Abstract
Background/Objectives
To determine the initial efficacy of a mailed screening and brief intervention to reduce at-risk drinking among persons aged 50 years and older.
Design
Pilot randomized controlled trial.
Setting
UCLA Department of Medicine Community Offices and Primary Care Network. Participants: 86 adults aged 50 years and above who were identified as at-risk drinkers by the Comorbidity Alcohol Risk Evaluation Tool (CARET).
Intervention
Participants were assigned randomly to receive personalized mailed feedback outlining their specific risks associated with alcohol use, an educational booklet on alcohol and aging, and the NIH Rethinking Drinking: Alcohol and Your Health booklet (intervention group) or nothing (control group).
Measurements
Alcohol-related assessments at baseline and at 3 months. CARET assessed at-risk drinking, number of risks, and types of risks.
Results
At 3 months, relative to controls, fewer intervention group participants were: at-risk drinkers (66% versus 88%), binge drinking (45% versus 68%), used alcohol with a medical or psychiatric condition (3% versus 17%) or with symptoms of such a condition (29% versus 49%).
Conclusion
A mailed brief intervention may be an effective approach to intervening with at-risk drinkers aged 50 and older.
Keywords: brief intervention, alcohol, older adults, mailed feedback
INTRODUCTION
The baby boom generation (born 1946–1964) is contributing to explosive growth in the population of adults aged 50 years and older.1. Data from the National Survey on Drug Use and Health, 20122 show 10.4 million people, including 12% of men and 8% of women aged 50 years and older, drink in excess of the low risk drinking limits recommended by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) (e.g., men < 65 years old: >14 drinks per week or 4 drinks on any day; women of all ages and men ≥ 65 years old: >7 drinks per week or 3 drinks on any day).3 Even if the prevalence of unhealthy alcohol use remains stable, this population growth means there will be many more older individuals who consume alcohol at unhealthy levels.
Physiological changes resulting from aging, such as decreases in lean body mass and total body water and increased blood brain barrier permeability and neuronal receptor sensitivity to alcohol, cause older adults to experience higher blood alcohol concentrations and increased impairment compared to younger adults4–5—even at equivalent consumption levels and with less awareness of their impairment6. The most common risks among older drinkers are interactions of alcohol and medications (e.g., antihypertensives, sedatives) and alcohol and comorbid medical or psychiatric conditions and/or their symptoms (e.g., hypertension, insomnia)7. We previously defined unhealthy or at-risk drinking among older adults as the use of alcohol that increases risk for harm, due both to the amount consumed and concurrent use of alcohol with medications and comorbidities8.
Screening and brief interventions (SBI) with unhealthy drinkers in primary care settings have demonstrated efficacy in reducing both alcohol consumption and prevalence of unhealthy drinking9. Among the few studies examining SBI in a primary care setting among older adults, findings generally demonstrate that older adults reduce their drinking when provided with brief advice or feedback about their drinking7, 10–12. Unhealthy drinkers, however, are rarely identified in primary care, resulting in frequent missed opportunities for early identification and brief intervention13.
Interventions that do not rely on in-person interactions (e.g., mail or computer-based) avoid many of the limitations of interventions targeting unhealthy drinking in clinical settings. For example, such interventions may: provide persons who do not regularly participate in the healthcare system access to important health information; offer flexibility of use; allow the user to maintain anonymity, thereby reducing potential stigma; provide a unique opportunity to individually tailor the intervention; and be far less costly than in-person interventions14. Further, postal services provide access for those who do not have access to a computer and the Internet. Studies employing mailed, written, personalized advice have reduced alcohol consumption in problem drinking college students15, 16, employees17, the general population18, 19, and those who visited an emergency department20. Evidence also suggests that unhealthy drinkers are more interested in receiving alcohol-related self-help materials compared to drinkers who drink at low risk levels21.
To our knowledge, no program has intervened with unhealthy or at-risk drinking among primary care patients aged 50 and over by using a standalone mail-based intervention to both recruit and assess participants. This study aimed to test the feasibility and initial efficacy of an entirely mailed SBI, personalized for adults 50 and older that was connected to primary care but not dependent on the participant having an appointment or seeing a primary care provider.
METHODS
Study design
The Comorbidity Alcohol Risk Evaluation (CARE) Study was a small randomized trial testing the feasibility and efficacy of a mailed SBI among unhealthy drinkers aged 50 years and older recruited from a community-based, academic, primary care network. The primary aims of the study were to reduce unhealthy or at-risk drinking and alcohol use at 3 months. The Institutional Review Board of the University of California at Los Angeles approved this study. All enrolled study participants provided written informed consent.
Participants
Between January, 2011 and October, 2012, 3,300 potential participants aged 50 years and older were identified using patient panel data from primary care clinics of 13 participating physicians belonging to the UCLA Department of Medicine Community Offices and Primary Care Network and sent a letter introducing the study as one investigating health behaviors; a survey with questions about fruit and vegetable intake, prescription and non-prescription medication use, exercise habits, and alcohol and tobacco use. Questions on behaviors other than alcohol consumption were used to legitimize alcohol use as a health issue22 and to mask the true purpose of the study to potential participants pre-randomization.
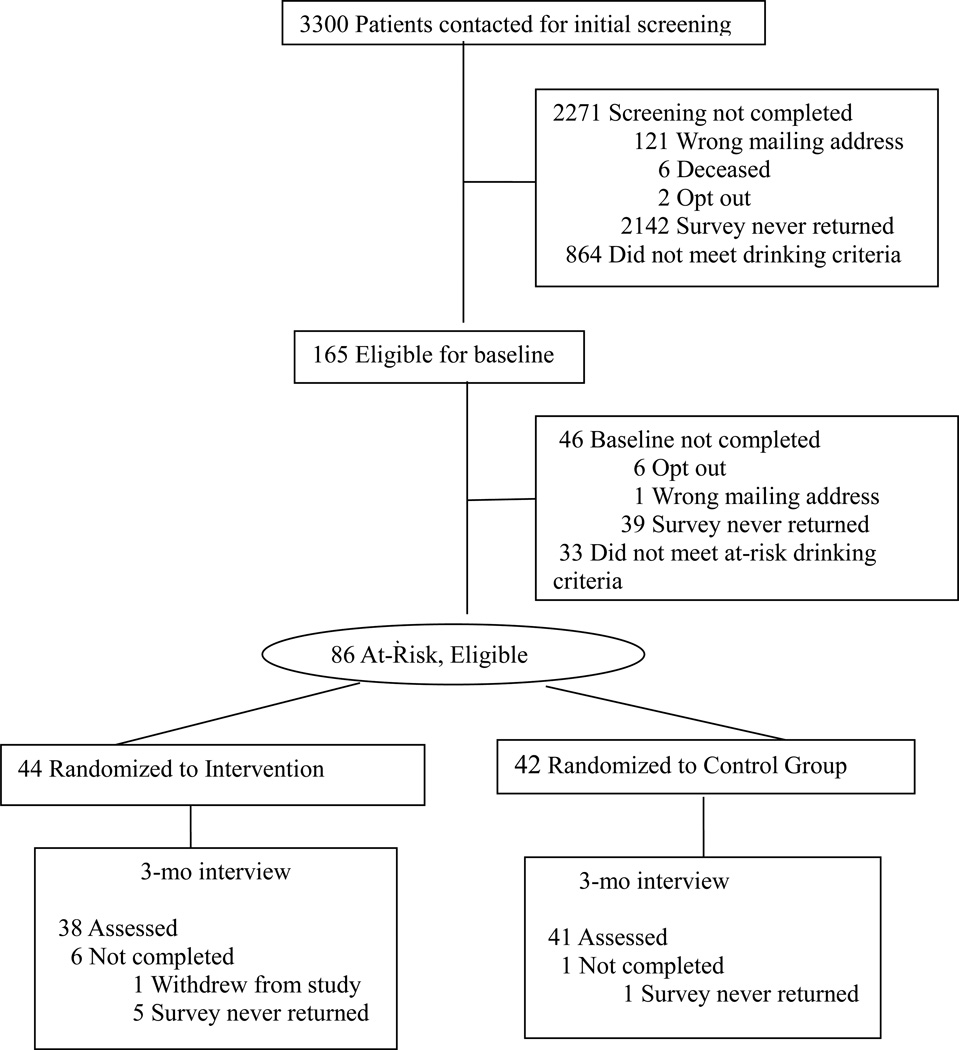
One thousand twenty-nine persons returned the survey (31.2% of those sent surveys) and 165 participants (16.0% of those returning surveys) met drinking criteria (i.e., drank at least 2 drinks, 3–4 times per week; Figure 1). These 165 respondents were sent: a second letter inviting them to participate in a study to test if giving information about healthy behaviors would improve or maintain health; a consent form; and a baseline survey. The survey included items on demographics (i.e., marital status, education completed, occupational status, race/ethnicity, age, and gender) current self-rated health status, and a variety of health behaviors (i.e., frequency and type of exercise, amount of fruits and vegetables consumed). The baseline survey also included the Comorbidity Alcohol Risk Evaluation Tool (CARET), used to identify unhealthy drinkers.7, 12
Figure 1.
Flow of individuals in the Comorbidity Alcohol Risk Evaluation Study
Identification of at-risk drinkers
The CARET includes questions on past 12 month, (a) quantity and frequency of alcohol use, (b) existing co-morbidities and symptoms of medical and psychiatric disorders, and (c) use of medications. Types of risk include: (1) exceeding particular quantity and frequency of drinking (e.g., 3 drinks 4 times per week); (2) binge drinking (>4 drinks on one occasion at least monthly); (3) alcohol use with co-morbid medical or psychiatric condition (e.g., >8 drinks per week with depression or >12 drinks with high blood pressure or diabetes); (4) alcohol use with symptoms of medical or psychiatric conditions (e.g., >4 drinks per week and frequently experiencing problems sleeping, memory problems, stomach pain or vomiting), and (5) alcohol use with medications (e.g., >12 drinks per week and using blood pressure medication; >8 drinks per week and using sedatives, pain medications, nitrate medicines, or blood thinners). For the CARET’s scoring rules, see Ettner et al.12. Responses were scored to designate a potential participant as either an at-risk (score 1–5) or not at-risk drinker (score 0). Not at-risk drinkers were not contacted again.
Randomization and blinding
Identified at-risk drinkers (N=86) were randomly assigned to the intervention (n=44) or control group (n=42). Research staff used consecutively numbered, sealed envelopes containing assignment information using a computer-generated set of random numbers to select permutated blocks of 2 and 4. Within each block, equal numbers were assigned to intervention or control groups..
Control group
Control group participants received a letter informing them the study was testing whether giving information on healthy behaviors would help reduce health risks, $5 gift card, and a reminder that they would be sent a follow-up survey in 3 months.
Intervention group
Intervention group participants received a letter informing them the study was testing whether giving information on healthy behaviors would help them reduce risks associated with alcohol use, a $5 gift card, a personalized feedback report, two alcohol education booklets (i.e., Healthy Drinking as You Age, and the National Institutes of Health Publication, Rethinking Drinking23) and reminder they would be sent a follow-up survey in 3 months. The feedback report outlined participant’s alcohol-related risks from their CARET responses and potential consequences. The Healthy Drinking as You Age booklet included information on recommended drinking limits and risks of combined use of alcohol with medications and comorbid conditions. Both the feedback report and the Healthy Drinking as You Age booklet were used in two prior studies7, 12.
Follow-up
All participants were sent a follow-up survey three months after baseline including questions about health behaviors over the past 3 months and the CARET. Returned surveys were scored to determine risk status. Participants were sent letters informing them of their risk status and all control group participants were informed that the study was testing whether giving information on healthy behaviors would help them reduce risks associated with alcohol use. Control group participants who were no longer at risk were sent the two alcohol education booklets and those who were still at–risk were given a personalized feedback report and the two alcohol education booklets. Intervention group participants who were still at-risk were given another personalized feedback report. All participants received a $10 gift card for completing the follow-up survey. Participant follow-up concluded in April 2013.
Statistical analyses
Participant characteristics are reported for the total sample and by group as frequencies (percentages) and mean and standard deviations (SD). T-tests and Chi Square tests were used to compare groups at baseline for continuous and categorical variables respectively. Among the 86 participants who completed the baseline survey, 79 (91.9%) completed the follow up assessment (Figure 1); 38 respondents (86.4%) of the intervention group and 41 respondents (97.6%) of the control group.
Using data from both time points, analyses were conducted using the LOGISTIC and REG procedures in SAS version 9.3 (SAS Institute, Cary NC, USA). The primary outcomes were at-risk drinker status, CARET risk score; drinks per week; and type of risk. Analysis of covariance models were fit for at-risk drinking status and for each type of risk. Linear regression models were fit for drinks per week and CARET risk score. For all models, baseline values of each of the outcome variables, except for at-risk drinking status were entered as covariates.
RESULTS
Baseline sample characteristics
Respondents had a mean age of just under 65 years, were primarily male (66%), White, non-Hispanic (88%), had graduated college or higher (77%), married (64%), and working full or part-time (64%) (Table 1). More than half of the respondents (56%) reported health status as very good or excellent.
Table 1.
Baseline Participant Characteristics
| Characteristics | Intervention (N=44) |
Control (N=42) |
Total (N=86) |
|---|---|---|---|
| Age, Mean (SD) | 63.2 (7.3) | 66.3 (9.2) | 64.7 (8.4) |
| Male gender | 30 (68) | 27 (64) | 57 (66) |
| Race | |||
| White, non-Hispanic | 37 (84) | 38 (93) | 75 88) |
| Hispanic/Latino | 6 (14) | 2 (5) | 8 (9) |
| Other | 1 (2) | 1 (2) | 2 (2) |
| Education | |||
| High school or less | 5 (11) | 1 (2) | 6 (7) |
| Technical or trade school | 0 (0) | 2 (5) | 2 (3) |
| Some college | 7 (16) | 5 (12) | 12 (14) |
| College degree or more | 32 (73) | 34 (81) | 66 (77) |
| Marital Status | |||
| Married | 31 (70) | 24 (57) | 55 (64) |
| Widowed, divorced, separated, never married | 13 (30) | 18 (43) | 31 (36) |
| Employment Status | |||
| Retired or homemaker | 14 (33) | 17 (40) | 31 (36) |
| Working full or part time | 29 (67) | 25 (60) | 53 (64) |
| Self Reported Health Status | |||
| Excellent or very good | 22 (50) | 26 (63) | 48 (56) |
| Good | 16 (36) | 13 (32) | 29 (34) |
| Fair or poor | 6 (14) | 2 (5) | 8 (9) |
| Alcohol Related Variables | |||
| Drinks per week, mean (SD) | 15.6 (8.8) | 14.4 (7.0) | 15.1 (7.9) |
| CARETa risk score (range 1 to 5), mean (SD) | 2.6 (1.6) | 2.3 (1.3) | 2.4 (1.4) |
| Type of Risk | |||
| Quantity and frequency of drinkingb | 22 (50) | 14 (33) | 36 (42) |
| Binge drinking (4 or more drinks per occasion at least monthly) | 33 (75) | 29 (69) | 62 (72) |
| Alcohol use with medical, psychiatric condition | 12 (27) | 9 (21) | 21 (24) |
| Alcohol use with symptoms | 24 (55) | 19 (45) | 43 (50) |
| Alcohol use with medications | 22 (50) | 26 (62) | 48 (56) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: SD, Standard Deviation.
Comorbidity Risk Evaluation Tool. This tool uses information on the domains described in each type of risk to determine if a respondent is an at-risk or not at-risk drinker. If a respondent meets at-risk criteria for two domains (e.g., they meet at-risk criteria for quantity and frequency of drinking because they report drinking 3 drinks per day 4 times a week, and for alcohol use with medications because they report also regular use of medications for sleep) they have a risk score of 2.
Those meeting the criterion for this risk drink three or more drinks per occasion at least four times a week, four or more drinks per occasion at least twice a week or five or more drinks per occasion at any frequency.
Respondents reported consuming a mean 15.1 drinks (SD = 7.9) per week and had a mean CARET risk score of 2.4 (SD = 1.4). Fifty-five persons (64%) had two categories of risk or more. Most respondents were identified as at-risk drinkers because of binge drinking (72%), followed by alcohol use with medications (56%), alcohol use with symptoms (50%), quantity and frequency of alcohol use (42%) and alcohol use with comorbidities (24%). There were no significant group differences for any baseline variable.
Three Month Outcomes
Table 2 shows descriptives for the three month follow up assessment and results from the ANCOVA and linear regression analyses. The number of drinks per week was reduced for all participants by about two standard drinks, yet there were no significant differences between the groups. CARET risk score was also reduced in both groups, but the intervention group demonstrated a statistically significant reduction compared to those in the control group. To address missing data at the 3-month follow-up we conducted sensitivity analyses using Last-Observation-Carried-Forward (LOCF) method24. These results were similar to those from the base model estimates. (Table 2)
Table 2.
Three Month Outcomes: Descriptives and Model Results
| Descriptives | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Intervention N=38 N(%) |
Control N=41 N (%) |
Total N=79 N(%) |
Base Model Estimates | Estimates from LOCFa | ||
| Alcohol Related Variables |
Beta Coefficient (95%CI) |
p-value |
Beta Coefficient (95%CI) |
p-value | |||
| Drinks per week, mean (SD) | 12.1 (7.0) | 13.5 (6.0) | 12.8 (6.5) | −1.95 (−4.37, +0.46) | 0.11 | −1.18 (−3.57, 1.21) | 0.33 |
| CARET risk score (range 1 to 5), mean (SD) | 1.6 (1.7) | 2.1 (1.4) | 1.9 (1.5) | −0.83 (−1.32, −0.32) | < 0.01 | −0.67 (−1.15, −0.19) | <0.01 |
| Odds Ratio (95% CI) | p-value | Odds Ratio (95% CI) | p-value | ||||
| At-risk drinker | 25 (66) | 36 (88) | 61 (77) | 0.27 (0.09, 0.84) | 0.03 | 0.32 (0.10, 1.00) | 0.05 |
| Type of risk | |||||||
| Quantity and frequency of drinking | 13 (34) | 17 (41) | 30 (38) | 0.39 (0.12, 1.25) | 0.11 | 0.42 (0.14, 1.33) | 0.14 |
| Binge drinking | 17 (45) | 28 (68) | 45 (57) | 0.28 (0.10, 0.79) | 0.02 | 0.33 (0.12, 0.90) | 0.03 |
| Alcohol use with medical, psychiatric condition | 1 (3) | 7 (17) | 8 (10) | 0.08 (0.01, 0.82) | 0.03 | 0.28 (0.06, 1.38) | 0.12 |
| Alcohol use with symptoms | 11 (29) | 20 (49) | 31 (39) | 0.31 (0.11, 0.90) | 0.03 | 0.38 (0.14, 1.07) | 0.07 |
| Alcohol use with medications | 15 (39) | 19 (46) | 34 (43) | 1.14 (0.35, 3.71) | 0.83 | 1.30 (0.41, 4.12) | 0.66 |
Data are presented as No. (%) unless otherwise indicated. Abbreviations: SD, Standard Deviation
Last Observation Carried Forward
Intervention group participants were 73% less likely to be an at-risk drinker compared to control group participants. Only 66% of the intervention group remained at-risk compared to 88% of the control group. Within type of risk, significant differences by condition emerged for binge drinking, alcohol use with a medical or psychiatric condition, and alcohol with symptoms of a medical or psychiatric condition. Intervention group participants were 72% less likely to be an at-risk binge drinker and 92% less likely to be at-risk due to a medical or psychiatric condition. Only one person in the intervention group compared to seven in the control group was at-risk due to alcohol use with a medical or psychiatric condition at follow up. Finally, intervention group participants were 69% less likely to be at-risk due to alcohol use with symptoms.
DISCUSSION
This is the first study to test the feasibility and efficacy of a standalone mailed SBI targeting adult drinkers aged 50 and older enrolled in primary care practices and the first to focus on at-risk or unhealthy drinking, specifically alcohol use that increases risk for harm due to the quantity consumed and/or concurrent use of alcohol with medications and comorbidities. This pilot trial demonstrated that at three months, compared to an assessment-only condition, a mailed SBI targeting a small sample of middle-aged and older at-risk drinkers did not reduce amount of weekly drinking but reduced the prevalence of at-risk drinking compared to the control group. The intervention also reduced the total number of risks and some categories of risk relative to the control group.
Our findings are consistent with studies of mailed SBI implemented with younger samples of drinkers18, 19, 25, as well as studies of more intensive SBI with older adults7, 10–12. Most studies on mailed interventions with younger populations demonstrate that all participants reduce their drinking, but there is a small significant reduction in drinking among participants who receive the intervention compared to a control group18, 19, 25. Among studies of in-person SBI on older adults in primary care settings, all had some degree of success in reducing alcohol use and/or alcohol-related outcomes7, 10–12. These studies differed from the current study in their much greater intensity of intervention, and all included some physician contact.
Limitations of the current study are primarily due to its being a pilot study. The sample size was small, indicating results should be interpreted with caution; however, the intent of this study was to gather data on initial efficacy and feasibility to plan for a larger study. In addition, similar to other studies among older adults in primary care7, 10–11, the sample was primarily Caucasian, male, well educated and in good health, thus limiting generalizability to other populations. Finally, the response rate to the initial screening survey was only 31%, however, this may still be a reasonable response rate as, unlike any of the other mailed interventions, no pre-screening aside from identifying those aged 50 years and older was conducted to identify potential respondents.
Overall, findings suggest that a standalone mail-based intervention may be an efficacious intervention with at-risk drinking older adults and potentially address some of the limitations of in-person SBI. While it is increasingly recognized that older adults should be routinely screened for alcohol misuse26, screening and subsequent identification of risky alcohol use are hampered by limited time in the office; potential discomfort among patients and providers assessing for unhealthy alcohol use; the similarities of symptoms of alcohol misuse with other illnesses common in later life; or that symptoms experienced by use of alcohol are a part of normal aging rather than resulting from the substance use itself27. A mail based intervention takes advantage of the relative anonymity of intervening outside the medical office and can intervene for those who may not otherwise come in for a visit, or may not choose to discuss drinking directly with their physician.
Future studies of standalone mailed brief interventions among older adult at-risk drinkers need to be done to confirm this small study’s preliminary and promising findings. Other studies should also address substances beyond alcohol, such as misuse of prescription pain medications or illegal drugs, particularly given the level of use of such substances among the Baby Boom generation28–29.
ACKNOWLEDGMENTS
This study was supported with funding from the National Institute on Alcohol Abuse and Alcoholism (K24 AA15957) and from the National Institute of Aging (P30AG10415 and P30AG028748).
Additional Contributions: We gratefully acknowledge the patients and clinicians at UCLA Healthcare without whom this study could not have been completed.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: All authors contributed to this paper.
Sponsor’s Role: None
REFERENCES
- 1.U.S. Census Bureau. Population profile of the United States. 2012. [Google Scholar]
- 2.Blazer DG, Wu L. The epidemiology of at risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. Am J Psychiat. 2009;166:1162–1169. doi: 10.1176/appi.ajp.2009.09010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Health & Human Services. Helping patients who drink too much: A clinician's guide. In: Services USDoHH, editor. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health; 2005. [Google Scholar]
- 4.Gilbertson R, Ceballos NA, Prather R, et al. Effects of acute alcohol consumption in older and younger adults: Perceived impairment versus psychomotor performance. J Stud Alcohol Drugs. 2009;70:242–252. doi: 10.15288/jsad.2009.70.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sklar AR, Gilbertson R, Boissoneault J, Nixon SJ, et al. Differential effects of moderate alcohol consumption on performance among older and younger adults. Alcohol Clin Exp Res. 2012;36:2150–2156. doi: 10.1111/j.1530-0277.2012.01833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blow FC, Barry KL. Older patients with at-risk and problem drinking patterns: New developments in brief interventions. J Geriatr Psychiat Neurol. 2000;13:115–123. doi: 10.1177/089198870001300304. [DOI] [PubMed] [Google Scholar]
- 7.Moore AA, Blow FC, Hoffing M, et al. Primary care-based intervention to reduce at-risk drinking in older adults: A randomized controlled trial. Addiction. 2011;106:111–120. doi: 10.1111/j.1360-0443.2010.03229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore AA, Morton SC, Beck JC, et al. A new paradigm for alcohol use in older persons. Med Care. 1999;37:165–179. doi: 10.1097/00005650-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Kaner E, Dickinson HO, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: A systematic review. Drug Alcohol Rev. 2009;28:301–323. doi: 10.1111/j.1465-3362.2009.00071.x. [DOI] [PubMed] [Google Scholar]
- 10.Fleming MF, Manwell LB, Barry KL, et al. Brief physician advice for alcohol problems in older adults: A randomized community-based trial. J Fam Pract. 1999;48:378–384. [PubMed] [Google Scholar]
- 11.Fink A, Elliot MN, Tsai M, et al. An evaluation of an intervention to assist primary care physicians in screening and educating older patients who use alcohol. J Am Geriatr Soc. 2005;53:1937–1943. doi: 10.1111/j.1532-5415.2005.00476.x. [DOI] [PubMed] [Google Scholar]
- 12.Ettner SL, Xu H, Duru OK, et al. The effect of an educational intervention on alcohol consumption, at-risk drinking, and health care utilization among older adults in primary care: The Project SHARE Study. J Stud Alcohol Drugs. 2014;75:447–457. doi: 10.15288/jsad.2014.75.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seppa K, Aalto M, Raevaara L, et al. A brief intervention for risky drinking-analysis of videotaped consultations in primary health care. Drug and Alcohol Rev. 2004;23:167–170. doi: 10.1080/09595230410001704145. [DOI] [PubMed] [Google Scholar]
- 14.Kavanagh DJ, Proctor DM. The role of assisted self-help in services for alcohol-related disorders. Addict Behav. 2011;36:642–629. doi: 10.1016/j.addbeh.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Agostinelli G, Brown JM, Miller WR. Effects of normative feedback on consumption among heavy drinking college students. J Drug Educ. 1995;25:31–40. doi: 10.2190/XD56-D6WR-7195-EAL3. [DOI] [PubMed] [Google Scholar]
- 16.Walters ST, Bennett ME, Miller JH. Reducing alcohol use in college students: A controlled trial of two brief interventions. J Drug Educ. 2000;30:361–372. doi: 10.2190/JHML-0JPD-YE7L-14CT. [DOI] [PubMed] [Google Scholar]
- 17.Walters ST, Woodhall WG. Mailed feedback reduces consumption among moderate drinkers who are employed. Prev Sci. 2003;4:287–294. doi: 10.1023/a:1026024400450. [DOI] [PubMed] [Google Scholar]
- 18.Wild TC, Cunningham JA, Roberts AB. Controlled study of brief personalized assessment-feedback for drinkers interested in self-help. Addiction. 2007;102:241–250. doi: 10.1111/j.1360-0443.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 19.Kavanagh DJ, Connolly JM. Mailed treatment to augment primary care for alcohol disorders: A randomized controlled trial. Drug Alcohol Rev. 2009;28:73–80. doi: 10.1111/j.1465-3362.2008.00011.x. [DOI] [PubMed] [Google Scholar]
- 20.Havard A, Shakeshaft AP, Conigrave KM, et al. Randomized controlled trial of mailed personalized feedback for problem drinkers in the emergency department: The short-term impact. Alcohol Clin Exp Res. 2012;36:523–531. doi: 10.1111/j.1530-0277.2011.01632.x. [DOI] [PubMed] [Google Scholar]
- 21.Wild TC, Roberts AB, Cunningham J, et al. Alcohol problems and interest in self-help: A population study of Alberta adults. Can J Public Health. 2004;95:127–132. doi: 10.1007/BF03405780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleming MF, Barry KL. A three-sample test of a masked alcohol screening questionnaire. Alcohol Alcohol. 1991;26:81–91. [PubMed] [Google Scholar]
- 23.National Institute on Alcohol Abuse and Alcoholism. Rethinking Drinking. Bethesda, MD: 2010. NIH Publication No. 13-3770; [Google Scholar]
- 24.Shao J, Shong B. Last observation carry-forward and last observation analysis. Stat Med. 2003;22:2429–2441. doi: 10.1002/sim.1519. [DOI] [PubMed] [Google Scholar]
- 25.Cunningham JA, Neighbors C, Wild C, et al. Ultra-brief intervention for problem drinkers: Results from a randomized controlled trial. PLoS One. 2012;7:e48003. doi: 10.1371/journal.pone.0048003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Institute of Medicine. The mental health and substance use workforce for older adults: In whose hands? Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 27.Kuerbis A, Sacco P, Blazer DG, et al. Substance use in older adults. Clin Geriatr Med. 2014;30:629–654. doi: 10.1016/j.cger.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of national findings. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 29.Han B, Gfroerer JC, Colliver JD, et al. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]