Abstract
Purpose/Objectives
To explore the feasibility of rural home telemonitoring for patients with lung cancer.
Design
Exploratory, descriptive, observational.
Setting
Patient homes within a 75-mile radius of the study hospital in West Virginia.
Sample
10 patients hospitalized with lung cancer as a primary or secondary-related diagnosis.
Methods
Data included referral and demographics, chart reviews, and clinical data collected using a HomMed telemonitor. Five patients received usual care after discharge; five had telemonitors set up at home for 14 days with daily phone calls for nurse coaching; mid- and end-study data were collected by phone and in homes through two months.
Main Research Variables
Enrollment and retention characteristics, physiologic (e.g., temperature, pulse, blood pressure, weight, O2 saturation) and 10 symptom datapoints, patient and family telemonitor satisfaction.
Findings
Of 45 referred patients, only 10 consented; 1 of 5 usual care and 3 of 5 monitored patients completed the entire study. Telemonitored data transmission was feasible in rural areas with high satisfaction; symptom data and physiologic data were inconsistent but characteristic of lung cancer.
Conclusions
Challenges included environment, culture, technology, and overall enrollment and retention. Physiologic and symptom changes were important data for nurse coaching on risks, symptom management, and clinician contact.
Implications for Nursing
Enrollment and retention in cancer research warrants additional study. Daily monitoring is feasible and important in risk assessment, but length of time to monitor signs and symptoms, which changed rapidly, is unclear. Symptom changes were useful as proxy indicators for physiologic changes, so risk outcomes may be assessable by phone for patient self-management coaching by nurses.
Keywords: care of the medically underserved, community health/home care, lung cancer, patient education, quality of life
Lung cancer is second only to heart disease as a cause of death for men and women in West Virginia (WV), and lung cancer death rates (90.5 per 100,000) in WV are higher than all cancer type death rates in the United States as a whole (WV Cancer Registry, 2012). Smoking, social inequality, and environmental exposure (e.g., coal mining), all of which are prominent factors in the WV population, contribute to lung cancer prevalence and higher mortality (Hendryx, O’Donnell, & Horn, 2008). Costs of care are high because of the expense of cancer treatments compounded by long-term oxygen therapy, repeated hospital stays, and emergency care visits. Providing even short-term, daily, out-of-hospital surveillance of patients with lung cancer at home could better standard care by improving patient reports of signs and symptoms to clinicians, thereby delaying or avoiding rehospitalization. However, the use of home telemonitoring devices for patients with lung cancer is not well documented and may not be feasible in rural, mountainous areas in WV.
Background
Telemonitoring in Chronically III Patients
Although ambiguous outcomes have been reported, often related to underpowered studies and dissimilar outcome measures, researchers and clinicians have found the use of home telemonitoring can be a key factor in cost-effective health care, as evidenced by studies dating back to 2001 (Dellifraine & Dansky, 2008). Examples of outcomes include a 50% reduction in admissions, with an 80% decrease in home visits for chronic obstructive pulmonary disease (COPD) (Cook, 2012) and improved patient responses such as better control of blood pressure management and increased activities of daily living (Finkelstein, Speedie, & Potthoff, 2006), and decreased healthcare visits and costs, including a 44% decrease in 30-day hospital readmissions of patients with heart failure (Anderson, 2012; Cook, 2012). However, telehealth research has focused primarily on chronic disease populations, particularly those with chronic heart failure (Giamouzis et al., 2012). Compared to patients with heart failure, unique challenges are associated with patients suffering from deteriorating disease symptoms and related post-treatment complications of lung cancer (e.g., acute exacerbations triggered by infections; symptom clusters such as pain and dyspnea signifying distress after surgery, chemotherapy, or radiotherapy) that affect functioning and outcomes (Fox & Lyon, 2006). Positive findings of improved knowledge of disease, treatment adherence, and medication management have been reported, as well as lower rehospitalization costs, all associated with using telemonitors in the care of patients with chronic lung disease. Hospitals in Spain documented an average cost savings of 810 Euros per patient (about $1,096 U.S. dollars), primarily from shorter hospital stays, fewer prescriptions, decreased home nursing visits, and less use of emergent care (Garcia-Aymerich et al., 2007; Paget, Jones, Davies, Evered, & Lewis, 2010; Puig-Junoy et al., 2007). Although telemonitoring alone has not clearly reduced rehospitalization or emergent care visits in areas with reliable access to healthcare services, remote monitoring that includes interaction with patients and nurses has helped reduce readmissions (Anderson, 2012; Chaudhry et al., 2010). Nevertheless, the overall benefits of using home telemonitoring to assist patients with lung disease currently are inconclusive because telehealth study outcomes have had wide confidence intervals and low power to detect significant differences (McLean et al., 2012). Determining the feasibility of telehealth monitoring and examining potential benefits of monitoring patients with lung disease living in rural areas such as Appalachian WV is necessary.
Lung Cancer and Telemonitoring in Appalachia
Incidence and mortality rates for lung cancer in WV exceed the national average, and cancer-related disparities are seen throughout the state’s 55 counties (WV Cancer Registry, 2012). Further compounding cancer burden are low screening rates (under- and uninsured); low literacy coupled with ineffective or inefficient communication (resulting in reduced access to screening and care); and geographic challenges, as the second-most rural state, in getting to and from place of residence to comparatively few and more distant points of healthcare delivery via noninterstate transportation (Borak, Salipante-Zaidel, Slade, & Fields, 2012). Those data support challenges in addressing cancer and research disparities in the Appalachian population in WV. In addition, the use of telehealth has not been investigated in patients with lung cancer living in these remote areas. To date, telemonitors have rarely been used in Appalachia, and no reported studies exist of community-dwelling adults with lung cancer. A pilot project funded by the National Institute of Health’s National Cancer Institute (NCI) included the current feasibility study of home telemonitoring among Appalachian patients with an intervention of nurse-coaching of patients to self-manage their lung cancer-related symptoms or treatment complications after hospital discharge. The mountainous remote locations of homes in WV were expected to present geographic obstacles to home telemonitoring that could prevent communication of the patient’s data from their home setting. It was not clear whether data obtained remotely would provide sufficient assessment to guide nurse-coaching and help patients understand their risk and potential actions.
Design and Goals
The focus in the current feasibility study was on the logistics needed to address the challenges of telemedicine and rural health research using distance technology and nurse-coaching by phone for patients with lung cancer who were being discharged from an academic health center hospital. The purpose of examining feasibility first was to better understand whether the telemonitor equipment itself would work and the nurse-coaching intervention would be acceptable, suitable, and usable by the study patients and their families living in rural areas.
The first feasibility goal was to explore patient enrollment and retention strategies to identify effective methods to inform rural patients about the study and keep them enrolled throughout a two-month period. The second goal of the feasibility study was to successfully transmit data from patients’ homes to the research nurses’ office computers via the telemonitor. The third goal was to examine the researchers’ ability to use the transmitted data to support patients in recognizing changes in their conditions and managing the changes or getting appropriate medical assistance. After a 14-day period of telemonitoring, the authors hypothesized that improved patient self-management skills, such as contact to a clinician or using prescribed medications for pain rather than using emergency care, could positively affect longer-term outcomes. Following proven feasibility, the NCI-funded pilot study would examine whether direct contacts between patients and clinicians for treatment and self-management would be less costly compared to emergency care or rehospitalization for two months. The feasibility study was, therefore, important in ensuring intervention fidelity prior to randomization in the pilot study and is the basis for this article.
Methods
The feasibility study used exploratory, descriptive, and observational methods to determine enrollment and retention issues in rural lung cancer research and the ability to do remote telemonitoring in Appalachia. The study also addressed telemonitor data sufficiency and applicability to a nurse-coaching intervention designed for Appalachian patients with lung cancer.
Participants and Setting
Patients were identified from an inpatient hospital list generated on a daily basis of all lung cancer admissions in West Virginia University’s Ruby Memorial Hospital in Morgantown. The inclusion criteria for patients were an admission primary diagnosis of lung cancer or lung cancer as a secondary diagnosis directly related to primary diagnoses such as COPD exacerbation, pleural effusion, or dyspnea; and expectation to be discharged to home. The project was reviewed and approved as a minimal-risk study by the institutional review board at West Virginia University. After staff nurses obtained the patient’s assent to be approached while in the hospital, eligible patients were told about the project by the research staff, and those interested signed the study’s informed consent form. Following consent, the 10 feasibility study participants’ vital signs, weight, oxygen saturation status, and symptom responses were assessed at the bedside using the telemonitoring equipment. All participants completed a series of surveys to assess their ability to perform activities of daily living, their pain, shortness of breath, mental status, and perception of their own health status (Time 1 data). Convenience sampling was used to divide the participants into two groups: (a) the first group of five patients received two home data collection visits from the clinical research nurses in addition to usual care after hospital discharge as a baseline comparison group; (b) the second group of five patients had a telemonitor placed in their homes for the first two weeks following hospital discharge in addition to usual care and the two data collection nurse visits. The study setting was the patient’s home.
Telemonitor and Protocol
Telemonitor
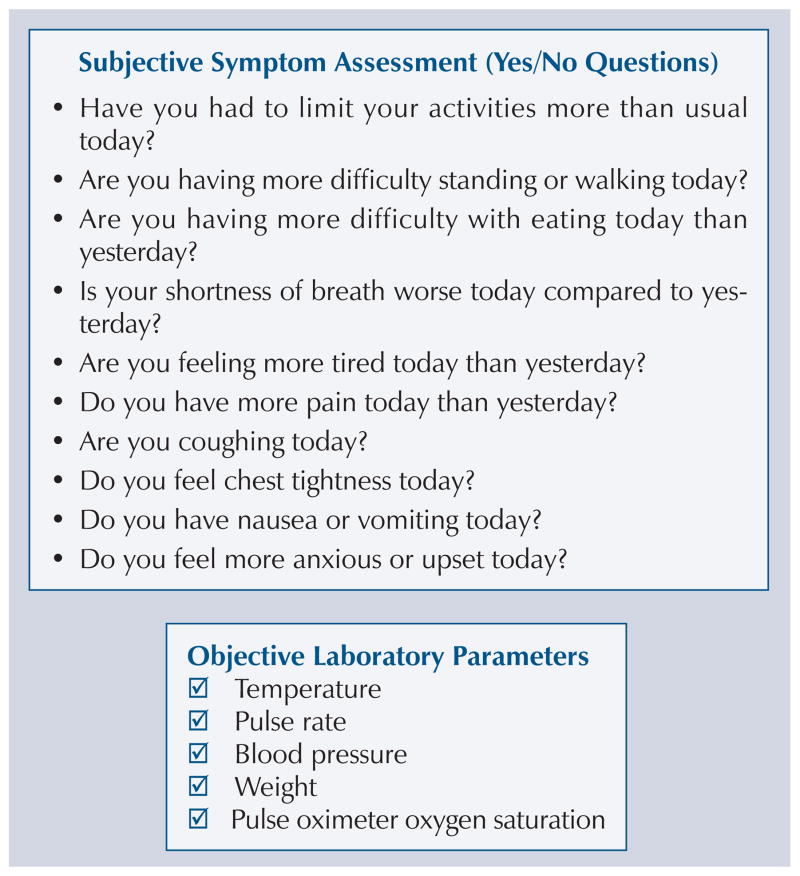
A contemporary telemonitor product—the Genesis DM, a U.S. Food and Drug Administration-approved, Class II, hospital-grade medical device was leased from Honeywell HomMed. Telemonitors were used to identify evidence of disease-related changes. The telemonitor device’s add-on peripherals and attachments for the current study included measurement modules for vital signs of pulse, blood pressure, and temperature; a weight scale; and an oxygen saturation sensor. The telemonitor was easy to use, with step-by-step directions provided in a friendly voice-talk or text-guided communication format; its simple manual operation used push-button data entry (YES/NO buttons) for patient responses to questions about symptom changes throughout the monitoring process. Symptom questions were selected from the telemonitor database on the basis of clinical observations of symptoms seen in patients with lung cancer using the short-form Pulmonary Functional Status Scale as a guide to changes that would indicate risk for decline in function (Chen, Narsavage, Culp, & Weaver, 2010). Figure 1 indicates the physiologic parameters and symptoms assessed via the telemonitors. The telemonitor data were electronically delivered to the central agency (the research office) using an electronic connection with a patient’s landline phone or an internal modem in the telemonitor, which could transmit without a phone line once the physiologic and symptom data were collected.
Figure 1.
Telemonitor Physiologic and Symptom Assessment Data Items
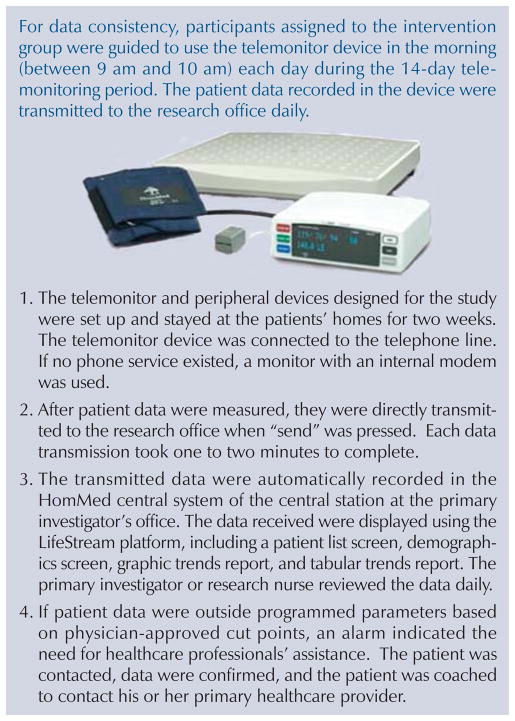
Intervention
The five patients constituting the intervention group were provided with the telemonitoring equipment within 48 hours of hospital discharge, instructed in its use, and asked to take their vital signs and answer symptom questions (e.g., “Is your pain worse today than yesterday? YES or NO”) using the telemonitor each day for 14 consecutive days. The clinical research nurse tested the telemonitoring equipment transmission at the time of home set-up by having the patient independently complete the data collection, send the data to the office, and then complete the same surveys as in the hospital (Time 2 data). The telemonitor transmitted data to the Honeywell LifeStream software program, which was accessible through the Internet from the research nurse’s office. For 14 days, a research nurse reviewed the vital signs within three hours of the transmission and placed a call to the patient to discuss the data. Vital signs outside the parameters established by the patient’s physician were discussed and the patient was guided to problem-solve through nurse-coaching (motivational interviewing), resulting in self-management or a call to their clinician. After 14 days, a research nurse visited the patient’s home to record the Time 3 study data, retrieve the telemonitoring equipment, and have the patient complete the study surveys in the nurse’s presence. In addition, telemonitored patients completed a survey that gauged their satisfaction with the telemonitoring equipment. If a family member assisted in the use of the equipment, he or she completed a similar survey on the level of satisfaction with the equipment. The home telemonitoring protocol is pictured in Figure 2.
Figure 2. Data Flow and Honeywell Telemonitoring System for Home Telemonitoring Intervention.
Note. Photo courtesy of Honeywell HomMed. Used with permission.
Usual care data collection protocol
Patients in the usual care group followed essentially the same protocol, except that they did not get the telemonitoring equipment in their homes and they did not receive daily telephone calls from the research nurse for 14 days. They were asked to complete surveys at the same time intervals (Time 1, Time 2, and Time 3) as the intervention group, with the exception of the satisfaction survey regarding telemonitoring.
Results
Feasibility Goal 1: Summary of Enrollment and Retention
The first goal was to examine the study’s patient enrollment and retention strategies to identify methods to inform patients about the study and keep them enrolled throughout the study period. It took three months to complete the feasibility study, during which the usual care (non-telemonitored) group and the intervention group enrolled five patients each from a total of 45 patients who had been referred. Three of those patients had been admitted to the hospital on two different occasions, so they were referred twice. Twenty patients were excluded because they did not meet the eligibility criteria—they were not discharged to home, were unable to complete questionnaires, lived outside a 75-mile radius of the study hospital, or did not have lung cancer as their primary or secondary diagnosis for their hospitalization. Five potentially eligible patients were discharged from the hospital prior to being informed about the study, 10 refused to participate, and 10 ultimately were enrolled in the feasibility study.
Patients who were not discharged to home included those going to rehabilitation facilities, nursing homes, or hospice care. Among those excluded for inability were patients who could not read, had hearing problems, mental status changes, or Glasgow Coma Scale scores less than 15 (fully awake on a scale ranging from 3–15; a score less than 15 indicates a physical or verbal impairment, making them ineligible for inclusion) who would not have been able to provide informed consent, answer the telephone, complete surveys, or use a monitor. The study was restricted to patients living within a 75-mile radius of the hospital so that nurses could realistically make home visits with relatively limited funding. Initially, patients without a landline were unable to participate, even with a General Packet Radio Service (GPRS) telemonitor, because data service coverage was not available where they lived. Ten patients refused for a variety of reasons, including lack of need, being too busy, or family or the patient being unwilling to participate in such a study.
Referrals of 18 patients took more than one month to attain the usual care group; 7 of the 18 did not meet the enrollment criteria because they were not discharged to home, did not have lung cancer as a primary or secondary discharge diagnosis, had altered mental status, or lived outside the 75-mile radius of the study’s academic hospital. Of the 11 qualified referrals, 4 were missed because they were discharged before they could be approached, 2 refused, and 5 consented. Four of the five patients in the usual care group did not complete the study. One was unable to participate because he did not have a telephone available at his rural home and a GPRS adaptor wireless data transmitter was not a component originally leased in the telemonitor contract, making transmission of Time 2 and Time 3 study data impossible after discharge. Three withdrew prior to the second data collection point because they did not want to complete the surveys, did not want to be part of the usual care group rather than the intervention, or were unresponsive after the first data collection.
The five telemonitored (intervention) participants were recruited from 27 patients who were referred during the second and third months. The primary investigator and clinical research nurses refined the consent process to include an introduction to the study with a study name card left for review and then, whenever possible, meeting the patient with a family member present to explain the study. The researchers were able to lease a telemonitor with a modem adapted to transmit from rural WV, so no additional patients were lost as a result of inability to transmit data. In the telemonitored group, three completed the study, one died, and another moved to a different state for additional lung cancer treatment. One did not complete the surveys at Time 3 when the research nurse visited his home to collect the equipment and finish the data collection at 14 days and also declined any subsequent home visit, but agreed that the surveys could be sent to him in the mail. The surveys were sent with a stamped preaddressed envelope in which to return them and he did return the completed surveys.
Table 1 compares the demographic characteristics and disease profile for the 10 enrolled patients. All were Caucasian, had a history of smoking (with one usual care patient still smoking), and had been hospitalized in the prior year, and four of the five patients in each group had been diagnosed more than a year prior to the study. Four usual care participants were considered to be overweight or obese based on their body mass index.
Table 1.
Demographic Characteristics and Disease Profile of Enrolled Patients (N = 10)
| Characteristic | Total
|
Usual Care (n = 5)
|
Telemonitored (n = 5)
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| X̄ | SD | Range | X̄ | SD | Range | X̄ | SD | Range | |
| Age (years) | 65.9 | 4.8 | 58–73 | 65.4 | 3.4 | 60–69 | 66.4 | 6.3 | 58–73 |
| Education (years) | 9.3 | 1.3 | 8–12 | 8.4 | 0.9 | 8–10 | 10.2 | 1.1 | 9–12 |
| Body mass index | 26 | 5.4 | 20.2–35.6 | 29.2 | 5.9 | 20.2–35.6 | 22.8 | 2 | 20.3–25.6 |
| Length of index hospital stay (days) | 4.3 | 2.4 | – | 2.8 | 1.1 | 2–4 | 5.8 | 2.5 | 2–8 |
| Charlson Comorbidity Index scorea | 8.1 | 3.4 | – | 9.6 | 3.8 | 5–15 | 6.6 | 2.3 | 3–9 |
| Characteristic | n | n | n |
|---|---|---|---|
| Gender | |||
| Male | 5 | 3 | 2 |
| Female | 5 | 2 | 3 |
| Education | |||
| Elementary school | 3 | 2 | 1 |
| High school | 3 | 1 | 2 |
| College or higher | 4 | 2 | 2 |
| Marital status | |||
| Not married | 6 | 3 | 3 |
| Married | 4 | 2 | 2 |
| Living situation | |||
| Living with family or relatives | 6 | 2 | 4 |
| Living alone | 4 | 3 | 1 |
| Smoking history | |||
| Past smoker | 9 | 4 | 5 |
| Active smoker | 1 | 1 | – |
| Household income ($) | |||
| Less than 50,000 | 7 | 4 | 3 |
| 50,000 or more | 3 | 1 | 2 |
| Payment coverage | |||
| Primary: Medicare | 8 | 4 | 4 |
| Primary: Commercial (Blue Cross/Blue Shield) | 2 | 1 | 1 |
| Secondary: Medicaid | 3 | 3 | – |
| Type of lung cancer | |||
| Non-small cell | 7 | 3 | 4 |
| Small cell | 3 | 2 | 1 |
| Cancer stage | |||
| I–IIIA | 2 | 2 | – |
| IIIB–IV extensive lesion | 7 | 3 | 4 |
| Small cell lung cancer in remission | 1 | – | 1 |
The Charlson Comorbidity Index is a weighted index; scores range from 0–11, with higher scores indicating severity of comorbid conditions and higher risk of one-year mortality.
The telemonitored group had four participants considered to be within normal weight by their body mass index. Overall, compared with the usual care group, the telemonitored patients were more educated (X̄ = 10.2 years, SD = 1.1), less overweight or obese, had more support (e.g., married and not living alone), and had higher socioeconomic status based on Medicaid use and income; the usual care group was sicker (higher Charlson Comorbidity Index score) but had fewer hospital days.
Physiologic data collected from all patients at discharge (Time 1) indicated that body temperature, systolic blood pressure, and pulse oximeter oxygen saturation were similar between patients with and without telemonitoring, except for body weight (see Table 2). Usual care patients at Time 1 reported having more symptoms than the telemonitored group, including dyspnea (60% versus 33%), fatigue (80% versus 67%), limited activities (80% versus 67%), pain (60% versus 33%), coughing (80% versus 67%), difficulty in standing and walking (80% versus 33%), anxiety and feeling upset (40% versus 33%), and decreased appetite (80% versus 33%). The differences are not statistically significant, and the usual care group symptoms may have been affected by the apparently higher severity of disease compared to the telemonitored group. The authors also standardized nurse-administered verbal data collection as part of the use protocol when participants had difficulty completing study survey forms by themselves because of changes in their condition. Nevertheless, the telemonitored group, with less severe disease conditions overall, had identifiable changes in data, indicating risks that were useful for nurse-coaching.
Table 2.
Physiologic Parameters at Discharge, 7 Days, and 14 Days Postdischarge
| Time of Measurement | Temperature (°F) | Pulse Rate (bpm) | Systolic BP (mmHg) | Diastolic BP (mmHg) | Body Weight (lbs) | Oxygen Saturation (%) |
|---|---|---|---|---|---|---|
| At discharge | 97 | 106 | 124 | 76 | 134.5 | 91 |
| Telemonitored | 97 | 104 | 119 | 72 | 144.3 | 92.5 |
| Usual care | 97.6 | 95 | 124 | 69 | 208.5 | 89 |
| 7 days postdischargea | 97.5 | 103 | 129 | 71 | 127.5 | 93 |
| 14 days postdischargea | 97.1 | 93 | 116 | 68 | 126.5 | 93 |
Data at 7 and 14 days were only for the telemonitored participants.
BP—blood pressure
Note. All physiologic parameters were measured by median.
The remainder of this article will focus on the five intervention group patients as the authors learned how to successfully transmit data from patients’ homes to the research nurse’s office computers via the telemonitor, as well as how to support patients in recognizing changes in their conditions and use nurse-coaching with motivational interviewing to help them identify ways to manage the changes or get appropriate medical assistance.
Feasibility Goal 2: Fourteen-Day Telemonitor Data Transmission Outcomes
The second goal of the feasibility study was to successfully transmit data from patients’ homes to the study office computers via the telemonitor. Working with Honeywell Corporation and patients in the intervention group, the authors identified a modem-telemonitor that could work in WV with data service coverage for the GPRS that was expanded to many rural areas by T-Mobile®. All telemonitored patients were able to be followed for 14 days postdischarge and completed all study surveys through Time 3 data collection. Three completed all data through Time 5; one died before the end of the study and another moved and was lost to follow-up after the first 14 days (Time 3) of data collection.
Physiologic parameters were examined for two weeks following hospital discharge, and the telemonitors were able to transmit meaningful data. No persistent pattern was observed of monitored physiologic values identified during the first 14 days after discharge, although all values fluctuated for the telemonitored patients. The importance of symptom data became clear as nurses assisted patients in identifying self-management strategies and responses. The telemonitors successfully captured changes in symptoms typically seen with patients with lung cancer. For example, Time 1 data symptoms consistently reported by patients with non-small cell lung cancer before discharge included tiredness, pain, coughing, and limited activities (three to four patients). The symptoms of tiredness, and limited activity persisted even when pain and coughing decreased; symptoms of poor appetite along with nausea and vomiting became evident after 14 days. Patients who reported having to limit their activities more than usual also reported two or more symptoms during the first 14 days postdischarge. The symptom changes in telemonitored patients with lung cancer during the first two weeks following hospital discharge were readily identified using the telemonitors, even when physiologic changes were not apparent. For example, individuals perceived shortness of breath (dyspnea) to be less severe than indicated by pulse oximeters, and symptoms of pain, appetite, and dyspnea changed rapidly. Nevertheless, based on symptom changes as well as physiologic indicators, nurses were able to help patients recognize their level of risk to motivate symptom management and clinician contact.
Feasibility Goal 3: Educating Patients for Self-Management Based on Telemonitor Data
The clinical research nurses were able to identify risks for poor outcomes based on nursing knowledge and physician-specified indicators for each patient; they could base patient teaching on the physiologic and symptom data. However, the goal of the study was patient self-management rather than patient teaching. Clinical research nurses and investigators together analyzed situations encountered by patients in the motivational interviewing coaching episodes to change their approach from patient teaching to nurse-coaching. One example of the impact of that approach was evident in working with a patient who had repeated low oxygen levels, although he was on continuous concentrated oxygen via nasal cannula; oxygen saturation data were consistent with increased difficulty breathing when moving out of bed. The clinical research nurse originally wanted to suggest medication use or other medical treatments appropriate to management of dyspnea. The research team discussed that approach in light of needing to improve adherence to the fidelity of the intervention following the first episode; on the second day, the clinical research nurse used the protocol’s nurse-coaching techniques with the patient and his wife to explore when it was happening, what happened, who they could call to help them during an episode, and how the resources could be efficiently applied in time and accessed. The wife decided to call the company who had installed the oxygen to come out and test the system. When they followed up, the oxygen supplier identified a defect in the tubing and replaced the system. That resulted in improved oxygenation for the last week of the study, and the patient and his wife reported their satisfaction with having been able to solve the problem. Nurse-coaching using motivational interviewing became a key component once the research nurses became more skilled at the techniques. Working with the intervention patients provided opportunities to refine skills and identify potential benefits of helping patients develop self-management skills.
Although one patient’s wife did not like the monitor location (e.g., bedroom), all patients and families who completed the satisfaction survey agreed or strongly agreed that they would want to use telemonitoring in the future and would recommend the use of a telemonitor to others. They felt more involved in their care, allowing them to gain a better understanding of their condition and to manage their health and provide a sense of security and peace of mind.
Discussion
These feasibility study findings helped the authors to understand the issues that would be faced in a randomized clinical trial study, and lessons were learned as feasibility study goals were attained. In looking at enrollment and retention (Goal 1), a change in Time 1 data collection, including obtaining demographic and disease profile data, to a period immediately following consent eliminated the possibility of missing patients prior to discharge. The feasibility study also allowed the primary investigator and clinical research nurses to refine the consent process to include the patient and family, as well as improved their ability to answer patients’ questions about the project to support eligible patients toward informed participation.
For Goal 2, the feasibility study provided relevant data used to modify the initial protocol and expand telemonitor use. A major change was identification of a modem GPRS monitor that could work in rural WV. Initially, only one company provided GPRS service in this rural mountainous region and coverage was limited; with two additional companies available, the best monitor transmission for that rural area was identified. Successful home telemonitoring provided data to fill the gap in knowledge about changes in the vital signs and symptoms of patients with lung cancer between hospital discharge and the usual two-week postdischarge clinician visit. Nevertheless, because symptom data could be collected via telephone, it may be possible to continue to monitor symptoms using the same questions that had been programmed into the telemonitor after the intervention’s two-week period. A modification to symptom data collection for two months also could help fill the knowledge gap about patient symptoms and be used for continued nurse-coaching. Similar to previous studies (McLean et al., 2012; Paget et al., 2010; Sicotte, Paré, Morin, Potvin, & Moreault, 2011), telemonitors were easy to use and satisfaction in using telemonitors was reported by home-dwelling patients who were ill and their families. Overall, patient and family satisfaction was consistent with previous research using the HomMed telemonitors for patients with heart failure (Narsavage & Jones, 2003; Paget et al., 2010).
Goal 3 of the intervention study was perhaps the greatest challenge: moving from a nurse perspective of providing suggestions to patients to the study protocol of helping patients’ and their families explore what they knew, what resources they had, and how they could access those resources. The data on physiologic and symptom changes were useful indicators of patient risk and nurses were able to use motivational interviewing techniques based on their nursing knowledge to coach patients to self-management.
Challenges recognized during the feasibility study included five important aspects that must be considered when conducting a telemonitor study in rural states such as WV.
Patients discharged to hospice care were too ill to fully participate in the study; therefore, hospice services were added as an exclusion criterion.
Patient homes with landline phone connections had successful transmission of data. The originally provided GPRS data system was only able to connect from an urban or suburban setting. Newer monitors had greater service areas and connected in remote rural mountains.
Finding homes for research visits was challenging, as rural areas had gravel or mud roads without street signs, little availability of Global Positioning System mapping directions, and often were only navigable by four-wheel drive vehicles. Getting detailed directions from patients was essential.
Patients’ perceptions of symptoms and physiologic values could vary and needed to be assessed together when things changed. Patients were advised to use the telemonitors more often if their condition changed other than at the scheduled research time.
Many participants were not able to continue to complete study survey forms by themselves, so standardized nurse-administered verbal data collection was needed.
Implications for Nursing Research
Enrollment and retention in cancer research in rural areas requires additional study. Less willingness to participate in the study was identified when there seemed to be no financial benefit or improved care unless the patient received a telemonitor. Research should offset financial limitations and address social needs for participation support of patients. Symptoms, assessable by phone, might be useful as proxy indicators for more involved physiologic testing to identify risk of lower functioning, use of emergent care, and length of time to monitor signs and symptoms after hospital discharge, and needs to be explored.
All the lessons learned and decisions made as a result of the feasibility study are expected to lead to a more efficient clinical trial. Difficulties in recruiting and retaining patients in the study likely will remain as a crucial issue; additional research is needed to explore recruitment and retention in Appalachia—perhaps using methods learned with recruitment and retention in minority populations. Nevertheless, the authors are confident that telemonitor assessment of data can provide information to coach patients, and are optimistic about the potential impact of nurse-coaching to develop self-management skills of patients living with lung cancer.
Knowledge Translation.
Assessment of patients living in rural areas is feasible using telemonitors.
Combining physiologic data with symptom information can identify patient risk after hospitalization.
Nurses can base coaching interventions on telemonitor data to enhance self-management of rural patients.
Footnotes
No financial relationships to disclose.
References
- Anderson C. Remote monitoring helps Geisinger cut readmissions. 2012 Retrieved from http://www.healthcareitnews.com/news/remote-monitoring-helps-geisinger-cut-readmissions.
- Borak J, Salipante-Zaidel C, Slade MD, Fields CA. Mortality disparities in Appalachia: Reassessment of major risk factors. Journal of Occupational and Environmental Medicine. 2012;54:146–156. doi: 10.1097/JOM.0b013e318246f395. [DOI] [PubMed] [Google Scholar]
- Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Krumholz HM. Telemonitoring in patients with health failure. New England Journal of Medicine. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YJ, Narsavage GL, Culp SL, Weaver TE. The development and psychometric analysis of the short-form Pulmonary Functional Status Scale (PFSS-11) Research in Nursing and Health. 2010;33:477–485. doi: 10.1002/nur.20403. [DOI] [PubMed] [Google Scholar]
- Cook R. Exploring the benefits and challenges of telehealth. Nursing Times. 2012;108(24):16–17. [PubMed] [Google Scholar]
- Dellifraine JL, Dansky KH. Home-based telehealth: A review and meta-analysis. Journal of Telemedicine and Telecare. 2008;14:62–66. doi: 10.1258/jtt.2007.070709. [DOI] [PubMed] [Google Scholar]
- Finkelstein SM, Speedie SM, Potthoff S. Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemedicine Journal and E-Health. 2006;12:128–136. doi: 10.1089/tmj.2006.12.128. [DOI] [PubMed] [Google Scholar]
- Fox SW, Lyon DE. Symptom clusters and quality of life in survivors of lung cancer. Oncology Nursing Forum. 2006;33:931–936. doi: 10.1188/06.ONF.931-936. [DOI] [PubMed] [Google Scholar]
- Garcia-Aymerich J, Hernandez C, Alonso A, Casas A, Rodriquez-Roisin R, Anto JM, Roca J. Effects of an integrated care intervention on risk factors of COPD readmission. Respiratory Medicine. 2007;101:1462–1469. doi: 10.1016/j.rmed.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Giamouzis G, Mastrogiannis D, Koutrakis K, Karayannis G, Parisis C, Rountas C, Triposkiadis F. Telemonitoring in chronic health failure: A systematic review. Cardiology Research and Practice. 2012;1(1):410820. doi: 10.1155/2012/410820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryx M, O’Donnell K, Horn K. Lung cancer mortality is elevated in coal-mining areas of Appalachia. Lung Cancer. 2008;62(1):1–7. doi: 10.1016/j.lungcan.2008.02.004. [DOI] [PubMed] [Google Scholar]
- McLean S, Nurmatov U, Liu JL, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease: Cochrane Review and meta-analysis. British Journal of General Practice. 2012;62(604):e739–e749. doi: 10.3399/bjgp12X658269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narsavage GL, Jones S. CareWatch: Homecare that is high tech AND high touch! 2003 Retrieved from http://www.nursinglibrary.org/vhl/handle/10755/148031.
- Paget T, Jones C, Davies M, Evered C, Lewis C. Using home telehealth to empower patients to monitor and manage long term conditions. Nursing Times. 2010;106(45):17–19. [PubMed] [Google Scholar]
- Puig-Junoy J, Casas A, Font-Planells J, Escarrabill J, Hernández C, Alonso J, Roca J. The impact of home hospitalization on healthcare costs of exacerbations in COPD patients. European Journal of Health Economics. 2007;8:325–332. doi: 10.1007/s10198-006-0029-y. [DOI] [PubMed] [Google Scholar]
- Sicotte C, Paré G, Morin S, Potvin J, Moreault MP. Effects of home telemonitoring to support improved care for chronic obstructive pulmonary diseases. Telemedicine and e-Health. 2011;17(2):95–103. doi: 10.1089/tmj.2010.0142. [DOI] [PubMed] [Google Scholar]
- West Virginia Cancer Registry. West Virginia Cancer Registry 2012 annual report. 2012 Retrieved from http://www.dhhr.wv.gov/oeps/cancer/Documents/WVCR%202012%20Annual%20Report_1_8_2013.pdf.