Abstract
Context:
The rising popularity and intensity of youth sports has increased the incidence of patellar dislocation. These sports-related injuries may be associated with significant morbidity in the pediatric population. Treatment requires understanding and attention to the unique challenges in the skeletally immature patient.
Evidence Acquisition:
PubMed searches spanning 1970-2013.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
Although nonoperative approaches are most often suitable for first-time patellar dislocations, surgical treatment is recommended for acute fixation of displaced osteochondral fractures sustained during primary instability and for patellar realignment in the setting of recurrent instability. While a variety of procedures can prevent recurrence, the risk of complications is not minimal.
Conclusion:
Patellar stabilization and realignment procedures in skeletally immature patients with recurrent patellar dislocation can effectively treat patellar instability without untoward effects on growth if careful surgical planning incorporates protection of growth parameters in the skeletally immature athlete.
Keywords: patellar instability, patellar dislocation, pediatric, adolescent
Patellar instability is characterized by dislocation or subluxation of the patella relative to the femoral trochlea, almost always in the lateral direction.22,27 Medial instability has been described, but almost exclusively in association with iatrogenic causes after treatment of lateral instability.43,70,95 Lateral patellar dislocation generally reflects either subtle congenital or trauma-induced anatomic abnormalities that can interfere with normal patellofemoral biomechanics, tracking, and knee function. With the continuing rise in participation and intensity of youth sports, more traumatic primary patellar dislocations are being seen in the pediatric and adolescent populations.36,49,91 After a sentinel dislocation, anywhere from 7% to 71% of patients have instability symptoms or events.24,36,52,72,75 The associated injuries may evolve into a chronic pathologic condition, with recurrent dislocations with minor trauma or attempted sports participation.36 Patients may also experience disconcerting anterior knee pain and apprehension of instability events, which may significantly interfere with activities of daily life.
To address this challenge, investigators have focused on enhancing the understanding of patellofemoral joint biomechanics through advanced imaging, modeling, and cadaveric investigations, with the goal of elucidating the critical factors of patellar stability. Building on emerging findings, a wide range of operative techniques have been proposed to prevent chronic or recurrent patellar instability. This diversity of treatment options underscores the continued controversy in the field regarding the optimal surgical approach. This is further complicated in the skeletally immature individual, in which case careful consideration of physeal and apophyseal anatomy is required.
Epidemiology
A recent database study of American emergency departments selected to represent the demographics of the US population estimated the incidence of patellar dislocation at 2.29 per 100,000 person-years for all age groups.100 However, the rates of acute, traumatic patellar dislocation peaked among adolescents 15 to 19 years old, with an incidence of 11.19 per 100,000 person-years. These injuries among young patients most often occurred during sporting activities, with approximately half of patients experiencing patellar dislocation during athletics. The most common sports involved were basketball, soccer, and football.100 Supporting evidence for increased incidence of patellar dislocation in young, active patients is common, with increased rates of patellar dislocation seen in subgroups such as active US military personnel, in whom the incidence is at 69 per 100,000 person-years at risk.42 Service members <20 years old were 84% more likely (95% CI, 1.61-2.10) to have patellar dislocation compared with those at or above the age of 40 years.42
Some of the same studies have worked to identify sex and racial differences in incidence of patellar dislocation. Originally, many believed that chronic, atraumatic recurrent patellofemoral instability occurred primarily in adolescent females in part because of increased joint laxity and physiologic or pathologic variations in lower joint alignment, such as genu valgum, femoral anteversion, external tibial torsion, and elevated Q-angles.36,42,64 However, recent data do not substantiate an increased incidence in women.100 Nevertheless, patellar dislocation occurs more frequently in children with connective soft tissue disorders or hypermobility syndromes, such as Ehlers-Danlos syndrome and Down syndrome.92 There is also some evidence that Caucasians and African-Americans may have increased rates of patellar dislocation, when compared with other races.42,100
Potential differences in rates of patellar dislocation by race and sex may also suggest an underlying genetic component to patellar instability. To support this hypothesis, several studies have questioned those presenting with patellar dislocation for a family history of knee instability. Reports ranging from 9% to greater than 50% have been found, depending on the source population and the method of sampling and inclusion criteria.8,29,80 Furthermore, reports of families with underlying abnormal anatomical features in association with recurrent patellar dislocations supports a genetic role for some proportion of these events.59,78 Most important, patients with prior instability episodes are 7 times more likely to have a recurrence,36 reflecting the dual roles of both a likely congenital predisposition toward instability in some cases and the clear destabilizing role of trauma in precipitating further instability in others.36
Anatomy
The normally concave trochlear groove and corresponding convex patellar subchondral surface are the osseous structures guiding patellar articulation. The groove has a complex architecture with increasing height of the groove’s lateral facet at the proximal aspect, providing a deeper “patellar track” in knee extension. Midway between flexion and extension, as increased forces are imposed by the patellar tendon and quadriceps musculotendinous unit, the patella comes into greatest contact with the femur’s articular surface. At 20° to 30° flexion, the patellar articular surface is most constrained by the walls of the trochlear groove.3,27,101 Failure of full bony engagement of the patella into the trochlear groove can manifest as patellar instability. Patients with patella alta may have abnormal patellar engagement with the trochlear groove during knee flexion and recurrent patellar dislocation.16,44,52,99 The importance of this feature in patellar instability underscores the importance of familiarity with one or more quantification methods of anatomic patellar height, including the Insall-Salvati ratio and the Blackburne-Peel modification.20
Just as the steepness of the patellar facets and the depth of the trochlear groove can prevent dislocation of the patella,77 conversely, trochlear dysplasia, or shallowness of the groove, can predispose to patellar instability. For example, in 1 study, up to 96% of patients with patellar dislocation had some degree of trochlear dysplasia.31 This type of abnormal bony architecture results in specific radiographic signs, including the Dejour “crossing sign” (Figure 1).31,33,81 Imaging can also allow for categorization of trochlea dysplasia into 4 types (A through D) via the classification system of Dejour.53 More recent work has used magnetic resonance imaging (MRI) to further delineate anatomical features of the trochlea that predispose patients to patellar instability.9,19,76
Figure 1.

Crossing sign on a lateral radiograph is the intersection of the trochelear floor and the most anterior edge of the lateral femoral condyle. Reproduced with permission from Dejour et al.31
Patellar dysplasia is another pathologic factor that may play a role in patellar instability. Patellar shape can be classified via the 3 Wiberg classifications (type A to C),11 which rely on medial facet concavity and lateral to medial patellar facet area. A longer lateral patellar facet has been shown to predispose patients to patellar instability.37,74
Soft tissue structures play a critical role in patellar stability. The Q angle, between the 2 force vectors of the patellar tendon and quadriceps tendon, increases with extension. As the knee extends and the Q angle increases, the extensor mechanism force pulls the patella laterally. Other lateralizing soft tissue structures include 3 layers of the lateral retinaculum, which can paradoxically also act as a lateral restraint against dislocation. Most superficially, the medial fascial extensions of the iliotibial band connect with the patellar and quadriceps tendons. The second layer of the lateral retinaculum consists of the lateral patellofemoral band, and the third or deepest synovial layer is part of the knee capsule (Figure 2).27 Combined with the horizontal vector generated through the Q angle, these soft tissue supports lateralize the patella. Of note, the Q angle is often difficult to clinically determine. One imaging parameter somewhat analogous to the Q angle is the tibial tubercle–trochlear groove (TT-TG) distance, which may be measured with advanced 3-dimensional imaging, such as computed tomography (CT) scans or MRI. The TT-TG distance is commonly used to determine one of the anatomic factors causing instability (Figure 3).28 In adults, 9 to 11 mm is generally considered normal; a pathological TT-TG distance is >20 mm or >15 mm, depending on the population studied.31,48,73 The TT-TG distances in skeletally immature athletes are significantly different between those with and without patellar dislocation.10 Specifically, the TT-TG distance was on average 4 mm larger in patients with patellar dislocation. Of note, the association of larger TT-TG distance with patellar dislocation did not change with age. However, approximately 10% of patients without patellar dislocation had a TT-TG distance >15 mm, emphasizing that not all knees with increased TT-TG distance are unstable.10
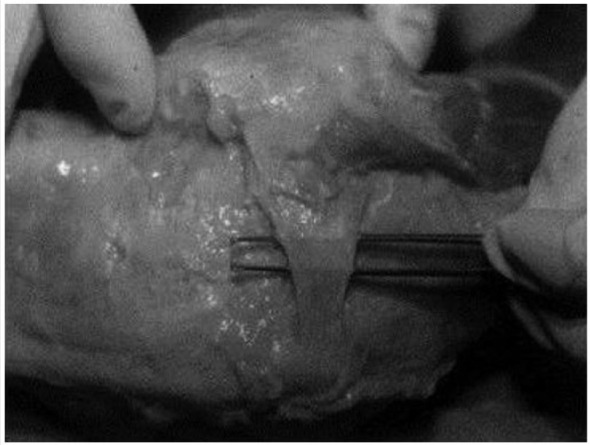
Figure 2.
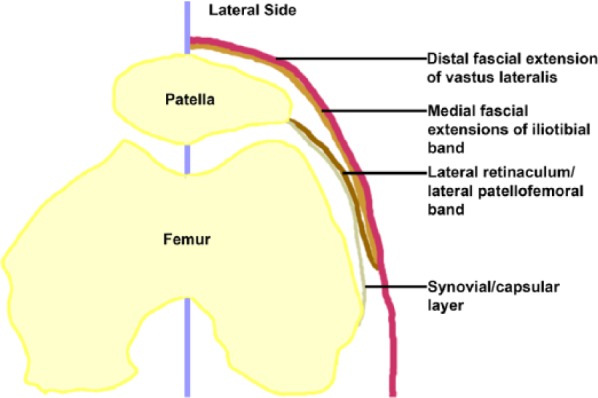
Lateral soft tissue structures.
Figure 3.
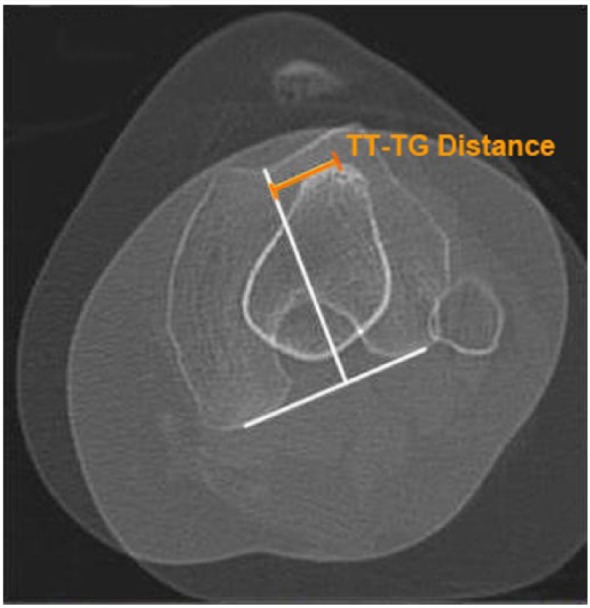
The tibial tubercle–trochlear groove (TT-TG) distance is determined by a line from the most anterior point of the tibial tuberosity to the line running through the trochlear groove (orange). Modified from Cooney et al28 with permission.
On the medial side of the knee, the medial patellofemoral ligament (MPFL) represents the primary soft tissue constraint that counteracts patellar lateralization and instability. The MPFL is a fascial band extending from the medial border of the patella to a site near the medial femoral epicondyle (Figure 2).4,79 Despite the MPFL being relatively thin and, at times, difficult to identify as a distinct anatomic structure, its mean tensile strength is 208 N.4 It is a widely accepted critical component of medial patellar stability, and may account for approximately 50% of the medial stabilizing force in the knee.18,32 The medial patellomeniscal ligament is a minor medializing force, providing approximately 13% of the restraint to lateral dislocation.1,32,86
One of the controversies surrounding MPFL anatomy is the location of the insertion site relative to the medial distal femoral physis (Figures 4 and 5). This is particularly important in procedures involving skeletally immature athletes because MPFL reconstruction must take care to avoid physeal disruption. Based on imaging studies in children and adolescents, the MPFL midpoint is 2 to 5 mm proximal to the medial femoral physis.88 However, other conflicting reports have emerged demonstrating a femoral insertion of the MPFL at an average of 5 mm distal to the medial physis in children and adolescents.47,62 The primary limitation of fixation of any MPFL reconstruction construct proximal to the physis in a growing child is the concern of proximal migration of the graft with continued growth, thereby altering the vector of the intended patellar checkrein. Currently, no consensus on the pattern of MPFL insertion relative to the medial femoral physis exists; the attachment site may migrate proximally with age.13 The insertion site is relatively close to the physis; surgical techniques may be associated with a risk of injury to the growth plate.
Figure 4.
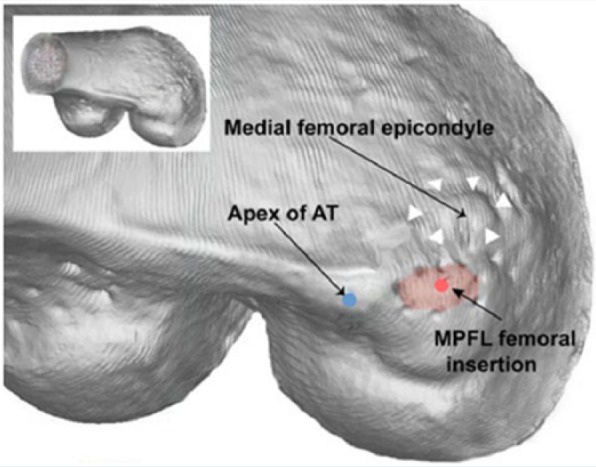
Medial patellofermoral ligament (MPFL) insertion site with the adductor tubercle and the medial femoral epicondyle. Blue dot, adductor tubercle apex; white triangle, medial femoral epicondyle; red area, MPFL insertion site. Modified from Fujino et al38 with permission.
Figure 5.
The medial patellofemoral ligament (MPFL). Reproduced with permission from Amis et al.4
An additional soft tissue constraint against patellar lateralization and instability is the medial quadriceps tendon–femoral ligament (MQTFL). Although originally described as part of the MPFL, the MQTFL has also been named and identified as a distinct structure to aid the development of new surgical targets for stabilization of patellar tracking.39,46,60 Based on cadaveric dissection studies performed by both Mochizuki et al60 and Fulkerson and Edgar,39 this structure originates from the distal anterior adductor tubercle and runs anteriorly to insert on the distal quadriceps tendon underneath the medialis muscle.
Finally, muscular forces from the vastus medialis obliquus (VMO) and vastus lateralis should provide balance in the femoral anatomical axis. Asymmetry of these muscle forces may play a role in lateral patellar dislocation.35
History and Physical Examination
In the pediatric and adolescent population, patellar dislocation usually occurs during sporting activities in which the leg internally rotates relative to a fixed foot, often including simultaneous quadriceps contraction. In 10% of cases, however, dislocation may occur from direct trauma to the medial patellar surface.50 As the patella dislocates laterally, the medial soft tissue supports, primarily the MPFL, are stretched or torn. Either the initial dislocation or a subsequent reduction can result in osteochondral fractures. Post–patellar dislocation MRI findings often include MPFL injury at either or both of its attachment sites, VMO edema, and/or osteochondral fractures.84
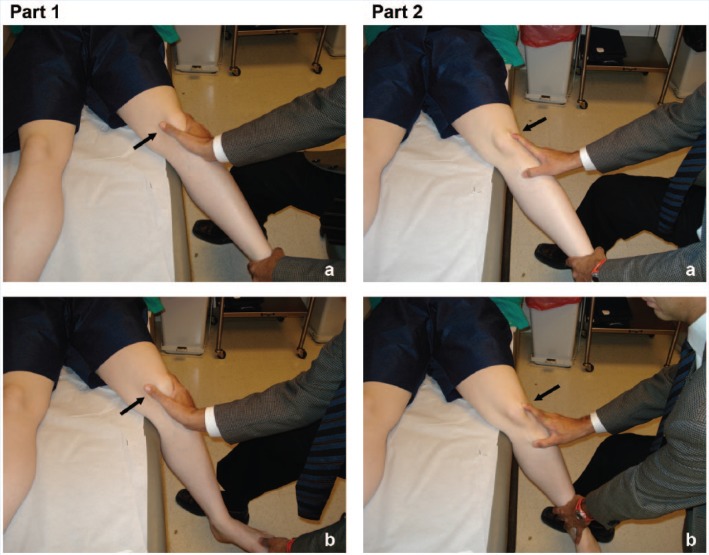
Physical examination findings consistent with patellar instability include the “Bassett sign” (tenderness to palpation over the medial femoral epicondyle at the MPFL attachment site), tenderness over the medial facet of the patella and the lateral aspect of the lateral femoral condyle, and a positive lateral patellar apprehension test.12,90 However, these tests have variable sensitivity.83 The moving patellar apprehension test for lateral patellar instability has a sensitivity of 100% and specificity of 88.4% (Figure 6).2
Figure 6.
The moving patellar apprehension test. The examiner moves the knee from full extension into flexion while simultaneously translating the patella laterally as far as possible in the first part. In part 2, the examiner flexes the knee to 90° and subsequently returns the knee to full extension while applying medial force of the patella. For a positive test, the patient expresses apprehension and/or activates the quadriceps with flexion and lateral translation of the patella during the first part of the test, while also experiencing no discomfort during the second part of the test. Reproduced with permission from Ahmad et al.2
Diagnostic Imaging
Standard workup for patellar instability includes anteroposterior, lateral, and 1 of several patellofemoral views (sunrise/skyline view at 20° of flexion or a Merchant view at a 30° downward angle on a knee flexed at 45°).58 Patients with an acute dislocation may not tolerate these flexion views. A standing alignment radiograph (hips-to-ankles) may be prudent to quantify additional risk factors for patellar instability, such as genu valgum.
For patellar height, the Insall-Salvati ratio is the vertical length of the patella over the length of the patellar tendon (from the inferior pole of the patella to the tendon’s corresponding insertion on the top of the tibial tubercle).45,98 Alternatively, the Blackburn-Peel ratio is the length of the patellar articular surface divided by the distance from the distal patella to a line crossing through the lowest pole of the tibial plateau.17,85 Trochlear dysplasia is evaluated on lateral radiographs by the crossing sign (see Figure 1).27,31 The Merchant view may also be used to assess patellar tilt on the sulcus angle and patellar subluxation by the congruence angle (Figures 7 and 8).58
Figure 7.
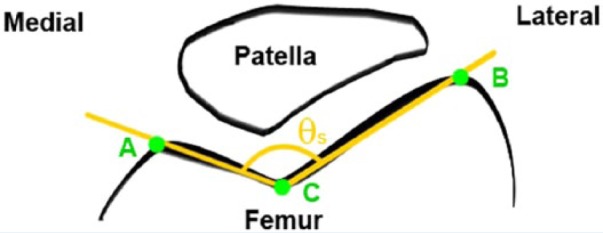
Sulcus angle (θs) is the angle between 2 intersecting lines drawn between the highest point of the medial femoral condyle (A), lowest point of the intercondylar sulcus (C), and the highest point of the lateral femoral condyle (B).
Figure 8.
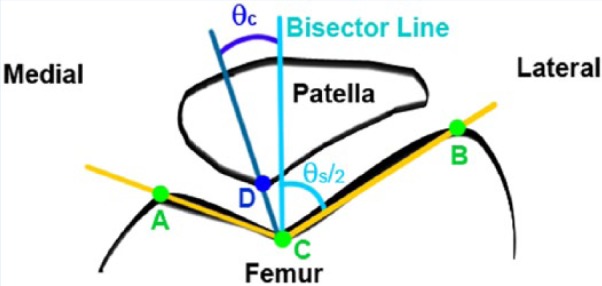
The congruence angle (θc) is determined by measuring the angle formed between a line bisecting the sulcus angle (θs), labeled “bisector line” in the figure, and a line from the lowest point of the intercondylar sulcus (C) and the lowest point on the articular ridge of the patella (D).
In mixed adult/pediatric patient populations, the MPFL’s femoral attachment is the most likely the site of injury.67,83 The MR STIR (short tau inversion recovery) sequence more precisely identifies MPLF disruption.47
Nonoperative Treatment
Nonoperative treatment remains the gold standard of treatment after primary patellar dislocation without osteochondral fragments.41,55,72 There is a lack of evidence supporting improved outcomes after surgery for a single dislocation.7,89,93 After primary patellar dislocation, nonoperative treatment can be successful in the majority of patients with early initiation of physical therapy and initial support with a knee immobilizer or hinged knee brace locked in extension for ambulation.24,27,57 Lateral patellar stabilization braces often enhance the patient’s sense of patellar stability.
Operative Treatment
In cases of primary patellar dislocation associated with large (>5 mm) displaced osteochondral fractures or chondral shear fragments, and/or complete avulsion of the VMO from the patellar insertion site, surgery may be indicated. In skeletally immature children, refixation of loose fragments, even those that are chondral-only in nature (ie, no bone on the backside of the fragment), should be considered.23,25,26,61,66,72,82,96 Lateral release, or division of the lateral retinacular tissue during removal of the osteochondral fragment, is controversial.15,51,54
Skeletally immature patients often have recurrent patellar dislocations after a sentinel dislocation.8 Young age at the time of primary dislocation is a risk factor for recurrence, with redislocation rates ranging from 7.14% to 71% (Table 1).5,52,72 Each additional dislocation can significantly increase the chances of further recurrence,36,72 which carry a substantial risk of irreparable cartilage damage and future patellofemoral arthritis.68,69 Cartilage injuries, ranging from severe fissuring to frank chondral defects, may occur in 95% of cases of patellar dislocation.69 Conservative treatments alone are therefore generally not considered adequate treatment for chronic instability. Unlike surgical treatments in adults, realignment and reconstruction approaches in children are associated with physeal injury and growth disturbance.63,97
Table 1.
Summary of published evidence regarding the rate of patellar dislocation after sentinel subluxation or dislocation
| Study authors (date) | Mean follow-up time | Age in years, range (mean) | Number of participants | Recurrence rate of patellar dislocation after sentinel subluxation or dislocation (%) |
|---|---|---|---|---|
| Apostolovic et al (2011)5 | Randomized prospective trial with mean follow-up time of 6.1 y | 12-16 (14.26) | 23 | 7.14 |
| Palmu et al (2008)72 | Randomized prospective trial with mean follow-up time of 14 y | 9-15 (13) | 28 | 71 |
| Lewallen et al (2013)52 | Single institution retrospective review with mean follow-up time of 3.1 y | 9-18 (14.9) | 198 | 38.4 (If immature physis and trochlear dysplasia, rate 69%) |
| Sillanpää et al (2009)89 | Randomized prospective trial with mean follow-up time of 7.0 y | 19-21 (20) | 21 | 29 |
| Nikku et al (2005)65 | Randomized prospective trial with mean follow-up time of 7.2 y | Range not reported, SD = 8 (20) | 57 | 39 |
| Christiansen et al (2008)26 | Randomized prospective trial with mean follow-up of 2 y | 13-39 (20) | 35 | 20 |
A variety of bony realignment procedures have been proposed to address patellar instability in adults but remain inapplicable to children and adolescents with open growth plates. Tibial-based bony realignment procedures are contraindicated in children with an open tibial tubercle apophysis because of the likelihood of an anterior tibial growth arrest and tibial recurvatum deformity. However, adolescent patients with closed growth plates can safely undergo tibial tubercle osteotomies or other bony realignment procedures.
As patients of increasingly younger age are presenting with greater incidence of patellar instability, the emergence of soft tissue–based procedures designed to respect physeal and apophyseal integrity has advanced our ability to address this spectrum of pathology in the skeletally immature athlete.63 Several soft tissue realignment techniques historically used in children include the Galeazzi semitendinosus tenodesis,40 the Roux-Goldthwait procedure,56 and the “3-in-1” procedure.71 However, a recent study with 70-month mean follow-up on 34 knees with the Galeazzi technique demonstrated that 41% of cases were associated with International Knee Documentation Committee (IKDC) scores <70 at final follow up, with 35% of patients being symptomatic enough to warrant repeat surgeries.9,40 Of note, surgeons must avoid excessive lateral release of the retinaculum, which can lead to continued lateral instability, medial subluxation or dislocation, persistent anterolateral knee pain, or apprehension.43 In addition, the site of MPFL insertion must be carefully considered.6
Because of tempered enthusiasm for the previously mentioned traditional procedures, a variety of MPFL reconstruction procedures have been proposed with promising short-term results.18 Although long-term data are currently lacking, this technique is advantageous in that it works toward preserving the original MPFL anatomy.63 In children aged 15 and 16 years, a semitendinosus tendon autograft was attached near the proximal medial collateral ligament attachment on the femur, as a proxy for the femoral MPFL insertion site. After a mean follow-up time of 7.4 years, Kujala scores were higher than 89 with no recurrent dislocations.30
Controversy regarding the proper attachment site of the MPFL insertion relative to the open physis has confounded selection of the optimal technique, as incorrect positioning can result in postsurgical complications in both skeletally mature and immature patients.
While any of this array of procedures may provide adequate short-term stabilization of the patellofemoral joint, the long-term sequelae of these interventions in young, growing patients has not been elucidated. Cadaveric studies have shown that even minimal proximal malpositioning of grafts on the femoral MPFL insertion site can alter contact forces between the medial patellar facet and trochlea, potentially predisposing patients to early onset osteoarthritis.34 Overtightening of grafts >10 N in cadaveric knees contributes to increased medial patellar facet loading.14 A clinical series of complications associated with graft malpositioning during MPFL reconstruction, some of which are described in skeletally immature patients, has been reported.21,94 While not specifically focused on the outcomes in skeletally immature patients, a systematic review highlighted the high rate (26%) of complications associated with MPFL reconstruction, which include patellar fracture, postoperative instability, flexion loss, and pain.87 Reconstruction of the MQTFL has been proposed as an alternative intervention to MPFL reconstruction that avoids the risk of patellar fracture while still providing an additional restraint to lateralization of the patella. In this approach, Fulkerson and Edgar39 describe use of either a semitendinosus autograft or posterior tibial tendon allograft to reconstruct the MQTFL through femoral attachment to the anterior adductor tubercle and central attachment to the distal quad tendon, thereby precluding the need for patellar drilling.
Conclusion
Conservative measures represent the gold standard of treatment for first-time dislocators. Evidence suggests that the majority of skeletally immature patients who have a patellar dislocation will go on to develop recurrent or chronic instability. Surgical techniques for recurrent patellar instability in children require specialized understanding of principles unique to the skeletally immature athlete.
Acknowledgments
The authors thank Kyna Donohue for her assistance in paper formatting and submission.
Footnotes
The authors report the following potential conflicts of interest: Sariah Khormaee, MD, PhD, was supported by National Institute of Neurological Disorders and Stroke, National Institutes of Health (5F30NS06468).
References
- 1. Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37:2021-2027. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS, McCarthy M, Gomez JA, Shubin Stein BE. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med. 2009;37:791-796. [DOI] [PubMed] [Google Scholar]
- 3. Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc. 2007;15:48-56. [DOI] [PubMed] [Google Scholar]
- 4. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215-220. [DOI] [PubMed] [Google Scholar]
- 5. Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop. 2011;35:1483-1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499-519. [DOI] [PubMed] [Google Scholar]
- 7. Arnbjörnsson A, Egund N, Rydling O, Stockerup R, Ryd L. The natural history of recurrent dislocation of the patella. Long-term results of conservative and operative treatment. J Bone Joint Surg Br. 1992;74:140-142. [DOI] [PubMed] [Google Scholar]
- 8. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472-479. [DOI] [PubMed] [Google Scholar]
- 9. Balcarek P, Jung K, Ammon J, et al. Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle–trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med. 2010;38:2320-2327. [DOI] [PubMed] [Google Scholar]
- 10. Balcarek P, Jung K, Frosch K-H, Stürmer KM. Value of the tibial tuberosity–trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39:1756-1761. [DOI] [PubMed] [Google Scholar]
- 11. Barnett AJ, Gardner ROE, Lankester BJA, Wakeley CJ, Eldridge JDJ. Magnetic resonance imaging of the patella: a comparison of the morphology of the patella in normal and dysplastic knees. J Bone Joint Surg Br. 2007;89:761-765. [DOI] [PubMed] [Google Scholar]
- 12. Bassett FH. Acute dislocation of the patella, osteochondral fractures, and injuries to the extensor mechanism of the knee. Amer Acad Orth Surg Instr Course Lect. 1976;(25):40-49. [Google Scholar]
- 13. Bathen M, Bastrom TP, Edmonds EW. Normal parameters of skeletally immature knees: developmental changes on magnetic resonance imaging. Orthop J Sports Med. 2013;1(4 suppl). 10.1177/2325967113S00040. [DOI] [PubMed] [Google Scholar]
- 14. Beck P, Brown NAT, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557-1563. [DOI] [PubMed] [Google Scholar]
- 15. Bedi H, Marzo J. The biomechanics of medial patellofemoral ligament repair followed by lateral retinacular release. Am J Sports Med. 2010;38:1462-1467. [DOI] [PubMed] [Google Scholar]
- 16. Benoit B, Laflamme GY, Laflamme GH, Rouleau D, Delisle J, Morin B. Long-term outcome of surgically-treated habitual patellar dislocation in children with coexistent patella alta. Minimum follow-up of 11 years. J Bone Joint Surg Br. 2007;89:1172-1177. [DOI] [PubMed] [Google Scholar]
- 17. Berg EE, Mason SL, Lucas MJ. Patellar height ratios. A comparison of four measurement methods. Am J Sports Med. 1996;24:218-221. [DOI] [PubMed] [Google Scholar]
- 18. Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35:484-492. [DOI] [PubMed] [Google Scholar]
- 19. Biedert R, Sigg A, Gal I, Gerber H. 3D representation of the surface topography of normal and dysplastic trochlea using MRI. Knee. 2011;18:340-346. [DOI] [PubMed] [Google Scholar]
- 20. Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241-242. [DOI] [PubMed] [Google Scholar]
- 21. Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27:1153-1159. [DOI] [PubMed] [Google Scholar]
- 22. Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010;38:181-188. [DOI] [PubMed] [Google Scholar]
- 23. Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38:2248-2254. [DOI] [PubMed] [Google Scholar]
- 24. Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports Med. 1988;16:244-249. [DOI] [PubMed] [Google Scholar]
- 25. Chotel F, Knorr G, Simian E, Dubrana F, Versier G. Knee osteochondral fractures in skeletally immature patients: French multicenter study. Orthop Traumatol Surg Res. 2011;97(suppl):S154-S159. [DOI] [PubMed] [Google Scholar]
- 26. Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24:881-887. [DOI] [PubMed] [Google Scholar]
- 27. Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90:2751-2762. [DOI] [PubMed] [Google Scholar]
- 28. Cooney AD, Kazi Z, Caplan N, Newby M, St Clair Gibson A, Kader DF. The relationship between quadriceps angle and tibial tuberosity-trochlear groove distance in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20:2399-2404. [DOI] [PubMed] [Google Scholar]
- 29. Crosby EB, Insall J. Recurrent dislocation of the patella. Relation of treatment to osteoarthritis. J Bone Joint Surg Am. 1976;58:9-13. [PubMed] [Google Scholar]
- 30. Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85:887-890. [PubMed] [Google Scholar]
- 31. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. [DOI] [PubMed] [Google Scholar]
- 32. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59-65. [DOI] [PubMed] [Google Scholar]
- 33. Earhart C, Patel DB, White EA, Gottsegen CJ, Forrester DM, Matcuk GR., Jr Transient lateral patellar dislocation: review of imaging findings, patellofemoral anatomy, and treatment options. Emerg Radiol. 2013;20:11-23. [DOI] [PubMed] [Google Scholar]
- 34. Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34:1478-1485. [DOI] [PubMed] [Google Scholar]
- 35. Farahmand F, Senavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res. 1998;16:136-143. [DOI] [PubMed] [Google Scholar]
- 36. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114-1121. [DOI] [PubMed] [Google Scholar]
- 37. Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schottle PB. The patella morphology in trochlear dysplasia—a comparative MRI study. Knee. 2006;13:145-150. [DOI] [PubMed] [Google Scholar]
- 38. Fujino K, Tajima G, Yan J, et al. Morphology of the femoral insertion site of the medial patellofemoral ligament [published online ahead of print December 3, 2013]. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-013-2797-0. [DOI] [PubMed] [Google Scholar]
- 39. Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;2:e125-e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS. Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop. 2012;32:621-625. [DOI] [PubMed] [Google Scholar]
- 41. Hing CB, Smith TO, Donell S, Song F. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2011;(11):CD008106. [DOI] [PubMed] [Google Scholar]
- 42. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38:1997-2004. [DOI] [PubMed] [Google Scholar]
- 43. Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383-388. [DOI] [PubMed] [Google Scholar]
- 44. Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67-69. [DOI] [PubMed] [Google Scholar]
- 45. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101-104. [DOI] [PubMed] [Google Scholar]
- 46. Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1511-1516. [DOI] [PubMed] [Google Scholar]
- 47. Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444-1449. [DOI] [PubMed] [Google Scholar]
- 48. Koëter S, Pakvis D, van Loon CJM, van Kampen A. Trochlear osteotomy for patellar instability: satisfactory minimum 2-year results in patients with dysplasia of the trochlea. Knee Surg Sports Traumatol Arthrosc. 2007;15:228-232. [DOI] [PubMed] [Google Scholar]
- 49. Kraus T, Švehlík M, Singer G, Schalamon J, Zwick E, Linhart W. The epidemiology of knee injuries in children and adolescents. Arch Orthop Trauma Surg. 2012;132:773-779. [DOI] [PubMed] [Google Scholar]
- 50. Larsen E, Lauridsen F. Results of conservative treatment of patellar dislocations. Acta Orthop Belg. 1982;48:455-462. [PubMed] [Google Scholar]
- 51. Lattermann C, Toth J, Bach BR., Jr. The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc. 2007;15:57-60. [DOI] [PubMed] [Google Scholar]
- 52. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41:575-581. [DOI] [PubMed] [Google Scholar]
- 53. Lippacher S, Dejour D, Elsharkawi M, et al. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40:837-843. [DOI] [PubMed] [Google Scholar]
- 54. Ma L, Wang C, Chen B, et al. Medial patellar retinaculum plasty versus medial capsule reefing for patellar dislocation in children and adolescents. Arch Orthop Trauma Surg. 2012;132:1773-1780. [DOI] [PubMed] [Google Scholar]
- 55. Mäenpää H, Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25:213-217. [DOI] [PubMed] [Google Scholar]
- 56. Marsh JS, Daigneault JP, Sethi P, Polzhofer GK. Treatment of recurrent patellar instability with a modification of the Roux-Goldthwait technique. J Pediatr Orthop. 2006;26:461-465. [DOI] [PubMed] [Google Scholar]
- 57. McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc. 2007;15:95-104. [DOI] [PubMed] [Google Scholar]
- 58. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396. [PubMed] [Google Scholar]
- 59. Miller GF. Familial recurrent dislocation of the patella. J Bone Joint Surg Br. 1978;60-B:203-204. [DOI] [PubMed] [Google Scholar]
- 60. Mochizuki T, Nimura A, Tateishi T, Yamaguchi K, Muneta T, Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21:305-310. [DOI] [PubMed] [Google Scholar]
- 61. Nakamura N, Horibe S, Iwahashi T, Kawano K, Shino K, Yoshikawa H. Healing of a chondral fragment of the knee in an adolescent after internal fixation. A case report. J Bone Joint Surg Am. 2004;86-A:2741-2746. [DOI] [PubMed] [Google Scholar]
- 62. Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19:2067-2071. [DOI] [PubMed] [Google Scholar]
- 63. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41:58-63. [DOI] [PubMed] [Google Scholar]
- 64. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513-515. [DOI] [PubMed] [Google Scholar]
- 65. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76:699-704. [DOI] [PubMed] [Google Scholar]
- 66. Nikku R, Nietosvaara Y, Kallio PE, Aalto K, Michelsson JE. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand. 1997;68:419-423. [DOI] [PubMed] [Google Scholar]
- 67. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139-143. [DOI] [PubMed] [Google Scholar]
- 68. Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35:1851-1858. [DOI] [PubMed] [Google Scholar]
- 69. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19:717-721. [DOI] [PubMed] [Google Scholar]
- 70. Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994;22:680-686. [DOI] [PubMed] [Google Scholar]
- 71. Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37:1814-1820. [DOI] [PubMed] [Google Scholar]
- 72. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463-470. [DOI] [PubMed] [Google Scholar]
- 73. Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop. 2011;35:1799-1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19:663-670. [DOI] [PubMed] [Google Scholar]
- 75. Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133:209-213. [DOI] [PubMed] [Google Scholar]
- 76. Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858-864. [DOI] [PubMed] [Google Scholar]
- 77. Post WR, Teitge R, Amis A. Patellofemoral malalignment: looking beyond the viewbox. Clin Sports Med. 2002;21:521-546. [DOI] [PubMed] [Google Scholar]
- 78. Rebolledo BJ, Nam D, Cross MB, Green DW, Sculco TP. Familial association of femoral trochlear dysplasia with recurrent bilateral patellar dislocation. Orthopedics. 2012;35:e574-e579. [DOI] [PubMed] [Google Scholar]
- 79. Reider B, Marshall JL, Koslin B, Ring B, Girgis FG. The anterior aspect of the knee joint. J Bone Joint Surg Am. 1981;63:351-356. [PubMed] [Google Scholar]
- 80. Reider B, Marshall JL, Warren RF. Clinical characteristics of patellar disorders in young athletes. Am J Sports Med. 1981;9:270-274. [DOI] [PubMed] [Google Scholar]
- 81. Rémy F, Chantelot C, Fontaine C, Demondion X, Migaud H, Gougeon F. Inter- and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia. Surg Radiol Anat. 1998;20:285-289. [DOI] [PubMed] [Google Scholar]
- 82. Rorabeck CH, Bobechko WP. Acute dislocation of the patella with osteochondral fracture: a review of eighteen cases. J Bone Joint Surg Br. 1976;58:237-240. [DOI] [PubMed] [Google Scholar]
- 83. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52-60. [DOI] [PubMed] [Google Scholar]
- 84. Seeley M, Bowman KF, Walsh C, Sabb BJ, Vanderhave KL. Magnetic resonance imaging of acute patellar dislocation in children: patterns of injury and risk factors for recurrence. J Pediatr Orthop. 2012;32:145-155. [DOI] [PubMed] [Google Scholar]
- 85. Seil R, Müller B, Georg T, Kohn D, Rupp S. Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc. 2000;8:231-236. [DOI] [PubMed] [Google Scholar]
- 86. Senavongse W, Amis AA. The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Joint Surg Br. 2005;87:577-582. [DOI] [PubMed] [Google Scholar]
- 87. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthroscopy. 2010;26:1083-1087. [DOI] [PubMed] [Google Scholar]
- 89. Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am. 2009;91:263-273. [DOI] [PubMed] [Google Scholar]
- 90. Smith TO, Davies L, O’Driscoll M-L, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15:255-262. [DOI] [PubMed] [Google Scholar]
- 91. Smith TO, Donell ST, Chester R, Clark A, Stephenson R. What activities do patients with patellar instability perceive makes their patella unstable? Knee. 2011;18:333-339. [DOI] [PubMed] [Google Scholar]
- 92. Smith TO, McNamara I, Donell ST. The contemporary management of anterior knee pain and patellofemoral instability. Knee. 2013;20(suppl 1):S3-S15. [DOI] [PubMed] [Google Scholar]
- 93. Smith TO, Song F, Donell ST, Hing CB. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:988-998. [DOI] [PubMed] [Google Scholar]
- 94. Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ. Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e87. [DOI] [PubMed] [Google Scholar]
- 95. Teitge RA, Torga Spak R. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20:998-1002. [DOI] [PubMed] [Google Scholar]
- 96. Uchida R, Toritsuka Y, Yoneda K, Hamada M, Ohzono K, Horibe S. Chondral fragment of the lateral femoral trochlea of the knee in adolescents. Knee. 2012;19:719-723. [DOI] [PubMed] [Google Scholar]
- 97. Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G. Treating patella instability in skeletally immature patients. Arthroscopy. 2013;29:1410-1422. [DOI] [PubMed] [Google Scholar]
- 98. Walker P, Harris I, Leicester A. Patellar tendon-to-patella ratio in children. J Pediatr Orthop. 1998;18:129-131. [PubMed] [Google Scholar]
- 99. Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am. 2007;89:1749-1755. [DOI] [PubMed] [Google Scholar]
- 100. Waterman BR, Belmont PJ, Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25:51-57. [DOI] [PubMed] [Google Scholar]
- 101. Wibeeg G. Roentgenographs and anatomic studies on the femoropatellar joint: with special reference to chondromalacia patellae. Acta Orthopaedica. 1941;12:319-410. [Google Scholar]