Abstract
Background & Aims
Non-alcoholic fatty liver disease (NAFLD) was shown to disproportionally affect Hispanic persons. We examined the prevalence of suspected NAFLD in Hispanic/Latino persons with diverse backgrounds.
Methods
We studied the prevalence of suspected NAFLD among 12,133 persons included in The Hispanic Community Health Study/Study of Latinos. We collected data on levels of aminotransferase, metabolic syndrome (defined by National Cholesterol Education Program-Adult Treatment Panel III guidelines), demographics, and health behaviors. Suspected NAFLD was defined based on increased level of aminotransferase in the absence of serologic evidence for common causes of liver disease or excessive alcohol consumption. In multivariate analyses, data were adjusted for metabolic syndrome, age, acculturation, diet, physical activity, sleep, and levels of education and income.
Results
In multivariate analysis, compared to persons of Mexican heritage, persons of Cuban (odds ratio [OR], 0.69; 95% confidence interval [CI], 0.57–0.85), Puerto Rican (OR, 0.67; 95% CI, 0.52–0.87), and Dominican backgrounds (OR, 0.71; 95% CI, 0.54–0.93) had lower rates of suspected NAFLD. Persons of Central American and South American heritage had a similar prevalence of suspected NAFLD compared to persons of Mexican heritage. NAFLD was less common in women than men (OR, 0.49; 95% CI, 0.40–0.60). Suspected NAFLD associated with the metabolic syndrome and all 5 of its components.
Conclusion
Based on an analysis of a large database of health in Latino populations, we found the prevalence of suspected NAFLD among Hispanic/Latino individuals to vary by region of heritage.
Keywords: HCHS/SOL, steatohepatitis, obesity, Hispanic Americans, life style
Background and Aims
Non-alcoholic fatty liver disease (NAFLD) is the most common cause of liver disease in the United States with a prevalence estimate of 30% 1. NAFLD is an umbrella term including both bland steatosis and non-alcoholic steatohepatitis (NASH), with the latter being a pathologic entity consisting of hepatic steatosis and inflammation. Persons with NASH are at risk for progression to cirrhosis 2 hepatocellular carcinoma, and liver disease-related mortality 3. The prevalence of NASH in the US population is estimated to be between 3% to 5% 1. A number of studies have found that Hispanic/Latino individuals, have the highest rate of NAFLD 4–7. NASH may be seen in up to 9.9%–19.4% of Hispanic persons within the United States 6, 7. Public health issues related to obesity such as NAFLD/NASH merit further study in the Hispanic/Latinos population. Hispanic/Latinos represent the largest minority population under the age of 18 in the United States 8, and nearly half of Hispanic youths between the ages of 6–11 years are overweight or obese 9.
NAFLD is a complex disease state resulting from an interplay between genetic, behavioral, and environmental factors. Ethnic differences in NAFLD are likely related to multiple causes 7, 10. For example, Hispanic/Latino persons have the highest rates of abdominal obesity in the US and were found to have a greater prevalence of the patatin-like phospholipase domain-containing protein 3 (PNPLA3) genetic polymorphism, which are both associated with NAFLD 11, 12. Population based differences in insulin resistance and obesity appear important as the histologic features of NAFLD are comparable between Hispanics and non-Hispanics when controlling for these risk factors13, 14. An important shortcoming of studies of NAFLD in Hispanics/Latinos in the US is that they primarily have focused on persons of Mexican American origin 5, 6. Hispanics/Latinos represent a diverse group of individuals who share a common language, but have differences in ancestry and culture. Chronic medical conditions do not necessarily affect all groups of Hispanic/Latinos with the same frequency. For instance, the prevalence and severity of pediatric asthma was found to disproportionally affect Puerto Rican youths 15. Studying Latinos of different heritage provides a means to assess rates of NAFLD in this heterogeneous group and to identify cultural and behavioral correlates of NAFLD in Hispanics/Latinos in the US.
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) was designed to estimate risk factors and the prevalence of chronic diseases among several distinct Hispanic/Latino groups in the US. Using elevated aminotransferase levels in the absence of other common causes of liver disease, this report describes the prevalence of suspected NAFLD by Hispanic/Latino group, as well as age group, which is consistent with a prior analysis of the National Health and Nutrition Examination Survey (NHANES) 6. In addition, the report describes behavioral and environmental factors associated with suspected NAFLD among diverse Hispanic/Latino groups.
Methods
The design and implementation of HCHS/SOL cohort has been described in detail 16. Briefly, HCHS/SOL is a multi-center study of 16,415 Hispanic/Latino adults that includes persons of Mexican, Puerto Rican, Dominican, Cuban, Central American, and South American backgrounds recruited from four US communities (Chicago, Bronx, Miami, and San Diego) from 2008 to 2011. Households in selected census tracts in the study regions were selected by stratified random sampling. Household members were contacted by telephone and home visits. Persons ages 18–74 years who self-identified as being Hispanic/Latino, had no plans to move over a 6 month period, and were able to attend a clinic examination were eligible to participate. Forty-two percent of eligible individuals enrolled in the study. The study was approved by the Institutional Review Board at each participating institution. All participants provided written informed consent.
Participants completed interviews to evaluate demographic data and health behaviors. Physical exams included abdominal girth with patients wearing light clothing, and resting brachial blood pressure was measured three times in a seated position. All blood samples were collected after an eight hour at the beginning of the study visit. Blood samples were handled uniformly and were centrifuged and frozen within 45 minutes of collection. Two food propensity questionnaires using National Cancer Institute method were used to estimate total daily carbohydrate consumption. Total carbohydrate intake was chosen as a dietary measure given associations between carbohydrate intake and inflammatory activity in persons with NAFLD 17, 18. Self-reported physical activity was quantified by combining the intensity of physical activity in metabolic equivalents and the duration of physical activity during work, transport and recreational activity. Alcohol use was determined by a questionnaire asking participants to detail the number of standard drinks of wine, beer and hard liquor consumed per week.
In the current analysis, demographic data consisted of age, gender and Hispanic/Latino background of origin. Education was categorized as <13 years, 13–15 years and >15 years. Health care use was measured as the number of physician visits during the prior 12 months. Acculturation was evaluated by Short Acculturation Scale for Hispanics language subscale. The Short Acculturation Scale for Hispanics language subscale characterizes language use on a 5-point ordinal number scale with a value of 1 for Spanish language only, 2 for Spanish better than English, 3 for both equal, 4 for English better than Spanish and 5 for English only. Household income was divided into <$10,000, $10,000–20,000, $20,001–40,000, $40,001–75,000, and > $75,000 per year.
The metabolic syndrome was defined as abnormal levels of three or more of the following metabolic components in accordance with National Cholesterol Education Program- Adult Treatment Panel III (NCEP-ATP III) criteria: increased waist circumference (>102 cm in men; > 88 cm in women), elevated triglycerides (>150 mg/dl), decreased high density lipoprotein (HDL) [< 40 mg/dl in men; < 50 mg/dl in women), elevated blood pressure (>130/85) and increased fasting glucose (> 110 mg/dl) 19. Diabetes was defined as the use of medication to treat diabetes or the presence of a fasting blood sugar ≥ 126 mg/dl, non-fasting blood sugar ≥ 200 mg/dl, post oral glucose tolerance test blood sugar ≥ 200 mg/dl or glycosylated hemoglobin ≥ 6.5%. Physical activity was compared by quartiles. Sleep habits were evaluated by a questionnaire assessing the quality of sleep over the prior four weeks.
The aminotransferase thresholds for the designation of suspected NAFLD and exclusion criteria used in this study were based on a previous analysis from the NHANES III survey by Clark et al 6. Elevated aminotransferase levels suggestive of NAFLD were defined as either aspartate aminotransferase (AST) >37 IU/mL or alanine aminotransferase (ALT) >40 IU/mL for men and AST or ALT >31 IU/mL for women. Although it is recognized that aminotransferases have limitations in the identification of NAFLD, patterns of ethnic differences in prevalence of NAFLD observed in population based data using aminotransferases6 were confirmed with imaging5 and histologic findings7. Exclusion criteria included missing aminotransferase data, seropositivity for hepatitis C or hepatitis B surface antigen, alcohol consumption > 7 drinks per week in women or > 14 drinks per week in men, and a transferrin saturation greater than 50%.
A total of 4,282 participants were excluded due to seropositivity for hepatitis B or C (n=356), excess alcohol consumption (n=799), elevated transferrin saturation (n=592), missing AST or ALT (n=174), missing data of interest (n=2,000), or the participant did not identify as being a member of one of the six Hispanic/Latino background groups or age >74 (n=361). The most common missing data of interest was income (n=1339), healthcare use (n=217), physical activity (n=117) and dietary carbohydrate (n=111). As such, 12,133 persons comprised the study cohort including 5,208 persons of Mexican heritage, 1,701 persons of Cuban heritage, 1,916 persons of Puerto Rican heritage, 1,083 persons of Dominican heritage, 1,342 persons of Central American heritage and 883 persons of South American heritage.
Statistical Analysis
Reported values (means, prevalence, and odds ratios [ORs]) were weighted to adjust for sampling probability and nonresponse 16, 20, 21. Descriptive characteristics were computed for all participants by sex and Hispanic/Latino background and were age standardized to the 2010 United States population as was previously described 21. Prevalence of elevated aminotransferase levels were calculated by sex and Hispanic/Latino background. The prevalence of suspected NAFLD was stratified by age group, sex, and Hispanic/Latino background. Survey-specific procedures were used to compute 95% confidence intervals to account for the 2-stage sampling design, stratification, and clustering. Comparisons across Hispanic/Latino groups were performed using the overall Wald test.
Logistic regression analyses were used to examine association of demographic, metabolic, and behavioral factors in the SOL cohort and prevalence of suspected NAFLD for men and women separately. All variables were entered into the multivariate analysis. Multivariate analysis was performed with each component of metabolic syndrome analyzed individually. Odds ratio with 95% CIs were computed. All statistical tests were 2-sided at a significance level of 0.05 and performed using SAS version 9.2 (SAS Institute).
Results
The mean age of the study population was 41.7 (41.1, 42.2) years. A majority of subjects were female (54.3%). Baseline characteristics for the study population are presented in Table 1, stratified by background with participants of Mexican background serving as the reference group. Persons of Mexican background were younger than those from each of the other ethnic groups. Higher rates of the metabolic syndrome were seen in persons of Puerto Rican background, and lower rates of the metabolic syndrome were observed in persons with Dominican and South American background. Additional differences were seen in acculturation, health care use, sleep disturbance, carbohydrate consumption and physical activity.
Table 1.
Age Standardized Baseline Characteristics for All Participants and by Hispanic/Latino Background
| Total | Mexica n (N=520 8) |
Cuban (N=1701) |
Puerto Rican (N=1916 ) |
Dominic an (N=1083 ) |
Central Americ an (N=1342 ) |
South American (N=883) |
|
|---|---|---|---|---|---|---|---|
| AGE, mean | 41.7(41.1–42.2) | 38.7(37.9–39.5) | 47.1(46.0–48.2)*** | 43.6(42.5–44.7)*** | 40.5(39.0–41.9)* | 40.3(39.2–41.3)* | 43.0(41.4–44.5)*** |
| Gender (Female %) | 54.3(53.0–55.6) | 56.8(54.6–59.0) | 46.3(43.6–49.0)*** | 53.5(49.9–57.1) | 61.7(58.0–65.5)* | 53.0(49.2–56.8) | 55.0(50.9–59.0) |
| Metabolic syndrome present % | 33.0(31.7–34.3) | 33.5(31.4–35.6) | 33.3(30.8–35.7) | 37.4(33.9–40.9) | 28.6(25.6–31.5)** | 31.9(29.0–34.7) | 24.6(20.9–28.3)*** |
| Waist circumference elevated % | 53.6(52.0–55.2) | 57.3(54.7–59.8) | 49.2(46.3–52.2)*** | 57.4(53.9–60.9) | 53.2(48.5–58.0) | 48.3(44.8–51.8)*** | 39.6(35.2–44.0)*** |
| Body Mass Index (kg/m2), mean | 29.6 (29.4–29.8) | 29.5 (29.1–29.8) | 29.1 (28.7–29.4) | 31.1 (30.6–31.7)*** | 29.9 (29.1–30.7) | 29.2 (28.8–29.5) | 28.2 (27.7–28.7)*** |
| Triglycerides elevated% | 30.1(28.8–31.3) | 32.6(30.6–34.7) | 30.9(28.4–33.4) | 27.0(23.6–30.5)** | 17.4(14.8–19.9)*** | 35.3(32.1–38.5) | 31.3(27.4–35.3) |
| HDL low % | 41.9(40.6–43.3) | 42.5(40.1–45.0) | 41.4(38.7–44.1) | 44.2(40.8–47.7) | 38.7(33.8–43.6) | 43.0(39.8–46.1) | 36.9(32.4–41.4)* |
| Blood pressure elevated % | 9.6(8.8–10.4) | 7.2(6.1–8.4) | 11.2(9.2–13.2)*** | 11.9(10.0–13.7)*** | 13.4(10.6–16.2)*** | 10.2(8.1–12.3)** | 6.9(5.0–8.7) |
| Fasting glucose elevated % | 14.1(13.2–14.9) | 15.3(13.9–16.6) | 11.8(9.8–13.9)** | 17.1(14.8–19.5) | 12.5(10.4–14.6)* | 13.3(11.3–15.3) | 8.3(6.0–10.5)*** |
| Diabetes % | 15.2 (14.4–16.1) | 17.2 (15.7–18.7) | 11.8 (9.9–13.7)*** | 17.1 (15.0–19.3) | 14.9 (12.9–16.9) | 14.6 (12.5–16.8) | 8.5 (6.5–10.5)*** |
| Acculturation(score), mean | 2.2(2.1–2.2) | 2.1(2.0–2.2) | 1.8(1.7–1.9)*** | 3.2(3.1–3.3)*** | 2.0(1.9–2.1)* | 1.7(1.6–1.8)*** | 1.9(1.8–2.0)*** |
| Physician visit, mean | 3.3(3.2–3.4) | 3.1(2.9–3.4) | 3.0(2.6–3.3) | 4.3(3.9–4.7)*** | 4.1(3.7–4.5)*** | 2.5(2.2–2.7)*** | 2.5(2.2–2.8)*** |
| Sleep disturbance, mean | 1.7(1.6–1.7) | 1.6(1.5–1.6) | 1.7(1.6–1.8)*** | 1.9(1.8–2.0)*** | 1.8(1.7–1.9)*** | 1.6(1.5–1.7) | 1.6(1.5–1.7) |
| Total carb, g mean | 255.1(253.1–257.1) | 255.8(253.3–258.2) | 280.3(276.4–284.2)*** | 242.2(237.4–247.0)*** | 221.0(216.7–225.4)*** | 252.2(246.8–257.6) | 261.3(255.8–266.7) |
| Physical activity, min/week, mean | 687.7(657.9–717.4) | 708.6(661.9–755.4) | 556.9(501.3–612.5)*** | 759.7(667.2–852.2) | 708.8(584.5–833.2) | 770.7(688.9–852.5) | 640.4(547.0–733.8) |
p<0.05
p<0.01
p<0.001
The Mexican group was chosen as the reference group in pairwise comparisons
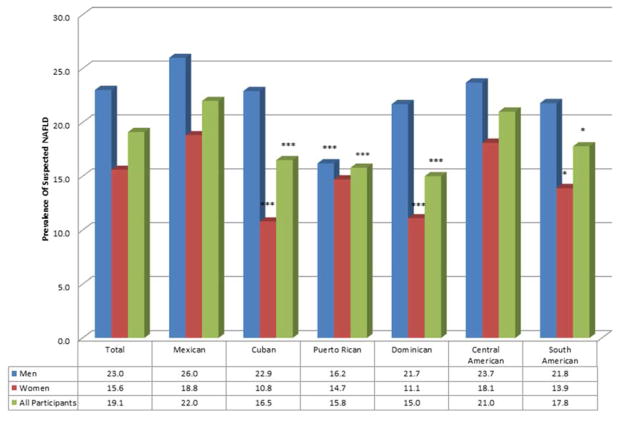
The prevalence of suspected NAFLD by Hispanic/Latino group and gender is shown in Figure 1. Suspected NAFLD was identified in 19.1% of participants overall, and was more common in men (23.2%) compared to women (15.7%, p=<0.001). Considering men and women together, Mexican and Central Americans had the highest prevalence of suspected NAFLD. Data from men showed significantly lower rates of rates of suspected NAFLD in persons of Puerto Rican background. Among women, lower rates of NAFLD were observed in the Cuban, Dominican, and South American groups
Figure 1.
Age-Standardized Prevalence of Nonalcoholic Fatty Liver Disease (NAFLD) based on elevated aminotransferase for All Participants, Men and Women and by Hispanic/Latino Background Group after excluding other etiologies (*p<0.05, ***p<0.001)
The relation between suspected NAFLD and metabolic, socio-demographic, and behavioral factors is presented in Table 2. The metabolic syndrome, elevated waist circumference, elevated triglycerides and decreased HDL cholesterol were strongly associated with suspected NAFLD in both men and women. Higher carbohydrate intake was associated with suspected NAFLD in the total cohort. Other associations varied by gender. Specifically, elevated blood pressure was associated with suspected NAFLD in men, while impaired fasting glucose was correlated with suspected NAFLD in women. Moreover, there was an inverse relation between educational level and suspected NAFLD in women. Acculturation, healthcare use, sleep, physical activity and income were not associated with suspected NAFLD in either gender.
Table 2.
Univariate Results for the Association of Metabolic, Socio-demographic, and Behavioral Factors with Suspected Nonalcoholic Fatty Liver Disease (NAFLD)
| Variable | All Participants (N=12,133) | Women (N=7,589) | Men (N=4,544) |
|---|---|---|---|
| Age | |||
| 18–30(reference group) | 1 | 1 | 1 |
| 30–40 | 1.32(1.09,1.61)*** | 1.32(0.96,1.83) | 1.39(1.04,1.85)* |
| 40–50 | 1.08(0.90,1.31)*** | 1.32(1.01,1.73)* | 0.97(0.74,1.27) |
| 50–60 | 1.09(0.88,1.34)*** | 1.70(1.24,2.34)** | 0.75(0.56,1.00)* |
| 60+ | 0.68(0.54,0.86)*** | 1.15(0.83,1.61) | 0.43(0.30,0.61)*** |
| Female | 0.62(0.53,0.71)*** | -- | -- |
| Hispanic/Latino origin group | |||
| Mexican(reference group) | 1 | 1 | 1 |
| Cuban | 0.71(0.59,0.86)** | 0.57(0.44,0.73)*** | 0.75(0.58,0.98)* |
| Puerto Rican | 0.65(0.52,0.82)** | 0.79(0.57,1.09) | 0.52(0.38,0.72)*** |
| Dominican | 0.62(0.48,0.81)** | 0.54(0.38,0.76)** | 0.76(0.52,1.09) |
| Central American | 0.93(0.75,1.16) | 0.97(0.74,1.29) | 0.87(0.64,1.18) |
| South American | 0.75(0.59,0.96)* | 0.73(0.53,1.01) | 0.76(0.54,1.09) |
| Metabolic syndrome (present/absent) | 2.18(1.90,2.50)*** | 2.54(2.11,3.05)*** | 1.98(1.62,2.41)*** |
| Waist circumference (elevated/normal) | 1.64(1.43,1.88)*** | 2.71(2.14,3.45)*** | 1.95(1.62,2.36)*** |
| Triglycerides (elevated/normal) | 2.28(1.97,2.63)*** | 2.31(1.90,2.80)*** | 2.06(1.69,2.51)*** |
| HDL(low/normal) | 1.67(1.45,1.92)*** | 2.02(1.67,2.44)*** | 1.67(1.37,2.05)*** |
| Blood pressure (elevated/normal) | 1.47(1.22,1.77)*** | 1.30(0.98,1.74) | 1.44(1.11,1.86)** |
| Fasting glucose (elevated/normal) | 1.73(1.47,2.04)*** | 2.59(2.08,3.22)*** | 1.15(0.90,1.47) |
| Acculturation (language preference) | 0.97(0.92,1.03) | 0.94(0.86,1.02) | 0.97(0.89,1.05) |
| Physician visit | 1.00(0.98,1.01) | 1.01(0.99,1.02) | 0.99(0.98,1.01) |
| Sleep disturbance | 1.00(0.93,1.08) | 1.06(0.96,1.17) | 1.00(0.90,1.11) |
| Total carbohydrate | 9.83(3.54,27.35)*** | 0.34(0.04,3.15) | 2.50(0.51,12.28) |
| Physical activity(quartile) | |||
| Quartile 1(reference group) | 1 | 1 | 1 |
| Quartile 2 | 1.02(0.85,1.24) | 1.02(0.80,1.30) | 1.02(0.76,1.37) |
| Quartile 3 | 0.88(0.73,1.06) | 0.81(0.63,1.03) | 0.84(0.62,1.12) |
| Quartile 4 | 1.07(0.89,1.29) | 0.76(0.57,1.02) | 0.98(0.75,1.28) |
| Education | |||
| <=12 years(reference group) | 1 | 1 | 1 |
| 13–15 years | 0.88(0.74,1.04) | 0.74(0.58,0.93)* | 1.03(0.82,1.30) |
| >=16 years | 0.94(0.78,1.14) | 0.85(0.65,1.11) | 1.02(0.78,1.34) |
| Income | |||
| Less $10,000(reference group) | 1 | 1 | 1 |
| 10,001–$20,000 | 1.06(0.85,1.31) | 1.07(0.85,1.36) | 0.96(0.66,1.41) |
| $20,001–$40,000 | 1.10(0.89,1.36) | 0.98(0.77,1.26) | 1.08(0.75,1.55) |
| $40,001–$75,000 | 1.10(0.85,1.44) | 0.97(0.63,1.48) | 1.03(0.69,1.54) |
| More than $75,000 | 1.05(0.70,1.58) | 0.68(0.39,1.19) | 1.02(0.59,1.74) |
p<0.05
p<0.01
p<0.001
Data displayed in Odds ratios and 95% confidence intervals
A multivariable model was constructed to further assess risk factors for suspected NAFLD (Table 3). When controlling for all measured variables, Mexican Americans continued to have significantly higher rates of suspected NAFLD than persons of Cuban, Puerto Rican and Dominican background. The metabolic syndrome components including waist circumference, dyslipidemia, and elevated fasting glucose remained significantly associated with suspected NAFLD. Age greater than 40 also was associated with lower rates of suspected NAFLD. A secondary multivariate analysis was conducted replacing impaired fasting glucose and waist circumference with the prevalence of diabetes and body mass index, respectively. In that analysis, persons of Cuban (OR 0.72, 95% CI 0.59,0.88), Puerto Rican (OR 0.62, 95% CI 0.48,0.80) and Dominican (OR 0.64, 95% CI 0.49,0.85) heritage continued to have the lower rates of suspected NAFLD compared to those of Mexican heritage. Additional gender specific data is shown in Table 3. Notable, both men and women of Puerto Rican background had lower rates of suspected NAFLD. Gender specific differences were noted in persons of Cuban and Dominican background. Specifically, in persons of Cuban and Dominican heritage, lower rates of suspected NAFLD were driven by women. In men, suspected NAFLD decreased with increasing age, a finding not observed in women. Components of the metabolic syndrome were associated with NAFLD in both genders with a few exceptions shown in Table 3.
Table 3.
Multivariable Association of Metabolic, Sociodemographic, and Behavioral Factors and Suspected Nonalcoholic Fatty Liver Disease (NAFLD)
| Elevated aminotransferase levels | All Participants | Women | Men |
|---|---|---|---|
| Age | |||
| 18–30(reference group) | 1 | 1 | 1 |
| 30–40 | 1.09(0.88,1.34) | 1.09(0.77,1.54) | 1.10(0.83,1.47) |
| 40–50 | 0.77(0.62,0.95)* | 0.96(0.70,1.33) | 0.66(0.48,0.90)** |
| 50–60 | 0.72(0.56,0.91)** | 1.15(0.79,1.68) | 0.45(0.32,0.62)*** |
| 60+ | 0.43(0.33,0.56)*** | 0.77(0.52,1.15) | 0.25(0.17,0.37)*** |
| Female | 0.49(0.40,0.60)*** | NA | NA |
| Hispanic/Latino origin group | |||
| Mexican(reference group) | 1 | 1 | 1 |
| Cuban | 0.69(0.57,0.85)*** | 0.55(0.42,0.72)*** | 0.83(0.62,1.10) |
| Puerto Rican | 0.67(0.52,0.87)** | 0.71(0.51,0.98)* | 0.58(0.41,0.83)** |
| Dominican | 0.71(0.54,0.93)* | 0.59(0.41,0.85)** | 0.84(0.57,1.25) |
| Central American | 0.93(0.75,1.15) | 0.99(0.76,1.30) | 0.86(0.63,1.17) |
| South American | 0.86(0.66,1.13) | 0.86(0.60,1.22) | 0.84(0.58,1.23) |
| Waist circumference (elevated/normal) | 1.95(1.67,2.28)*** | 2.13(1.65,2.75)*** | 1.89(1.54,2.33)*** |
| Triglycerides (elevated/normal) | 1.76(1.50,2.07)*** | 1.59(1.29,1.97)*** | 1.82(1.44,2.29)*** |
| HDL(low/normal) | 1.33(1.16,1.54)*** | 1.55(1.27,1.90)*** | 1.23(0.99,1.53) |
| Blood pressure (elevated/normal) | 1.30(1.06,1.61)* | 1.11(0.80,1.56) | 1.46(1.10,1.94)** |
| Fasting glucose (elevated/normal) | 1.53(1.26,1.86)*** | 1.96(1.53,2.50)*** | 1.24(0.93,1.65) |
| Acculturation (language preference) | 0.96(0.89,1.03) | 0.99(0.90,1.09) | 0.94(0.84,1.04) |
| Healthcare use | 1.00(0.99,1.02) | 1.00(0.99,1.02) | 1.01(0.99,1.03) |
| Sleep disturbance | 1.04(0.96,1.12) | 1.04(0.95,1.15) | 1.02(0.91,1.15) |
| Total Carbohydate | 1.26(0.33,4.91) | 0.68(0.08,6.06) | 1.01(0.99,1.03) |
| Physical activity(quartile) | |||
| Quartile 1(reference group) | 1 | 1 | 1 |
| Quartile 2 | 1.04(0.86,1.27) | 1.02(0.80,1.32) | 1.05(0.77,1.43) |
| Quartile 3 | 0.85(0.70,1.03) | 0.85(0.67,1.10) | 0.82(0.60,1.13) |
| Quartile 4 | 0.91(0.74,1.10) | 0.77(0.56,1.06) | 0.90(0.68,1.21) |
| Education | |||
| <=12 years(reference group) | 1 | 1 | 1 |
| 13–15 years | 0.95(0.80,1.13) | 0.86(0.68,1.09) | 1.00(0.78,1.29) |
| >=16 years | 1.08(0.89,1.31) | 1.19(0.90,1.56) | 1.09(0.82,1.46) |
| Income | |||
| Less $10,000(reference group) | 1 | 1 | 1 |
| 10,001–$20,000 | 0.99(0.79,1.23) | 1.13(0.88,1.46) | 0.86(0.59,1.27) |
| $20,001–$40,000 | 1.01(0.81,1.26) | 1.07(0.83,1.39) | 0.95(0.66,1.38) |
| $40,001–$75,000 | 1.05(0.79,1.39) | 1.15(0.76,1.74) | 0.98(0.65,1.50) |
| More than $75,000 | 1.01(0.66,1.55) | 0.75(0.43,1.32) | 1.06(0.59,1.91) |
p<0.05
p<0.01
p<0.001
Data displayed in Odds ratios and 95% confidence intervals
Conclusions
The growing number of Hispanic/Latinos in the US 8, the high rates of childhood obesity among Hispanic youths 9, and the high prevalence of NAFLD 5 makes understanding the epidemiology of NAFLD in Hispanic/Latinos particularly important. The current study of more than 12,000 people from the unique HCHS/SOL cohort provides essential new information regarding the prevalence of NAFLD among diverse Hispanic/Latino groups. Persons of Mexican and Central American backgrounds had a higher prevalence of NAFLD compared to those of Puerto Rican, Dominican, and Cuban heritage. Persons with South American heritage had lower rates of suspected NAFLD compared to persons of Mexican heritage, however, the effect was not maintained when adjusting for other variables. These differences were not explained by differences in rates of metabolic syndrome, diet, physical activity, or acculturation. That is, when controlling for these factors, suspected NAFLD was still less common in Hispanic/Latino persons of Puerto Rican, Dominican and especially Cuban backgrounds. Suspected NAFLD was more common in individuals younger than age 40, and in men.
With prior studies highlighting the association of body mass index and diabetes13, 14 with the prevalence of NAFLD, a separate multivariate analysis was conducted substituting body mass index and diabetes for waist circumference and impaired fasting glucose, respectively. The differences seen in the prevalence of NAFLD based on heritage were unchanged. Total dietary carbohydrate was associated with suspected NAFLD in univariate ananlysis but not multivariate analysis. Moreover, in further analysis, total caloric intake was not associated with suspected NAFLD in multivariate analysis. Other factors including acculturation, health care use, physical activity, education and income were not directly associated with the odds of having NAFLD.
Although previous studies have highlighted the increased prevalence of NAFLD in Hispanic/Latino persons 4, 5, 7, none of these studies have examined rates of NAFLD based on background. The US Hispanic/Latino population is comprised of persons of diverse heritage. The persistence of differences in rates of suspected NAFLD when controlling for factors typically associated with NAFLD such as physical activity and the metabolic syndrome suggests a role for other undefined factors. Evidence is mounting that genetic polymorphisms can contribute to the development of NAFLD 22 such as the risk allele for PNPLA3 11. Although the function of the PNPLA3 gene is not known, the risk allele is associated with higher levels of hepatic triglyceride content and inflammation and is most common is persons of Hispanic/Latino background 11.
Hispanic/Latino populations in different regions have a variable mixture of Native American, European and African Ancestry 23, potentially affecting the genetic risk for NAFLD. The risk allele also has been shown to confer susceptibility to increased hepatic fat content resulting from dietary intake 24. Carbohydrate consumption in children was associated with excess hepatic fat content only in the cohort that had the PNPLA3 high risk allele suggesting the importance of genetic predisposition and lifestyle choices in the development of NAFLD 24. As such, the prevalence of NAFLD in specific populations appears to result from a complex interaction of behavioral and genetic factors that are not fully understood. It is possible that further examination of dietary and lifestyle factors may factor into the presence and progression of NAFLD when evaluated in the context of groups with a greater genetic predisposition.
The current study has limitations similar to those of previous population-based studies that have estimated the prevalence of NAFLD. More specifically, aminotransferase thresholds were used as a surrogate biomarker for NAFLD, as the HCHS/SOL study did not include liver imaging or liver biopsies. The values of aminotransferases chosen as abnormal in the study were selected to be consistent with other large population-based studies 6. It has been noted that significant liver disease can occur in patients with NAFLD who have “normal” alanine aminotransferase levels 25. Additionally, there is incomplete consensus on what constitutes the upper limit of normal for aminotransferases with more stringent criteria being proposed 26. When more stringent cut off values for ALT of > 19 in women and > 30 in men were applied to this population, 43.0% of women and 40.4% of men had an elevated level. Other causes of elevated aminotransferases such as medication-induced liver injury, autoimmune hepatitis, and other metabolic or genetic liver diseases were not excluded in the present analysis. However, based on prevalence data for these disorders, the impact of inclusion of these diseases is likely minimal. The higher prevalence of suspected NAFLD in younger persons deserves further comment. Alanine aminotransferase activity has been shown to decrease with age 27, thus potentially underestimating the prevalence of NAFLD in older persons in this study. Finally self-reported data for alcohol consumption, diet, physical activity and acculturation are subject to reporting bias. The major strengths of this study are the large number of Hispanic/Latino individuals from diverse backgrounds and the systematic collection of data on components of the metabolic syndrome, behavioral factors, and acculturation.
Hispanics/Latinos are now the largest and fastest growing minority group in the United States. Thus, it is important to more fully understand disease processes which disproportionally affect Hispanic/Latino populations. NAFLD has a particularly high prevalence in Hispanic/Latino individuals compared to other ethnic groups and Hispanic/Latinos are over-represented in cohorts with cirrhosis from NAFLD 28. Identification of Hispanic/Latino groups at the greatest risk for liver disease is important for identifying underlying NAFLD, implementing early interventions with lifestyle modification, and initiating appropriate evaluation for risk of cirrhosis and liver cancer. Data from the current study show that the risk of NAFLD is not equal in persons of Hispanic/Latino background. Genetic differences based on ancestral origins of Hispanic/Latino groups offer a plausible hypothesis that merits future study. Such studies could include measurement of PNPLA3 risk alleles in a diverse group of Hispanic persons and further examination of dietary and behavioral measures in the context of underlying genetic risk.
Acknowledgments
Grant Support
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Instituteon Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements.
The authors thank the staff and participants of HCHS/SOL for their important contributions.
List of Abbreviations
- HDL
High density lipoprotein
- HCHS/SOL
Hispanic Community Health Study/Study of Latinos
- NCEP-ATP
National Cholesterol Education Program- Adult Treatment Panel
- NHANES
National Health and Nutrition Examination Survey
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- PNPLA3
patatin-like phospholipase domain-containing protein 3
- US
United States
Footnotes
Disclosures: No author has any financial disclosure or conflict of interest relevant to this work The authors are solely responsible for the writing and content of the manuscript All authors were involved in the design of this study, interpretation of data, critical revision of the manuscript and approval of the final version. ERK and SJC were responsible for the manuscript drafting
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–85. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 2.Angulo P. Long-term mortality in nonalcoholic fatty liver disease: is liver histology of any prognostic significance? Hepatology. 2010;51:373–5. doi: 10.1002/hep.23521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soderberg C, Stal P, Askling J, et al. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602. doi: 10.1002/hep.23314. [DOI] [PubMed] [Google Scholar]
- 4.Kallwitz ER, Guzman G, TenCate V, et al. The histologic spectrum of liver disease in African-American, non-Hispanic white, and Hispanic obesity surgery patients. Am J Gastroenterol. 2009;104:64–9. doi: 10.1038/ajg.2008.12. [DOI] [PubMed] [Google Scholar]
- 5.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 6.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98:960–7. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 7.Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–31. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 8.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288:82–90. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ortiz-Lopez C, Lomonaco R, Orsak B, et al. Prevalence of prediabetes and diabetes and metabolic profile of patients with nonalcoholic fatty liver disease (NAFLD) Diabetes Care. 2012;35:873–8. doi: 10.2337/dc11-1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Romeo S, Kozlitina J, Xing C, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–5. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Jama. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 13.Lomonaco R, Ortiz-Lopez C, Orsak B, et al. Role of ethnicity in overweight and obese patients with nonalcoholic steatohepatitis. Hepatology. 2011;54:837–45. doi: 10.1002/hep.24483. [DOI] [PubMed] [Google Scholar]
- 14.Bambha K, Belt P, Abraham M, et al. Ethnicity and nonalcoholic fatty liver disease. Hepatology. 2012;55:769–80. doi: 10.1002/hep.24726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lara M, Akinbami L, Flores G, et al. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 16.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–41. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Solga S, Alkhuraishe AR, Clark JM, et al. Dietary composition and nonalcoholic fatty liver disease. Dig Dis Sci. 2004;49:1578–83. doi: 10.1023/b:ddas.0000043367.69470.b7. [DOI] [PubMed] [Google Scholar]
- 18.Toshimitsu K, Matsuura B, Ohkubo I, et al. Dietary habits and nutrient intake in non-alcoholic steatohepatitis. Nutrition. 2007;23:46–52. doi: 10.1016/j.nut.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 19.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 20.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–9. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwimmer JB, Celedon MA, Lavine JE, et al. Heritability of nonalcoholic fatty liver disease. Gastroenterology. 2009;136:1585–92. doi: 10.1053/j.gastro.2009.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sans M. Admixture studies in Latin America: from the 20th to the 21st century. Hum Biol. 2000;72:155–77. [PubMed] [Google Scholar]
- 24.Davis JN, Le KA, Walker RW, et al. Increased hepatic fat in overweight Hispanic youth influenced by interaction between genetic variation in PNPLA3 and high dietary carbohydrate and sugar consumption. Am J Clin Nutr. 2010;92:1522–7. doi: 10.3945/ajcn.2010.30185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fracanzani AL, Valenti L, Bugianesi E, et al. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology. 2008;48:792–8. doi: 10.1002/hep.22429. [DOI] [PubMed] [Google Scholar]
- 26.Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137:1–10. doi: 10.7326/0003-4819-137-1-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 27.Elinav E, Ben-Dov IZ, Ackerman E, et al. Correlation between serum alanine aminotransferase activity and age: an inverted U curve pattern. Am J Gastroenterol. 2005;100:2201–4. doi: 10.1111/j.1572-0241.2005.41822.x. [DOI] [PubMed] [Google Scholar]
- 28.Browning JD, Kumar KS, Saboorian MH, et al. Ethnic differences in the prevalence of cryptogenic cirrhosis. Am J Gastroenterol. 2004;99:292–8. doi: 10.1111/j.1572-0241.2004.04059.x. [DOI] [PubMed] [Google Scholar]