Abstract
Introduction: Childhood adversity is gaining increasing attention as a plausible etiological factor in the development of psychotic disorders. Childhood residential mobility is a potential risk factor that has received little attention in this context. Methods: We used registry data to estimate associations of residential mobility with narrow and broad schizophrenia and bipolar disorder across the course of childhood among 1.1 million individuals born in Denmark 1971–1991 and followed from age 15 through 2010. We assessed effect modification by sex, family history of mental disorder, the presence of siblings close in age, and distance moved. Results: In individual-year models adjusted for family history, urbanicity at birth, and parental age, mobility at all ages except the year of birth was associated with heightened risk of narrow and broad schizophrenia, and risk increased with age at moving and with the number of moves. Further adjustment for mobility at all ages 0–15 revealed associations mainly during the latter half of childhood, which were strongest during adolescence. Associations between mobility and bipolar disorder were fewer and weaker compared to schizophrenia. There was modest evidence of interaction with family history of psychiatric diagnosis, but little evidence for interaction by sex, the presence of closely-aged siblings, or distance moved. Schizophrenia associations did not appear attributable to increased mobility among adolescents with earlier onset. Conclusions: Mobility may increase risk for psychotic disorders, particularly schizophrenia. Children may be especially vulnerable during adolescence. Future research should investigate the importance of school changes and the potential for interaction with genetic risk.
Key words: epidemiology, residential mobility, childhood adversity
Introduction
Childhood adversity is gaining attention as an etiologically relevant factor in the epidemiology of psychotic disorders.1–3 Much research has focused on long-term consequences of traumas such as abuse and neglect.4,5 However, other forms of adversity, including social and economic disadvantage,6,7 peer victimization or bullying,8 and disruptive family environments,9 may have etiological importance. Such adversities may disrupt processes of stress reactivity, cognition and emotion regulation in the developing brain,10 by acting alone or in conjunction with earlier environmental or genetic exposures.11
Childhood residential mobility is a potential common form of adversity that could impact psychosis risk. Mobility disrupts the continuity of children’s psychosocial contexts, challenging them to navigate new and unfamiliar neighborhoods, schools, and peer groups.12,13 Childhood mobility has been associated with psychotic-like symptoms in children14 as well as outcomes such as depression, behavioral problems, drug use, and attempted suicide.13,15–17 However, few studies of the influence of mobility on risk for adult psychotic disorders exist.18–20 Two previous Danish studies found that residential changes during upbringing were associated with schizophrenia19 but not bipolar disorder.18 These results warrant replication. Furthermore, no studies have assessed the potential for effect modification of mobility associations by factors that are relevant to the effects of mobility in children.
This study investigates how childhood residential mobility, conceptualized as a form of adversity that disrupts psychosocial development, affects risk for schizophrenia and bipolar disorder in adulthood. We expand upon the results of previous studies in 3 ways. First, we reinvestigate associations of childhood residential mobility with schizophrenia and bipolar disorder in Denmark, using a more recent cohort that allows for greater power to detect age- and dose-specific associations and more stringent control for confounding. Second, because developmental insults may differentiate schizophrenia and bipolar disorder etiologically,21,22 we include explicit presentation of associations with bipolar disorder and include broadly as well as narrowly defined schizophrenia to allow comparison of these 3 outcomes. Third, we test for interactions between mobility and the following factors: (a) sex, based on evidence that mobility may affect boys and girls differently13,16; (b) distance moved, using change of geographic region as a proxy for moving a greater distance; (c) the presence of siblings within 3 years of age of the participant, both based on the relevance of contextual factors and social ties to the mental health effects of mobility in children12,23; (d) family history of mental disorder, based on evidence that genetic liability may increase susceptibility to environmental exposures.24 We also include a test for interaction with age during follow-up to assess whether the associations of schizophrenia with mobility later in childhood are confined to those with earlier onset.
Methods
Study Population
We used the Danish Civil Registration System25 (CRS) to establish a population-based cohort of ≈1.1 million individuals born in Denmark between January 1st, 1971, and June 30th, 1991. The CRS contains continually-updated information on all Danish residents, including vital status, sex, date of birth, identity of parents and siblings, and place of birth and residence. Residential information has been recorded prospectively for all Danish residents and is complete at the municipality level since 1971.25 Individuals were included if both parents were identified in the CRS and born in Denmark, and the individual was alive and residing in Denmark on his or her 15th birthday. Compared to previous studies of mobility in Denmark,18,19 the current study cohort consisted entirely of individuals with residential history information available from birth, with more recent follow-up. It also excludes first- and second-generation immigrants, among whom risk of schizophrenia is increased.26,27
Psychiatric Diagnoses and Family History
We linked CRS data to the Danish Psychiatric Central Register, which contains all admissions to inpatient psychiatric facilities since 1969 and specialty outpatient and emergency room visits since 1995.28 Diagnoses followed the International Classification of Diseases, 8th revision (ICD-8) prior to 1994 and the ICD-10 from 1994 onward.29,30 Diagnoses were defined as follows: narrow schizophrenia: ICD-10 F20 or ICD-8 295 (excluding 295.79); broad schizophrenia: ICD-10 F20-F29 or ICD-8 295, 297, and 298.39; bipolar disorder: ICD-10 F30 and F31 or ICD-8 296.19 and 296.39. Onset was defined as the first day of the first visit during which a diagnosis was recorded. Family history of disorder was measured in the same manner and represented using 3 categorical variables, one each for mothers, fathers, and siblings. Parents were defined by legal relationship, and siblings were identified as individuals with the same mother. For analyses of narrow schizophrenia, family members were classified hierarchically as having narrow schizophrenia, broad schizophrenia, any other mental disorder, or none. For analyses of broad schizophrenia, family members were classified hierarchically as having narrow or broad schizophrenia, any mental disorder, or none. For analyses of bipolar disorder, family members were classified hierarchically as having bipolar disorder, another affective disorder (ICD-10 F32-F39 or ICD-8 296 (excluding 296.19 and 296.39), 298.09, 298.19, 300.49, and 301.19), any mental disorder, or none.
Residential Mobility
We used the CRS to measure mobility according to 2 different geographical classifications. First, because the effect of moving was previously accounted for by municipality changes as opposed to moves within municipalities,19 moves were defined as changes between any of 276 municipalities in Denmark before the 2007 municipality reform. We calculated the number of moves during each year of age between birth and the 15th birthday. Moves to and from foreign countries were extremely rare (less than ½% in all ages) and not counted. The number of moves was categorized as 0, 1, 2, or 3+ for narrow and broad schizophrenia and as 0, 1, or 2+ for bipolar disorder.
Second, as a proxy for distance, moves were classified according to changes between five larger geographical regions in Denmark instituted after the 2007 municipality reform (as these are merely geographical classifications, the time periods do not influence the study). For these analyses, mobility in each year was classified as no moves, change(s) of municipality within the same region, or change(s) of municipality between regions.
Additional Measures
Birth period, age, sex, parental age, urbanicity level at birth, and the presence of siblings within 3 years of age were created using CRS information. Birth period and sex were combined into a 6-category variable indicating males and females who were born in 1971–1980, 1981–1985, and 1985–1991. For narrow and broad schizophrenia, age was grouped as 15, 16, 17, 18, 19, 20–21, 22–23, 24–25, 26–27, 28–29, 30–34, 35+. For bipolar disorder, age was grouped as 15–16, 17–18, 19, 20–21, 22–23, 24–25, 26–27, 28–29, 30–34, 35+. Maternal and paternal age at birth were categorized as <22, 22–25, 26–29, 30–34, and 35+. Urbanicity level at birth was classified as capital, capital suburb, provincial city, provincial town, or rural.31 Three binary variables were created indicating the presence of older, younger, and any siblings within 3 years of age.
Study Design and Analysis
Data were analyzed prospectively. The study started on the 15th birthday and ended at disorder onset, death, emigration from Denmark, or December 31, 2010 (whichever came first), when cohort members were between 19 and 39 years old. Poisson regression, implemented in the GENMOD procedure of SAS 9.2,32 was used to estimate incidence rate ratios (RRs) for each disorder, approximating Cox regression.33 Models were adjusted for birth period, age, sex, their interaction, calendar year, urbanicity at birth, parental age, and family history of mental disorder. Age, calendar year, and family history were measured over the course of follow-up and included as time-varying covariates. Mobility, birth period, sex, parental age, urbanicity, and the presence of siblings were time-fixed. Calendar year was categorized into 1-year bands except that years 1986–1988 were collapsed for narrow and broad schizophrenia and 1986–1993 were collapsed for bipolar disorder. Likelihood ratio tests were used to test each mobility variable as a whole and for interaction tests. Likelihood ratio-based 95% confidence intervals were calculated for each estimate. Score tests were used to check the models for overdispersion.34
We estimated both individual-year models (containing mobility for one age at a time) and mutually-adjusted models (containing mobility during all ages 0–15). We tested for interactions with sex, family history (which for simplicity was dichotomized as any disorder in a parent or sibling vs none35), having siblings, and for narrow and broad schizophrenia, age during follow-up (categorized as younger than 20, 20–24, and 25 or older), in models adjusted for birth period, age, sex, their interaction, and calendar year. Sibling interaction was considered among those with mothers born on or after April 1st, 1935 to ensure completeness of sibling information in the registry.25 We also tested for an overall interaction between mobility at all ages and family history for narrow and broad schizophrenia. For region change, interactions were evaluated using contrast tests.
This study was approved by the Danish Data Protection Agency.
Results
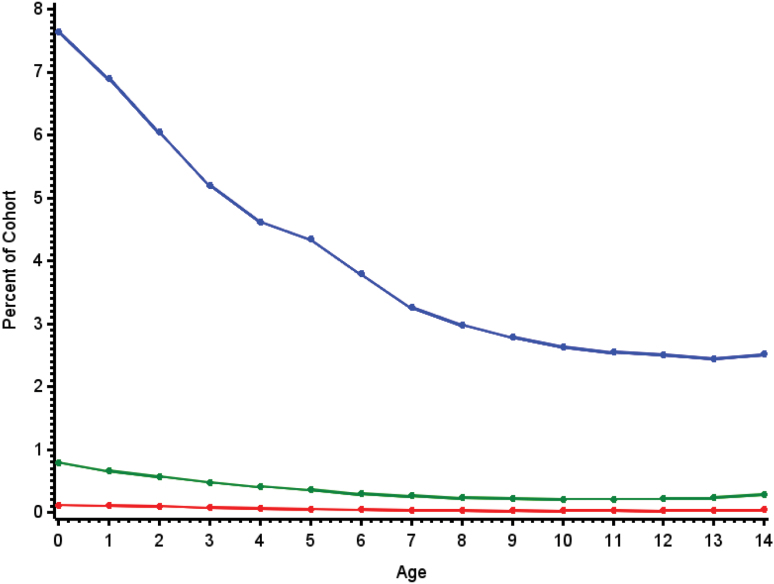
Among the 1.1 million persons born in Denmark 1971–1991, 7277 cases of narrow schizophrenia, 12 970 cases of broad schizophrenia, and 2841 cases of bipolar disorder were identified during the 16.8 million person-years of follow-up. Figure 1 depicts the proportion of individuals who moved once, twice, and 3 or more times each year. Mobility was highest in the year of birth and declined across childhood. Less than 1% of cohort members moved twice in a given year, and very few moved 3 or more times.
Fig. 1.
Proportion of cohort members who moved once (blue line), twice (green line), and 3 or more times (red line) by age during childhood. For a color version, see this figure online.
Individual-Year Models
Mobility was associated with narrow schizophrenia at all ages except the year of birth. Associations appeared to increase with the number of moves at each age, and with age at moving (figure 2A). Moving once was significantly associated with schizophrenia in all years except age 0 and estimates ranged from 1.07 (95% CI = 0.99–1.16) to 1.86 (95% CI = 1.68–2.05). Moving twice was significantly associated in all years except 0, 1 and 9, and estimates ranged from 1.17 (95% CI = 0.95–1.42) to 2.12 (95% CI = 1.65–2.68). Moving 3 or more times was significantly associated for ages 5 and 10–14, with estimates ranging from 0.81 (95% CI = 0.37–1.51) to 3.72 (95% CI = 2.32–5.61).
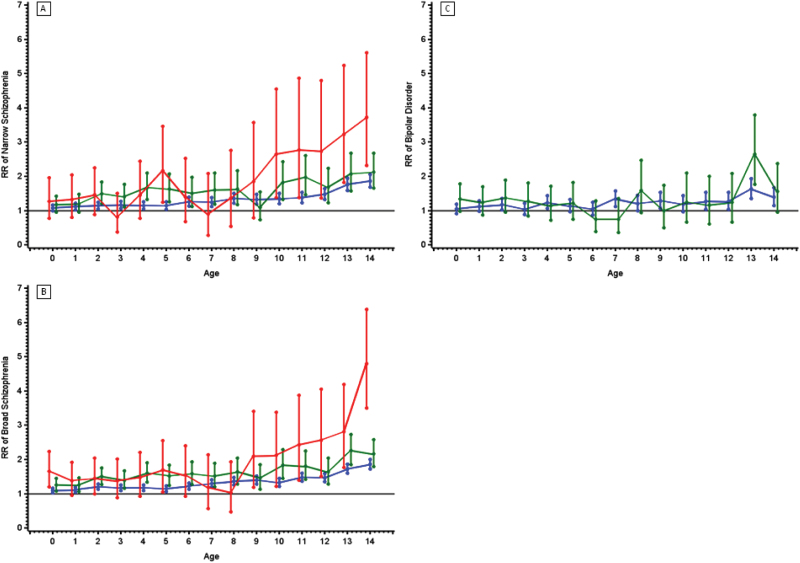
Fig. 2.
Relative risks and 95% confidence intervals (vertical lines) of narrowly defined schizophrenia (A), broadly defined schizophrenia (B), and bipolar disorder (C) associated with moving each year from birth through age 14. Blue lines represent RRs for 1 move. Green lines represent RRs for 2 moves for narrow and broad schizophrenia and 2 or more moves for bipolar disorder. Red lines represent 3 or more moves. Estimates are adjusted for age, sex, calendar year, birth period, parental age, urbanicity level at birth, and history of mental disorder in a parent or sibling. For a color version, see this figure online.
Mobility was associated with broad schizophrenia at all ages. The pattern of RRs largely mirrored that observed for narrow schizophrenia (figure 2B). The largest RR was for those who moved 3 or more times at age 14 (RR = 4.80, 95%CI = 3.50–6.38).
Mobility was associated with bipolar disorder at ages 2, 4, 7–9, and 13–14. The pattern of increasing risk with number of moves and age at moving was less evident than for narrow and broad schizophrenia, except for an apparent jump in RR at age 13 (figure 2C). Moving once was significantly associated with bipolar disorder at ages 2, 4, 7–9, and 11–14, and estimates ranged from 1.04 (95% CI = 0.89–1.21) to 1.63 (95% CI = 1.35–1.93). Moving 2 or more times was significantly associated with bipolar disorder risk only at age 13, with estimates ranging from 0.75 (95% CI = 0.39–1.28) to 2.65 (95% CI = 1.76–3.79).
RRs of all 3 outcomes for moves at ages 0, 5, 10 and 15 are presented in table 1.
Table 1.
Adjusted Relative Risks of Narrow Schizophrenia, Broad Schizophrenia, and Bipolar Disorder Associated With Residential Mobility at Ages 0, 5, 10, and 15a,b
| Age | Movesc | Narrow Schizophrenia | Broad Schizophrenia | Bipolar Disorder | |||
|---|---|---|---|---|---|---|---|
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | ||
| 0 | 0 | 1.00 | — | 1.00 | — | 1.00 | — |
| 1 | 1.07 | (0.99–1.16) | 1.09 | (1.03–1.16) | 1.05 | (0.92–1.19) | |
| 2 | 1.17 | (0.95–1.42) | 1.25 | (1.07–1.45) | 1.34 | (0.98–1.78) | |
| 3 | 1.27 | (0.77–1.96) | 1.66 | (1.19–2.23) | |||
| 5 | 0 | 1.00 | — | 1.00 | — | 1.00 | — |
| 1 | 1.14 | (1.03–1.26) | 1.14 | (1.06–1.23) | 1.13 | (0.96–1.33) | |
| 2 | 1.63 | (1.26–2.06) | 1.52 | (1.25–1.84) | 1.21 | (0.75–1.83) | |
| 3 | 2.17 | (1.25–3.46) | 1.69 | (1.05–2.55) | |||
| 10 | 0 | 1.00 | — | 1.00 | — | 1.00 | — |
| 1 | 1.34 | (1.20–1.50) | 1.33 | (1.22–1.44) | 1.19 | (0.97–1.43) | |
| 2 | 1.82 | (1.33–2.43) | 1.84 | (1.45–2.29) | 1.25 | (0.67–2.10) | |
| 3 | 2.65 | (1.37–4.55) | 2.12 | (1.22–3.38) | |||
| 14 | 0 | 1.00 | — | 1.00 | — | 1.00 | — |
| 1 | 1.86 | (1.68–2.05) | 1.86 | (1.73–2.00) | 1.39 | (1.15–1.67) | |
| 2 | 2.12 | (1.65–2.68) | 2.16 | (1.79–2.58) | 1.55 | (0.95–2.37) | |
| 3 | 3.72 | (2.32–5.61) | 4.80 | (3.50–6.38) | |||
Note: RR, relative risk; CI, confidence interval.
aEstimates adjusted for age, sex, birth period, calendar year, urbanicity of birth, parental age, and parent or sibling mental disorder.
bAmong 1.1 million individuals born in Denmark between 1971 and 1991 who were followed for the disorder of interest from their 15th birthday through 2010.
cFor narrow and broad schizophrenia, “3” represents 3 or more moves. For bipolar disorder, “2” represents 2 or more moves.
Mutual Adjustment
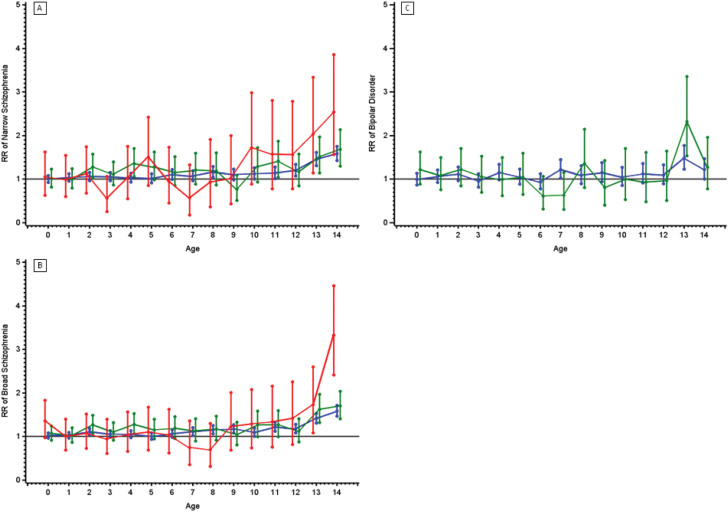
Figure 3 depicts mutually-adjusted associations. Note that the scale is slightly reduced compared to figure 2. Although mutual adjustment generally reduced the magnitude of estimates and widened CIs, inferences from the individual-year models remained largely intact, especially for the second half of childhood. Mobility was associated with narrow schizophrenia at ages 8 and 10–14, with broad schizophrenia at ages 2, 4, and 7–14, and with bipolar disorder at ages 7 and 13 only. The tendency for RRs for schizophrenia to increase with age at moving was still visible across childhood for those who moved once, and from age 11 onward for those who moved 2 and 3 or more times. This pattern was again less apparent for bipolar disorder, except for an increase in RR for moves at age 13.
Fig. 3.
Relative risks and 95% confidence intervals (vertical lines) of narrowly defined schizophrenia (A), broadly defined schizophrenia (B), and bipolar disorder (C) associated with moving each year from birth through age 14. Blue lines represent RRs for 1 move. Green lines represent RRs for 2 moves for narrow and broad schizophrenia and 2 or more moves for bipolar disorder. Red lines represent 3 or more moves. Estimates are adjusted for age, sex, calendar year, birth period, parental age, urbanicity level at birth, history of mental disorder in a parent or sibling, and mobility at all other ages. For a color version, see this figure online.
Interaction
Ages for which interactions were statistically significant are presented in the supplementary table. We found little evidence that mobility associations were modified by sex, having siblings, or distance moved.
There was modest evidence of interaction with family history of psychiatric diagnosis. The overall mobility-by-family history interactions were significant for both narrow (χ2 = 66.8354, df = 45, P =.0189) and broad (χ2 = 110.0736, df = 45, P < .0001) schizophrenia. Individual-year model interactions were significant at 2 different ages for narrow schizophrenia, 5 different ages for broad schizophrenia, and 5 different ages for bipolar disorder (supplementary material). For the majority of these interactions, estimates indicated lower relative risks when family history was present. Group-specific RRs were generally positive or nonsignificant; in no case was the association between mobility and disorder significantly positive in one group and significantly negative in the other. Associations between mobility and all 3 outcomes, by the presence of family history of psychiatric diagnosis, are presented in supplementary figures 1–3.
Interactions with age during follow-up were significant only at ages 2 and 10 for narrow schizophrenia. The model for age 7 was not estimated due to sparse data. Tests were significant at ages 10 and 11 for broad schizophrenia. For both sets of age 10 and 11 estimates, only the age 11 estimates for broad schizophrenia indicated that RRs were greater for those in the youngest age group (data not shown).
Discussion
Childhood residential mobility was associated with heightened risk of narrow and broad schizophrenia, which increased with the number of moves in a year and with the age at moving. Associations with bipolar disorder were fewer and showed less of an increase with age and the number of moves. These associations were robust to adjustment for family history of disorder, implying that associations are not entirely attributable to the presence of mental disorder in the family. Associations were also robust to adjustment for urbanicity at birth and parental age, and to the exclusion of first- and second-generation immigrants.
This study presents a number of new findings that have important implications for the epidemiology of psychotic disorders. Mobility was associated with schizophrenia after controlling for mobility at all ages simultaneously, and the increase in risk with age at moving was preserved. This implies that mobility associations during adolescence were not completely confounded by earlier mobility, or by factors that create a general propensity for mobility among families (as long as this propensity is independent of the child’s age). It also highlights adolescence as a period of vulnerability to psychosocial adversity. Stable social contexts may help adolescents navigate the social world and meet the challenges posed by emerging adulthood.36,37 Executive function, impairment of which is a core feature of schizophrenia, continues to develop during adolescence.38 Adolescence is also a period of heightened dopamine activity, and a sensitive period for the effects of social stress on HPA axis function and long-term dopamine regulation.37,39,40 Adolescence is also important in 2-hit models of schizophrenia,11,41 in which early and later exposures interact (eg, ref. 42).
This is the first study to assess effect modification of the associations between childhood mobility and adult psychotic disorders. We found modest, preliminary evidence for effect modification by family history of disorder. Although interactions were not in the expected direction, this may be related to our use of a multiplicative model, as the direction of statistical interactions can depend on the type of model being used.43 Although this study does not provide a formal test of gene-environment interaction, the possibility of such effects is intriguing. Future studies should explore whether mobility confers risk differently according to genetic liability or the presence of specific genetic variants.24
We found little evidence of effect modification by sex, having siblings, or distance moved. The fact that relative risks did not differ significantly between those who changed regions and those who changed municipalities within a given region suggests that once a municipality change occurs, additional distance is not associated with additional risk. One possible explanation is that both municipality and region changes are proxies for changes of school.19 The potential importance of school change is consistent with the lower magnitude of associations of mobility in early childhood, before children enter school, and the higher magnitude of associations during adolescence, when peer relationships are especially salient. It is also consistent with evidence that school mobility is associated with psychotic-like symptoms in early adolescents.14
This study is the first to report associations between childhood mobility and bipolar disorder in adulthood. Associations with bipolar disorder were fewer and weaker than those with schizophrenia and showed less increase with age, implying some specificity of effect for mobility. We conducted additional sensitivity analyses to assess whether the associations with bipolar disorder were attributable to the presence of diagnostic overlap, but did not find evidence for this explanation (see supplementary material). Future studies should explore potential associations between childhood mobility and bipolar disorder in adulthood.
Whether our results reflect causal effects of mobility on psychotic disorder is unknown. For example, mobility may be a marker for other childhood adversities, such as parental discord, that increase risk for adult disorder.44 Although we cannot rule out the possibility of confounding, it may not fully explain our findings for schizophrenia, as mobility associations persisted for the latter half of childhood after adjustment for mobility in all other years and increased with age during this period. It is also possible that associations between mobility and schizophrenia during adolescence are due to greater mobility among children with prodromal symptoms, a form of reverse causation or protopathic bias.45 Although this cannot be ruled out, our findings did not support this explanation, as we did not find strong evidence that children who moved during adolescence were more likely to have earlier onset.
This study was limited in that we lacked information on why families moved. We were therefore unable to account for social, economic, or other individual- or family-related conditions or events during childhood that may have prompted a move and increased disorder risk.44 We were also unable to investigate many circumstances under which moves might confer greater or less risk. In addition, our results may not generalize outside of Denmark or to first- and second-generation immigrants. We also lacked data on school attendance, so were unable to test whether the effect of moving might be explained by school change. We used a proxy measure for distance moved, and using a more direct measure of distance may yield different results. Because the oldest cohort members were 39 years old at the end of follow-up, our findings may not apply to onset occurring later in adulthood. Finally, we investigated mobility up to age 15 and therefore did not account for the possible contribution of mobility during late adolescence and early adulthood.
An important strength of this study is that we had access to full residential information for the entire exposure period of interest, which was measured prospectively, without relying on recall, and independently of the outcomes under study. In addition, the catchment area for the psychiatric registry includes the entire Danish population, for whom psychiatric care is accessible and provided free of charge. This allowed for investigation of age-specific mobility effects. It also allowed us to control for family history of mental illness, which is perhaps the most important confounder in studies of environmental risk factors for psychiatric disorder.
This study extends previous investigations of childhood mobility and schizophrenia and bipolar disorder in Denmark.18,19 We found that childhood residential mobility is associated with increased risk for psychotic disorders in adulthood, and may be relatively more specific to schizophrenia compared to bipolar disorder. Children may be especially vulnerable to the effects of mobility during adolescence. Risk does not appear to be modified by sex, having siblings, or distance moved. Future studies should investigate the possible modifying role of genetic risk, the role of school changes in predicting risk, and potential interactions with early environmental exposures.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
National Institute of Mental Health (5T32MH014592); the Intramural Research Program of the NIMH; the National Institute on Drug Abuse (DA026652 to W.W.E.); the Stanley Medical Research Institute; and by The Lundbeck Foundation.
Supplementary Material
Acknowledgments
This study was conducted when Diana Paksarian was with the Department of Mental Health, Johns Hopkins Bloomberg School of Public Health. Diana is now with the National Institute of Mental Health. The views and opinions expressed in this manuscript are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or agencies or the U.S. government. Results from this study were presented as a poster at the 14th International Congress on Schizophrenia Research in Orlando, Florida on April 23, 2013, and the corresponding abstract was published in Schizophrenia Bulletin (2013) 39(Suppl 1): S74–S75. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Read J, Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiat Scand. 2005;112:330–350. [DOI] [PubMed] [Google Scholar]
- 2. Fisher HL, Jones PB, Fearon P, et al. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychol Med. 2010;40:1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2012;1:1–13. [DOI] [PubMed] [Google Scholar]
- 4. Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Castle DJ, Scott K, Wessely S, Murray RM. Does social deprivation during gestation and early life predispose to later schizophrenia? Soc Psychiatry Psychiatr Epidemiol. 1993;28:1–4. [DOI] [PubMed] [Google Scholar]
- 7. Wicks S, Hjern A, Gunnell D, Lewis G, Dalman C. Social adversity in childhood and the risk of developing psychosis: a national cohort study. Am J Psychiatry. 2005;162:1652–1657. [DOI] [PubMed] [Google Scholar]
- 8. Schreier A, Wolke D, Thomas K, et al. Prospective study of peer victimization in childhood and psychotic symptoms in a nonclinical population at age 12 years. Arch Gen Psychiatry. 2009;66:527. [DOI] [PubMed] [Google Scholar]
- 9. Bebbington PE, Bhugra D, Brugha T, et al. Psychosis, victimisation and childhood disadvantage evidence from the second British National Survey of Psychiatric Morbidity. Br J Psychiatry. 2004;185:220–226. [DOI] [PubMed] [Google Scholar]
- 10. Meyer-Lindenberg A, Tost H. Neural mechanisms of social risk for psychiatric disorders. Nat Neurosci. 2012;15:663–668. [DOI] [PubMed] [Google Scholar]
- 11. Fatemi SH, Folsom TD. The neurodevelopmental hypothesis of schizophrenia, revisited. Schizophr Bull. 2009;35:528–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hango DW. The long-term effect of childhood residential mobility on educational attainment. Sociol Quart. 2006;47:631–664. [Google Scholar]
- 13. DeWit DJ. Frequent childhood geographic relocation: its impact on drug use initiation and the development of alcohol and other drug-related problems among adolescents and young adults. Addict Behav. 1998;23:623–634. [DOI] [PubMed] [Google Scholar]
- 14. Singh SP, Winsper C, Wolke D, Bryson A. School mobility and prospective pathways to psychotic-like symptoms in early adolescence: a prospective birth cohort study. J Am Acad Child Adolesc Psychiatry. 2014;53:518–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychol Med. 2003;33:1341–1355. [DOI] [PubMed] [Google Scholar]
- 16. Osypuk TL, Tchetgen EJT, Acevedo-Garcia D, et al. Differential mental health effects of neighborhood relocation among youth in vulnerable families: results from a randomized trial. Arch Gen Psychiatry. 2012;69:1284–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qin P, Mortensen PB, Pedersen CB. Frequent change of residence and risk of attempted and completed suicide among children and adolescents. Arch Gen Psychiatry. 2009;66:628. [DOI] [PubMed] [Google Scholar]
- 18. Pedersen CB, Mortensen PB. Urbanicity during upbringing and bipolar affective disorders in Denmark. Bipolar Disord. 2006;8:242–247. [DOI] [PubMed] [Google Scholar]
- 19. Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry. 2001;58:1039. [DOI] [PubMed] [Google Scholar]
- 20. Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson JE, Allebeck P. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Arch Gen Psychiatry. 2010;67:914. [DOI] [PubMed] [Google Scholar]
- 21. Demjaha A, MacCabe JH, Murray RM. How genes and environmental factors determine the different neurodevelopmental trajectories of schizophrenia and bipolar disorder. Schizophr Bull. 2012;38:209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Murray RM, Sham P, Van Os J, Zanelli J, Cannon M, McDonald C. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophr Res. 2004;71:405–416. [DOI] [PubMed] [Google Scholar]
- 23. Buu A, DiPiazza C, Wang J, Puttler LI, Fitzgerald HE, Zucker RA. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. J Stud Alcohol Drugs. 2009;70:489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull. 2008;34:1066–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pedersen CB, Gøtzsche H, Møller JØ, Mortensen PB. The Danish civil registration system. Dan Med Bull. 2006;53:441–449. [PubMed] [Google Scholar]
- 26. Pedersen C, Demontis D, Pedersen M, et al. Risk of schizophrenia in relation to parental origin and genome-wide divergence. Psychol Med. 2012;42:1515–1521. [DOI] [PubMed] [Google Scholar]
- 27. Cantor-Graae E, Pedersen CB. Full spectrum of psychiatric disorders related to foreign migration: a Danish population-based cohort study. JAMA Psychiatry. 2013;70:427–435. [DOI] [PubMed] [Google Scholar]
- 28. Mors O, Perto GP, Mortensen PB. The Danish psychiatric central research register. Scand J Public Health. 2011;39:54–57. [DOI] [PubMed] [Google Scholar]
- 29. Organization WH. International Classification of Diseases, Eighth Revision (ICD-8). Geneva, Switzerland: World Health Organization; 1967. [Google Scholar]
- 30. Organization WH. The ICD-10 Classification of Mental and Behavioral Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 31. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603–608. [DOI] [PubMed] [Google Scholar]
- 32. SAS Institute Inc. SAS Statistical Software, Vol 9.2 Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- 33. Laird N, Olivier D. Covariance analysis of censored survival data using log-linear analysis techniques. J Am Stat Assoc. 1981;76:231–240. [Google Scholar]
- 34. Breslow NE. Generalized linear models: checking assumptions and strengthening conclusions. Stat Appl. 1996;8:23–41. [Google Scholar]
- 35. Mortensen PB, Pedersen MG, Pedersen CB. Psychiatric family history and schizophrenia risk in Denmark: which mental disorders are relevant? Psychol Med. 2010;40:201–210. [DOI] [PubMed] [Google Scholar]
- 36. Eaton W, Harrison G. Life chances, life planning, and schizophrenia: a review and interpretation of research on social deprivation. Int J Mental Health. 2001:58–81. [Google Scholar]
- 37. Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–669. [DOI] [PubMed] [Google Scholar]
- 38. Freedman D, Brown AS. The developmental course of executive functioning in schizophrenia. Int J Dev Neurosci. 2011;29:237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Trainor BC. Stress responses and the mesolimbic dopamine system: social contexts and sex differences. Horm Behav. 2011;60:457–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. McCormick CM. An animal model of social instability stress in adolescence and risk for drugs of abuse. Physiol Behav. 2010;99:194–203. [DOI] [PubMed] [Google Scholar]
- 41. Keshavan MS. Development, disease and degeneration in schizophrenia: a unitary pathophysiological model. J Psychiatr Res. 1999;33:513–521. [DOI] [PubMed] [Google Scholar]
- 42. Giovanoli S, Engler H, Engler A, et al. Stress in puberty unmasks latent neuropathological consequences of prenatal immune activation in mice. Science. 2013;339:1095–1099. [DOI] [PubMed] [Google Scholar]
- 43. Zammit S, Owen MJ, Lewis G. Misconceptions about gene-environment interactions in psychiatry. Evid Based Ment Health. 2010;13:65–68. [DOI] [PubMed] [Google Scholar]
- 44. Dong M, Anda RF, Felitti VJ, et al Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Arch Pediatr Adolesc Med. 2005;159:1104–1110. [DOI] [PubMed] [Google Scholar]
- 45. Salas M, Hotman A, Stricker BH. Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol. 1999;149:981–983. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.