Abstract
Context:
The appropriateness of current reference ranges for thyroid function testing in older adults has been questioned.
Objective:
This study aimed to determine the relationship between thyroid function tests within the euthyroid range and adverse outcomes in older adults not taking thyroid medication.
Design, Setting, and Participants:
US community-dwelling adults years of older (n = 2843) enrolled onto the Cardiovascular Health Study with TSH, free T4 (FT4), and total T3 concentrations in the euthyroid range.
Main Outcome Measures:
Incidence of atrial fibrillation, coronary heart disease, heart failure, hip fracture, dementia, and all-cause death were measured.
Results:
No departures from linearity were detected. Higher TSH was negatively associated (P = .03) and higher FT4 was positively associated (P = .007) with mortality. Higher FT4 was associated with atrial fibrillation (P < .001) and heart failure (P = .004). Compared with the first quartile, individuals with TSH in the fourth quartile had a 9.6 per 1000 person-year lower incidence of dementia (P < .05) and those with FT4 in the fourth quartile had higher incidences of atrial fibrillation, coronary heart disease, heart failure, and mortality (11.0, 8.0, 7.8, and 14.3 per 1000 person-years, respectively, all P < .05). Total T3 was not associated with any outcome.
Conclusions:
Higher TSH and lower FT4 concentrations within the euthyroid range are associated with lower risk of multiple adverse events in older people, including mortality. This suggests tolerance for lower thyroid hormone levels in this age group. Clinical trials are needed to evaluate the risk-benefit profile of new thresholds for initiating treatment and optimal target concentrations for thyroid hormone replacement in older people.
The definition of euthyroid or “normal” thyroid function is based on the 95% confidence interval (CI) of the TSH distribution in a young adult population without thyroid disease. Individuals with TSH concentrations outside the reference range and normal free T4 (FT4) concentrations are labeled as having subclinical hypothyroidism if the TSH concentration is above the reference range or subclinical hyperthyroidism if the TSH concentration is below it. Numerous observational studies have examined the relationship between subclinical thyroid dysfunction and adverse outcomes, using euthyroid individuals as the reference group (1). These studies have shown increased risk of atrial fibrillation (AF), fracture, and dementia in subclinical hyperthyroidism (2–5) and coronary heart disease (CHD) and heart failure in subclinical hypothyroidism, at higher levels of TSH (6, 7).
From a physiologic standpoint, it is likely that there is a continuum of effects across the spectrum of thyroid function, including within the designated euthyroid range. These effects may be opposing and organ specific at different ends of the thyroid function spectrum. For example, higher levels of thyroid hormones may adversely stimulate the heart, increasing the risk of AF, while simultaneously improving metabolism (8). Several large cohort studies have examined, individually, the relationship between thyroid function tests within the euthyroid range and AF (9, 10), CHD (11–13), nonvertebral fracture (14–16), dementia (17–20), and mortality (13, 21–24). What is lacking, and of clinical relevance, is the simultaneous examination of cardiovascular, musculoskeletal, and cognitive outcomes in the same cohort. Furthermore, few longitudinal studies have focused on older individuals, in whom the baseline risk of adverse events is high and mild differences in thyroid function could be the tipping point.
Although TSH is the primary thyroid function test in clinical use, FT4 concentrations have been shown in some analyses to predict adverse events better than TSH concentrations do (18, 19, 22, 25). We sought to examine the relationships, individually, between TSH, FT4, and total T3 concentrations and incident AF, CHD, heart failure, hip fracture, dementia, and total mortality in euthyroid men and women enrolled onto the Cardiovascular Health Study (CHS), a cohort of community-dwelling men and women age 65 years and older.
Materials and Methods
Study participants
CHS is a multicenter, population-based cohort study of risk factors for cardiovascular disease and stroke in older adults (26). The original cohort of 5201 participants was sampled from Medicare eligibility lists of men and women age 65 years and older from four US centers (Forsyth County, North Carolina; Sacramento County, California; Washington County, Maryland; and Allegheny County, Pennsylvania) in 1989–1990. In 1992–1993, 687 additional African-American participants were recruited. To be eligible individuals had to be noninstitutionalized, expecting to remain in the area for 3 years, not in active treatment for cancer, not wheelchair bound at home, not requiring a proxy respondent at entry, and capable of providing medical consent. Eligible household members of the sampled individual were recruited. Institutional review boards at all four sites and the coordinating center at the University of Washington approved the study. All participants gave written informed consent.
Annual study visits through 1999 included a detailed medical history, examination of medication bottles, physical examination, and assessment of health status. Blood was stored in −70°C freezers for future testing. Participants have been contacted semiannually (by phone or in-person at study visits) regarding hospitalizations or new occurrences of cardiovascular events since the study's inception. When a participant reports a hospitalization or cardiovascular event, the field center obtains medical records, including discharge abstracts, for endpoint assessments. Greater than 90% of participants were retained through the end of study visits in 1999, and retention remains over 85% in ongoing followup. Additional outcome data have been obtained in all participants, including those lost to followup, using data collected from Centers for Medicare and Medicaid Services (CMS). Ascertainment of mortality is 100%.
Thyroid function measurements
Serum TSH (third generation assay), FT4, total T3, and antithyroid peroxidase antibody concentrations (TPOAb) were measured in 3996 participants in 2010 from banked samples obtained at the 1992–1993 visit. TSH and FT4 can be analyzed reliably in samples stored for up to 23 years (27). Assays were performed at the CHS Central Blood Analysis Laboratory at the University of Vermont using chemiluminescent immunoassays on the Elecsys 2010 analyzer (Roche Diagnostics) as previously described (25). Reference ranges were 0.45–4.5 mU/L for TSH, 9.2–21.8 pmol/L (0.7–1.7 ng/dL) for FT4, 1.3–3.1 nmol/L (85–201 ng/dL) for T3, and at least 37 IU/L for TPOAb positivity.
Outcomes
Atrial fibrillation was determined from annual electrocardiography through 1999; hospital discharge codes 427.3, 427.31, or 427.32; and diagnosis from outpatient or carrier claims from CMS through 2010. Coronary heart disease was defined as the occurrence of angina, myocardial infarction, coronary angioplasty, bypass surgery, or coronary heart death. Provisional CHD and heart failure diagnoses based on interview, review of medical records, and other support documents were reviewed and adjudicated by the study's morbidity and mortality subcommittee (28). A composite cardiovascular outcome was defined as CHD, heart failure, or AF. Diagnoses of hip fractures were ascertained from hospital discharge codes and CMS inpatient data. A committee of neurologists, psychiatrists, and neuropsychologists classified dementia status using data collected at study visits, as defined in the CHS Memory study (29). Information about deaths was obtained through medical records, death certificates, autopsy, and coroner reports. Atrial fibrillation events were considered through June 30, 2009, dementia events through the 1998–1999 visit, and cardiovascular events, hip fractures, and deaths through December 31, 2010.
Statistical analysis
Participants whose endogenous TSH, FT4, and T3 concentrations were all within reference ranges at the 1992–1993 visit were included in analyses. Participants with prevalent disease for a specific outcome were excluded from analyses of the incidence of that outcome. In addition, participants taking bisphosphonates (n = 7) were excluded from the hip fracture models. We created spline plots to explore the shape of the association of each thyroid function test with each outcome and used generalized additive models to test for statistically significant departures from linearity. Incidence rates were calculated for each outcome by quartile of each thyroid test. Cox proportional hazards models were used to assess associations of each thyroid function test with the incidence of each outcome and a composite cardiovascular outcome. Modeling was performed in stages, adjusting for age, sex, race, and initiation of thyroid hormone replacement as a time-dependent covariate in Model 1. Outcome-specific covariates, selected based on prior analyses in the CHS cohort, were added in Model 2. The staged approach was used because many of the traditional outcome-specific covariates could be mediators, rather than confounders, of the association between thyroid function and the outcome, raising concern for potential overadjustment in Model 2. TSH was modeled with and without log transformation; results did not differ, and the untransformed model is presented for greater interpretability. Proportional hazards assumptions were checked using Schoenfeld residuals and no violations were found. All models were tested for interaction with age, sex, and race by examining the statistical significance of interaction terms with a Wald test. Sensitivity analyses were performed excluding participants with positive TPOAb tests, to examine associations in those without autoimmunity. Competing risks analyses were performed for all outcomes except mortality, with death as the competing outcome. Statistical analyses were performed using STATA version 12 (StataCorp LP). Spline plots were prepared using R version 2.13.0 (http://www.r-project.org).
Results
Of 3996 participants with thyroid function testing in 1992–1993, 3264 (82%) were in the euthyroid TSH range. After excluding participants taking thyroid hormone preparations (n = 216), antithyroid medication (n = 1), or amiodarone (n = 0); missing FT4 or T3 measurements (n = 43); or with FT4 or T3 measurements outside the reference range (n = 161), 2843 participants remained for analysis. These euthyroid participants had a mean age of 74.5 years, comprised 56.2% women, and 81.4% were Caucasian race (Table 1). The mean TSH concentration was 2.15 mU/L, FT4 was 15.6 pmol/L (1.2 ng/dL), and total T3 was 1.81 nmol/L (117.8 ng/dL); 7.8% were TPOAb positive.
Table 1.
Characteristics of the Euthyroid Cohort
| Characteristic | Summary |
|---|---|
| Age, y | 74.5 (5.1) |
| Female | 1599 (56.2) |
| Caucasian | 2313 (81.4) |
| Current smoker | 317 (11.2) |
| Any alcohol use | 1288 (45.3) |
| BMI, kg/m2 | 26.8 (4.7) |
| Diabetes | 491 (17.3) |
| Coronary heart disease | 628 (22.1) |
| Heart failure | 137 (4.8) |
| Stroke | 149 (5.2) |
| Atrial fibrillation | 170 (6.0) |
| TPO Ab positive | 217 (7.8) |
| TSH, mU/L | 2.15 (0.97) |
| FT4, pmol/L | 15.6 (2.1) |
| T3, nmol/L | 1.81 (0.29) |
Abbreviation: BMI, body mass index.
n = 2843. Data are mean (sd) or N (%).
Repeat thyroid function tests 2 years later were available in 80% of participants; 95% (2166/2279) remained euthyroid, 1.1% (26/2279) became subclinically hyperthyroid, 3.4% (77/2279) became subclinically hypothyroid, 2 (<1%) became overtly hypothyroid, and eight (<1%) initiated thyroid medication. Through the end of followup, 133 participants (4.7%) initiated thyroid hormone replacement and two initiated antithyroid medication.
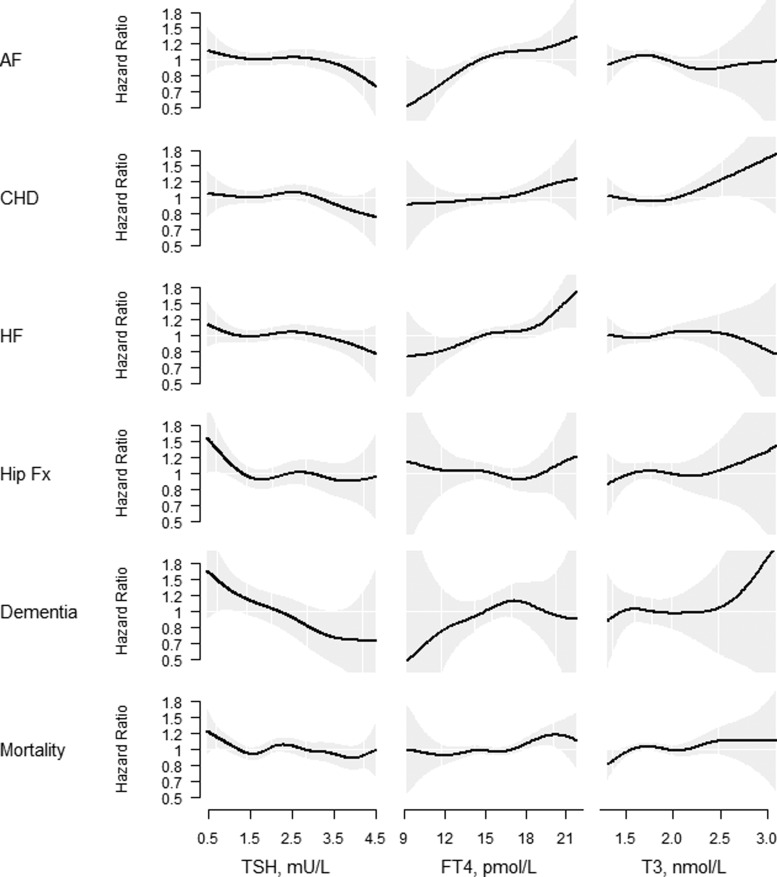
Figure 1 displays the risk of each outcome within the reference range of each thyroid test, adjusted for age, sex, and race. No statistically significant departures from linearity were detected. Over 17 years of followup, 812 participants developed AF. TSH and T3 concentrations were not associated with incident AF, whereas FT4 concentration was (Model 1: hazard ratio [HR], 1.06; 95% CI, 1.03–1.10; P < .001; Model 2: HR, 1.04; 95% CI, 1.01–1.08; P = .02) (Table 2). Incident CHD occurred in 786 participants. No association between any of the thyroid function tests and incident CHD was found. Incident heart failure occurred in 870 participants. TSH and T3 concentrations were not associated with incident heart failure, whereas FT4 concentration was positively associated (Model 1: HR, 1.05; 95% CI, 1.02–1.09; P = .004; Model 2: HR, 1.04; 95% CI, 1.00–1.07; P = .03). TSH concentration was negatively associated (Model 2: HR, 0.94; 95% CI, 0.88–1.00; P = .04) and FT4 concentration positively associated (Model 1: HR, 1.04; 95% CI, 1.01–1.07; P = .008; Model 2: HR, 1.03; 95% CI, 1.00–1.06; P = .02) with a composite measure of cardiovascular disease.
Figure 1.
Spline regression graphs depicting the adjusted associations of continuous concentrations of TSH (left), FT4 (middle), and T3 (right) with incident AF, CHD, heart failure (HF), hip fracture (Hip Fx), dementia, and total mortality. Spline regressions are adjusted for age, sex, and race.
Table 2.
Risk of Atrial Fibrillation, Coronary Heart Disease, Heart Failure, or a Composite Cardiovascular Disease Measure for a One Unit Higher TSH, FT4, or Total T3
| Model | No. of Events/No. at Risk | TSH, mU/L |
Free T4, pmol/L |
Total T3, nmol/L |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | ||
| Atrial fibrillation | 812/2673 | |||||||||
| Model 1 | 0.94 | 0.87–1.01 | .09 | 1.06 | 1.03–1.10 | <.001 | 0.90 | 0.70–1.15 | .40 | |
| Model 2 | 0.94 | 0.87–1.02 | .12 | 1.04 | 1.01–1.08 | .02 | 0.86 | 0.67–1.11 | .24 | |
| Coronary heart disease | 786/2215 | |||||||||
| Model 1 | 0.95 | 0.88–1.03 | .20 | 1.03 | 0.99–1.06 | .13 | 1.23 | 0.97–1.56 | .09 | |
| Model 2 | 0.95 | 0.88–1.02 | .15 | 1.02 | 0.98–1.05 | .28 | 1.13 | 0.89–1.45 | .31 | |
| Heart failure | 870/2706 | |||||||||
| Model 1 | 0.95 | 0.88–1.02 | .17 | 1.05 | 1.02–1.09 | .004 | 1.07 | 0.85–1.35 | .54 | |
| Model 2 | 0.94 | 0.87–1.01 | .09 | 1.04 | 1.00–1.07 | .03 | 1.04 | 0.82–1.32 | .77 | |
| Composite cardiovascular outcome | 1128/2073 | |||||||||
| Model 1 | 0.94 | 0.88–1.00 | .05 | 1.04 | 1.01–1.07 | .008 | 1.09 | 0.89–1.33 | .43 | |
| Model 2 | 0.94 | 0.88–1.00 | .04 | 1.03 | 1.00–1.06 | .02 | 0.97 | 0.79–1.19 | .78 | |
Model 1 for all outcomes is adjusted for age, sex, race and initiation of thyroid meds (time-varying).
Model 2 for atrial fibrillation additionally adjusted for BMI, hypertension, fasting glucose, current smoking, any alcohol use, valvular disease history, and use of any diuretic or β blocker.
Model 2 for coronary heart disease additionally adjusted for BMI, hypertension, diabetes, current smoking, low-density lipoprotein cholesterol, lipid lowering medication use, and C-reactive protein.
Model 2 for heart failure additionally adjusted for BMI, hypertension, diabetes, current smoking, coronary heart disease, atrial fibrillation, stroke, claudication, any alcohol use, and creatinine (natural log).
Model 2 for composite cardiovascular disease outcome additionally adjusted for BMI, hypertension, diabetes, stroke, claudication, current smoking, C-reactive protein, and creatinine.
No association was found between any of the thyroid function tests and hip fracture (340 events) or dementia (229 events) (Table 3). There were a total of 2161 deaths. In Model 1, TSH concentration was negatively associated (HR, 0.95; 95% CI, 0.91–0.99; P = .03) and FT4 concentration was positively associated (HR, 1.03; 95% CI, 1.01–1.05; P = .007) with total mortality. These estimates were no longer statistically significant after additional adjustment (Model 2: HR, 0.96; 95% CI, 0.91–1.00; P = .05 for TSH, and HR, 1.01; 95% CI, 0.99–1.03; P = .17 for FT4).
Table 3.
Risk of Hip Fracture, Dementia, and Total Mortality for a One Unit Higher TSH, FT4, or Total T3
| Model | No. of Events/No. at Risk | TSH, mU/L |
Free T4, pmol/L |
Total T3, nmol/L |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | ||
| Hip fracture | 340/2803 | |||||||||
| Model 1 | 0.93 | 0.83–1.04 | .20 | 0.99 | 0.94–1.05 | .79 | 1.07 | 0.74–1.55 | .73 | |
| Model 2 | 0.94 | 0.84–1.05 | .26 | 0.98 | 0.94–1.04 | .56 | 1.03 | 0.71–1.51 | .86 | |
| Dementia | 229/1824 | |||||||||
| Model 1 | 0.87 | 0.76–1.00 | .05 | 1.04 | 0.97–1.10 | .26 | 1.01 | 0.63–1.59 | .98 | |
| Model 2 | 0.88 | 0.76–1.01 | .07 | 1.02 | 0.96–1.09 | .52 | 1.06 | 0.66–1.68 | .81 | |
| Total Mortality | 2161/2843 | |||||||||
| Model 1 | 0.95 | 0.91–0.99 | .03 | 1.03 | 1.01–1.05 | .007 | 1.12 | 0.97–1.30 | .12 | |
| Model 2 | 0.96 | 0.91–1.00 | .05 | 1.01 | 0.99–1.03 | .17 | 1.12 | 0.96–1.30 | .15 | |
Model 1 for hip fracture and total mortality are adjusted for age, sex, race, and initiation of thyroid meds (time varying). Model 1 for dementia also includes an age2 term.
Model 2 for hip fracture additionally adjusted for oral steroid use, kilocalories of exercise (ln), current smoking, alcohol use, and weight.
Model 2 for dementia additionally adjusted for body mass index (BMI), hypertension, diabetes, current smoking, any alcohol use, total cholesterol, stroke history, claudication, and apoe4 genotype.
Model 2 for mortality additionally adjusted for BMI, hypertension, diabetes, current smoking, coronary heart disease, heart failure, stroke, claudication, depression score, creatinine, and kcal of activity.
There were no interactions between any of the thyroid function tests and sex. Sex-stratified models were examined specifically for hip fracture, which showed similar, nonsignificant results. In the incident heart failure models, there was a significant interaction of 80 years of age or older with FT4 concentration (P = .03) and of race with TSH concentration (P = .01).
For all outcomes with the exception of dementia, results were unchanged in sensitivity analyses excluding individuals who were TPOAb positive (Supplemental Table 1) and in competing risk analyses (Supplemental Table 2). The dementia HR for TSH was 0.84 (95% CI, 0.72–0.98; P = .02) after excluding TPOAb-positive individuals and 0.86 (95% CI, 0.75–0.99; P = .04) in competing risk analyses, suggesting increased risk of dementia at lower TSH concentrations.
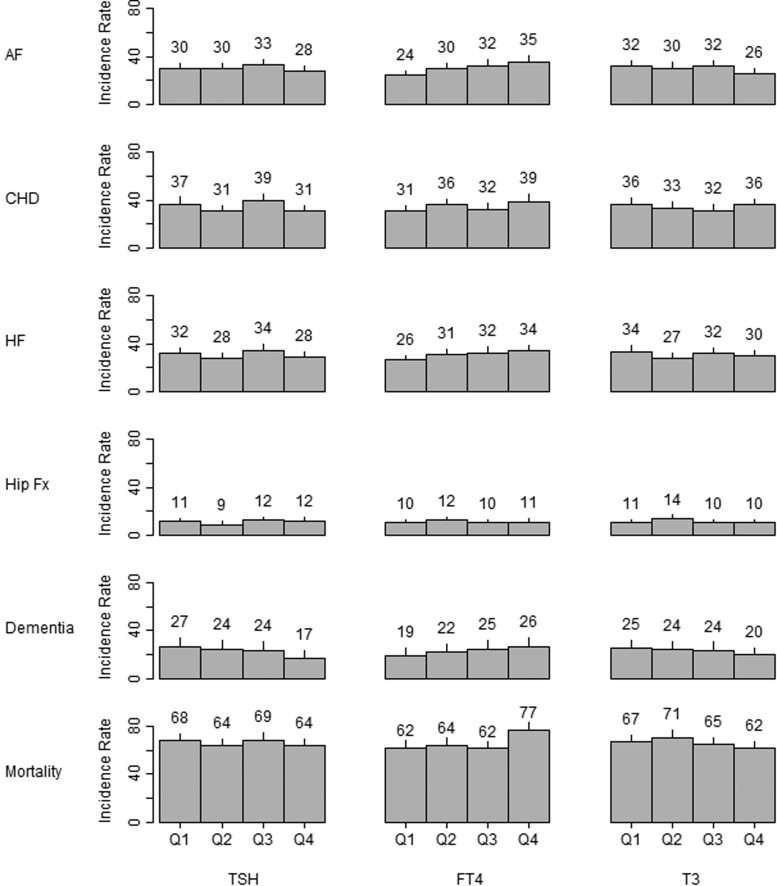
We also examined differences in incidence rates across quartiles within each reference range (Figure 2). Compared with individuals with a FT4 concentration in the first quartile, those with FT4 concentrations in fourth quartile had significantly higher rates of AF (difference of 11.0 per 1000 person years; 95% CI, 5.0–16.9), CHD (difference of 8.0 per 1000 person years; 95% CI, 1.1–15.0), heart failure (difference of 7.8 per 1000 person years; 95% CI, 2.0–13.6), and mortality (difference of 14.3 per 1000 person years; 95% CI, 6.1–22.5) (all P < .05). Incidence rates of hip fracture (difference of 0.5 per 1000 person years; 95% CI, −2.8–3.8) and dementia (difference of 7.0 per 1000 person years; 95% CI, −1.4–15.5) were also higher in quartile 4 vs quartile 1, although these comparisons were not statistically significant. Compared with individuals with TSH concentrations in the first quartile, those with TSH concentrations in the fourth quartile had significantly lower absolute rates of dementia (difference of −9.6 per 1000 person years; 95% CI, −17.9 to −1.2).
Figure 2.
Incidence rates per 1000 person years (95% CI) for incident AF, CHD, heart failure (HF), hip fracture (Hip Fx), dementia, and total mortality by quartile of TSH (left), FT4 (middle), and T3 (right). For TSH, Q1 is 0.45–1.39 mU/L, Q2 is 1.40–2.00 mU/L, Q3 is 2.01–2.82 mU/L, and Q4 is 2.83–4.50 mU/L. For FT4, Q1 is 9.20–14.20 pmol/l (0.70–1.10 ng/dL), Q2 is 14.3–15.6 pmol/L (1.11–1.21 ng/dL), Q3 is 15.7–19.0 pmol/L (1.22–1.48 ng/dL), and Q4 is 19.1–21.8 pmol/L (1.48–1.70 ng/dL). For T3, Q1 is 1.31–1.60 nmol/L (85–104 ng/dL), Q2 is 1.61–1.77 nmol/L (105–115 ng/dL), Q3 is 1.78–1.98 nmol/L (116–129 ng/dL), and Q4 is 1.99–3.10 nmol/L (130–201 ng/dL).
Discussion
We examined the relationship between thyroid function testing within the euthyroid range and outcomes encompassing the cardiovascular, musculoskeletal, and cognitive systems in a cohort of community-dwelling individuals 65 years of age and older. We found increased risk of AF and heart failure at higher concentrations of FT4. In select models, we found increased risk of dementia at lower concentrations of TSH. Lower TSH and higher FT4 concentrations were associated with an increased risk of mortality, although these associations were attenuated after adjustment for covariates that could be in the causal pathway, including hypertension, heart failure, and physical activity. The clinical significance of the reported relative risks is difficult to interpret because they are measured in terms of one unit increments of the assays. However, the absolute risks suggest that these differences have clinical relevance, with clinically meaningful differences in rates of AF, CHD, heart failure, dementia, and total mortality at opposite ends within the reference range.
Thyroid function is generally conceived as having a U-shaped relationship with harmful outcomes, with adverse clinical consequences at hyperthyroid or hypothyroid extremes. In our study population and for levels within the reference range, no U-shaped associations were present. This suggests that there is no optimal set of thyroid function tests within current reference ranges to reflect the euthyroid ideal in this age group.
When modeled as a continuous measure, we detected associations between higher concentrations of FT4 within the euthyroid range and AF and heart failure. In addition, for all outcomes except hip fracture, the point estimate of the effect was greater than one, and incidence rates were highest in the upper part of the reference range, suggesting a consistency of adverse FT4 effects at higher concentrations. Based on negative feedback regulation, relationships between TSH and outcomes would be expected to be inverse to those of FT4. TSH concentration was negatively associated with all the outcomes, although this was not statistically significant across all models. Because of the log-linear relationship between TSH and FT4, minor alterations in FT4 induce larger changes in TSH concentrations. Thus, it would be expected that TSH would be the more sensitive biomarker of thyroid status. However, TSH concentrations reflect pituitary effects of thyroid hormone, which may differ from end-organ effects. It is interesting to note that the TSH association was strongest for the outcome affecting the brain (dementia), whereas the FT4 associations were strongest for outcomes directly involving the heart (AF and heart failure).
In addition, the TSH-T4 setpoint may be altered at older ages, as evidenced by the increase in TSH with increasing age, shown both cross sectionally (30) and longitudinally (25, 31). The mortality data from our study also support a survival advantage in those with higher TSH, suggesting a superimposed survivor effect in the oldest-old. Prescription of levothyroxine has increased, particularly in older individuals with TSH concentrations less than 10 mU/L (32). However, associations between mildly elevated TSH concentrations and clinical outcomes are not detectable when studying populations of older individuals (2, 25, 33–37), leading some researchers to question the benefits of treating mildly elevated TSH concentrations and to advocate for a change in the TSH reference range. Our analyses support shifting the TSH reference range upward and the FT4 reference range downward in older people. However, this is an observational study of endogenous thyroid function, and we did not study the relative benefits of achieving higher TSH targets or lower FT4 targets through intervention. In addition, we did not detect a threshold of risk for any outcome, only linear effects. There is no physiologic reason to select the 95% CI to define the reference range. Basing the reference range on clinical outcomes is a more logical approach. Our data support existing recommendations to monitor older individuals with mild subclinical hypothyroidism without treatment, because the lowest-risk individuals in our analytic sample were those with the highest TSH and/or lowest FT4 concentrations. Our findings also suggest the possibility of using higher target TSH concentrations in older people already using thyroid hormone replacement, as well as the opportunity to study the effects of antithyroid treatment to lower FT4 and raise TSH in older people with higher FT4 and lower TSH concentrations within the reference range.
This report of associations between TSH and FT4 concentrations within the euthyroid range and multiple outcomes in the same cohort of participants allowed the assessment of consistency across measures. Other longitudinal studies of participants not taking thyroid medication and focusing on the euthyroid range have shown concordance with our findings with respect to AF (10), CHD (12, 13), hip fracture (14, 16), dementia (18–20), and mortality (13, 22, 23), although others have reported increased CHD death in women with higher TSH concentrations (11), increased nonvertebral fracture risk in postmenopausal women with lower TSH and higher FT4 and FT3 concentrations (15), and no association between TSH concentration and incident dementia (17) or mortality (21). A large Korean study with a younger study population than ours (mean age, 40 y) reported associations between lower FT4 and FT3 concentrations within the euthyroid range and all-cause mortality, although no relationships with TSH were seen (24).
Although T3 is the direct mediator of thyroid function, we were unable to detect associations between total T3 concentrations and any outcome. Possible explanations include the short half-life of T3, measurement of total instead of FT3 concentrations, or inadequacy of serum T3 as a surrogate for tissue T3 concentrations. Participants had comorbid illnesses, raising the possibility of an effect of nonthyroidal illness on T3 concentrations. However, participants included in this analysis all had T3 concentrations within the euthyroid range. In addition, even if a subset were affected by nonthyroidal illness, there should have been concordance between FT4 and T3 concentrations in the upper ranges for the AF outcome, which was not detected.
Study strengths include the large number of participants with up to 18 years of followup, full set of thyroid function tests, assessment of thyroid medication use longitudinally, wealth of data on covariates, adjudicated events, and robustness in sensitivity models and competing risk analyses. In addition, we were able to demonstrate relative stability in TSH testing, with over 95% remaining euthyroid 2 years later. Use of different reference ranges may have affected our results slightly, although a linear trend was seen throughout the reference range used. The interactions detected in the heart failure models should be interpreted in the setting of multiple testing and require replication. Because extensive testing was required to diagnose dementia, followup for this outcome was limited to the main study years of CHS, and thus had shorter followup than the other outcomes. It is possible that there were higher-risk participants who were excluded due to use of thyroid medication who would have had thyroid function testing in the upper portion of the TSH range without thyroid medication. In addition, our findings may not be generalizable outside of older populations.
Conclusions
These analyses provide physiologic insight into organ-specific events related to mild differences in thyroid function in older people and suggest that higher TSH and lower FT4 concentrations within the euthyroid range are associated with lower risk of multiple adverse events, including mortality. Our findings have implications for the optimal TSH range in older people, which may need to be higher than the currently defined reference ranges. Our findings may also provide a basis for refinement of target thyroid function testing goals in older people who require thyroid hormone replacement.
Acknowledgments
The research reported in this article was supported by Grants R01AG032317 and K24AG042765 from the National Institute on Aging, Contracts HHSN268201200036C, HHSN268200800007C, N01 HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, and Grant HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. Additional support was provided by Grant AG023629 from the National Institute on Aging.
A full list of principal CHS investigators and institutions can be found at https://CHS-NHLBI.org.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- AF
- atrial fibrillation
- CHD
- coronary heart disease
- CHS
- Cardiovascular Health Study
- CI
- confidence interval
- CMS
- Centers for Medicare and Medicaid Services
- HR
- hazard ratio
- TPOAb
- antithyroid peroxidase antibody concentrations.
References
- 1. Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012;379:1142–1154. [DOI] [PubMed] [Google Scholar]
- 2. Cappola AR, Fried LP, Arnold AM, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA. 2006;295:1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Collet TH, Gussekloo J, Bauer DC, et al. Subclinical hyperthyroidism and the risk of coronary heart disease and mortality. Arch Intern Med. 2012;172:799–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bauer DC, Ettinger B, Nevitt MC, Stone KL. Risk for fracture in women with low serum levels of thyroid-stimulating hormone. Ann Intern Med. 2001;134:561–568. [DOI] [PubMed] [Google Scholar]
- 5. Vadiveloo T, Donnan PT, Cochrane L, Leese GP. The thyroid epidemiology, audit, and research study (TEARS): Morbidity in patients with endogenous subclinical hyperthyroidism. J Clin Endocrinol Metab. 2011;96:1344–1351. [DOI] [PubMed] [Google Scholar]
- 6. Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304:1365–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gencer B, Collet TH, Virgini V, et al. Subclinical thyroid dysfunction and the risk of heart failure events: An individual participant data analysis from 6 prospective cohorts. Circulation. 2012;126:1040–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Taylor PN, Razvi S, Pearce SH, Dayan CM. Clinical review: A review of the clinical consequences of variation in thyroid function within the reference range. J Clin Endocrinol Metab. 2013;98:3562–3571. [DOI] [PubMed] [Google Scholar]
- 9. Gammage MD, Parle JV, Holder RL, et al. Association between serum FThyroxine concentration and atrial fibrillation. Arch Intern Med. 2007;167:928–934. [DOI] [PubMed] [Google Scholar]
- 10. Heeringa J, Hoogendoorn EH, van der Deure WM, et al. High-normal thyroid function and risk of atrial fibrillation: The Rotterdam Study. Arch Intern Med. 2008;168:2219–2224. [DOI] [PubMed] [Google Scholar]
- 11. Asvold BO, Bjøro T, Nilsen TI, Gunnell D, Vatten LJ. Thyrotropin levels and risk of fatal coronary heart disease: The Hunt Study. Arch Intern Med. 2008;168:855–860. [DOI] [PubMed] [Google Scholar]
- 12. Asvold BO, Bjøro T, Platou C, Vatten LJ. Thyroid function and the risk of coronary heart disease: 12-year follow-up of the hunt study in norway. Clin Endocrinol (Oxf). 2012;77:911–917. [DOI] [PubMed] [Google Scholar]
- 13. Pereg D, Tirosh A, Elis A, et al. Mortality and coronary heart disease in euthyroid patients. Am J Med. 2012;125:826 e827–e812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Waring AC, Harrison S, Fink HA, et al. A prospective study of thyroid function, bone loss, and fractures in older men: The MrOS study. J Bone Miner Res. 2013;28:472–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Murphy E, Glüer CC, Reid DM, et al. Thyroid function within the upper normal range is associated with reduced bone mineral density and an increased risk of nonvertebral fractures in healthy euthyroid postmenopausal women. J Clin Endocrinol Metab. 2010;95:3173–3181. [DOI] [PubMed] [Google Scholar]
- 16. Leader A, Ayzenfeld RH, Lishner M, Cohen E, Segev D, Hermoni D. Thyrotropin levels within the lower normal range are associated with an increased risk of hip fractures in euthyroid women, but not men, over the age of 65 years. J Clin Endocrinol Metab. 2014;99:2665–2673. [DOI] [PubMed] [Google Scholar]
- 17. Tan ZS, Beiser A, Vasan RS, et al. Thyroid function and the risk of alzheimer disease: The Framingham study. Arch Intern Med. 2008;168:1514–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Jong FJ, Masaki K, Chen H, et al. Thyroid function, the risk of dementia and neuropathologic changes: The Honolulu-Asia Aging Study. Neurobiol Aging. 2009;30:600–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yeap BB, Alfonso H, Chubb SA, et al. Higher FThyroxine levels predict increased incidence of dementia in older men: The Health in Men Study. J Clin Endocrinol Metab. 2012;97:E2230–E2237. [DOI] [PubMed] [Google Scholar]
- 20. Moon JH, Park YJ, Kim TH, et al. Lower-but-normal serum TSH level is associated with the development or progression of cognitive impairment in elderly: Korean Longitudinal Study on Health and Aging (KLOSHA). J Clin Endocrinol Metab. 2014;99:424–432. [DOI] [PubMed] [Google Scholar]
- 21. Waring AC, Harrison S, Samuels MH, et al. Thyroid function and mortality in older men: A prospective study. J Clin Endocrinol Metab. 2012;97:862–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yeap BB, Alfonso H, Hankey GJ, et al. Higher FThyroxine levels are associated with all-cause mortality in euthyroid older men: The Health in Men Study. Eur J Endocrinol. 2013;169:401–408. [DOI] [PubMed] [Google Scholar]
- 23. Ceresini G, Ceda GP, Lauretani F, et al. Thyroid status and 6-year mortality in elderly people living in a mildly iodine-deficient area: The Aging in the Chianti Area Study. J Am Geriatr Soc. 2013;61:868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang Y, Chang Y, Ryu S, et al. Thyroid hormones and mortality risk in euthyroid individuals: The Kangbuk Samsung Health Study. J Clin Endocrinol Metab. 2014;99:2467–2476. [DOI] [PubMed] [Google Scholar]
- 25. Waring AC, Arnold AM, Newman AB, Bùzková P, Hirsch C, Cappola AR. Longitudinal changes in thyroid function in the oldest old and survival: The Cardiovascular Health Study All-stars Study. J Clin Endocrinol Metab. 2012;97:3944–3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: Design and rationale. Ann Epidemiol. 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 27. Männistö T, Surcel HM, Bloigu A, et al. The effect of freezing, thawing, and short- and long-term storage on serum thyrotropin, thyroid hormones, and thyroid autoantibodies: Implications for analyzing samples stored in serum banks. Clin Chem. 2007;53:1986–1987. [DOI] [PubMed] [Google Scholar]
- 28. Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. [DOI] [PubMed] [Google Scholar]
- 29. Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N. Evaluation of dementia in the Cardiovascular Health Cognition Study. Neuroepidemiology. 2003;22:1–12. [DOI] [PubMed] [Google Scholar]
- 30. Surks MI, Hollowell JG. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the us population: Implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab. 2007;92:4575–4582. [DOI] [PubMed] [Google Scholar]
- 31. Bremner AP, Feddema P, Leedman PJ, et al. Age-related changes in thyroid function: A longitudinal study of a community-based cohort. J Clin Endocrinol Metab. 2012;97:1554–1562. [DOI] [PubMed] [Google Scholar]
- 32. Taylor PN, Iqbal A, Minassian C, et al. Falling threshold for treatment of borderline elevated thyrotropin levels-balancing benefits and risks: Evidence from a large community-based study. JAMA Intern Med. 2014;174:32–39. [DOI] [PubMed] [Google Scholar]
- 33. Gussekloo J, van Exel E, de Craen AJ, Meinders AE, Frölich M, Westendorp RG. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004;292:2591–2599. [DOI] [PubMed] [Google Scholar]
- 34. Hyland KA, Arnold AM, Lee JS, Cappola AR. Persistent subclinical hypothyroidism and cardiovascular risk in the elderly: The Cardiovascular Health Study. J Clin Endocrinol Metab. 2013;98:533–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Garin MC, Arnold AM, Lee JS, Tracy RP, Cappola AR. Subclinical hypothyroidism, weight change, and body composition in the elderly: The Cardiovascular Health Study. J Clin Endocrinol Metab. 2014;99:1220–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Garin MC, Arnold AM, Lee JS, Robbins J, Cappola AR. Subclinical thyroid dysfunction and hip fracture and bone mineral density in older adults: The Cardiovascular Health Study. J Clin Endocrinol Metab. 2014;99:2657–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Razvi S, Shakoor A, Vanderpump M, Weaver JU, Pearce SH. The influence of age on the relationship between subclinical hypothyroidism and ischemic heart disease: A metaanalysis. J Clin Endocrinol Metab. 2008;93:2998–3007. [DOI] [PubMed] [Google Scholar]