Abstract
Here we wanted to investigate predictive value of neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR) in the diagnosis of brucellosis. Thirty-two brucellosis patients diagnosed with positive serum agglutination test and thirty-two randomized healthy subjects were enrolled in this study retrospectively. Result with ROC analyzes the baseline NLR and hemoglobin values were found to be significantly associated with brucellosis (P = 0.01, P = 0.01, resp.). Herein we demonstrated for the first time that NLR values were significantly associated with brucellosis. This situation can help clinicians during diagnosis of brucellosis.
1. Introduction
Brucellosis is a zoonotic disease that is transmittable to humans from infected animal reservoirs especially from milk and milk products [1]. Brucellosis may present with a broad spectrum of unspecific clinical manifestations, for example, fever, chills, sweating, malaise, arthralgia, weakness, back pain, and headache [2]. Many organ systems may be involved and it can be severe like endocarditis [3]. Most commonly serum agglutination test is used for diagnosis of brucellosis and its result conforms with complement fixation or Coombs' test [4]. In the diagnosis of brucellosis the gold standard test is culture of brucellosis [5]. Which patients must we suspect for brucellosis? In our clinic we suspect feverish patients with a history of milk and milk products intake. Laboratory and clinic findings are unclear in brucellosis patients. Because brucellosis patients show unspecific symptoms and unspecific laboratory findings, we aimed to investigate predictive contribution value of neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR) in diagnosis of brucellosis.
2. Methods and Statistics
We collected clinical and laboratory data of thirty-two patients with brucellosis diagnosed with serum agglutination test and randomized thirty-two healthy people's data from hospital records retrospectively. We collected patients' blood samples at the admission and then we analyzed laboratory parameters that consist of haematological, biochemical, and serological tests. The white blood cell (WBC) and neutrophil and lymphocyte counts were recorded and NLR and PLR were calculated from these parameters. The cut-off titer value for serum agglutination test was 1/160 in diagnosis of brucellosis. We compare haematological parameters that consist of NLR and PLR between two groups.
All analyses were performed using SPSS for Windows (version 21.0; SPSS/IBM, Chicago, IL). Student's t-test, Pearson's chi-squared test, and logistic regression test were used when suitable. A P value <0.05 was considered statistically significant.
3. Results
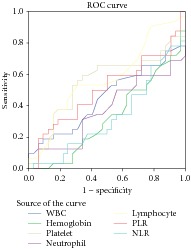
The mean age of brucellosis patients was 41,7 ± 16,1. 62,5% of patients were male and 37,5% female, respectively. The most common brucellosis symptoms at the time of diagnosis were fatigue (37,5%), anorexia (34,4%), joint pain (34,4%), myalgia (31,3%), fever (25%), chills (18,8%), and feeling cold (18.8%), respectively (Table 1). We compare haematological parameters that consist of NLR and PLR between brucellosis patients and healthy groups. Result with ROC analyzes the baseline NLR and hemoglobin values were found to be significantly associated with brucellosis (P = 0.01, P = 0.01, resp.) (Table 2). There were no observed significant correlations with result of Fisher's exact test for NLR and hemoglobin values (Table 3). Result with Student's t-test, the PLR, neutrophil, lymphocyte, platelet count, WBC mean values was not significantly different between two groups (P > 0.05) (Table 4).
Table 1.
Symptoms and signs of patients with brucellosis at the admission.
| n | % | |
|
| ||
| Fatigue | 12 | 37,5 |
| Anorexia | 11 | 34,4 |
| Joint pain | 11 | 34,4 |
| Myalgia | 10 | 31,3 |
| Sacroiliitis | 8 | 25 |
| Fever | 6 | 18,8 |
| Feeling cold | 6 | 18,8 |
| Splenomegaly | 6 | 18,8 |
| History of ingestion of fresh cheese | 5 | 15,6 |
| Chill | 4 | 12,5 |
| Hepatomegaly | 3 | 9,4 |
| Night sweats | 3 | 9,4 |
| Headache | 3 | 9,4 |
| Abdominal pain | 2 | 6,3 |
| Nausea | 1 | 3,1 |
| Vomiting | 1 | 3,1 |
| Constipation | 1 | 3,1 |
Table 2.
Model selection with ROC curve estimation in regression analysis for brucellosis.
| Variable(s) | P value | 95% confidence interval | |
|---|---|---|---|
| Lower bound | Upper bound | ||
| WBC | 0,50 | 0,30 | 0,59 |
| Hemoglobin | 0,01 | 0,19 | 0,45 |
| Platelet | 0,48 | 0,40 | 0,69 |
| Neutrophil | 0,07 | 0,23 | 0,51 |
| Lymphocyte | 0,31 | 0,43 | 0,71 |
| PLR | 0,95 | 0,35 | 0,64 |
| NLR | 0,01 | 0,19 | 0,46 |
|
| |||
| Diagonal segments are produced by ties | |||
|
| |||
| |||
Table 3.
Comparison of haematological parameters between brucellosis and healthy group (Fisher's exact test).
| Fisher's exact test | Number | P value | |
|---|---|---|---|
| NLR < 1.5 | Healthy group | 21 | 0,06 |
| Brucellosis group | 11 | ||
| NLR > 1.5 | Healthy group | 14 | |
| Brucellosis group | 18 | ||
|
| |||
| Hemoglobin < 12.5 | Healthy group | 11 | 0,07 |
| Brucellosis group | 21 | ||
| Hemoglobin > 12.5 | Healthy group | 5 | |
| Brucellosis group | 27 | ||
Table 4.
Comparison of haematological parameters between brucellosis and healthy group (Student's t-test).
| Mean | SD | P value | ||
|---|---|---|---|---|
| PLR | Brucellosis group | 108,31 | 41,61 | 0,93 |
| Healthy group | 109,29 | 46,84 | ||
|
| ||||
| Neutrophil | Healthy group | 3640,62 | 1031,08 | 0,10 |
| Brucellosis group | 3106,25 | 1356,21 | ||
|
| ||||
| WBC | Brucellosis group | 6187,50 | 1968,42 | 0,53 |
| Healthy group | 6459,37 | 1163,65 | ||
|
| ||||
| Platelet | Brucellosis group | 242031,2 | 86953,63 | 0,67 |
| Healthy group | 234281,2 | 62631,65 | ||
|
| ||||
| Lymphocyte | Brucellosis group | 2356,25 | 664,26 | 0,37 |
| Healthy group | 2203,12 | 545,64 | ||
4. Discussion
We know that laboratory parameters and clinical symptoms are unspecific in brucellosis. High NLR values were found in inflammatory processes compared to noninflammatory processes in the literature [6–8].
NLR has been investigated for many diseases [9–16] but there are few studies between NLR and infectious diseases and there is not any study between brucellosis and NLR.
Therefore, we investigated predictive contribution value of NLR, PLR, and the other haematological parameters in diagnosis of brucellosis.
We compare NLR, PLR, and the other haematological parameters between brucellosis and healthy subjects. Result with ROC analyzes the baseline NLR and hemoglobin values were found to be significantly associated with brucellosis (P = 0.01, P = 0.01, resp.). There were no observed significant correlations with result of Fisher's exact test for NLR and hemoglobin values (P > 0.05). Result with Student's t-test, the PLR, neutrophil, lymphocyte, platelet count, WBC mean values was not significantly different between two groups (P > 0.05).
In a study conducted on patients with tuberculosis and sarcoidosis, Iliaz et al. demonstrated that the NLR was higher in patients with tuberculosis compared to the patients with sarcoidosis [17].
In a study conducted on patients with tuberculosis and bacterial community-acquired pneumonia, Yoon et al. showed that NLR levels were significantly lower in patients with pulmonary tuberculosis than in patients with bacterial community-acquired pneumonia [18].
In a study conducted on patients with Behçet disease, Rifaioglu et al. demonstrated that the NLR was higher in patients with active Behçet disease compared to controls and those with inactive Behçet disease [19].
In a study conducted on patients with Sjögren's syndrome, which is a chronic inflammatory disease, NLR was found significantly higher compared to the control group [20].
Additionally, in many studies on coronary artery disease, which is also an inflammatory process, a positive correlation was found for the NLR [21, 22].
In the literature high NLR values were found in inflammatory processes compared to control. In contrast with the literature data we found low NLR in brucellosis patients compared to control. In our study we demonstrated for the first time that NLR values were significantly associated with brucellosis.
Major limit of our study was the retrospective study that was considered. Single blood sampling was the other limitation of our study. For these reasons new prospectively controlled and randomized trials with multiple blood sampling must be performed to confirm our results. In spite of that we have suggested that low NLR may be useful data for brucellosis.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Moreno E. Retrospective and prospective perspectives on zoonotic brucellosis. Frontiers in Microbiology. 2014;5, article 213 doi: 10.3389/fmicb.2014.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galińska E. M., Zagórski J. Brucellosis in humans—etiology, diagnostics, clinical forms. Annals of Agricultural and Environmental Medicine. 2013;20(2):233–238. [PubMed] [Google Scholar]
- 3.Scarano M., Pezzuoli F., Patanè S. Brucella infective endocarditis. International Journal of Cardiology. 2014;172(3):e509–e510. doi: 10.1016/j.ijcard.2014.01.110. [DOI] [PubMed] [Google Scholar]
- 4.Mantur B. G., Amarnath S. K., Shinde R. S. Review of clinical and laboratory features of human brucellosis. Indian Journal of Medical Microbiology. 2007;25(3):188–202. doi: 10.4103/0255-0857.34758. [DOI] [PubMed] [Google Scholar]
- 5.Hekmatimoghaddam S., Sadeh M., Khalili M. B., Mollaabedin M., Sazmand A. Comparison of PCR, wright agglutination test and blood culture for diagnosis of brucellosis in suspected patients. Pakistan Journal of Biological Sciences. 2013;16(22):1589–1592. doi: 10.3923/pjbs.2013.1589-1592. [DOI] [PubMed] [Google Scholar]
- 6.Lowsby R., Gomes C., Jarman I., et al. Neutrophil to lymphocyte count ratio as an early indicator of blood stream infection in the emergency department. Emergency Medicine Journal. 2014 doi: 10.1136/emermed-2014-204071. [DOI] [PubMed] [Google Scholar]
- 7.Yıldız A., Yüksel M., Oylumlu M., Polat N., Akıl M. A., Acet H. The association between the neutrophil/lymphocyte ratio and functional capacity in patients with idiopathic dilated cardiomyopathy. Anadolu Kardiyoloji Dergisi. 2015;15(1):13–17. doi: 10.5152/akd.2014.5131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imtiaz F., Shafique K., Mirza S., Ayoob Z., Vart P., Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. International Archives of Medicine. 2012;5(1, article 2) doi: 10.1186/1755-7682-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Templeton A. J., McNamara M. G., Šeruga B., et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Journal of the National Cancer Institute. 2014;106(6) doi: 10.1093/jnci/dju124.dju124 [DOI] [PubMed] [Google Scholar]
- 10.Nakano K., Hosoda M., Yamamoto M., Yamashita H. Prognostic significance of pre-treatment neutrophil: lymphocyte ratio in Japanese patients with breast cancer. Anticancer Research. 2014;34(7):3819–3824. [PubMed] [Google Scholar]
- 11.Graziosi L., Marino E., de Angelis V., Rebonato A., Cavazzoni E., Donini A. Prognostic value of preoperative neutrophils to lymphocytes ratio in patients resected for gastric cancer. American Journal of Surgery. 2014 doi: 10.1016/j.amjsurg.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Kang M. H., Go S. I., Song H. N., et al. The prognostic impact of the neutrophil-to-lymphocyte ratio in patients with small-cell lung cancer. The British Journal of Cancer. 2014;111(3):452–460. doi: 10.1038/bjc.2014.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koh Y. W., Lee H. J., Ahn J. H., Lee J. W., Gong G. Prognostic significance of the ratio of absolute neutrophil to lymphocyte counts for breast cancer patients with ER/PR-positivity and HER2-negativity in neoadjuvant setting. Tumor Biology. 2014;35(10):9823–9830. doi: 10.1007/s13277-014-2282-5. [DOI] [PubMed] [Google Scholar]
- 14.Kacan T., Babacan N. A., Seker M., et al. Could the neutrophil to lymphocyte ratio be a poor prognostic factor for non small cell lung cancers? Asian Pacific Journal of Cancer Prevention. 2014;15(5):2089–2094. doi: 10.7314/APJCP.2014.15.5.2089. [DOI] [PubMed] [Google Scholar]
- 15.Leithead J. A., Rajoriya N., Gunson B. K., Ferguson J. W. Neutrophil-to-lymphocyte ratio predicts mortality in patients listed for liver transplantation. Liver International. 2015;35(2):502–509. doi: 10.1111/liv.12688. [DOI] [PubMed] [Google Scholar]
- 16.Kuyumcu M. E., Yesil Y., Oztürk Z. A., et al. The evaluation of neutrophil-lymphocyte ratio in Alzheimer's disease. Dementia and Geriatric Cognitive Disorders. 2012;34(2):69–74. doi: 10.1159/000341583. [DOI] [PubMed] [Google Scholar]
- 17.Iliaz S., Iliaz R., Ortakoylu G., Bahadir A., Bagci B. A., Caglar E. Value of neutrophil/lymphocyte ratio in the differential diagnosis of sarcoidosis and tuberculosis. Annals of Thoracic Medicine. 2014;9(4):232–235. doi: 10.4103/1817-1737.140135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoon N.-B., Son C., Um S.-J. Role of the neutrophil-lymphocyte count ratio in the differential diagnosis between pulmonary tuberculosis and bacterial community-acquired pneumonia. Annals of Laboratory Medicine. 2013;33(2):105–110. doi: 10.3343/alm.2013.33.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rifaioglu E. N., Şen B. B., Ekiz Ö., Dogramaci A. C. Neutrophil to lymphocyte ratio in Behçet's disease as a marker of disease activity. Acta Dermatovenerologica Alpina, Pannonica, et Adriatica. 2014;23(4):65–67. [PubMed] [Google Scholar]
- 20.Hu Z. D., Sun Y., Guo J., et al. Red blood cell distribution width and neutrophil/lymphocyte ratio are positively correlated with disease activity in primary Sjögren's syndrome. Clinical Biochemistry. 2014;47(18):287–290. doi: 10.1016/j.clinbiochem.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Balta S., Demirkol S., Aparcı M., Celik T., Ozturk C. The neutrophil lymphocyte ratio in coronary heart disease. International Journal of Cardiology. 2014;176(1):p. 267. doi: 10.1016/j.ijcard.2014.06.098. [DOI] [PubMed] [Google Scholar]
- 22.He J., Li J., Wang Y., Hao P., Hua Q. Neutrophil-to- lymphocyte ratio(NLR) predicts mortality and adverse-outcomes after S T-segment elevation myocardial infarction in Chinese people. International Journal of Clinical and Experimental Pathology. 2014;7(7):4045–4056. [PMC free article] [PubMed] [Google Scholar]


