEV1 |
| Yang and Fu 2010 (53) | NRCT | Gansu, China | 60(30/30) | 50–70 | 50–70 | Taijiquan | Non-intervention | 35 minutes per time and more than 4 times per week for 1 year. | SBP,DBP,HR,FVC, Step test index |
| Lan et al. 1998 (54) | NRCT | Taiwan, China | 39(21/18) | 60.05±4.48 | 66±3.85 | Yang’s Tai Chi Chung | Non-intervention | 1 hour and 4.6 ± 1.3 times per week for 11.2 ± 1.4 months. | HR,VO2peak;O2 pulse, MMV |
| Chang et al.2013 (55) | NRCT | Taiwan, China | 133(64/69) | 56.45±8.51 | 62.26±12.91 | Tai Chi Chung | Non-intervention | 60 minutes per time and three times per week at a park for 12 weeks. | SBP,DBP |
| Thornton et al. 2004(56) | NRCT | UK | 40(20/20) | 47.2±4.07 | 48.4±4.33 | Yang’s Tai Chi | Non-intervention | three times per week for 12 weeks. | SBP,DBP |
| Lu et al.2003 (57) | NRCT | Taiwan, China | 40(20/20) | 52.8±7.5 | 56.3±8.5 | Yang’s Tai Chi Chuan | Non-intervention | 40 minutes per time and 3 times per week for an average of 1.9±1.0 years。 | SBP,DBP |
| Rong et al. 2009 (58) | CS | Beijing, China | 421(212/209) | Over 45 | Over 45 | Taijiquan | Non-intervention | More than 30 minutes per time and more than 4 times per week for more than 5 years. | FVC, Step test index |
| Yan Y 2013 (59) | CS | Liaoning, China | 98(48/50) | over 45 | over 45 | Taijiquan | Non-intervention | More than 30 minutes per time and more than 3 times per week for 1year. | FVC, Step test index |
| Li XH 2008(60) | CS | Liaoning, China | 60(30/30) | 65.3±4.8 | 66.1±4.6 | Taijiquan | Non-intervention | From 40 to 60 minutes per time and more than 4 times per week for 1 years. | FVC,HR,SV,CO |
| Peng CZ 2006 (61) | CS | Zhejiang, China | 380(180/200) | 61.94±3.64 | 62.07±3.16 | Taijiquan | Non-intervention | More than 30 minutes per time and 3 times per week for 5 years | FVC,HR,SV,CO,MMV |
| Liang YW 2001(62) | CS | Guangdong, China | 33(15/18) | 66.7±7.4 | 64.6 ± 3.9 | Taijiquan | Non-intervention | No description | FVC,HR,SV,CO,MMV,SBP,DBP |
| Lai et al.1995 (63) | CS | Taiwan, China | 84(45/39) | 62.6±6.1 | 63.1±4.75 | Yang’s Tai Chi Chuan | Non-intervention | 54 minutes per time and 5 times per week for 2 years. | HR,VO2peak O2 pulse, MMV |
| Lan et al. 2004 (64) | CS | Taiwan, China | 24(12/12) | 58.8±7.9 | 59.9±5.2 | Yang’s Tai Chi Chuan | Non-intervention | 54 minutes per time and 3 times per week for 4.7±3.3 years. | HR,VO2peak O2 pulse, MMV |
| Lei et al.2001 (65) | SCT | Fujian, China | 39 | 6I.87±4.4 | Taijiquan. | 30 minutes per time and 7 to 14 times per week for 1 year. | SV,CO,VPE,EWK,HOV,SBP,DBP | ||
| Han YZ 2010 (66) | SCT | Jilin, China | 50 | 61.1±6.14 | Taijiquan | No less than 1 hour per time and mean 4 times per week for 6 months | HR,SBP,DBP,FVC | ||
| Wang GJ 2010 (67) | SCT | Jilin, China | 50 | 63.5±2.8 | Taijiquan | No description | SBP,DBP,HR,FVC,VO2peak,Step test index | ||
Abbreviations: RCT, randomized controlled trial; NRCT, non-randomized controlled trial; CS, Cohort study; SCT, Self-control trail; SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate; SV, stroke volume; CO, cardiac output; HOV, myocardial oxygen consumption; EWK, left heart energy effective utilization; VPE, left ventricular effective pump power; FVC, forced vital capacity; FEV1, forced vital capacity in the first second; MMV maximal minute ventilation; VO2peak, peak oxygen uptake; O2 pulse, oxygen pulse.
Methodological Quality
Of 2 included RCT, one trial described the random sequence generation by using the coin, and another utilized the blinding of outcome assessment. The remaining 18 trials were designed as non- randomized control, Self-control trial and cohort study. 3 studies indicated no dropouts. 4 studies reported dropouts as well as withdraw, and described their numbers and reason in detail. In all, all included studies were considered high risk of bias. The detail of risk of bias was illustrated in Table 2.
Table 2. The risk of bias about included studies.
| Author, year | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias | Total bias |
|---|---|---|---|---|---|---|---|---|
| Nguyen et al. 2012 (48) | Unclear | Unclear | High | High | Unclear | High | Unclear | High |
| Lu et al.2012 (49) | Low | Low | High | High | Unclear | High | Unclear | High |
| Tu HL 2005 (50) | High | High | High | High | Unclear | High | Unclear | High |
| Xu and Wen 1997 (51) | High | High | High | High | Unclear | High | Unclear | High |
| Liu and Jin 2010 (52) | High | Unclear | High | Unclear | Unclear | High | Unclear | High |
| Yang and Fu 2010 (53) | High | High | High | High | Unclear | High | Unclear | High |
| Lan et al. 1998 (54) | High | High | High | Unclear | Unclear | High | High | High |
| Chang et al.2013 (55) | High | High | High | Low | High | Unclear | Unclear | High |
| Thornton et al. 2004 (56) | High | High | High | Low | Unclear | Low | Unclear | High |
| Lu et al.2003 (57) | High | High | High | High | Unclear | High | Unclear | High |
| Rong et al. 2009 (58) | High | High | High | High | Unclear | Low | Unclear | High |
| Yan Y 2013 (59) | High | High | High | High | Unclear | High | Unclear | High |
| Li XH 2008 (60) | High | High | High | High | High | Unclear | Unclear | High |
| Peng CZ 2006 (61) | High | High | High | High | Unclear | High | Unclear | High |
| Liang YW 2001 (62) | High | High | High | High | Unclear | High | Unclear | High |
| Lai et al.1995 (63) | High | High | High | Unclear | Unclear | High | High | High |
| Lan et al. 2004 (64) | High | High | High | Unclear | Unclear | High | Unclear | High |
| Lei et al.2001 (65) | High | High | High | High | High | High | Unclear | High |
| Han YZ 2010 (66) | High | High | High | High | Unclear | Unclear | Unclear | High |
| Wang GJ 2010 (67) | High | High | High | High | Unclear | High | Unclear | High |
Measures of Effect
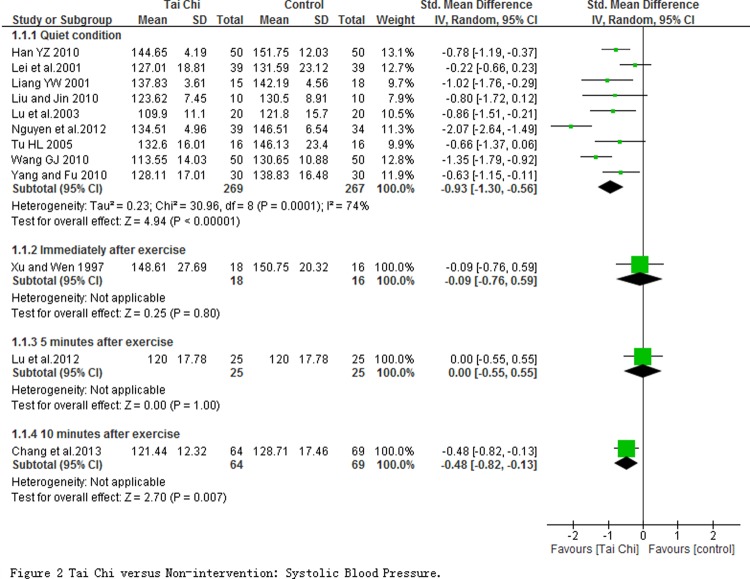
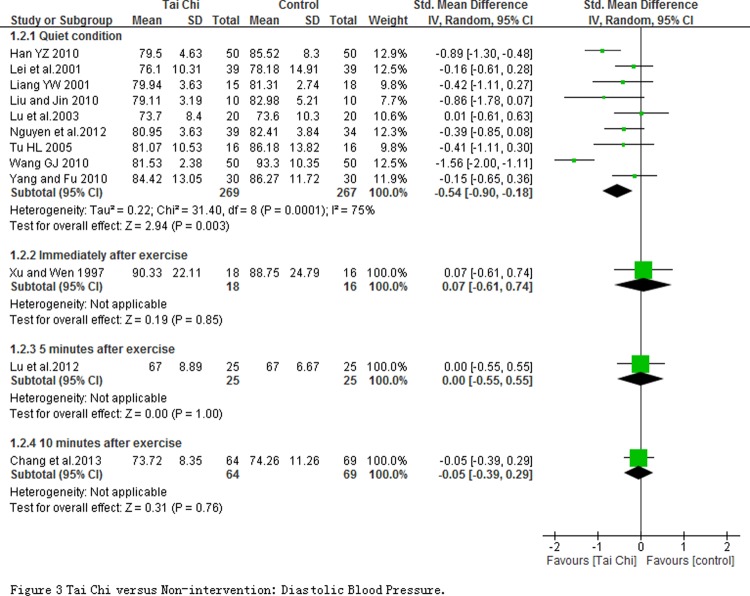
The effect of cardiovascular efficiency. 12 studies involving in 753 participants reported the systolic and diastolic blood pressures which were measured at quiet condition and at immediately as well as 5 and 10 minute after exercise. Meta-analyses including 9 studies with 536 subjects revealed that SPB (SMD = -0.93; 95% CI-1.30 to-0.56; P < 0.00001; Fig. 2) and DBP (SMD = -0.54, 95% CI-0.90 to-0.18, P < 0.00001; Fig. 3) in TC exercise group significantly decreased at quiet condition comparing with non-intervention group. But significant changes on SBP or DBP between groups were not observed at immediately, 5 and 10 minutes after exercise except for the SBP at 10 minute. Moreover, one non-randomized study reported that the blood pressure had a significant decrease regardless of systolic or diastolic blood pressure after 12 weeks TC training, whereas no obvious change was found in the control group [68].
Fig 2. Tai Chi versus Non-intervention: Systolic Blood Pressure.
Fig 3. Tai Chi versus Non-intervention: Diastolic Blood Pressure.
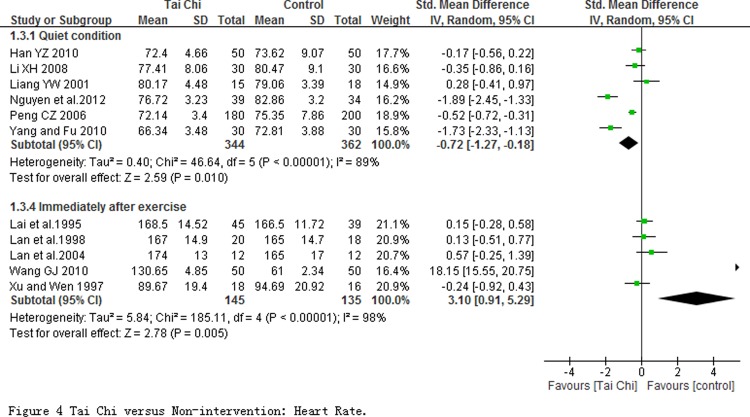
11 studies with 986 participants reported heart rate outcome which was measured at quiet condition in 6 studies and immediately after exercise in other 5 studies. Of 6 studies with HR measured at quiet condition, the pooled result of meta-analysis showed a significant decline (SMD = -0.72; 95% CI-1.27, -0.18; P = 0.010; Fig. 4). But heterogeneity among studies was substantive with I 2 = 89%, and not obviously changed after sensitivity analysis by removing any one of those studies. No study but one (Wang 2010) was found a significant effect on heart rate at immediately measured after exercise. But pooled analysis showed a significant increase (SMD = 3.10; 95% CI 0.91 to 5.29) with a substantive heterogeneity (I 2 = 98%, P = 0.005). The pooled result was changed as SMD being 0.13 (95% CI 0.17 to 0.42) with low heterogeneity (I 2 = 0%, P = 0.4) after sensitivity analysis was conducted by removing Wang 2010.
Fig 4. Tai Chi versus Non-intervention: Heart Rate.
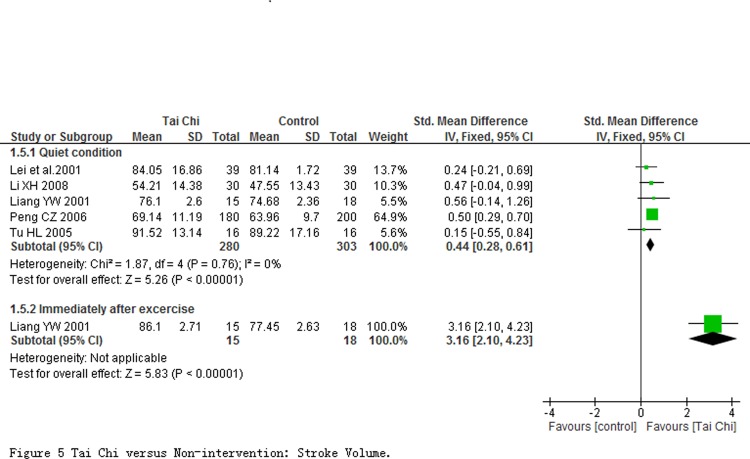
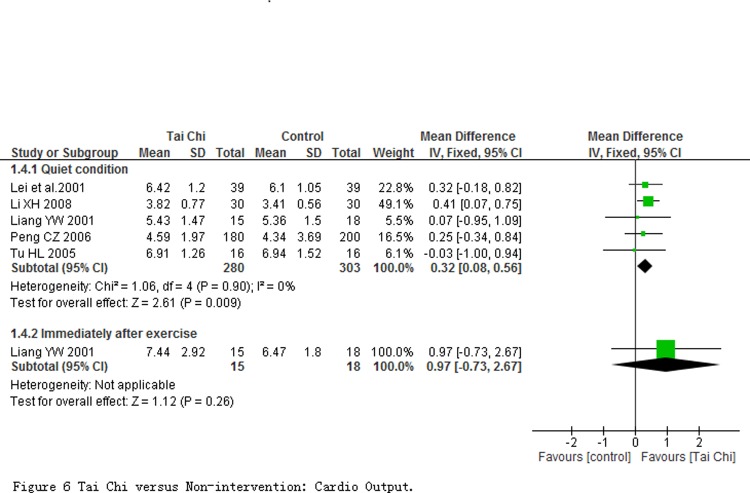
Stroke volume (SV) and cardio output (CO) were evaluated at quiet condition in 5 studies involving 583 participants, and were immediately evaluated after exercise in one study with 33 participants. Comparing to non-intervention, results of meta-analyses revealed that SV and CO in participants with TC exercise at quiet condition had a significant improvement with the pooled SMD of SV being 0.44 (95% CI 0.28 to 0.61; P < 0.00001; Fig. 5) and pooled MD of CO being 0.32 L/min (95% CI 0.08 to 0.56; P = 0.009; Fig. 6), respectively. One study reported a significant improvement in SV other than CO at immediately evaluated after exercise.
Fig 5. Tai Chi versus Non-intervention: Stroke Volume.
Fig 6. Tai Chi versus Non-intervention: Cardio Output.
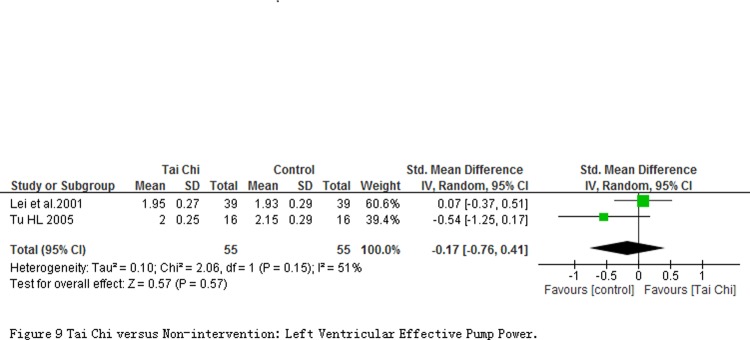
2 studies involving 110 participants measured outcomes about Myocardial oxygen consumption (HOV), Left heart energy effective utilization (EWK) and Left ventricular effective pump power (VPE) at quiet condition. Comparing to controls, the significant reduction on the HOV (MD = -4.11 mL/min; 95% CI-7.31 to-0.91; P = 0.01; Fig. 7) and increase on the EWK (MD = 0.02%; 95% CI 0.00 to 0.04; P = 0.03; Fig. 8) in participants with TC exercise were observed. But the significant changes was not found in the VPE outcome (MD = -0.03 Kg/n; 95% CI-0.14 to 0.07; P = 0.55; Fig. 9).
Fig 7. Tai Chi versus Non-intervention: Myocardial Oxygen Consumption.
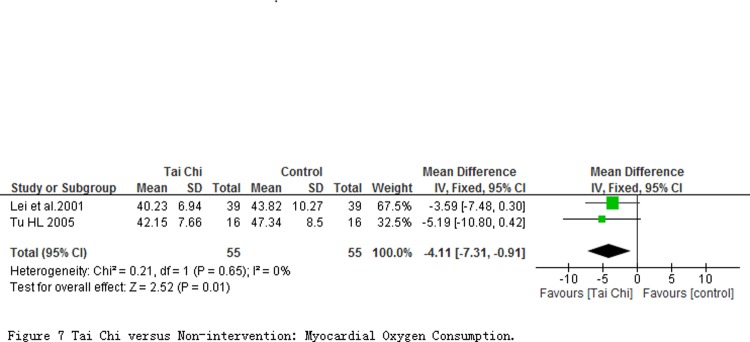
Fig 8. Tai Chi versus Non-intervention: Left Heart Energy Effective Utilization.
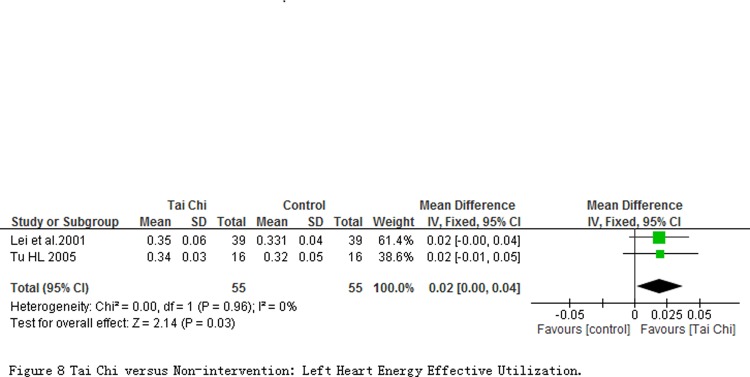
Fig 9. Tai Chi versus Non-intervention: Left Ventricular Effective Pump Power.
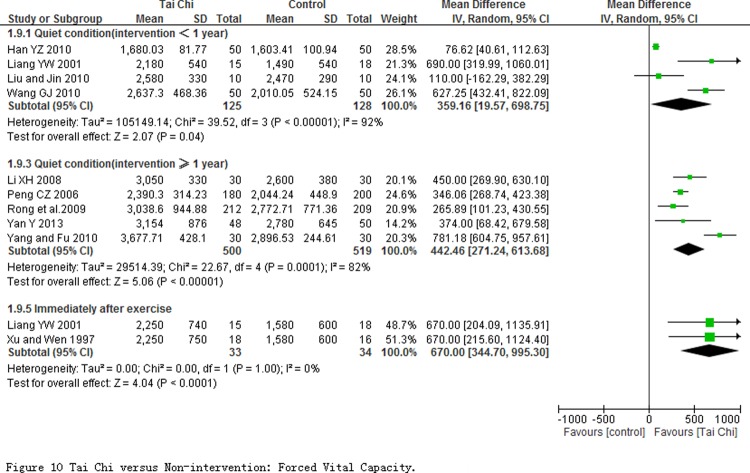
The effect of respiratory efficiency. Forced vital capacity (FVC) was measured at quiet condition in 9 studies (involving in 1272 participants), and measured immediately after exercise in 2 studies with 67 participants (Fig. 10). Comparing to non-intervention, Subgroup analyses showed TC exercise had a mean of 359.16 mL improvement (95% CI 19.57 to 698.75, P = 0.04) for less than one year intervention, and a mean of 442.46 mL improvement (95% CI 271.24 to 613.68, P <0.0001) for more than one year intervention. But heterogeneity among studies was substantive, and I 2 value were 92%, 82% respectively. The heterogeneity in subgroup with intervention period less than one year was not obviously changed after sensitivity analysis was performed by removing one of any studies. But in subgroup with intervention period more than one year, the heterogeneity among studies took an obvious change from I 2 = 82% to 0% when sensitivity analysis was conducted by removing Yang and Fu 2010. Additionally, when measured immediately after exercise, the pooled result from 2 studies showed TC training significantly enlarged the FVC efficiently (MD = 670.00 mL; 95% CI 344.70 to 995.30; P<0.0001).
Fig 10. Tai Chi versus Non-intervention: Forced Vital Capacity.
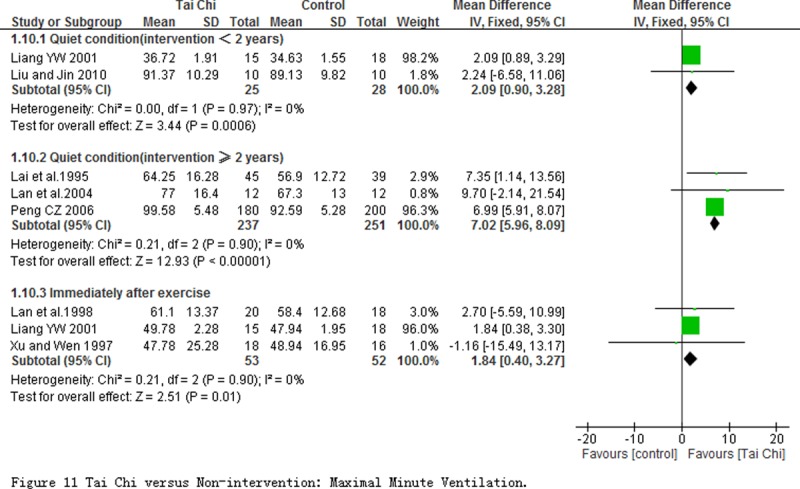
5 studies measured the maximal minute ventilation (MMV) at the quiet condition. Comparing to non-intervention, the subgroup analyses on the basis of the different intervention period showed TC exercise had significant improvement to MMV regardless of intervention period for less than 2 years (MD = 2.09 L/min; 95% CI 0.90 to 3.28; P = 0.0006) or more than 2 years (MD = 7.02 L/min; 95% CI 5.96 to 8.09; P<0.00001). 3 studies immediately evaluated this outcome after exercise, and the pooled result showed a obvious improvement of MMV (MD = 1.84 L/min; 95% CI 0.40 to 3.27; P = 0.01) in participants with TC exercise comparing with those with non-intervention (Fig. 11).
Fig 11. Tai Chi versus Non-intervention: Maximal Minute Ventilation.
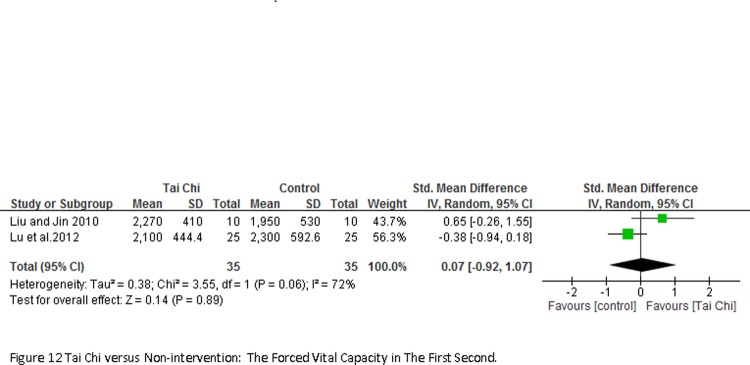
2 studies involving 70 participants reported the forced vital capacity in the first second (FEV1) measured at quiet condition (Fig. 12). Result of meta-analyses showed no significant changes between TC exercise and control groups (SMD = -0.07; 95% CI-0.92 to 1.07; P = 0.89).
Fig 12. Tai Chi versus Non-intervention: The Forced Vital Capacity in The First Second.
The peak oxygen uptake (V·O2peak) at quiet condition was evaluated in 4 studies with 246 participants (Fig. 13), and the pooled result showed a significant increase in TC exercise group (SMD = 1.33; 95% CI 0.97 to 1.70; P < 0.00001) with no heterogeneity.
Fig 13. Tai Chi versus Non-intervention: Peak Oxygen Uptake.
The effect of cardiorespiratory endurance. 3 studies (involving 146 participants, Fig. 14) reported the oxygen pulse (O2 pulse) at quiet condition. Comparing to non-intervention, the result of meta-analyses showed a significant improvement (SMD = 1.04; 95% CI 0.69 to 1.39; P < 0.00001) in participants with TC exercise.
Fig 14. Tai Chi versus Non-intervention: Oxygen Pulse.
4 studies with 679 participants reported stair test index at quiet condition. The pooled result revealed a significant SMD for the effect of TC exercise on stair test index at quiet condition (SMD = 1.34; 95% CI 0.27 to 2.40; P = 0.01; Fig. 15). But heterogeneity among studies was substantive (I 2 = 96%, P<0.00001), and no obvious changes in heterogeneity by sensitivity analysis through removing any one of those studies.
Fig 15. Tai Chi versus Non-intervention: Stair Test Index.
Adverse events
No included study reported the adverse events.
Discussion
Summary of Main Results
In this systematic review, 20 studies with 1783 healthy adults comparing TC exercise with non-intervention were included. The measured outcomes on CRF involved in cardiovascular efficiency, respiratory efficiency, and cardiorespiratory endurance. The review indicated that TC exercise might have a significant impact in improving cardiovascular efficiency by reducing resting blood pressure (SBP: SMD = -0.93; DBP: SMD = -0.94) and resting heart rate (SMD = -0.72), as well as enhancing stroke volume (MD = 0.44 mL/n) and cardiac output (MD = 0.32 L/min) at quiet condition, and HOV, EWK and VPE. There was substantial unexplained statistical heterogeneity observed in the resting blood pressure and resting heart rate, and small included studies in the HOV, EWK and VPE analysis, which suggested that the need for caution in interpreting these results. In addition, the present review also found significant improvement of TC exercise on respiratory function expressed by FVC, MMV, EFV1, VO2peak, and on cardiorespiratory endurance by measured stair test index and oxygen pulse. This review found no significant effect of Tai Chi exercise on VPE and EFV1. Nevertheless, these findings suggest that TC manifests promise as an optional exercise modality for the healthy adults to enhance CRF.
Tai Chi is a Chinese traditional mind-body exercise with a low to moderate exercise intensity [69]. The exercise intensity of TC mainly depends on its training style, posture and duration, and variation in training style and duration will result in substantial differences in exercise intensity [70]. In the present review, Yang style Tai Chi was used in six included studies, and other 14 studies did not report the definite style of TC practiced (only Taiji or Taijiquan). Furthermore, their training duration of TC varied greatly; the length of time ranged from 8 weeks to several years and frequency from 2 times to 7 times per week with 12 to 60 minute per time. These discrepancies may prevent to elucidate the potential applications for TC. Previous systematic reviews indicated that TC might be safe and effective in reducing blood pressure, improving aerobic capacity and exercise tolerance for patients with cardiovascular conditions and risk factors [71–72]. However, no previous review systematically assessed TC exercise for cardiorespiratory function regardless of healthy population or patients. A narrative review [73] demonstrated TC exercise had beneficial effects on outcomes of cardiorespiratory function including resting blood pressure, oxygen uptake (VO2), oxygen pulse, step index, and peak work rate in healthy older or patients with chronic disease. Another narrative review also suggested that Tai Chi exercise might have benefits to cardiovascular risk factors, such as hypertension, diabetes, dyslipidemia, poor exercise capacity, and endothelial dysfunction in patients with CVD, and indicated that Tai Chi exercise might promote cardiovascular health for patients with CVD [74]. However, these results are difficult to confirm the effect of TC for cardiorespiratory function owing to the unclear controls for evaluating the comparisons and unknown methodological quality in included studies.
Limitations and Suggestions for Future Research
This review and meta-analysis included 20 studies and covered randomized controlled, non- randomized controlled, self-controlled trial and cohort study. And the conclusion can be, to a great extent, certified more comprehensively and accurately owing to the diversity of experiments design. Even though the meta-analysis has confirmed some promising conclusions, there is also a great deal of limitation. The review extracted a large amount of non-random controlled trails and cohort study as well as 3 self-control trails which had inherent imperfection with poor quality of methodology and high risk of bias. The trails were filled with multifarious interference factor, and the results of meta-analysis were triggered to reach high heterogeneity and low reliability. Furthermore, another primary and extremely important limitation of this review is the subgroup analysis. Some of subgroups with certain outcomes only included one study or two due to the limitation of eligible trails. Until more trails are available with identical outcomes, we didn’t evaluate accurately and broadly the effect of TC to CRF.
The increasing number of healthy community-dwellers was inclined to selecting TC as their fitness programs thanks to the free of limitation of field, instrument and gender. TC is regarded as a kind of historic civilization treasure in China, adhering to the simple dialectical ideology which harmonizes Yin-Yang, dynamic-static state and facilitate homeostasis body and spirit. Especially, TC is a moderate form of exercise which requires control of balance and weight [75], and coordination of movements [76]. In addition to those, TC also need muscles relaxed whilst concentrating on the specific mental attention and mix deep breathing regulation and meditation together [77–78]. And just because of those, TC might be the preliminarily recommended as a fitness program for the adults especially for the elderly. TC has been shown to be a kind of effective program to improve CRF [21] and health fitness [54]. However, the research for TC is not lucubrated and comprehensive so far. We have searched more than ten thousands of studies in Chinese and over one thousand in English up to October 2013. Most of studies about TC cover balance, hypertension, autonomic nerve, cardiovascular, lung disease and so on. There are several trials about the influence of TC on the CRF for the elderly. However, no one study with low risk has described all the indicators about the CRF. And more random, single-blind paralleled trails are need conducted randomization and allocation concealment with more standardized outcomes.
Conclusion
The results of this review suggest that TC exercise is helpful for the healthy adults on improving the most outcomes of CRF, mainly on blood pressure, stroke volume, FVC, MMV, and VO2peak. However, concerning the low methodological quality, and the discrepancies of study design and TC training protocols in the included studies, the accurate conclusion can’t be drawn so far and these findings need to be interpreted cautiously. More larger-scale well-designed trails using standardized training protocols are needed till the specific and accurate conclusions can be perorated.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study is supported by the Collaboration Innovation Center for Rehabilitation Technology (number 1 Collaboration Center (2012)) and Rehabilitation Research Center for Traditional Chinese Medicine, State Administration of Traditional Chinese Medicine of the People’s Republic of China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Laukkanen JA, Kurl S, Salonen JT (2002) Cardiorespiratory fitness and physical activity as risk predictors of future atherosclerotic cardiovascular diseases. Curr Atheroscler Rep 4: 468–476. [DOI] [PubMed] [Google Scholar]
- 2. Rentis JM, Trenell MI, Vasdev N, French R, Dines G et al. (2013) Impaired cardiopulmonary reserve in an elderly population is related to postoperative morbidity and length of hospital stay after radical cystectomy. BJU Int 112: E13–19. 10.1111/bju.12219 [DOI] [PubMed] [Google Scholar]
- 3. Lee D-C, Artero EG, Sui X, Blair SN (2010) Mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol 24: 27–35. 10.1177/1359786810382057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP et al. (2013) Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J 77: 281–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y et al. (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301: 2024–2035. 10.1001/jama.2009.681 [DOI] [PubMed] [Google Scholar]
- 6. Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R et al. (2002) Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care 25: 1612–1618. [DOI] [PubMed] [Google Scholar]
- 7. Barlow CE, LaMonte MJ, Fitzgerald SJ, Kamprt JB, Perrin JL et al. (2006) Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. Am J Epidemiol 163: 142–150. [DOI] [PubMed] [Google Scholar]
- 8. Lang CC, Agostoni P, Mancini DM (2007) Prognostic significance and measurement of exercise-derived hemodynamic variables in patients with heart failure. Journal of Cardiac Failure 13: 672–679. [DOI] [PubMed] [Google Scholar]
- 9. Snowden CP, Prentis J, Jacques B, Anderson H, Manas D et al. (2013) Cardiorespiratory fitness predicts mortality and hospital length of stay after major elective surgery in older people. Ann Surg 257: 999–1004. 10.1097/SLA.0b013e31828dbac2 [DOI] [PubMed] [Google Scholar]
- 10. Malagrino PA, Sponton CH, Esposti RD, Franco-Penteado CF, Fernandes RA et al. (2013) Prevalence of dyslipidemia in middle-aged adults with NOS3 gene polymorphism and low cardiorespiratory fitness. Arq Bras Endocrinol Metabol 57: 33–43. [DOI] [PubMed] [Google Scholar]
- 11. Fujie S, Iemitsu M, Murakami H, Sanada K, Kawano H et al. (2013) Higher cardiorespiratory fitness attenuates arterial stiffening associated with the Ala54Thr polymorphism in FABP2. Physiol Genomics 45: 237–242. 10.1152/physiolgenomics.00089.2012 [DOI] [PubMed] [Google Scholar]
- 12. Yu R, Yau F, Ho SC, Woo J (2013) Longitudinal changes in physical activity levels over 5 years and relationship to cardiorespiratory fitness in Chinese midlife women. J Sports Med Phys Fitness 53: 680–686. [PubMed] [Google Scholar]
- 13. Sloan RA, Haaland BA, Leung C, Padmanabhan U, Koh HC et al. (2013) Cross-validation of a non-exercise measure for cardiorespiratory fitness in Singaporean adults. Singapore Med J 54: 576–580. [DOI] [PubMed] [Google Scholar]
- 14. Singhal N, Siddhu A (2014) Association of leisure-time physical activity with cardiorespiratory fitness in Indian men. J Phys Act Health 11: 296–302. 10.1123/jpah.2012-0029 [DOI] [PubMed] [Google Scholar]
- 15. Tsimaras V, Giagazoglou P, Fotiadou E, Christoulas K, Angelopoulou N et al. (2003) Jog-walk training in cardiorespiratory fitness of adults with Down syndrome. Percept Mot Skills 96: 1239–1251. [DOI] [PubMed] [Google Scholar]
- 16. Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H et al. (2006) Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur J Public Health 16: 179–184. [DOI] [PubMed] [Google Scholar]
- 17. Ahmaidi S, Masse-Biron J, Adam B, Choquet D, Freville M et al. (1998) Effects of interval training at the ventilatory threshold on clinical and cardiorespiratory responses in elderly humans. Eur J Appl Physiol Occup Physiol 78: 170–176. [DOI] [PubMed] [Google Scholar]
- 18. Govindasamy D, Paterson DH, Poulin MJ, Cunningham DA (1992) Cardiorespiratory adaptation with short term training in older men. Eur J Appl Physiol Occup Physiol 65: 203–208. [DOI] [PubMed] [Google Scholar]
- 19. Mossberg KA, Amonette WE, Masel BE (2010) Endurance training and cardiorespiratory conditioning after traumatic brain injury. J Head Trauma Rehabil 25: 173–183. 10.1097/HTR.0b013e3181dc98ff [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yan JH, Gu WJ, Sun J, Zhang WX, Li BW et al. (2013) Efficacy of Tai Chi on pain, stiffness and function in patients with osteoarthritis: a meta-analysis. PLoS One 8: e61672 10.1371/journal.pone.0061672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bu B, Haijun H, Yong L, Chaohui Z, Xiaoyuan Y et al. (2010) Effects of martial arts on health status: a systematic review. J Evid Based Med. 2010;3:205–19. 10.1111/j.1756-5391.2010.01107.x [DOI] [PubMed] [Google Scholar]
- 22. Hong Y, Li JX, Robinson PD (2000) Balance control, flexibility, and cardiorespiratory fitness among older Tai Chi practitioners. Br J Sports Med 34: 29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lan C, Chen SY, Lai JS, Wong AM (2013) Tai Chi Chuan in Medicine and Health Promotion. Evid Based Complement Alternat Med 2013: 502131 10.1155/2013/502131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheon SM, Chae BK, Sung HR, Lee GC, Kim JW (2013) The Efficacy of Exercise Programs for Parkinson’s Disease: Tai Chi versus Combined Exercise. J Clin Neurol 9: 237–243. 10.3988/jcn.2013.9.4.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Birdee GS, Cai H, Xiang YB, Yang G, Li H et al. (2013) T’ai chi as exercise among middle-aged and elderly Chinese in urban China. J Altern Complement Med 19: 550–557. 10.1089/acm.2012.0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee LY, Chong YL, Li NY, Li MC, Lin LN et al. (2013) Feasibility and effectiveness of a Chen-style Tai Chi programme for stress reduction in junior secondary school students. Stress Health 29: 117–124. 10.1002/smi.2435 [DOI] [PubMed] [Google Scholar]
- 27. Manson J, Rotondi M, Jamnik V, Ardern C, Tamim H (2013) Effect of tai chi on musculoskeletal health-related fitness and self-reported physical health changes in low income, multiple ethnicity mid to older adults. BMC Geriatr 13: 114 10.1186/1471-2318-13-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N et al. (2013) Efficacy of supervised Tai Chi exercises versus conventional physical therapy exercises in fall prevention for frail older adults: a randomized controlled trial. Disabil Rehabil 35: 1429–1435. 10.3109/09638288.2012.737084 [DOI] [PubMed] [Google Scholar]
- 29. Li J, Hong Y, Chan K (2001) Tai Chi: physiological characteristics and beneficial effects on health. Br J Sport Med 35: 148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yeh GY, Wang C, Wayne PM, Phillips RS (2008) The effect of tai chi exercise on blood pressure: a systematic review. Prev Cardiol 11:82–9. [DOI] [PubMed] [Google Scholar]
- 31. Lan C, Chen SY, Lai JS (2008) Changes of aerobic capacity, fat ratio and flexibility in older TCC practitioners: a five-year follow-up. Am J Chin Med 36: 1041–1050. [DOI] [PubMed] [Google Scholar]
- 32. Lan C, Chen SY, Lai JS, Wong MK (1999) The effect of Tai Chi on cardiorespiratory function in patients with coronary artery bypass surgery. Med Sci Sports Exerc 31:634–8. [DOI] [PubMed] [Google Scholar]
- 33. Xiong KY, He H, Ni GX (2013) Effect of skill level on cardiorespiratory and metabolic responses during Tai Chi training. Eur J Sport Sci 13: 386–391. 10.1080/17461391.2011.635706 [DOI] [PubMed] [Google Scholar]
- 34. Niu R, He R, Luo BL, Hu C (2014) The Effect of Tai Chi on Chronic Obstructive Pulmonary Disease: A Pilot Randomised Study of Lung Function, Exercise Capacity and Diaphragm Strength. Heart Lung Circ 23: 347–352. 10.1016/j.hlc.2013.10.057 [DOI] [PubMed] [Google Scholar]
- 35. Chan AW, Lee A, Lee DT, Suen LK, Tam WW et al. (2013) The sustaining effects of Tai chi Qigong on physiological health for COPD patients: a randomized controlled trial. Complement Ther Med 21: 585–594. 10.1016/j.ctim.2013.09.008 [DOI] [PubMed] [Google Scholar]
- 36. Lo HM, Yeh CY, Chang SC, Sung HC, Smith GD (2012) A Tai Chi exercise programme improved exercise behaviour and reduced blood pressure in outpatients with hypertension. Int J Nurs Pract 18: 545–551. 10.1111/ijn.12006 [DOI] [PubMed] [Google Scholar]
- 37. Taylor-Piliae RE, Hoke TM, Hepworth JT, Latt LD, Najafi B et al. (2014) Effect of Tai Chi on Physical Function, Fall Rates and Quality of Life Among Older Stroke Survivors. Arch Phys Med Rehabil 95: 816–824. 10.1016/j.apmr.2014.01.001 [DOI] [PubMed] [Google Scholar]
- 38. Leung RW, McKeough ZJ, Alison JA (2013) Tai Chi as a form of exercise training in people with chronic obstructive pulmonary disease. Expert Rev Respir Med 7: 587–592. 10.1586/17476348.2013.839244 [DOI] [PubMed] [Google Scholar]
- 39.See comment in PubMed Commons belowTaylor-Piliae RE, Froelicher ES (2004) Effectiveness of Tai Chi exercise in improving aerobic capacity: a meta-analysis. J Cardiovasc Nurs 19:48–57. [DOI] [PubMed] [Google Scholar]
- 40. Taylor-Piliae RE (2008) The effectiveness of Tai Chi exercise in improving aerobic capacity: an updated meta-analysis. Med Sport Sci 52:40–53. 10.1159/000134283 [DOI] [PubMed] [Google Scholar]
- 41. Lee MS, Lee EN, Emst E (2009) Is tai chi beneficial for improving aerobic capacity? A systematic review. Br J Sport Med 43:569–73. 10.1136/bjsm.2008.053272 [DOI] [PubMed] [Google Scholar]
- 42. Savović J, Weeks L, Sterne JA, Turner L, Altman DG et al. (2014) Evaluation of the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials: focus groups, online survey, proposed recommendations and their implementation. Syst Rev 3: 37 10.1186/2046-4053-3-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Minton O, Richardson A, Sharpe M, Hotopf M, Stone P (2008) A systematic review and meta-analysis of the pharmacological treatment of cancer-related fatigue. J Natl Cancer Inst 100: 1155–1166. 10.1093/jnci/djn250 [DOI] [PubMed] [Google Scholar]
- 45. Lan C, Lai JS, Chen SY, Wong MK (2001) 12-month Tai Chi training in the elderly: its effect on health fitness. Medicine & Science in Sports &Exercise 5: 12–19. 10.1002/bmc.3406 [DOI] [PubMed] [Google Scholar]
- 46. Motivala SJ, Sollers J, Thayer J, Irwin MR (2006) Tai Chi Chih Acutely Decreases Sympathetic Nervous System Activity in Older Adults. J Gerontol A Biol Sci Med Sci 61: 1177–1180. [DOI] [PubMed] [Google Scholar]
- 47. Fu X, Guo J (2009) The effect of Tai Chi training on the function and component of physical health in the elderly. Journal of Gansu Normal Colleges 14: 73–76. [Google Scholar]
- 48. Nguyen MH, Kruse A (2012) The effects of Tai Chi training on physical fitness, perceived health, and blood pressure in elderly Vietnamese. Open Access J Sports Med 3: 7–16. 10.2147/OAJSM.S27329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lu WA, Kuo CD (2012) Effect of 3-Month Tai Chi Chuan on Heart Rate Variability, Blood Lipid and Cytokine Profiles in Middle-Aged and Elderly Individuals. International Journal of Gerontology 6: 267–272. [Google Scholar]
- 50. Tu HL (2005) The effects of different exerciseS on the elderly cardiovascular system. Journal of Wuhan Institute of Physical Education 39: 70–73. [Google Scholar]
- 51. Xu M, Wen ZH (1997) The changes in cardiorespiratory function following before and after Tai Chi training in the elderly. Journal of Chengdu Physical Education Institude 3: 79–82. [Google Scholar]
- 52. Liu XD, Jin HZ (2010) The effect of Tai Chi training on cardiovascular fitness in the elderly. China Practice Medicine 5: 34–35. [Google Scholar]
- 53. Yan Y, Fu X (2010) The effect of Tai Chi on physical health in the mid-aged and elderly. Science Information 28: 271–272. [Google Scholar]
- 54. Lan C, Lai JS, Chen SY, Wong MK (1998) 12-month Tai Chi training in the elderly: its effect on health fitness. Med Sci Sports Exerc 30: 345–351. [DOI] [PubMed] [Google Scholar]
- 55. Chang MY, Yeh SC, Chu MC, Wu TM, Huang TH (2013) Associations Between Tai Chi Chung Program, Anxiety, and Cardiovascular Risk Factors. Am J Health Promot 28: 16–22. 10.4278/ajhp.120720-QUAN-356 [DOI] [PubMed] [Google Scholar]
- 56. Thornton EW, Sykes KS, Tang WK (2004) Health benefits of Tai Chi exercise: improved balance and blood pressure in middle-aged women. Health Promot Int 19: 33–38. [DOI] [PubMed] [Google Scholar]
- 57. Lu WA, Kuo CD (2003) The effect of Tai Chi chuan on the autonomic nervous modulation in older persons. Med Sci Sports Exerc 35: 1972–1976. [DOI] [PubMed] [Google Scholar]
- 58. Rong XJ, Li CZ, Liang DD (2009) The effect of Tai Chi exercise on cardiorespiratory function in the mid-aged and elderly. Chinese Journal of Rehabilitation Medicine 24: 345–347. [Google Scholar]
- 59. Yan Y (2013) The effect of 24-type Tai Chi exercise on cardiorespiratory function in the mid-ade and elderly. Journal of Liaoning Normal University(Natural Science Edition) 36: 124–127. [Google Scholar]
- 60. Li XH (2008) The effect of Tai Chi training on cardiorespiratory function in the male elderly. Journal of Henan Normal University (Natural Science) 36: 123–125. [Google Scholar]
- 61. Peng CZ (2006) The effect of Tai Chi training on body composition and cardiorespiratory function in the elderly. Fighting and martial science 6: 32–34. [Google Scholar]
- 62. Liang YW (2001) The effect of Tai Chi exercise on cardiorespiratory function in the elderly. Journal of Physical Education 8: 64–66. [Google Scholar]
- 63. Lai JS, Lan C, Wong MK, Teng SH (1995) Two-Year Trends in Cardiorespiratory Function Among Older Tai Chi Chuan Practitioners and Sedentary Subjects. J Am Geriatr Soc 43:1222–1227. [DOI] [PubMed] [Google Scholar]
- 64. Lan C, Chou SW, Chen SY, Lai JS, Wong MK (2004) The Aerobic Capacity and Ventilatory Efficiency During Exercise in Qigong and Tai Chi Chuan Practitioners. Am J Chin Med 32: 141–150. [DOI] [PubMed] [Google Scholar]
- 65. Lei XS, Ni HY, Chen QY, Zheng HW, Huang YF et al. (2001) The effect of 42-type Tai Chi exercise on cardiovascular function and Respiratory endurance in the mid-ade and elderly. Modern Rekabitltalion Journal 5: 64–65. [Google Scholar]
- 66.Han YZ (2010) Study on the phased evaluation of Tai chi training on Lung and Heart Function and ability of balance for elderly person. National Traditional Sports College, Northeast Normal University.
- 67. Wang GJ (2010) The effect of Tai Chi training on cardiorespiratory function in the elderly. Chinese Journal of Gerontology 12: 3802–3803. [Google Scholar]
- 68. Thornton EW, Sykes KS, Tang WK (2004) Health benefits of Tai Chi exercise: improved balance and blood pressure in middle-aged women. Health Promot Int 19: 33–38. [DOI] [PubMed] [Google Scholar]
- 69. Lan C, Chen SY, Lai JS (2004) Relative exercise intensity of Tai Chi Chuan is similar in different ages and gender. Am J Chin Med 32:151–60. [DOI] [PubMed] [Google Scholar]
- 70. Lan C, Chen SY, Lai JS (2008) The exercise intensity of Tai Chi Chuan. Med Sport Sci 52:12–9. 10.1159/000134225 [DOI] [PubMed] [Google Scholar]
- 71. Yeh GY, Wang C, Wayne PM, Phillips R (2009) Tai chi exercise for patients with cardiovascular conditions and risk factors: A SYSTEMATIC REVIEW. J Cardiopulm Rehabil Prev 29:152–60. 10.1097/HCR.0b013e3181a33379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ng SM, Wang CW, Ho RT, Ziea TC, He J, et al. (2012) Tai chi exercise for patients with heart disease: a systematic review of controlled clinical trials. Altern Ther Health Med 18:16–22. [PubMed] [Google Scholar]
- 73. Li JX, Hong Y, Chan KM (2001) Tai Chi: physiological characteristics and beneficial effects on health. Br J Sport Med 35: 148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lan C, Chen SY, Wong MK, Lai JS (2013) Tai chi chuan exercise for patients with cardiovascular disease. Evid Based Complement Alternat Med 2013:983208 10.1155/2013/983208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Gatts S (2008) A Tai Chi Chuan training model to improve balance control in older adults. Curr Aging Sci 1: 68–70. [DOI] [PubMed] [Google Scholar]
- 76. Verhagen AP, Immink M, van der Meulen A, Bierma-Zeinstra SM (2004) The efficacy of Tai Chi Chuan in older adults:a systematic review. Fam Pract 21: 107–113. [DOI] [PubMed] [Google Scholar]
- 77. Ho RT, Au Yeung FS, Lo PH, Law KY, Wong KO et al. (2012) Tai-Chi for Residential Patients with Schizophrenia on Movement Coordination, Negative Symptoms, and Functioning: A Pilot Randomized Controlled Trial. Evid Based Complement Alternat Med 2012: 923925 10.1155/2012/923925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Yeh GY (2008) Commentary on the Cochrane review of Tai Chi for rheumatoid arthritis. Explore (NY) 4: 275–27. 10.1016/j.explore.2008.04.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.