Abstract
Context:
Current literature has clearly shown that the indications for surgical treatment of clavicle fractures in adults are expanding. Although clavicle fractures in children and adolescents have traditionally been treated nonoperatively, surgical treatment of displaced clavicle fractures may be indicated for adolescent athletes.
Evidence Acquisition:
A review of relevant articles published between 1970 and 2013 was completed using MEDLINE and the terms clavicle fracture and adolescent athlete.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
Excellent outcomes and rapid return to competition can be achieved with surgical management of displaced clavicle fractures in the adolescent athlete with high functional demands similar to those of their adult counterparts. Complications include hardware irritation, screw loosening, pin migration, peri-incisional numbness, and refracture. Athletes and families must be counseled regarding complications and potential need for secondary surgery to remove hardware.
Conclusion:
The adolescent athlete with a displaced, shortened, or comminuted clavicle fracture presents a unique, controversial dilemma for the surgeon. Earlier return to competition can be achieved with surgical management to restore length and alignment and may prevent malunion, nonunion, and poor outcomes.
Keywords: clavicle fracture, adolescent athlete, displaced midshaft clavicle fracture
Nearly 45 million children and adolescents participate in organized sports in the United States. With the increase in athletic competition, along with the demands placed on participants in organized sports, a rise in sports injuries has also been observed.7 The clavicle is the most commonly fractured bone in both adults and children,1,4,11,13 accounting for 5% to 15% of all fractures and 35% to 44% of those in the shoulder region.22,28-30 Approximately 85% of pediatric clavicle fractures result from sports or recreational activities,31 and they are among the most common fractures in adolescents.28
As children transition into adolescence, their activity levels and competitive expectations can be greater than those of adults. Therefore, a potential role for surgical treatment of clavicle fractures in highly functional adolescent athletes to improve time to return to sport and functional outcomes may exist. Few articles have evaluated adolescent clavicle fractures treated with surgical fixation, with the majority being retrospective review studies.1,6,10,13,18,21,34,35 Even fewer studies have specifically investigated outcomes of surgical versus nonsurgical management of clavicle fractures in adolescents.35
The purpose of our literature review was to examine surgical indications, union rate, method of fixation, time to union, return to sport, and complications of surgical treatment of clavicle fractures in the adolescent athlete.
Adolescent Clavicle Fracture Anatomic Considerations
Most clavicle fractures occur in the middle third, or midshaft, because of a fall directly onto the shoulder or a direct blow to the clavicle (Figure 1).29 In the adolescent clavicle, growth and remodeling may resemble that of an adult more than that of a young child because most clavicle length is reached at a relatively early age.1,6,16,18,35 Eighty percent of the clavicle’s growth is complete by age 9 years in girls and by age 12 years in boys, which may have implications for remodeling potential in adolescents.5 Furthermore, when comparing clinical relevance of shortening between adults and adolescents, consider interindividual variation in total clavicle length. Two centimeters of shortening in a 10-cm skeletally immature clavicle will result in a relative shortening of 20%, whereas 2 cm of shortening in a 17-cm adult clavicle will result in relative shortening of 12%.33 Therefore, the clinical impact of absolute shortening in adult studies may have an equal or even greater impact on the adolescent total clavicle length and relative shortening. Because of low repeatability and variability in clavicle length and shortening with measurements based on plain radiographs,32 using 3-dimensional computed tomography scans to evaluate length, shortening, and comminution of clavicle fractures may be indicated.10,26
Figure 1.

Anteroposterior radiograph showing a middle third diaphyseal clavicle fracture in a 14-year-old boy.
Nonsurgical Versus Surgical Management
Nonsurgical management with a sling or figure-of-8 immobilization is appropriate for nearly all clavicle fractures in children because of their excellent healing and remodeling capabilities.22,26,29 In the 1960s, Neer22 and Rowe29 reported higher nonunion rates with operatively treated fractures than with nonoperative treatment, making closed treatment of clavicle fractures widely accepted as the standard of care.
Although few studies have focused on the management of adolescents, several have included adolescents in their patient populations,2,8,17,19,24,36 leading surgeons to question the utility of operative treatment in younger age groups. A survey of 302 members of the Pediatric Orthopedic Society of North America (POSNA) determined that >90% of members favored nonoperative treatment of nondisplaced clavicle fractures.3 However, nearly half of all respondents favored surgical treatment of teenagers (age 16-19 years) with segmental fracture patterns. Fifty percent of members indicated that they were more likely to choose surgical treatment for an elite overhead-throwing adolescent athlete with a completely displaced clavicle fracture.
Several studies have compared surgical and nonsurgical treatment of clavicle fractures in adult athletes, with significant advantages shown in postoperative strength,37 outcome scores,12,19,36 quicker time to return to competition,12,19,20,27,36 and lower refracture rates with surgical treatment.20 Although mild decreases in shoulder function may be readily tolerated, an early return to activity with unimpaired function is of great importance for athletes, with time lost due to injury resulting in missed practices and competition at both the amateur and professional levels.12,19
Studies of adults with clavicle fractures have reported inferior outcomes with nonsurgical treatment than with surgical treatment.9,17,24,25 McKee et al17 demonstrated decreased strength in the injured arm with nonsurgical treatment. Abduction strength was 67% of that of the contralateral arm. Weakness in abduction strength may be most notable in highly active adolescent overhead throwing athletes who rely on extremes of motion and strength. These negative effects may be long lasting: A 10-year follow-up study reported that 46% of nonoperatively treated patients did not consider themselves fully recovered, with 29% having pain during activity and 9% having pain at rest.25
Indications for Surgical Management of Fractures
Absolute indications for surgical treatment of clavicle fractures in both adults and adolescents are open fractures, severe angulation, or displacement causing potential risk for skin perforation, neurovascular compromise, and symptomatic nonunion (Figure 2).4,13,26,30,38 Relative indications for surgery include fracture shortening >1.5 to 2 cm, or 14% to 15% of the contralateral side, polytrauma, floating shoulder, significant seizure or neuromuscular disorder, Neer Type II displaced distal-third fractures, and unsightly cosmetic appearance due to displacement.26,30,38
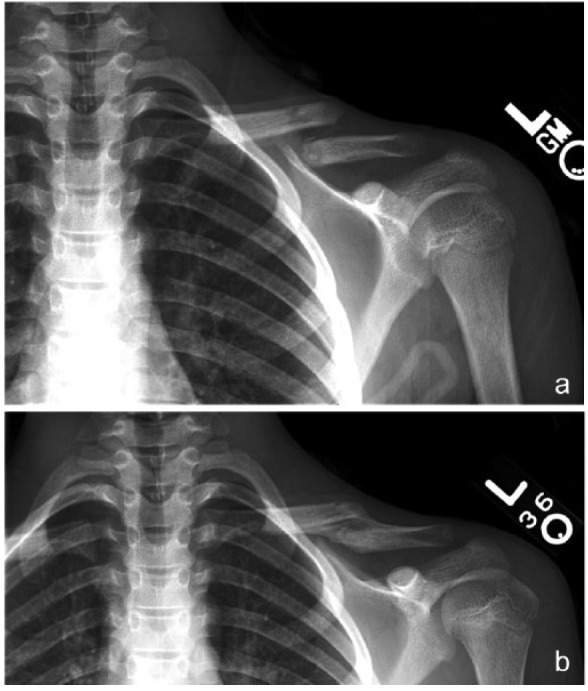
Figure 2.

Middle third diaphyseal clavicle fracture with skin tenting and potential compromise in a 15-year-old girl. (a) Anteroposterior radiograph shows a middle third diaphyseal clavicle fracture with severe displacement. (b) Anteroposterior radiograph at 12 weeks after surgery shows a successful anatomic restoration and radiographic union.
In a recent review of adolescent clavicle fractures, Pandya et al26 reported that adolescents with clavicle fractures that are completely displaced (no cortical contact), comminuted, or present with a transverse Z-shaped fragment should undergo surgical fixation (Figure 3). Relative shortening by itself is insufficient to warrant surgical treatment and must be accompanied by comminution, marked displacement, or skin tenting. The Z-variant was the most common in 57.9% of adolescents studied by Hosalkar et al10 and in 41% by Vander Have et al.35
Figure 3.

Middle third comminuted diaphyseal clavicle fracture in a 16-year-old male patient. (a) Anteroposterior radiograph shows a middle third diaphyseal clavicle fracture with comminution and a Z-shaped fragment. (b) Anteroposterior radiograph at 10 weeks after surgery shows a successful anatomic restoration and radiographic union.
Nonunion and Malunion with Nonsurgical Treatment
Although nonunion of adolescent clavicle fractures is rare,23 malunion is more common given limited remaining growth for potential remodeling (Figure 4). With nonsurgical treatment, maintenance of closed reduction until bony consolidation is nearly impossible. Therefore malunion, whether symptomatic or asymptomatic, is nearly inevitable.9,17,33 Adolescents with >2 cm of shortening were more likely to develop symptomatic malunion with nonsurgical treatment, with 4 of 5 patients electing to have a corrective osteotomy.35 Their symptoms were pain with prolonged overhead activity, easy fatigability, axillary pain, and drooping shoulder with painful bony prominence. All 4 patients returned to activities at a mean 12 weeks after surgery. Similarly, symptomatic malunion has been reported in 18% of nonsurgically treated adult patients.2
Figure 4.
Middle third diaphyseal clavicle fracture malunion in a 10-year-old boy. (a) Anteroposterior radiograph shows a middle third diaphyseal clavicle fracture with complete displacement and extensive shortening. (b) Anteroposterior radiograph 15 weeks later shows radiographic malunion.
In a cadaveric study, Matsumura et al15 associated clavicular shortening with decreased scapular external rotation and posterior tilting during elevation. Similarly, in a retrospective review of clavicle malunions with >1.5 cm shortening evaluated with 3-dimensional reconstructive computed tomography scanning, investigators found increased sternoclavicular joint angulation and alteration of scapulothoracic relationships.14 Peak shoulder abduction velocity and weakness in shoulder external rotation, adduction, and internal rotation were also significantly reduced in the injured arm.
Surgical Treatment and Outcomes
Kubiak and Slongo13 retrospectively reviewed 15 surgically treated clavicle fractures in children aged 9 to 15 years: 8 had midshaft fractures, 2 medial fractures, and 5 lateral fractures. The most common indication for surgery was displacement and interposition of soft tissue. There were no reports of infection, instability, or poor functional results. All patients recovered complete range of motion at last follow-up.
Mehlman et al18 evaluated clinical and radiographic results of surgical fixation of completely displaced clavicle shaft fractures in 24 patients younger than 16 years (mean, 12.7 years; range, 7-16 years). Twenty-two patients were treated with plate and screw fixation. At an average follow-up of 16 months, all parents were satisfied with their child’s treatment, and 21 of 24 (87%) patients returned to unrestricted sports activities. There were 3 complications: transverse ulnar nerve symptom of 3 months duration, scar sensitivity, and mildly painful scar.
Comparison Groups of Nonoperatively Treated Patients
Namdari et al21 reported on 14 patients (mean age, 12.9 years; range, 10-15 years) with displaced midshaft clavicle fractures treated with plate fixation. Twelve were originally treated nonoperatively but underwent surgery because of increased displacement at 3 weeks. Average follow-up was 37.9 months, and mean postoperative QuickDASH (Disabilities of the Arm, Shoulder, and Hand) scores were 7 (range, 0-37.5), with an average score for DASH sport modalities of 1.1. Similarly, Hosalkar et al10 found excellent outcomes of surgically treated clavicle fractures in 19 adolescent patients. Finally, Vander Have et al35 compared outcomes in surgical (n = 17) and nonsurgical (n = 25) treatment groups in 42 consecutive adolescent patients with 43 closed midshaft clavicle fractures (mean age, 15.4 years; range, 12-17 years). The mean time to union was 9.9 weeks (range, 6-16 weeks) in the nonoperative group versus 7.5 weeks (range, 6-10 weeks) in the operative group. There were no significant intraoperative or postoperative complications. Symptomatic malunion, with a mean fracture shortening of 26 mm, developed in 5 patients in the nonoperative group. There were no nonunions in either group.
Return to Sport
Surgical treatment of clavicle fractures in adult athletes have reported faster return to sport,12,19,20,27,36 improved strength,37 and higher satisfaction scores.12,19,36 Jubel et al12 evaluated intramedullary surgical treatment for mid-third clavicle fractures in 12 top-performance athletes; 6 were adolescents. They resumed training an average of 5.9 days after surgery and returned to competition at an average of 16.8 days.
Complications of Surgical Treatment
The surgical treatment of adolescent clavicle fractures has associated risks and potential complications seen with adult clavicle fractures: infection (0%-18%), nonunion (2%-15%), neurovascular injury (0%-5%), adhesive capsulitis (0%-7%), refracture after hardware removal (0%-8%), and symptomatic hardware (50%-100%) (Figure 5).11,35 Paresthesia over surgical site, unsatisfactory appearance of scar, pseudobursae, skin perforation from hardware, and refracture have been reported in younger patients by Kubiak and Slongo.13
Figure 5.

Middle third diaphyseal clavicle fracture requiring hardware removal in a 17-year-old male patient. (a) Anteroposterior radiograph shows a middle third diaphyseal clavicle fracture with complete displacement and shortening. (b) Anteroposterior radiograph at 12 weeks after surgery shows radiographic union and prominent lateral hardware requiring removal.
Hardware removal because of irritation is the most common secondary surgical procedure after surgical treatment of clavicle fractures; 41% of adolescents complained of irritation from pin prominence that was relieved with hardware removal.6 Three patients (17.6%) treated with plate fixation elected hardware removal because of local prominence.35
Conclusion
The adolescent athlete with a displaced, shortened, or comminuted clavicle fracture presents a unique, controversial dilemma for the treating surgeon, the athlete, and the patient’s family. The athlete’s age, years of growth remaining, potential for remodeling, and level of functional demand of sporting activities should be considered when evaluating the adolescent patient for appropriate treatment modalities. Excellent outcomes and earlier return to competition can be achieved with surgical management of displaced adolescent athlete clavicle fractures (Figure 6). However, patients and families must be counseled regarding the known complications.
Figure 6.

Surgical management of a clavicle fracture in a 16-year-old male patient. (a) Anteroposterior radiograph demonstrating a middle third diaphyseal clavicle fracture with complete displacement and extensive shortening. (b) Anteroposterior radiograph 5 months after surgery shows successful anatomic restoration and radiographic union.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Caird MS. Clavicle shaft fractures: are children little adults? J Pediatr Orthop. 2012;32(suppl 1):S1-S4. [DOI] [PubMed] [Google Scholar]
- 2. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg. 2007;89:1-10. [DOI] [PubMed] [Google Scholar]
- 3. Carry PM, Koonce R, Pan Z, Polousky JD. A survey of physician opinion: adolescent midshaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop. 2011;31:44-49. [DOI] [PubMed] [Google Scholar]
- 4. Curtis RJ. Operative management of children’s fractures of the shoulder region. Orthop Clin North Am. 1990;21:315-324. [PubMed] [Google Scholar]
- 5. Dameron TB, Rockwood CA. Fractures and dislocations of the shoulder. In: Rockwood CA, Wilkins KE, King RE, eds. Fractures in Children. Philadelphia, PA: JB Lippincott; 1984:624-676. [Google Scholar]
- 6. Frye BM, Sheila R, McDonough EB, Bal GK. Operative treatment of adolescent clavicle fractures with an intramedullary clavicle pin. J Pediatr Orthop. 2012;32:334-339. [DOI] [PubMed] [Google Scholar]
- 7. Goldberg AS, Moroz L, Smith A, Ganley T. Injury surveillance in young athletes: a clinician’s guide to sports injury literature. Sports Med. 2007;37:265-278. [DOI] [PubMed] [Google Scholar]
- 8. Grassi FA, Tajana MS, D’Angelo F. Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma. 2001;50:1096-1100. [DOI] [PubMed] [Google Scholar]
- 9. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537-539. [DOI] [PubMed] [Google Scholar]
- 10. Hosalkar HS, Parikh G, Bomar JD, Bittersohl B. Open reduction and internal fixation of displaced clavicle fractures in adolescents. Orthop Rev (Pavia). 2012;4:e1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11. Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007;15:239-248. [DOI] [PubMed] [Google Scholar]
- 12. Jubel A, Andermahr J, Bergmann H, Prokop A, Rehm KE. Elastic stable intramedullary nailing of midclavicular fractures in athletes. Br J Sports Med. 2003;37:480-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kubiak R, Slongo T. Operative treatment of clavicle fractures in children: a review of 21 years. J Pediatr Orthop. 2002;22:736-739. [PubMed] [Google Scholar]
- 14. Ledger M, Leeks N, Ackland T, Wang A. Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg. 2005;14:349-354. [DOI] [PubMed] [Google Scholar]
- 15. Matsumura N, Ikegami H, Nakamichi N, Nakamura T, Nagura T, Imanishi N. Effect of shortening deformity of the clavicle on scapular kinematics. Am J Sports Med. 2010;38:1000-1006. [DOI] [PubMed] [Google Scholar]
- 16. McGraw MA, Mehlman CT, Lindsell CJ. Postnatal growth of the clavicle: birth to 18 years of age. J Pediatr Orthop. 2009;29:937-943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88:35-40. [DOI] [PubMed] [Google Scholar]
- 18. Mehlman CT, Yihua G, Boachanf C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29:851-855. [DOI] [PubMed] [Google Scholar]
- 19. Meier C, Grueninger P, Platz A. Elastic stable intramedullary nailing for midclavicular fractures in athletes: indications, technical pitfalls and early results. Acta Orthop Belg. 2006;72:269-275. [PubMed] [Google Scholar]
- 20. Morgan RJ, Bankston LS, Hoenig MP, Connor PM. Evolving management of middle-third clavicle fractures in the National Football League. Am J Sports Med. 2010;38:2092-2096. [DOI] [PubMed] [Google Scholar]
- 21. Namdari S, Ganley TJ, Baldwin K, et al. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop. 2011;31:507-511. [DOI] [PubMed] [Google Scholar]
- 22. Neer CS., II Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006-1011. [DOI] [PubMed] [Google Scholar]
- 23. Nogi J, Heckman JD, Hakala M, Sweet DE. Non-union of the clavicle in a child: a case report. Clin Orthop Relat Res. 1975;(110):19-21. [DOI] [PubMed] [Google Scholar]
- 24. Nordqvist A, Peterson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end results study after conservative treatment. J Orthop Trauma. 1998;12:572-576. [DOI] [PubMed] [Google Scholar]
- 25. Nowak J, Holgersson M, Larsson S. Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J Shoulder Elbow Surg. 2004;13:479-486. [DOI] [PubMed] [Google Scholar]
- 26. Pandya NK, Namdari S, Hosalkar HS. Displaced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20:498-505. [DOI] [PubMed] [Google Scholar]
- 27. Rabe SB, Oliver GD. Clavicular fracture in a collegiate football player: a case report of rapid return to play. J Athl Train. 2011;46:107-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Robinson MC. Fractures of the clavicle in the adult. epidemiology and classification. J Bone Joint Surg Br. 1998;80:476-484. [DOI] [PubMed] [Google Scholar]
- 29. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29-42. [PubMed] [Google Scholar]
- 30. Sarwark JF, King EC, Luhmann SJ. Proximal humerus, scapula, and clavicle. In: Beaty JA, Kasser JR, eds. Rockwood and Wilkins’ Fractures in Children. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:704-771. [Google Scholar]
- 31. Shah RR, Kinder J, Peelman J, Moen T, Saarwark J. Pediatric clavicle and acromioclavicular Injuries. J Pediatr Orthop. 2010;30:S69-S72. [Google Scholar]
- 32. Silva SR, Fox J, Speers M, et al. Reliability of measurements of clavicle shaft fracture shortening in adolescents. J Pediatr Orthop. 2013;33:e19-e22. [DOI] [PubMed] [Google Scholar]
- 33. Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106-112. [DOI] [PubMed] [Google Scholar]
- 34. Taylor DC, Krasinski KL. Adolescent shoulder surgeries: consensus and controversies. J Bone Joint Surg Am. 2009;91:462-473. [PubMed] [Google Scholar]
- 35. Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30:307-312. [DOI] [PubMed] [Google Scholar]
- 36. Verborgt O, Pittoors K, Van Glabbeek F, Declercq G, Nuyts R, Somville J. Plate fixation of middle-third clavicle fractures in the semi-professional athlete. Acta Orthop Belg. 2005;71:17-21. [PubMed] [Google Scholar]
- 37. Witzel K. Intramedullary osteosynthesis in fractures of the mid-third of the clavicle in sports traumatology. Z Orthop Unfall. 2007;145:639-642. [DOI] [PubMed] [Google Scholar]
- 38. Zenni EJ, Jr, Krieg JK, Rosen MJ. Open reduction and internal fixation of clavicle fractures. J Bone Joint Surg. 1981;63:147-151. [PubMed] [Google Scholar]


