Abstract
Individuals who drink alcohol for the explicit motive of facilitating or enhancing sex may be more likely to engage in risky sexual behavior, including having sex under the influence of alcohol. However, efforts to assess sexual motives for drinking have been very limited to date. We examined the psychometric properties of a 5-item measure of sexual motives for drinking (SMD) in a sample of HIV-positive heavy drinking men who have sex with men. Findings provided excellent support for the scale's internal consistency and concurrent validity with a well-established measure of sexual alcohol expectancies (SAEs). Good discriminant validity was also established, as SMDs were correlated with other drinking motives but uniquely predicted the proportion of sex acts occurring under the influence of alcohol and other drugs, over-and-above other drinking motives and SAEs. SMDs were not significantly associated with unprotected anal intercourse. Adjusting for alcohol problem severity, higher SMDs were associated with lower willingness to consider changing drinking. Results suggest this measure of SMDs exhibits sound psychometric properties and may be useful in studies examining the association between alcohol use and sexual behavior.
Keywords: men who have sex with men, HIV, drinking motives, sex
Motivational models of alcohol use suggest that individuals hold differing expectations about the likely effects of alcohol, and that these different expectancies contribute to related self-reported motives for drinking; these motives, in turn, can act as proximal predictors of alcohol use patterns and problems (Cooper, Frone, Russell, & Mudar, 1995; Read, Wood, Kahler, Maddock, & Palfai, 2003). Identified motives for drinking have included drinking to cope with negative emotions, drinking to enhance pleasure, and drinking to facilitate social interactions, with validated subscales available to measure each (Cooper et al., 1995; Cooper, Russell, Skinner, & Windle, 1992). Although a great deal of research has examined the co-occurrence of alcohol use and sexual behavior (Irwin, Morgenstern, Parsons, Wainberg, & Labouvie, 2006; Mustanski, 2008; Vosburgh, Mansergh, Sullivan, & Purcell, 2012), a scale to assess the extent to which individuals drink to facilitate and enhance sex—that is, a sexual motives for drinking scale—has not been developed and validated to date.
Many individuals hold positive expectancies regarding alcohol's impact on sexual behavior, including increasing sexual pleasure and reducing inhibitions (Maisto et al., 2010), and these expectancies can influence sexual attitudes and intentions following alcohol consumption (Maisto, Carey, Carey, & Gordon, 2002; Maisto, Carey, Carey, Gordon, & Schum, 2004; Maisto, Carey, Carey, Gordon, Schum, et al., 2004; Maisto, Palfai, Vanable, Heath, & Woolf-King, 2012). Positive alcohol sex expectancies may lead some individuals to drink specifically for the purpose of enhancing sexual pleasure and reducing sexual inhibitions (Leigh, 1990b), although holding positive alcohol-sex expectancies does not necessarily translate into drinking for those motives (Leigh, 1990a). A scale to assess sexual motives for drinking could be valuable for sex-risk prevention and intervention research because individuals who regularly drink to facilitate or enhance sex may be especially likely, then, to engage in sex while under the influence of alcohol. Sex that occurs under the influence of alcohol may be more likely to be unprotected and, thus, entail risk for acquiring or transmitting sexually transmitted infections (STIs), including HIV (Fritz, Morojele, & Kalichman, 2010; Sander et al., 2013). This conceptual model is shown in Figure 1. Sexual motives for drinking may be important also because such motives may make people less willing to change drinking if they do not perceive there to be a sufficient alternative means for facilitating sex. In that way, sexual motives for drinking may detract from openness to changing heavy drinking and, therefore, are important to investigate empirically.
Figure 1.
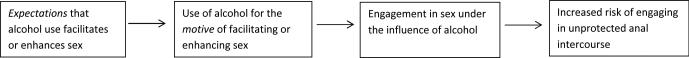
Proposed relationships of sexual motives for drinking with alcohol-sex expectancies, sex under the influence of alcohol, and risk of unprotected anal intercourse.
The present study evaluated the psychometric properties of a brief measure of sexual motives for drinking (SMD), including examining its internal consistency and its concurrent, incremental, and discriminant validity. We utilized data from a sample of 109 HIV-positive heavy-drinking men who have sex with men (MSM). Although examining SMD in any population could be valuable, HIV-positive MSM are a population of particular concern regarding sexual behaviors that may entail HIV transmission risk; an initial validation of the scale in a relatively homogenous sample of heavy drinkers can provide a more clear picture of the associations of SMD with alcohol consumption and sexual behaviors without having to take into account the added complexities of gender, sexual orientation, and HIV status.
We hypothesized that SMD would correlate positively with alcohol-sex expectancies (concurrent validity) and with having a higher proportion of sex occurring under the influence of substances and more condomless sex. We also hypothesized that SMDs would predict the frequency of unprotected anal intercourse and sexual events under the influence more strongly than alcohol-sex expectancies and more strongly than measures of other drinking motives (incremental validity). We further hypothesized that greater SMD would predict lower readiness to consider changing drinking above and beyond the effects of alcohol problems and other drinking motives (incremental validity). Finally, we hypothesized that SMD would be less strongly associated with alcohol-related problems than drinking for coping motives (discriminant validity), which has been shown to be a robust predictor of alcohol problems in a variety of samples (e.g., Read et al., 2003), including in patients receiving treatment for HIV (Elliott, Aharonovich, O'Leary, Wainberg, & Hasin, 2013, 2014).
Method
Data come from the baseline assessments of participants in a clinical trial testing an intervention to reduce heavy alcohol use among MSM receiving treatment for HIV. Participants were recruited from an urban community health center that specializes in providing comprehensive care to lesbian, gay, bisexual, and transgender individuals. Data are derived from the first 109 men who participated in either the pilot of the study (n = 5) or the randomized phase (n = 104). For inclusion, participants had to: (1) be at least 18 years of age; (2) drink heavily at least once per month on average (≥5 drinks) or drink more than 14 drinks per week on average; (3) have a confirmed diagnosis of HIV; and (4) be a man who reports having had sex (insertive or receptive, oral or anal) with a male partner in the past 12 months. Those on ART had to be stabilized on their current regimen for at least three months prior to study enrollment. Participants were excluded if they: (1) reported current injection drug use; (2) were currently psychotic, suicidal, or manic; (3) were currently being treated, or had been treated in the past three months, for an HIV-related opportunistic infection; or (4) were currently receiving treatment for an alcohol or drug problem.
Participants were recruited through flyers posted at the clinic or during scheduled visits with their HIV care providers. Potential participants first completed a brief eligibility screening with study staff. Those who appeared eligible based on their responses were scheduled for a baseline visit. Participants were asked to abstain from alcohol for 24 hours prior to this assessment, which was confirmed at the start of the visit by alcohol breath analysis. At baseline, participants provided informed consent approved by the (removed for blinding) Institutional Review Boards. Potential participants then completed confirmation screening for eligibility and the remainder of the baseline interview.
A total of 626 individuals were approached for screening at the clinic or called the study to inquire about participating. Of these, 239 declined to be screened. Of those screened, 142 appeared eligible for the study, of whom 123 completed a baseline assessment. In total, 109 were fully eligible, completed the full baseline interview, and comprise the sample presented here.
Measures
Current alcohol and substance use disorders, major depressive disorder, mania, and psychotic symptoms were assessed using the SCID-NP (First, Spitzer, Gibbon, & Williams, 1994). The Short Inventory of Problems [SIP; (Miller, Tonigan, & Longabaugh, 1995)] was used to assess problems related to alcohol use occurring in the past 3 months. The Precontemplation subscale (e.g., “I don't think I drink too much”) from the Readiness to Change Questionnaire (Rollnick, Heather, Gold, & Hall, 1992) was used as the measure of resistance to changing drinking, given that all participants were currently drinking heavily. Depressive symptoms were assessed using the Center for Epidemiologic Studies–Depression scale [CES-D; (Radloff, 1977)].
The Timeline Followback interview [TLFB; (Sobell & Sobell, 1980)] was used to assess alcohol and drug use as well as sexual behavior. The TLFB interview is a structured interview that uses a calendar to cue memory so that accurate recall is enhanced. It has been shown to be a reliable and valid method of assessing alcohol and drug use (Fals-Stewart, O'Farrell, Freitas, McFarlin, & Rutigliano, 2000; Sobell & Sobell, 1980; Sobell & Sobell, 1979), as well as sexual behavior (Carey, Carey, Maisto, Gordon, & Weinhardt, 2001; Weinhardt et al., 1998). This interview assessed each occasion of sexual activity over the past 30 days, with detailed information on the type of partner (primary, casual, or anonymous); HIV status of partner (positive, negative, or unknown); type of sexual activity (oral, anal, vaginal; insertive or receptive); condom use; and whether the participant was under the influence of alcohol or drugs at the time of sex. Four variables were derived from this measure for these analyses: (1) percent days having oral, anal, or vaginal sex (i.e., any sexual activity); (2) percent of sex events that occurred while under the influence of alcohol or other substances; (3) percent days of unprotected anal intercourse (UAI); and (4) percent of UAI days occurring under the influence.
Motives for drinking were assessed with the 15-item Drinking Motives Questionnaire (Cooper et al., 1992), which has been shown to have strong psychometric properties and validity (Cooper et al., 1995). Participants indicated how often they drank for each specific reason using a 0 = almost never to 5 = almost always/always Likert-type scale. Five items each assessed coping motives (e.g., “To forget your worries”); enhancement motives (e.g., “Because you like the feeling”); and social facilitation motives (“To be sociable”). We created five additional items to match the number of items in the other motives subscales, and which assess drinking in order to enjoy sex more, feel less inhibited, or feel more confident sexually, drawing from prior work on alcohol-sex expectancies (Leigh, 1990a; Maisto et al., 2010). See Table 1 for item content.
TABLE 1.
Demographic characteristics of the sample (N = 109)
| Characteristics | Mean (SD) or N (%) |
|---|---|
| Age (Range: 20 – 63, M ± SD) | 42.5 (10.6) |
| Race | |
| White | 77 (70.6) |
| Black or African American | 26 (24.8) |
| American Indian/Alaska Native | 5 (4.6) |
| Asian | 1 (0.9) |
| Ethnicity (Hispanic or Latino) | 20 (18.3) |
| Marital Status | |
| Single/Never married | 54 (49.5) |
| Married/Domestic partnership | 26 (23.9) |
| In a committed relationship | 14 (12.8) |
| Divorced/Separated | 9 (8.3) |
| Widowed | 4 (3.7) |
| Education | |
| Some high school | 2 (1.8) |
| High school diploma/GED | 13 (11.9) |
| Some college education | 39 (35.8) |
| College graduate | 22 (20.2) |
| Some graduate school | 10 (9.2) |
| Technical or business school | 8 (7.3) |
| Graduate or professional degree | 15 (13.8) |
| Income | |
| $0 - $29,999 | 51 (46.8) |
| $30,000 - $99,999 | 37 (33.9) |
| $100,000 or more | 20 (18.3) |
| Sexual identity | |
| Gay/homosexual | 101 (92.7) |
| Bisexual | 6 (5.5) |
| Other | 2 (1.8) |
| Years since HIV diagnosis | 10 (7.7) |
| On antiretroviral therapy | 99 (90.8) |
| Detectable viral load (>75 copies) | 11 (10.1) |
| Number of drinks per week | 22.1 (21.8) |
| % Alcohol dependent | 41 (37.6) |
| % Substance dependent (non-alcohol) | 15 (13.8) |
Sexual alcohol expectancies (SAEs) were assessed using a 13-item scale (Leigh, 1990a, 1990b). Participants indicated how much they believed alcohol positively affects sexual arousal and behavior on a 0 = not at all to 3 = very much scale (e.g., “When I drink enough alcohol to feel the effects, I enjoy sex more”). The total scale score (α = .90) was used in all analyses.
Data Analysis Plan
We examined item-test correlations and Cronbach's alpha for all SMD items, and then conducted a principal factors analysis (PFA) with varimax rotation to determine whether SMD items assessed a separate dimension than the other items on the Drinking Motives Questionnaire. We then examined the SMD scale's correlations with SAEs (concurrent validity) and the other drinking motives scales, as well as with four sexual behaviors: % of days in the past 30 engaging in oral, anal, or vaginal sex, % of sex acts occurring under the influence of alcohol and/or other substances, % of all sex events that involved unprotected anal intercourse (UAI), and % of days on which UAI events occurred with HIV-negative or HIV-status unknown partners. We then ran a set of regression analyses to test whether SMD provided incremental validity in predicting (a) the proportion of sex acts occurring under the influence of substances, (b) scores on the Precontemplation scale, and (c) frequency of alcohol-related problems (SIP total scores).
Results
Sample Description
Demographic and clinical characteristics of participants are presented in Table 1. Only a small portion met criteria for substance dependence, but 55.9% reported at least some use of the following drugs over the 30-day period: marijuana, methamphetamine, cocaine, opiates, MDMA, or Adderall. The mean number of days of marijuana use over the 30-day period was 6.7 (SD = 10.7, Range 0-30); methamphetamine use was 0.17 (SD = 0.78, Range 0-6), cocaine use was 1.1 (SD = 3.5, Range 0-21), opiate use was 0.27 (SD = 2.40, Range 0-25), MDMA use was 0.05 (SD = 0.25, range 0-2), and Adderall use was 0.03 (SD = 0.21, Range 0-2) days.
Reliability of sex-related motives for drinking (SMD) items
As shown in Table 2, item-test correlations were excellent, ranging from 0.80 to 0.86, suggesting that all individual items exhibited excellent consistency with the scale. Alpha for the 5-item scale was excellent at .89, and no items detracted from internal consistency. Results of PFA showed that the five SMD items loaded solely on a single factor with loadings ranging from .55 to .79, and no other items cross-loading on that factor higher than .40.
TABLE 2.
Item-test and Cronbach's alphas for Sex Motives for Drinking (SMD) items
| Associations with SMD items |
|||
|---|---|---|---|
| Sex motives for drinking items | Item-test r | Avg. inter-item r | α * |
| 2. Because it helps you enjoy sex more | 0.86 | 0.61 | 0.86 |
| 8. To feel less inhibited sexually | 0.88 | 0.60 | 0.86 |
| 12. To feel more confident in approaching sex partners | 0.85 | 0.62 | 0.87 |
| 19. To make you more horny | 0.80 | 0.65 | 0.88 |
| 20. To make you feel less nervous a/b sex | 0.80 | 0.65 | 0.88 |
| Total | 0.63 | 0.89 | |
Note. Cronbach's alpha value if that item were deleted.
Concurrent validity
As shown in Table 3, SMD exhibited a strong, positive correlation with SAEs, providing evidence of concurrent validity, while also showing that about half of the variance in the scales was unique. SMD also was strongly positively correlated with other drinking motives. SMD was positively correlated with the average number of drinks consumed per week and with level of alcohol problems. SMD was correlated significantly with the percent of total sex occasions that occurred while under the influence of alcohol or other substances. SMD was not significantly correlated with frequency of sex and contrary to our hypotheses, was not significantly correlated with the percent of sex events involving UAI, or the percent of days of UAI with HIV-negative or unknown status partners.
TABLE 3.
Bivariate correlations between SMDs, SAEs, other drinking motives, and sex-related variables
| Drinking Motives |
Sex-Related Alcohol Expectancies (SAE) | Sex Drinking Motives (SMD) | |||
|---|---|---|---|---|---|
| Enhancement | Coping | Social Facilitation | |||
| SAE | 0.40* | 0.57* | 0.44* | ||
| SMD | 0.50* | 0.64* | 0.46* | 0.69* | |
| Age | −0.03 | −0.04 | −0.20* | −0.08 | 0.05 |
| Avg. Drinks per Week | 0.26* | 0.14 | 0.08 | 0.16 | 0.32* |
| Alcohol Problems | 0.27* | 0.49* | 0.13 | 0.47* | 0.47* |
| % Sex Days | 0.04 | 0.01 | −0.08 | 0.06 | 0.17 |
| % Alc/Drug Affected Sexa | 0.12 | 0.09 | 0.14 | 0.28* | 0.35* |
| % UAIa | 0.20* | −0.02 | 0.15 | 0.02 | 0.11 |
| % Days UAI w/HIV- or HIV? Partnerb | 0.15 | −0.03 | −0.03 | 0.09 | 0.10 |
Note
p < .05. SMD = Sex-related Motives for Drinking, SAE = Sex-related Alcohol Expectancies. UAI = unprotected anal intercourse.
Of all sex occasions.
Of the 30 days assessed.
Incremental validity
We examined incremental validity by exploring the unique associations of the SMD scale with relevant sex and alcohol-related outcomes over-and-above other pertinent predictors, such as level of alcohol use, SAEs, and other drinking motives. In the first case, the outcome of interest consisted of the ratio of total sex events that were alcohol and drug affected over the total number of sex events (% days UAI was not examined further given the nonsignificant bivariate association with SMDs reported above). See Table 4 for results. In this linear regression model, SMDs were significantly positively related to having a higher ratio of alcohol or drug affected sex relative to all sex activity. SAEs were unrelated to this outcome when controlling for SMDs. The only other variable that was associated with this outcome was coping motives, with results indicating that, controlling for other drinking motives, drinking to cope was associated with a lower proportion of sex occurring under the influence.
TABLE 4.
Linear regression predicting the ratio of the total occasions on which alcohol and drug-affected sex was reported over the total sex occasions reported
| Variable | B | SE | p | sr2 |
|---|---|---|---|---|
| Age | −0.01 | 0.01 | .167 | 0.02 |
| Income | −0.01 | 0.01 | .702 | 0.01 |
| Education | −0.02 | 0.02 | .436 | 0.01 |
| Avg. drinks per week | 0.01 | 0.01 | .420 | 0.01 |
| Coping motives | −0.15 | 0.07 | .036 | 0.04* |
| Enhancement motives | −0.04 | 0.07 | .583 | 0.01 |
| Social facilitation motives | −0.01 | 0.07 | .966 | 0.00 |
| SAEs | 0.08 | 0.08 | .325 | 0.01 |
| Sexual motives for drinking (SMD) | 0.22 | 0.08 | .006 | 0.06* |
Note. SAEs = Sex-related alcohol expectancies. Final model, F(9, 98) = 2.87, p = .004, Adj. R2= 0.14.
p < .05.
Next, we tested whether SMD would exhibit a positive association with scores on the Precontemplation scale. See Table 5 for results. Alcohol-related problems were negatively associated with Precontemplation scores, such that participants who reported more alcohol-related problems were less likely to deny considering changes to their drinking. Although the bivariate association between SMD and Precontemplation was nonsignificant (r = -.04), controlling for other drinking motives, SMDs were positively associated with Precontemplation scores over-and-above alcohol use and alcohol-related problems—suggesting that those who frequently drink to facilitate sex report a greater intention not to change drinking behavior.
TABLE 5.
Linear regression of readiness to change - precontemplation
| Variable | B | SE | p | sr2 |
|---|---|---|---|---|
| Age | 0.01 | 0.03 | .793 | 0.01 |
| Income | 0.02 | 0.08 | .832 | 0.01 |
| Education | −0.42 | 0.16 | .012 | 0.05* |
| Avg. drinks per week | −0.02 | 0.01 | .241 | 0.01 |
| Alcohol-related problems | −0.15 | 0.04 | < .001 | 0.10* |
| Coping motives | −0.67 | 0.47 | .162 | 0.01 |
| Enhancement motives | −0.76 | 0.48 | .117 | 0.02 |
| Social facilitation motives | 0.29 | 0.46 | .532 | 0.01 |
| Sex motives (SMD) | 0.96 | 0.47 | .044 | 0.03* |
Note. Final model, F(9, 98) = 3.96, p < .001, Adj. R2= 0.20.
p < .05.
Discriminant validity
Finally, we examined whether SMD would be less strongly associated with alcohol-related problems compared to coping motives. Results supported this hypothesis (Table 6). Coping motives were positively associated with alcohol-related problems, consistent with previous literature (e.g., Read et al., 2003). However, SMDs were not significantly associated with alcohol problems when controlling for other drinking motives.
TABLE 6.
Linear regression of alcohol-related problems
| Variable | B | SE | p | sr2 |
|---|---|---|---|---|
| Age | −0.02 | 0.06 | .757 | 0.01 |
| Income | −0.38 | 0.20 | .061 | 0.02 |
| Education | 0.19 | 0.40 | .630 | 0.01 |
| Avg. drinks per drinking day | 0.05 | 0.03 | .164 | 0.01 |
| Coping motives | 3.59 | 1.10 | .001 | 0.07* |
| Enhancement motives | 0.21 | 1.18 | .856 | 0.01 |
| Social facilitation motives | −1.81 | 1.12 | .096 | 0.02 |
| Sex motives (SMD) | 1.83 | 1.13 | .109 | 0.02 |
Note. Final model, F(8, 99) = 6.74, p < .001, Adj. R2= 0.30.
p < .05.
Discussion
Results indicate that a 5-item measure of sexual motives for drinking alcohol, developed for this study, showed good psychometric properties in a sample of heavy-drinking MSM living with HIV. Internal consistency was excellent, as was concurrent validity with a well-established measure of sexual alcohol expectancies; however, the SMD scale was also distinguishable from the SAE scale, with which it shared about 50% common variance. The measure showed good incremental validity, as it was a stronger predictor than SAEs of the proportion of sex acts that occurred under the influence of alcohol or other substances. Although expecting that alcohol may enhance sex may be a necessary condition for being motivated to drink for that reason (Leigh, 1990a), results provide support for our hypothesis that SMDs are more proximal predictors of engaging in sex under the influence than expectancies. For interventions that address the risk associated with HIV-positive MSM having sex under the influence of alcohol (e.g., Velasquez et al., 2009), it may prove valuable to tailor intervention strategies accordingly based on the extent to which men report conscious motives to use alcohol to facilitate sex, as opposed to reporting unplanned sexual behavior resulting from alcohol's disinhibiting effects.
The SMD scale also showed good discriminant validity with regards to other drinking motives. Although SMD correlated strongly with drinking for other motives, in a multiple regression model the SMD scale was the only unique predictor of the percentage of sex acts that occurred under the influence. SMD correlated positively with alcohol problems but, as hypothesized, it was the coping motives scale that most strongly and uniquely predicted alcohol problems in a multivariate model. Finally, although the association between SMD and unwillingness to consider changing drinking was not significant on a bivariate level, when controlling for other drinking motives and alcohol-related problems, greater SMD predicted less willingness to consider change (i.e., greater levels of precontemplation). That is, at a given level of alcohol problem severity, having greater SMD may make MSM less willing to change their drinking behavior. These results suggest that addressing the tendency to drink specifically to facilitate sex, perhaps by challenging alcohol's effects on sex and/or exploring alternative ways of seeking sex, may be a valuable target of intervention for these individuals.
The hypothesis that was not supported in this study was that greater SMD would be associated with having more UAI. Our results suggest that, while some MSM may be motivated to drink alcohol as a means of enhancing sex, other factors may be more relevant to predicting behaviors that increase risk of STIs and HIV transmission, including level of alcohol use on a given occasion, as well other attitudinal and contextual variables not assessed in these analyses (e.g., condom attitudes). The current study examined SMDs using global retrospective measures. Accurately reporting these highly specific reasons for drinking on particular occasions may be difficult for those who drink heavily, potentially obscuring their relationship with sex risk outcomes. As such, future research should explore the potential role of motives closer in time to decisions to drink.
Limitations
The present study validated a measure of SMD with promising results. However, the sample analyzed, though of high public health significance, was limited solely to MSM receiving care for HIV who drank heavily and agreed to participate in an alcohol intervention study. Results should only be generalized beyond this subpopulation of MSM with caution. It will be valuable to examine whether the scale performs similarly when used with women or with men who have sex exclusively with women. Likewise, that all MSM were living with HIV may influence the meaning and context of UAI. For MSM who are uninfected, the consequences of UAI are different and, therefore, behaviors regarding alcohol and UAI may differ.
Conclusions
Sexual motives for drinking can be assessed reliably when added to a well-validated measure of drinking motives. The scale may be useful for researchers focusing on alcohol use and sexual behavior, as it may help identify individuals who are especially likely to engage in sex under the influence of alcohol and for whom interventions to reduce drinking may also impact sexual behavior.
Acknowledgments
source of funding: The study was supported by grants P01AA019072, T32AA007459 and K05 AA019681 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
Conflicts of interest: The authors have no financial relationship with the study sponsor, and no conflicts of interest to disclose.
References
- Carey MP, Carey K, Maisto S, Gordon C, Weinhardt L. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. International Journal of STD & AIDS. 2001;12(6):365–375. doi: 10.1258/0956462011923309. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69(5):990–1005. doi: 10.1037//0022-3514.69.5.990. doi: 10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4(2):123–132. doi: 10.1037/1040-3590.4.2.123. [Google Scholar]
- Elliott JC, Aharonovich E, O'Leary A, Wainberg M, Hasin DS. Drinking motives among HIV primary care patients. AIDS and Behavior. 2013:1–9. doi: 10.1007/s10461-013-0644-4. doi: 10.1007/s10461-013-0644-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Aharonovich E, O'Leary A, Wainberg M, Hasin DS. Drinking motives as prospective predictors of outcome in an intervention trial with heavily drinking HIV patients. Drug and Alcohol Dependence. 2014;134:290–295. doi: 10.1016/j.drugalcdep.2013.10.026. doi: 10.1016/j.drugalcdep.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68(1):134–144. doi: 10.1037//0022-006x.68.1.134. doi: 10.1037/0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for Axis I DSM-IV disorders. New York State Psychiatric Institute; New York: 1994. [Google Scholar]
- Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. The Lancet. 2010;376(9739):398–400. doi: 10.1016/S0140-6736(10)60884-7. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin TW, Morgenstern J, Parsons JT, Wainberg M, Labouvie E. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: An event level analysis of timeline followback data. AIDS and Behavior. 2006;10(3):299–307. doi: 10.1007/s10461-005-9045-7. doi: 10.1007/s10461-005-9045-7. [DOI] [PubMed] [Google Scholar]
- Leigh BC. Alcohol expectancies and reasons for drinking: Comments from a study of sexuality. Psychology of Addictive Behaviors. 1990a;4(2):91–96. doi: 10.1037/h0080578. [Google Scholar]
- Leigh BC. The relationship of sex-related alcohol expectancies to alcohol consumption and sexual behavior. British Journal of Addiction. 1990b;85(7):919–928. doi: 10.1111/j.1360-0443.1990.tb03722.x. doi: 10.1111/j.1360-0443.1990.tb03722.x. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. Journal of Studies on Alcohol. 2002;63(4):476–485. doi: 10.15288/jsa.2002.63.476. PMCID: PMC2423734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Experimental and Clinical Psychopharmacology. 2004;12(4):288–297. doi: 10.1037/1064-1297.12.4.288. doi: 10.1037/1064-1297.12.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL, Lynch KG. The relationship between alcohol and individual differences variables on attitudes and behavioral skills relevant to sexual health among heterosexual young adult men. Archives of Sexual Behavior. 2004;33(6):571–584. doi: 10.1023/B:ASEB.0000044741.09127.e6. doi: 10.1023/B:ASEB.0000044741.09127.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, McGinnis K, Cook R, Conigliaro J, Bryant K, Justice AC. Factor structure of Leigh's (1990) Alcohol Sex Expectancies Scale in individuals in treatment for HIV disease. AIDS and Behavior. 2010;14(1):174–180. doi: 10.1007/s10461-008-9457-2. doi: 10.1007/s10461-008-9457-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Palfai T, Vanable PA, Heath J, Woolf-King SE. The effects of alcohol and sexual arousal on determinants of sexual risk in men who have sex with men. Archives of Sexual Behavior. 2012;41(4):971–986. doi: 10.1007/s10508-011-9846-x. doi: 10.1007/s10508-011-9846-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse: Test manual. Vol. 4. NIAAA Project MATCH Monograph Series; Washington, DC: 1995. [Google Scholar]
- Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS and Behavior. 2008;12(1):118–126. doi: 10.1007/s10461-007-9335-3. doi: 10.1007/s10461-007-9335-3. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [Google Scholar]
- Read JP, Wood MD, Kahler CW, Maddock JE, Palfai TP. Examining the role of drinking motives in college student alcohol use and problems. Psychology of Addictive Behaviors. 2003;17(1):13–23. doi: 10.1037/0893-164x.17.1.13. doi: 10.1037/0893-164X.17.1.13. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction. 1992;87(5):743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, Ostrow DG. Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS (London, England) 2013;27(5):815–823. doi: 10.1097/QAD.0b013e32835cff4b. doi: 10.1097/QAD.0b013e32835cff4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Convergent validity: An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell L, Sobell M, Ward E, editors. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. Pergamon Press; New York: 1980. pp. 177–183. [Google Scholar]
- Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. Journal of Consulting and Clinical Psychology. 1979;46(5):901–907. doi: 10.1037//0022-006x.46.5.901. doi: 10.1037/0022-006X.46.5.901. [DOI] [PubMed] [Google Scholar]
- Velasquez MM, von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(4):657–667. doi: 10.1037/a0015519. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior. 2012;16(6):1394–1410. doi: 10.1007/s10461-011-0131-8. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline follow-back sexual behavior interview. Annals of Behavioral Medicine. 1998;20(1):25–30. doi: 10.1007/BF02893805. doi: 10.1007/BF02893805. [DOI] [PMC free article] [PubMed] [Google Scholar]


