Abstract
Objective: Life expectancy in individuals with schizophrenia continues to increase. It is not clear whether cognitive deficits associated with schizophrenia remain as strong predictors of function in older and younger individuals. Thus, we assessed the relationship between cognition and functional competence in individuals with schizophrenia across 7 decades of life. Methods: We analyzed data obtained in 232 community-dwelling participants with schizophrenia (age range: 19–79 years). Cognition was assessed using the Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery. Functional competence was assessed using the UCSD Performance-based Skills Assessment, which includes measures of Comprehension and Planning of Recreational Activities Skills, Financial Skills, Communication Skills, Transportation Skills, and Household Management Skills. To assess the effects of Global Cognition on functional competence, we performed hierarchical multivariate linear or logistic regression analyses controlling for age, education, gender, and negative symptoms. Results: Participants’ mean age was 49.1 (SD = 13.2, range = 19–79 years), 161 (69%) were male, and 55 (24%) were aged ≥60. Global Cognition was a predictor of Comprehension and Planning Skills (Exp(β) = 1.048), Financial Skills (Exp(β) = 1.104), Communication Skills (ΔR 2 = .31) and Transportation Skills (Exp(β) = 1.066), but not Household Management Skills after adjusting for age, education, gender, and negative symptoms of schizophrenia. Conclusion: Cognition remains a strong predictor of functional competence across the lifespan. These findings suggest that treating cognitive impairment associated with schizophrenia could improve individuals’ function independent of their age.
Key words: aging, cognition, functional, competence, lifespan, schizophrenia
Introduction
Schizophrenia is one of the most disabling mental illnesses1,2: the Global Burden of Disease study lists schizophrenia as the eighth leading cause of disability.3 Disability associated with schizophrenia is due to functional impairments that span multiple domains including independent living,4–8 social functioning,9–11 and vocational abilities.5,12 As such, these impairments have a tremendous personal and economic impact.13–15 Functional abilities are also affected by the normal aging process.16 For example, older healthy individuals are slower in completing instrumental activities of daily life.17 Thus, as the population of individuals with schizophrenia grows older,18–20 understanding the interactions between schizophrenia and aging on functional abilities could provide an opportunity to better design age-sensitive interventions for remediation of functional impairments.
Among young and middle-aged individuals with schizophrenia, cognitive deficits are consistently among the strongest predictors of functional outcomes.21–26 Cognitive deficits associated with schizophrenia persist into late life and seem to progress at similar rates as those observed among older healthy individuals.27,28 However, it is not known whether the cognitive deficits associated with schizophrenia impact functional abilities independent of aging and, to the same extent, across the lifespan.
Real-world functioning is determined not only by schizophrenia or aging-related factors, but also by environmental factors.29 Hence, assessing functional competence in a laboratory setting allows for understanding the impact of the illness and aging on function without the confounding effect of the environment.6,30–34 Currently, no studies have assessed the relationship between cognition and functional competence in patients with schizophrenia across the lifespan.
Several publications reported significant correlations between cognition and functional competence in older individuals with schizophrenia.4,6,24,25,32,35–40 Some of these publications4,6,25,35–38 included individuals older than 40 years with a mean age in the 50s rather than late-life samples. Other publications focused on individuals older than 50 years.30,32,39,40 However, these latter publications could not assess the relationship between cognition and function across the lifespan because of a narrow age range. One publication30 included a wide age range of individuals with schizophrenia (27–87 years); however, they did not assess the effect of aging on the relationship between cognition and function.
To address this gap in the literature, we analyzed the relationship between cognition and function in participants aged 19–79 years with comparable numbers of individuals aged <40, 40–49, 50–59, and ≥60 years. We used the University of San Diego Performance-Based Skills Assessment (UPSA)6 to assess functional competence and a comprehensive neuropsychological assessment using the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS)—Consensus Cognitive Battery (MCCB).41,42 Our primary hypothesis was that cognition would be a predictor of functional competence across the lifespan even after controlling for age. We also explored whether the relationship between cognition and function changes in strength across the lifespan.
Methods
Participants
Our data were obtained in 59 participants at the Centre for Addiction and Mental Health (CAMH) in Toronto, Canada,28 and 173 participants during the MATRICS Psychometric and Standardization Study (MATRICS PASS).43 These 232 community-dwelling participants’ ages ranged from 19 to 79 years. The numbers of participants were: 51, aged <40 years; 56, aged 40–49 years; 70, aged 50–59 years; and 55 aged ≥60 years.
Eligibility criteria for the CAMH participants were (1) age ≥50 years; (2) meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) TR criteria for a current diagnosis of schizophrenia or schizoaffective disorder; (3) clinically stable as operationalized by (a) not having been hospitalized within 3 months and (b) having had no change in antipsychotic medication dosage within 4 weeks prior to assessment; (4) ability and willingness to speak English; (5) corrected hearing and visual acuity; (6) ability and willingness to provide written informed consent; (7) not meeting criteria for a cognitive disorder secondary to a neurological disease or brain injury; (8) Mini-Mental State Examination (MMSE)44 score of ≥18 years because individuals with very low MMSE scores are unlikely to be able to complete a neuropsychological battery such as the MCCB; (9) not having a current major depressive or manic episode; (10) no alcohol or other substance abuse within the past 6 months; and (11) no electroconvulsive therapy within 6 months prior to assessment.28
Eligibility criteria for the MATRICS PASS participants were comparable to those for CAMH participants except for age: MATRICS PASS included individuals aged 18–65 years.43 All participants signed a written informed consent approved by the local ethics board.
Measures
Clinical Symptoms.
We confirmed the diagnosis with the Structured Clinical Interview for DSM-IV Disorders.45 We assessed the severity of clinical symptoms with the Positive And Negative Syndrome Scale (PANSS)46 in CAMH participants and with the Brief Psychiatric Rating Scale—Extended Version (BPRS-E)47 in MATRICS PASS participants. Given that negative symptoms are strong predictors of function in individuals with schizophrenia,48,49 we included a negative symptoms score based on the negative symptoms shared by the PANSS and BPRS-E (ie, blunted affect, uncooperativeness, emotional withdrawal, motor retardation, and disorientation).
Cognition.
We assessed cognitive performance with the MCCB. The MCCB consists of 10 neuropsychological tests that assess 7 cognitive domains: Attention/Vigilance (Continuous Performance Test-Identical Pairs); Speed of processing (Digit-Symbol-Coding, Category Fluency Test, Trail Making Test—Part A); Social cognition (Mayer-Salovey-Caruso Emotional Intelligence Test: Managing Emotions); Working memory (Visual Memory Spatial Span, Letter-Number Span); Verbal learning (Hopkins Verbal Learning Test-Revised); Visual learning (Brief Visuospatial Memory Test-Revised); and Reasoning and problem solving (Mazes). The MCCB was developed to capture change in separate cognitive domains in clinical trials of cognitive enhancement in schizophrenia.41–43 In this analysis, we generated a composite T-score of Global Cognition by weighing the 7 cognitive domains equally (mean = 50, SD = 10). To do so, we standardized each cognitive test based on a sample of 333 community-dwelling age and sex-matched healthy individuals.28 Then, we standardized the sums of the T-scores for the tests comprising each cognitive domain. These 333 healthy individuals were recruited at CAMH or in MATRICS PASS at the same time as the recruitment of the participants with schizophrenia. At CAMH, Master’s level psychometrists administered the MCCB supervised by a senior neuropsychologist (M.A.B.).
Function.
We assessed participants’ functional competence with the UPSA.6,50 The UPSA is a functional competence measure that was developed specifically to assess functional competence in individuals with schizophrenia. It assesses competence to comprehend and plan recreational activities, manage finances, communicate, use public transportation, and manage household chores. At CAMH, a research nurse administered the UPSA, supervised by one of the investigators (T.K.R.).
Data Analysis.
First, we performed descriptive analyses and reported on the demographic, clinical, cognitive, and functional variables. We checked the functional measures (Comprehension and Planning of Recreational Activities Skills, Financial Skills, Communication Skills, Transportation Skills, and Household Management Skills) for normality of distribution. If the data were not found to be normally distributed, we performed a binary classification of the outcome variables using the median as the cut-off score. Second, we performed univariate linear or logistic regression analyses between Global Cognition and each functional measure. Third, to assess the impact of Global Cognition on functional competence after controlling for other predictors, we performed multivariate linear or logistic regression analyses that included, in addition to Global Cognition, age or age + age2 where the best-fitted model was quadratic, education, gender, and negative symptoms scores. Finally, we centered the variables of age and Global Cognition and included the interaction term age × Global Cognition or (age + age2) × Global Cognition in the multivariate regression analyses, to assess whether age moderates the relationship between cognition and function. We conducted all analyses using SPSS Version 21.0.51
Results
Demographic, Clinical, Cognitive, and Functional Characteristics
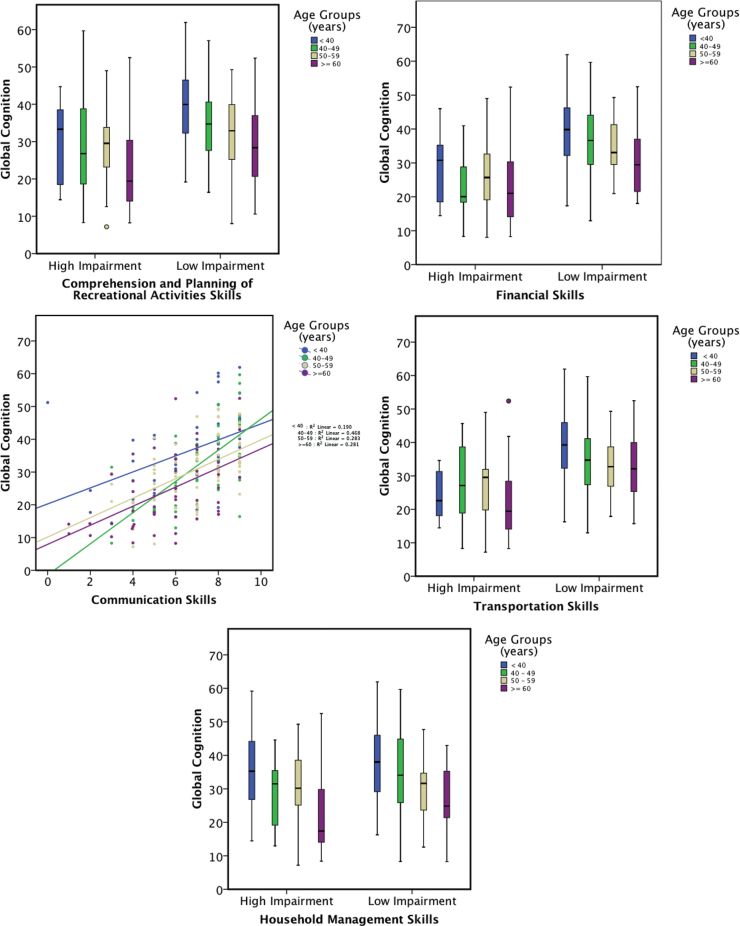
Table 1 shows demographic, clinical, cognitive, and functional characteristics of participants from CAMH and MATRICS PASS. Figure 1 illustrates the relationships between Global Cognition (T-scores) and each of the 5 functional measures of the UPSA within each of the 4 age groups: <40, 40–49, 50–59, ≥60 years.
Table 1.
Demographic, Clinical, Cognitive and Functional Characteristics
| Total | |
|---|---|
| Number of participants (N) | 232 |
| Age (years) | |
| Range | 19–79 |
| Mean (SD) | 49.1 (13.2) |
| Female, N (%) | 71 (31%) |
| Years of education, mean (SD) | 12 (3) |
| Ethnicity, N (%) | 148 (64%) |
| Caucasian African Descent | 57 (25%) |
| Hispanic/Latino | 11 (5%) |
| Asian or Pacific Islander | 8 (3%) |
| Native American/Canadian or Alaskan | 1 (<1%) |
| Other | 7 (3%) |
| Negative symptoms score, mean (SD) | 8.34 (3.12) |
| Global Cognition (MCCB)a, mean T-score (SD) | 30.9 (11.9) |
| UPSA functional domains scores (range of score) mean (SD) | |
| Communication (0–9) | 6.6 (2.0) |
| Finances (0–11) | 9.8 (1.6) |
| Comprehension and Planning of Recreational Activities (0–14)b | 10.6 (2.9) |
| Transportation (0–6) | 5.2 (1.3) |
| Household chores (0–4) | 3.3 (0.9) |
Note: MATRICS PASS, Measurement and Treatment Research to Improve Cognition in Schizophrenia Psychometric and Standardization Study; UPSA, University of California San Diego Performance-Based Skills Assessment.
aComposite score of the MATRICS Consensus Cognitive Battery.
bOnly the data from the second role-play scenario (trip to the zoo) was used in this analysis as it was the only one administered in MATRICS PASS.
Fig. 1.
Relationships between Global Cognition and Functional Measures. This figure illustrates that irrespective of age, individuals with schizophrenia with low impairments in Comprehension and Planning of Recreational Activities Skills, Financial Skills, Communication Skills, and Transportation Skills have higher performance in Global Cognition. This relationship is comparable across the 4 age groups. In contrast, individuals with low impairments in Household Management Skills do not have higher Global Cognition when compared with those who are highly impaired (see the main text for statistical analyses). Circles in the box plots figures refer to outliers.
Relationship Between Global Cognition and Functional Measures
Data on Comprehension and Planning of Recreational Activities Skills, Financial Skills, Transportation Skills, and Household Management Skills were not normally distributed. Thus, we performed a binary classification as described in what follows.
Data on Comprehension and Planning of Recreational Activities Skills were skewed, with a median score of 11 out of 14. We chose a score of ≥12 (48.3%) to indicate low impairment, and a score of ≤11 (51.7%) to indicate high impairment. Univariate logistic regression analysis revealed that Global Cognition alone is a significant predictor of Comprehension and Planning of Recreational Activities Skills (β = .063, SE = 0.013, Wald = 22.496, df = 1, p <.001, Exp(β) = 1.065). After adding age + age2, education, gender, and negative symptoms score as independent variables in a multivariate logistic regression analysis, Global Cognition remained a significant predictor of Comprehension and Planning (β = .047, S E = 0.015, Wald = 9.378, df = 1, p =.002, Exp(β) = 1.048). Education (β = .154, S E = 0.064, Wald = 5.827, df = 1, p = .016, Exp(β) = 1.166) and gender (β = −.820, S E = 0.344, Wald = 5.681, df = 1, p = .017, Exp(β) = 0.440) were significant predictors whereas negative symptoms did not contribute significantly to variation in Comprehension and Planning of Recreational Activities Skills. The variable age + age2 was a significant predictor of this functional measure; however, its effect size was almost null (β < .001, S E < 0.001, Wald = 9.161, df = 1, p = .002, Exp(β) = 1.000). The inclusion of the interaction term (age + age2) × Global Cognition in this regression analysis did not contribute significantly to variation in Comprehension and Planning of Recreational Activities Skills.
Data on Financial Skills were negatively skewed, with a median score of 11 out of 11. We chose a score of 11 (51.1%) to indicate low impairment and a score of ≤10 (48.9%) to indicate high impairment. Univariate logistic regression analysis revealed that Global Cognition alone is a predictor of Financial Skills (β = .111, S E = 0.017, Wald = 43.373, df = 1, p <.001, Exp(β) = 1.117). After adding age + age2, education, gender, and negative symptoms score, Global Cognition remained a significant predictor of Financial Skills (β = .095, S E = 0.019, Wald = 25.967, df = 1, p <.001, Exp(β) = 1.100). Age + age2 (β = −.001, S E < 0.001, Wald = 12.308, df = 1, p < .001, Exp(β) = 0.999) was also a significant predictor. Education, gender, and negative symptoms did not contribute significantly to variation in Financial Skills. The inclusion of the interaction term (age + age2) × Global Cognition in this regression analysis did not contribute significantly to variation in Financial Skills.
Data on Communication Skills were normally distributed. Univariate linear regression analysis revealed that Global Cognition was a significant predictor of Communication Skills (R = .561, Adjusted R 2 = .311, β = .093, S E = 0.009, standardized β = .561, t = 10.019, p <.001). After adding age + age2, education, gender, and negative symptoms score as independent variables in a multivariate linear regression analysis, Global Cognition remained a significant predictor of Communication Skills (R = .561, R 2 = .314, β = .089, S E = 0.011, standardized β = .535, t = 8.076, p <.001). Age + age2, education, gender, and negative symptoms did not contribute significantly to variation in Communication Skills. The inclusion of the interaction term (age + age2) × Global Cognition did not contribute significantly to variation in Communication Skills.
Data on Transportation Skills were skewed, with a median score of 6 out of 6. We chose a score of 6 (58%) to indicate low impairment, and a score of ≤5 (42%) to indicate high impairment. Global Cognition alone was a significant predictor of Transportation Skills (β = .090, S E = 0.015, Wald = 35.055, df = 1, p < .001, Exp(β) = 1.095). After adding age + age2, education, gender and negative symptoms score, Global Cognition (β = .064, S E = 0.018, Wald = 12.999, df = 1, p <.001, Exp(β) = 1.066), age + age2 (β = −.001, S E < 0.001, Wald = 26.157, df = 1, p <.001, Exp(β) = 0.999), education (β = .133, S E = 0.068, Wald = 3.848, df = 1, p =.05, Exp(β) = 1.143), and gender (β = −.802, S E = 0.381, Wald = 4.437, df = 1, p = .035, Exp(β) = .448) contributed significantly to variation in Transportation Skills, whereas negative symptoms did not. The inclusion of the interaction term (age + age2) × Global Cognition in this regression analysis did not contribute significantly to variation in Transportation Skills.
Data on Household Management Skills were skewed, with a median score of 3 out of 4. We chose a score of 4 (48.3%) to indicate low impairment, and a score of ≤3 (51.7%) to indicate high impairment. Global Cognition alone was a significant predictor of Household Management Skills (β = .026, S E = 0.012, Wald = 4.921, df = 1, p =.027, Exp(β) = 1.026). After adding age, education, gender, and negative symptoms score, age remained the only variable to contribute significantly to variation in Household Management Skills (β = −.024, S E = 0.012, Wald = 3.891, df = 1, p = .049, Exp(β) = 0.976). The inclusion of the interaction term age × Global Cognition in this regression analysis did not contribute significantly to variation in Household Management Skills.
Discussion
To our knowledge, this is the first study that used a life- span approach to examine the relationship between cognition and functional competence in schizophrenia. In our sample of 232 individuals with schizophrenia, aged 19–79 years, Global Cognition as assessed using the composite score of the MCCB was a strong predictor of functional competence after controlling for age on measures of Comprehension and Planning of Recreational Activities Skills, Financial Skills, Communication Skills, and Transportation Skills, but not Household Management Skills.
Across the lifespan and after controlling for age, the strength of the relationship between cognition and function varied between small and large effect sizes depending on the functional domain. Cognition accounted for 31% of variance in communication skills, constituting a large effect size. However, effects sizes were small in the other functional domains: Financial Skills, Comprehension and Planning of Recreational Activities Skills, and Transportation Skills. The sizes of these effects are comparable to what other studies have found among adult and midlife individuals with schizophrenia.21 For example, in a sample of 96 individuals with schizophrenia with a mean age ~40 years, cognition accounted for 28% of variance in total functional competence (total score of UPSA).31 Thus, cognition predicts functional competence in individuals with schizophrenia regardless of age and to a magnitude similar to the magnitude in studies of younger and middle-aged individuals. This is further confirmed by the fact that in our study there was no interaction between age and cognition in the prediction of functional competence. These results suggest that the strength of the relationship between cognition and function does not vary with age.
Focusing on late life, our results suggest that for a 70-year old male individual with schizophrenia with 12 years of formal education performing at 2 SDs below average on global cognition, improving his cognition by 1 SD will result in enhancing his performance on Financial and Transportation Skills to the levels of a male individual in early 60s. Improving his cognition by 1 SD will result in enhancing his performance on Communication and Comprehension and Planning of Recreational Activities by 6–10%.
Several other studies that assessed the relationship between cognition and functional competence in middle-age and older individuals with schizophrenia found an effect of cognition on function.4,6,25,32,35–40 However, they did not assess for an aging effect due to narrow age ranges. In contrast, the lifespan approach and the wide age range in our study allowed us to demonstrate, for the first time, the impact of cognition on functional competence independent of aging effect, as well as the impact of aging on the relationship between cognition and function. Our findings suggest that improving cognition in individuals with schizophrenia is likely to improve function at any age, including late in life.
Although our study found significant associations between cognition and function, the strengths of these associations were moderate. Several factors can explain these moderate associations. One is the fact that some of the cognitive abilities needed for the functional tasks assessed by UPSA are not well captured by MCCB. For example, mental arithmetic52 and visuospatial construction37 are strongly associated with financial competence but not assessed by MCCB. Future studies using a more extensive neuropsychological battery might show stronger associations between cognition and function.
We found a relatively weak aging effect on 4 functional competencies and no effect on the fifth one. This aging effect is consistent with the normal aging effect on these functional competencies.53 It is possible that the effect of aging on functional competencies could be underestimated because we are assessing competence in a laboratory setting rather than real life and, therefore, may not be capturing the effect of aging through medical and physical morbidities.54 In contrast, the effect of aging could also be overestimated due to the fact that older individuals with schizophrenia have had more years of “inexperience” at some of these tasks when compared with younger individuals, rendering them less competent at these tasks than expected. For example, older individuals with schizophrenia might have not written checks (finance) or gone grocery shopping (household chores), or used a map (transportation) for many more years than younger individuals with schizophrenia.
We did not find any significant relationship between negative symptoms and function. However, our finding is limited by the assessment tool used for negative symptoms. In addition, other studies that reported on a relationship between negative symptoms and function using a better scale of negative symptoms found a weak relationship.25
Our study has some further limitations. We assessed participants at various locations and within the contexts of 2 different studies. The participants recruited at CAMH were ≥50 years and constituted the vast majority of the group of participants ˃60 years. This design feature limited our ability to control for a site confounding effect because there were almost no older participants from the MATRICS PASS sites and all CAMH participants were older, ie, site and age were highly correlated. The design of our study is cross-sectional. Thus, our findings are limited by cohort and survival effects. This also limits our ability to conclude on a causal relationship between cognition and function. Although interventions that aimed to improve cognition have improved functional competence,55 we cannot exclude the possibility that improving functional competence may improve cognition. Another limitation is that a recent study found that the MCCB and measures of functional competence (including a brief version of the UPSA) constitute a single latent trait.56 This recent study questions the extent to which these functional measures are capturing behaviors and phenotypes beyond what the cognitive measures are capturing. Finally, some of the UPSA functional measures are correlated. These correlations range from being small and nonsignificant (eg, between Financial and Household Skills) to 0.48 (between Financial and Transportation Skills). One approach would have been to perform factor analysis using our own sample. However, given that our focus was not on the UPSA scale per se, and we were interested in presenting our results in relationship to how UPSA is being administered with its distinct subscales, we chose to present our results for each individual functional measure.
In conclusion, our study is the first to demonstrate a cognitive effect on functional competencies that is independent of aging and that persists across the lifespan. Our results suggest that cognitive enhancement is likely to improve function at all ages among individuals with schizophrenia. Longitudinal studies of cognition and function are needed to characterize the trajectories of these dimensions of the illness especially as the population of individuals with schizophrenia continues to grow older.
Funding
MATRICS initiative through the National Institute of Mental Health at the National Institutes of Health contract (N01MH22006) to the University of California, Los Angeles; Canadian Institutes of Health Research (CIHR 200017 to B.H.M., and CIHR180087 to T.K.R.).
Acknowledgments
The authors would like to acknowledge all participants and their families for their contribution to this work. Dr Butters has received remuneration for providing neuropsychological assessment services for GlaxoSmithKline and received salary support from NIH R01 MH072947 and MH080240. Dr Kern is an officer with MATRICS Assessment, Inc and he receives financial compensation for his role in the nonprofit organization. The other authors report no conflicts of interest.
References
- 1. Strassnig MCR, Newcomer J, Harvey P. Cognitive deficits, obesity and disability in schizophrenia. Transl Neurosci. 2012;3:345–354. [Google Scholar]
- 2. Świtaj P, Anczewska M, Chrostek A, et al. Disability and schizophrenia: a systematic review of experienced psychosocial difficulties. BMC Psychiatr. 2012;12:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nat Med. 1998;4:1241–1243. [DOI] [PubMed] [Google Scholar]
- 4. Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. 2007;33:1364–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Karagianis J, Novick D, Pecenak J, et al. Worldwide-Schizophrenia Outpatient Health Outcomes (W-SOHO): baseline characteristics of pan-regional observational data from more than 17,000 patients. Int J Clin Pract. 2009;63:1578–1588. [DOI] [PubMed] [Google Scholar]
- 6. Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. [DOI] [PubMed] [Google Scholar]
- 7. Bowie CR, Depp C, McGrath JA, et al. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am J Psychiatr. 2010;167:1116–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Perivoliotis D, Granholm E, Patterson TL. Psychosocial functioning on the independent living skills survey in older outpatients with schizophrenia. Schizophr Res. 2004;69:307–316. [DOI] [PubMed] [Google Scholar]
- 9. Green MF, Leitman DI. Social cognition in schizophrenia. Schizophr Bull. 2008;34:670–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Penn DL, Sanna LJ, Roberts DL. Social cognition in schizophrenia: an overview. Schizophr Bull. 2008;34:408–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sparks A, McDonald S, Lino B, O’Donnell M, Green MJ. Social cognition, empathy and functional outcome in schizophrenia. Schizophr Res. 2010;122:172–178. [DOI] [PubMed] [Google Scholar]
- 12. Harvey PD, Heaton RK, Carpenter WT, Jr, et al. Functional impairment in people with schizophrenia: focus on employability and eligibility for disability compensation. Schizophr Res. 2012;140:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cohen C VI, Reyes P, Diwan S, et al. Schizophrenia in later life: clinical symptoms and social well-being. Psychiatr Serv. 2008;59:232–234. [DOI] [PubMed] [Google Scholar]
- 14. Rossler W JSH, van Os J, Riecher-Rossler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15:399–409. [DOI] [PubMed] [Google Scholar]
- 15. Salokangas RK, Honkonen T, Stengård E, Koivisto AM. Subjective life satisfaction and living situations of persons in Finland with long-term schizophrenia. Psychiatr Serv. 2006;57:373–381. [DOI] [PubMed] [Google Scholar]
- 16. Hébert R. Functional decline in old age. CMAJ. 1997;157:1037–1045. [PMC free article] [PubMed] [Google Scholar]
- 17. Owsley C, Sloane M, McGwin G, Jr, Ball K. Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology. 2002;48:254–265. [DOI] [PubMed] [Google Scholar]
- 18. Gilmer T. OV, Folsom D., Fuentes D., et al. Costs of community-based public mental health services for older adults: variations related to age and diagnosis. Int J Geriatr Psychiatry. 2006;21:1121–1126. [DOI] [PubMed] [Google Scholar]
- 19. Goeree R, Farahati F, Burke N, et al. The economic burden of schizophrenia in Canada in 2004. Curr Med Res Opin. 2005;21:2017–2028. [DOI] [PubMed] [Google Scholar]
- 20. Folsom DP, McKibbin C, Jeste DV, Patterson T. Use of primary care and by middle aged and older persons with schizophrenia. Prim Care Community Psychiatr. 2006;11:101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatr. 1996;153:321–330. [DOI] [PubMed] [Google Scholar]
- 22. Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. [DOI] [PubMed] [Google Scholar]
- 23. Bowie CR, Harvey PD. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am. 2005;28:613–6–33, 626. [DOI] [PubMed] [Google Scholar]
- 24. Bowie CR, Harvey PD. Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr Dis Treat. 2006;2:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Evans JD, Heaton RK, Paulsen JS, et al. The relationship of neuropsychological abilities to specific domains of functional capacity in older schizophrenia patients. Biol Psychiatr. 2003;53:422–430. [DOI] [PubMed] [Google Scholar]
- 26. Harvey PD, Penn D. Social cognition: the key factor predicting social outcome in people with schizophrenia? Psychiatry (Edgmont). 2010;7:41–44. [PMC free article] [PubMed] [Google Scholar]
- 27. Rajji TK, Mulsant BH. Nature and course of cognitive function in late-life schizophrenia: a systematic review. Schizophr Res. 2008;102:122–140. [DOI] [PubMed] [Google Scholar]
- 28. Rajji T VA, Butters M, Miranda D, et al. Cognitive performance of individuals with schizophrenia across seven decades: a study using the MATRICS consensus cognitive battery. Am J Geriatr Psychiatr. 2013;21:108–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Patterson T MB. Measurement of functional capacity: a new approach to understanding functional differences and real-world behavioral adaption in those with mental illness. Annu Rev Clin Psychol. 2010;6:139–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatr. 2008;63:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gupta M, Bassett E, Iftene F, Bowie CR. Functional outcomes in schizophrenia: understanding the competence-performance discrepancy. J Psychiatr Res. 2012;46:205–211. [DOI] [PubMed] [Google Scholar]
- 32. Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatr. 2006;163:418–425. [DOI] [PubMed] [Google Scholar]
- 33. Harvey PD. Assessment of everyday functioning in schizophrenia. Innov Clin Neurosci. 2011;8:21–24. [PMC free article] [PubMed] [Google Scholar]
- 34. McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: relevance to persons with schizophrenia. Schizophr Res. 2004;72:53–67. [DOI] [PubMed] [Google Scholar]
- 35. Patterson TKJ, Eastham J, Heaton R, et al. Correlates of functional status in older patients with schizophrenia. Psychiatr Res. 1998;80:41–52. [DOI] [PubMed] [Google Scholar]
- 36. Klapow JC, Evans J, Patterson TL, et al. Direct assessment of functional status in older patients with schizophrenia. Am J Psychiatr. 1997;154:1022–1024. [DOI] [PubMed] [Google Scholar]
- 37. Twamley EDR, Navak G, Palmer B, et al. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatr. 2002;159:2013–2020. [DOI] [PubMed] [Google Scholar]
- 38. Mausbach BT, Bowie CR, Harvey PD, et al. Usefulness of the UCSD performance-based skills assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. J Psychiatr Res. 2008;42:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Harvey PD, Bertisch H, Friedman JI, et al. The course of functional decline in geriatric patients with schizophrenia: cognitive-functional and clinical symptoms as determinants of change. Am J Geriatr Psychiatr. 2003;11:610–619. [DOI] [PubMed] [Google Scholar]
- 40. McClure MM, Bowie CR, Patterson TL, et al. Correlations of functional capacity and neuropsychological performance in older patients with schizophrenia: evidence for specificity of relationships? Schizophr Res. 2007;89:330–338. [DOI] [PubMed] [Google Scholar]
- 41. Nuechterlein KGM, Kern R, Baade L, et al. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatr. 2008;165:203–213. [DOI] [PubMed] [Google Scholar]
- 42. Kern RNK, Green M, Baade L, et al. The MATRICS consensus cognitive battery, part 2: co-norming and standardization. Am J Psychiatr. 2008;165:214–220. [DOI] [PubMed] [Google Scholar]
- 43. Kern RGJ, Dickinson D, Green M, et al. The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res. 2011;126:124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 45. First MB, Pincus HA. The DSM-IV text revision: rationale and potential impact on clinical practice. Psychiatr Serv. 2002;53:288–292. [DOI] [PubMed] [Google Scholar]
- 46. Kay SR, Opler LA, Lindenmayer JP. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res. 1988;23:99–110. [DOI] [PubMed] [Google Scholar]
- 47. Velligan D, Prihoda T, Dennehy E, et al. Brief psychiatric rating scale expanded version: how do new items affect factor structure? Psychiatr Res. 2005;135:217–228. [DOI] [PubMed] [Google Scholar]
- 48. Foussias G, Mann S, Zakzanis KK, et al. Prediction of longitudinal functional outcomes in schizophrenia: the impact of baseline motivational deficits. Schizophr Res. 2011;132:24–27. [DOI] [PubMed] [Google Scholar]
- 49. Foussias G, Mann S, Zakzanis KK, van Reekum R, Remington G. Motivational deficits as the central link to functioning in schizophrenia: a pilot study. Schizophr Res. 2009;115:333–337. [DOI] [PubMed] [Google Scholar]
- 50. Leifker FR, Patterson TL, Bowie CR, Mausbach BT, Harvey PD. Psychometric properties of performance-based measurements of functional capacity: test-retest reliability, practice effects, and potential sensitivity to change. Schizophr Res. 2010;119:246–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. IBM SPSS Statistics for Windows. Version 21.0. Armonk, NY: IBM Corp; 2012. [Google Scholar]
- 52. Sherod MG, Griffith HR, Copeland J, et al. Neurocognitive predictors of financial capacity across the dementia spectrum: normal aging, mild cognitive impairment, and Alzheimer’s disease. J Int Neuropsychol Soc. 2009;15:258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rueda AD. Everyday functioning in cognitively intact elderly: base rate of IADL functioning and comparison to healthy younger adults [dissertation]. Ann Arbor, MI: Clinical Psychology, Washington State University; 2010. [Google Scholar]
- 54. Cohen CI, Cohen GD, Blank K, et al. Schizophrenia and older adults. An overview: directions for research and policy. Am J Geriatr Psychiatr. 2000;8:19–28. [DOI] [PubMed] [Google Scholar]
- 55. Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am J Psychiatr. 2012;169:710–718. [DOI] [PubMed] [Google Scholar]
- 56. Harvey PD, Raykov T, Twamley EW, et al. Factor structure of neurocognition and functional capacity in schizophrenia: a multidimensional examination of temporal stability. J Int Neuropsychol Soc. 2013;19:656–663. [DOI] [PMC free article] [PubMed] [Google Scholar]