Abstract
Dengue fever and dengue haemorrhagic fever are important arthropod-borne viral diseases. Each year, there are ~50 million dengue infections and ~500,000 individuals are hospitalized with dengue haemorrhagic fever, mainly in Southeast Asia, the Pacific and the Americas. Illness is produced by any of the four dengue virus serotypes. A global strategy aimed at increasing the capacity for surveillance and outbreak response, changing behaviours and reducing the disease burden using integrated vector management in conjunction with early and accurate diagnosis has been advocated. Antiviral drugs and vaccines that are currently under development could also make an important contribution to dengue control in the future.
Dengue is the most important arthropod-borne viral infection of humans. Worldwide, an estimated 2.5 billion people are at risk of infection, approximately 975 million of whom live in urban areas in tropical and sub-tropical countries in Southeast Asia, the Pacific and the Americas1. Transmission also occurs in Africa and the Eastern Mediterranean, and rural communities are increasingly being affected. It is estimated that more than 50 million infections occur each year, including 500,000 hospitalizations for dengue haemorrhagic fever, mainly among children, with the case fatality rate exceeding 5% in some areas1–4.
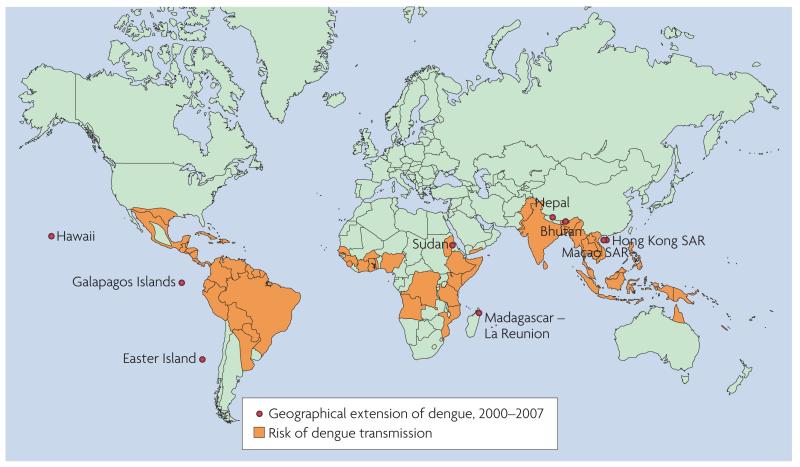
The annual average number of dengue fever/dengue haemorrhagic fever (DF/DHF) cases reported to the World Health Organization (WHO) has increased dramatically in recent years. For the period 2000–2004, the annual average was 925,896 cases, almost double the figure of 479,848 cases that was reported for the period 1990–1999. In 2001, a record 69 countries reported dengue activity to WHO and in 2002, the Region of the Americas alone reported more than 1 million cases. Although there is poor surveillance and no official reporting of dengue to WHO from countries in the African and Eastern Mediterranean regions, in 2005–2006 outbreaks of suspected dengue were recorded in Pakistan, Saudi Arabia, Yemen, Sudan and Madagascar1–4, and a large outbreak of dengue involving >17,000 cases was documented in the Cape Verde islands in 20095.Travellers from endemic areas might serve as vehicles for further spread6–9. Dengue epidemics can have a significant economic and health toll. In endemic countries in Asia and the Americas, the burden of dengue is approximately 1,300 disability-adjusted life years (DALYs) per million population, which is similar to the disease burden of other childhood and tropical diseases, including tuberculosis, in these regions10.
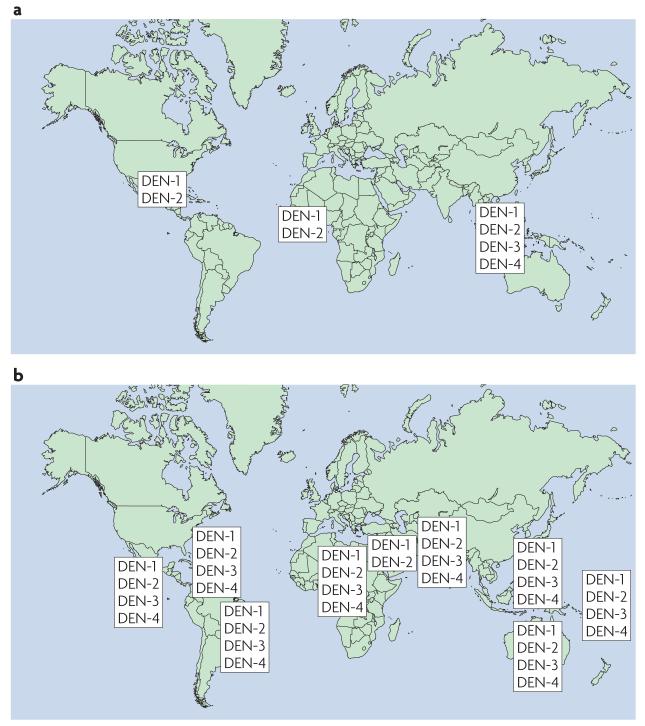
The geographical areas in which dengue transmission occurs have expanded in recent years (FIG. 1), and all four dengue virus serotypes (DENV-1–4) are now circulating in Asia, Africa and the Americas, a dramatically different scenario from that which prevailed 20 or 30 years ago (FIG. 2). The molecular epidemiology of these serotypes has been studied in an attempt to understand their evolutionary relationships11.
Figure 1. Countries and areas at risk of dengue transmission, 2007.
Data from WHO.
Figure 2. The dengue virus genome.
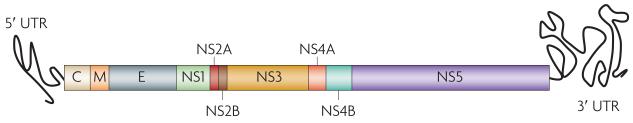
The single open reading frame encodes three structural proteins (the capsid (C), membrane (M) and envelope (E) glycoproteins) and seven non-structural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B and N55).
This Review will provide an update on our understanding of the pathogenesis of this successful pathogen, how we diagnose and control infection and the progress that has been made in vaccine development.
Dengue virus pathogenesis
Dengue viruses belong to the genus flavivirus within the Flaviviridae family. DENV-1–4 evolved in non-human primates from a common ancestor and each entered the urban cycle independently an estimated 500–1,000 years ago12. The virion comprises a spherical particle, 40–50 nm in diameter, with a lipopolysaccharide envelope. The positive single-strand RNA genome (FIG. 3), which is approximately 11 kb in length, has a single open reading frame that encodes three structural proteins — the capsid (C), membrane (M) and envelope (E) glycoproteins — and seven non-structural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B and NS5). Important biological properties of dengue viruses, including receptor binding, haemagglutination of erythrocytes and the induction of neutralizing antibodies and the protective immune response, are associated with the E glycoprotein. Each DENV shares around 65% of the genome, which is approximately the same degree of genetic relatedness as West Nile virus shares with Japanese encephalitis virus. Despite these differences, each serotype causes nearly identical syndromes in humans and circulates in the same ecological niche13.
Figure 3. The change in distribution of dengue serotypes.
The figure shows the distribution in 1970 (a) and 2004 (b). Reproduced with permission from REF. 141.
The mosquito vectors, principally Aedes aegypti, become infected when they feed on humans during the usual five-day period of viraemia. The virus passes from the mosquito intestinal tract to the salivary glands after an extrinsic incubation period, a process that takes approximately 10 days and is most rapid at high ambient temperatures14. Mosquito bites after the extrinsic incubation period result in infection, which might be promoted by mosquito salivary proteins15. In the skin, dengue viruses infect immature dendritic cells through the non-specific receptor dendritic cell-specific ICAM3-grabbing non-integrin (DC-SIGN)16. Infected dendritic cells mature and migrate to local or regional lymph nodes where they present viral antigens to T cells, initiating the cellular and humoral immune responses. There is also evidence of abundant replication of DENVs in liver parenchymal cells and in macrophages in lymph nodes, liver and spleen, as well as in peripheral blood monocytes17. Both in vitro and in vivo, macrophages and monocytes participate in antibody-dependent enhancement (ADE)18–20. ADE occurs when mononuclear phagocytes are infected through their Fc receptors by immune complexes that form between DENVs and non-neutralizing antibodies. These non-neutralizing antibodies result from previous heterotypic dengue infections or from low concentrations of dengue antibodies of maternal origin in infant sera21. The co-circulation of four DENV serotypes in a given population might be augmented by the ADE phenomenon22.
DENVs produce several syndromes that are conditioned by age and immunological status. During initial dengue infections, most children experience subclinical infection or mild undifferentiated febrile syndromes. During secondary dengue infections the pathophysiology of the disease changes dramatically, particularly sequential infections in which infection with DENV-1 is followed by infection with DENV-2 or DENV-3, or infection with DENV-3 is followed by infection with DENV-223–25. Such infections can result in an acute vascular permeability syndrome known as dengue shock syndrome (DSS). The severity of DSS is age-dependent, with vascular leakage being most severe in young children, a phenomenon that is thought to be related to the intrinsic integrity of the capillaries26,27. In adults, primary infections with each of the four DENV serotypes, particularly with DENV-1 and -3, often results in DF. Some outbreaks of primary DENV-2 infections have been predominantly subclinical24. Nonetheless, dengue infections in adults are often accompanied by a tendency for bleeding that can lead to severe haemorrhages.
Dengue infections can be life-threatening when they occur in individuals with asthma, diabetes and other chronic diseases28–30. Host factors that increase the risk of severe dengue disease include female sex, several human leukocyte antigen (HLA) class I alleles, a promoter variant of the DC-SIGN receptor gene, a single-nucleotide polymorphism in the tumour necrosis factor (TNF) gene and AB blood group31–36. Host factors that reduce the risk of severe disease during a second dengue infection include race, second or third degree malnutrition, and polymorphisms in the Fcγ receptor and vitamin D receptor genes37–42. Secondary dengue infections in adults can produce the classical DSS or severe disease complicated by haemorrhages. The severity of secondary dengue infections has been observed to increase from month-to-month during island outbreaks43; the longer the interval between the first and second infection the more severe is the accompanying disease44,45. Tertiary dengue infections can cause severe disease, but only rarely25.
In vitro studies demonstrate that the infection of human monocytes and mature dendritic cells results in increased virus replication as a result of the suppression of the interferon system45. Type I interferon-associated genes are less abundantly activated in peripheral blood mononuclear cells taken from patients with severe dengue disease compared with milder disease46. Subsequently, the increased number of infected cells present targets for CD4+ and CD8+ T cells, resulting in large quantities of interleukin (IL)-10, IL-2, interferon (IFN)-γ and TNF that, singly or in combination, might contribute to endothelial damage and altered haemostasis. Virions released from infected cells might also directly damage endothelial cells and the uptake of the non-structural protein NS1 by hepatocytes might promote viral infection of the liver47–49. During DHF, the complement cascade is also activated and the levels of the complement activation products C3a and C5a correlate with the severity of illness49. Soluble and membrane-associated NS1 have been demonstrated to activate human complement. The levels of the terminal SC5b–9 complement complex and plasma NS1 correlated with disease severity, suggesting links between the virus, complement activation and the development of DHF/DSS50. Alternative hypotheses of dengue pathogenesis include the suggestions that secondary T-cell responses are blunted because stimulation of T-cell memory results in the production of heterotypic CD4+ and CD8+ cells that have a diminished capacity to kill but nonetheless release inflammatory cytokines that contribute to disease severity51; that severe disease is caused by DENVs of increased virulence52; and the suggestion that cross-reactivity between NS1 and human platelets and endothelial cells raises antibodies that damage these cells53.
One working hypothesis of dengue pathogenesis that is consistent with the available evidence is that severe disease in infants with primary infections and in older individuals with secondary infections is the result of ADE of infection of mononuclear phagocytes. Infection by an antibody–virus complex suppresses innate immune responses, increasing intracellular infection and generating inflammatory cytokines and chemokines that, collectively, result in enhanced disease. Liver infection and a pathogenic role for NS1 add to the complexity. In patients with DF, IFN production and activated natural killer cells can limit disease severity.
Clinical signs and immunological response
Dengue-associated deaths are usually linked to DHF/ DSS. Even though no vaccines or drugs are available, severe disease can be successfully managed by careful monitoring of the warning signs and early initiation of aggressive intravenous rehydration therapy. During the early febrile stage (the symptoms of which include fever, malaise, headache, body pains and rash), clinicians cannot predict which patients will progress to severe disease. Later, during defervescence, symptoms such as bleeding, thrombocytopenia of <100,000 platelets mm−3, ascites, pleural effusion, haematocrit >20% and clinical warning signs, such as severe and continuous abdominal pain, restlessness and/or somnolence, persistent vomiting and a sudden reduction in temperature (from fever to subnormal temperature) associated with profuse perspiration, adynamia (loss of strength or vigor) and sometimes fainting, can be indicative of plasma extravasation and the imminence of shock. At this point, patients should receive fluid replacement (crystalloids) to avoid haemodynamic instability, narrowness of blood pressure and hypotension. Early resuscitation can prevent other complications, such as massive haemorrhage, disseminated intravascular coagulation, multiple organ failure, and respiratory failure due to non-cardiogenic pulmonary oedema54–57. Treatment of uncomplicated dengue cases is only supportive, including plenty of oral fluids during the febrile period and paracetamol (acetaminophen), the daily dosage of which should not be exceeded to prevent intoxication mainly related to liver function. When dengue shock becomes prolonged or recurrent, intravenous fluids should be given carefully according to age and dosage to prevent fluid overload as this can result in pulmonary oedema.
Recent publications have suggested that the WHO syndromic case definition of DHF/DSS should be evaluated for clinical utility58–62. A prospective multi-centre study in several Latin-American and Southeast asian countries is planned that will provide standardized descriptions of dengue clinical presentations in the context of the current WHO case definitions.
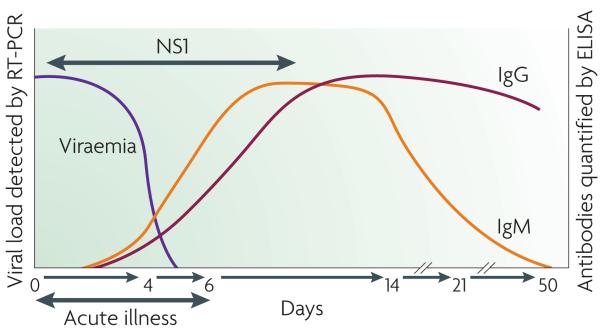
The acquired immune response to dengue infection consists of the production of antibodies that are primarily directed against the virus envelope proteins. The response varies depending on whether it is a primary or secondary infection63,64. A primary antibody response is seen in individuals who are not immune to dengue and a secondary immune response is observed in patients who have had a previous dengue infection (FIG. 4). A primary infection is characterized by a slow and low-titre antibody response. Immunoglobulin (Ig)M antibodies are the first isotype to appear, by day 3–5 of illness in 50% of hospitalized patients and by day 6–10 of illness in 93–99% of cases. The IgM levels peak ~2 weeks after the onset of fever and then generally decline to undetectable levels over the next 2–3 months54,55,65. Dengue-specific IgG is detectable at low titre at the end of the first week of illness and slowly increases. By contrast, during a secondary infection, high levels of IgG antibodies that crossreact with many flaviviruses are detectable even in the acute phase and rise dramatically over the following 2 weeks65. The kinetics of the IgM response are more variable; as IgM levels are significantly lower in secondary dengue infections, false-negative test results for dengue-specific IgM have been reported during secondary infections55,66,67. Following a dengue infection, IgG can be lifelong, which complicates the serodiagnosis of past, recent and current infections65,67. IgA and IgE responses have also been documented but the utility of detecting these immunoglobulins as markers for dengue serodiagnosis requires further study68.
Figure 4. Dengue virus, antigen and antibody responses used in diagnosis.
Ig, immunoglobulin; NS, non-structural.
In areas where two or more flaviviruses are circulating, multiple and sequential flavivirus infections make differential diagnosis difficult owing to the presence of pre-existing antibodies and the phenomenon of original antigenic sin (during sequential flavivirus infections, B-cell clones responding to the first infection synthesize antibodies with higher affinity for the first infecting virus than for the second infecting virus)69.
Laboratory diagnosis of dengue infection
Laboratory confirmation of dengue infection is crucial as the broad spectrum of clinical presentations, ranging from mild febrile illness to several severe syndromes, can make accurate diagnosis difficult. Among the methods available for dengue diagnosis, virus isolation provides the most specific test result. However, facilities that can support viral culture are not always available. The detection of the viral genome or viral antigens also provides evidence of infection.
Seroconversion of IgM or IgG antibodies is the standard for serologically confirming a dengue infection. The presence of IgM or high levels of IgG in acute serum collected from a suspected dengue case suggests a probable dengue infection54,55. BOX 1 shows the laboratory criteria for confirmed and probable dengue infections.
Box 1. Laboratory diagnosis of a dengue virus infection.
Confirmed dengue infection
Virus isolation
Genome detection
Antigen detection
IgM or IgG seroconversion
Probable dengue infection
IgM positive
Elevated IgG titre (that is, 1,280 or greater by haemagglutination inhibition test)
Virus isolation
The Aedes albopictus mosquito C6/36 cell line is the method of choice for DENV isolation, although other mosquito (such as Aedes pseudoscutellaris AP61) and mammalian (including Vero cells, LLC-MK2 cells and BHK21 cells) cell lines can also be used70,71. Sera that have been collected from suspected dengue cases in the first 3–5 days of fever (the viraemic phase) can be used for virus isolation. After an incubation period permitting virus replication, viral identification is performed using dengue-specific monoclonal antibodies in immunofluorescence and PCR assays63,64,72,73. Serum is often used for virus isolation but plasma, leukocytes, whole blood and tissues obtained at autopsy can also be used63,74,75.
Serological testing
Serological assays are most commonly used for diagnosis of dengue infection as they are relatively inexpensive and easy to perform compared with culture or nucleic acid-based methods. When a dengue infection occurs in individuals who have experienced a previous dengue infection, a secondary immune response occurs, which generates high levels of IgG through the stimulation of memory B cells from the previous infection as well as an IgM response to the current infection. Because high levels of IgG compete with IgM for antigen binding, an IgM capture assay can be used.
MAC-ELISA
The Armed Forces Research Institute of Medical Sciences (AFRIMS) developed an IgM antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA) for dengue in regions where dengue and Japanese encephalitis virus co-circulate65. Today, many groups have developed their own in-house MAC-ELISAs. Dengue-specific IgM in the test serum is detected by first capturing all IgM using human-specific IgM bound to a solid phase. The assay uses a mixture of four dengue antigens (usually derived from dengue virus-infected cell culture supernatants or infected suckling mouse brain preparations)76. Compared to the haemagglutination inhibition assay as the gold standard, MAC-ELISA shows a sensitivity and specificity of 90% and 98%, respectively, in samples collected after 5 days of fever55. In addition to serum, dengue-specific IgM can be detected in whole blood on filter paper (sensitivity 98.1% and specificity 98.5%)77,78 and in saliva (sensitivity 90.3% and specificity 92.0%)79, but not in urine68. More than 50 commercial kits are available with variable sensitivity and specificity65,80–82. False-positive results due to dengue-specific IgG and crossreactivity with other flaviviruses is a limitation of the MAC-ELISA, mainly in regions where multiple flaviviruses co-circulate. Some tests also show non-specific reactivity in sera from patients with malaria and leptospirosis82.
IgG ELISA
An ELISA for dengue-specific IgG detection can be used to confirm a dengue infection in paired sera. It is also widely used to classify primary or secondary infections53,54,63,64. Some protocols use serum dilutions to titre dengue-specific IgG83 and others use the ratio of IgM to IgG66,84. The assay uses the same dengue antigens as MAC-ELISA and it correlates with results from the haemagglutination inhibition assay. In general, an IgG ELISA lacks specificity within the flavivirus serocomplex groups, however it has been demonstrated that the IgG response to the prM membrane glycoprotein is specific to individual flaviviruses as no crossreactivity was observed in sera collected from individuals infected with dengue or Japanese encephalitis virus85. Similarly, it has been demonstrated that IgG specific for the NS5 protein can potentially discriminate between infections caused by West Nile, dengue and St Louis encephalitis viruses86. Finally, dengue-specific IgG was shown to have high specificity in an assay using a recombinant polypeptide located in the N-terminal region of the envelope protein87. IgG assays are also useful for sero-epidemiological studies to identify past dengue infection.
IgM:IgG ratio
A dengue virus E and M protein-specific IgM:IgG ratio can be used to distinguish primary from secondary dengue virus infections. IgM capture and IgG capture ELISAs are the most common assays for this purpose. According to this method, a dengue infection is defined as a primary infection if the IgM:IgG OD ratio is greater than 1.2 (using patient sera at 1:100 dilution) or 1.4 (using patient sera at 1:20 dilution), or as a secondary infection if the ratio is less than 1.2 or 1.4 (REFS 88,89). However, in a recent publication the authors indicated that the IgM:IgG ratio varies depending on whether the patient has a serologically non-classical or classical dengue infection, and redefined the ratios84. Hence the cut-off for the IgM:IgG ratio is not well defined.
Neutralization assays
The plaque reduction neutralization technique (PRNT) and the micro-neutralization assay are used to define the infecting serotypes following a primary infection. These tests are mainly for research and vaccine studies90–94.
Nucleic acid amplification tests
Many nucleic acid amplification tests (NAATs) have been developed for the diagnosis of dengue infection. Some techniques are quantitative and others can be used for serotyping. However, none has been commercialised to date and quality assurance materials are not widely available to ensure the quality of the results.
Reverse transcriptase PCR (RT-PCR)
Many dengue RT-PCR assays have been described in the past 10 years. These in-house assays target different genes and use different amplification procedures. The most commonly used NAATs are based on a single RT-PCR assay95,96, a nested RT-PCR assay96 or a one-step multiplex RT-PCR assay97. The nested PCR reaction involves an initial reverse transcription and amplification step using dengue primers that target a conserved region of the virus genome followed by a second amplification step that is serotype specific. The products of these reactions are separated by electrophoresis on an agarose gel, which allows the dengue serotypes to be differentiated on the basis of size. The sensitivity of RT-PCR assays in comparison to virus isolation in mosquito cell culture varies between 25% and 79%98.
Real-time RT-PCR
The real-time RT-PCR assay is a one-step assay that allows virus titre to be quantified in approximately 1.5 hours. The detection of the amplified target by fluorescent probes replaces the need for post-amplification electrophoresis. Many real-time RT-PCR assays have been developed that are either ‘singleplex’, detecting one single serotype per reaction, or ‘multiplex’, identifying all four serotypes from a single sample99–101. One advantage of this assay is the ability to determine viral titre early in dengue illness, which is believed to be an important predictor of disease severity102.
Nucleic acid-sequence based amplification assay (NASBA)
The NASBA assay is an isothermal RNA-specific amplification assay that has been adapted for dengue virus. Its performance is comparable to that of other NAATs103.
Antigen detection
Dengue antigens can be detected in tissues such as liver, spleen and lymph nodes as well as tissues from fatal cases (slides from paraffin-embedded, fresh or frozen tissues) using an enzyme and a colorimetric substrate with antibodies that target dengue-specific antigens104–106.
NS1 antigen and antibody detection
NS1 is a glycoprotein produced by all flaviviruses and is essential for viral replication and viability. Because this protein is secreted into the bloodstream, many tests have been developed to diagnose DENV infections using NS1. These tests include antigen-capture ELISA, lateral flow antigen detection and measurement of NS1-specific IgM and IgG responses. NS1 antigen detection kits are now commercially available. As yet, these kits do not differentiate between the different DENV serotypes. Additional independent studies are needed to confirm the performance of these kits and to further validate the diagnostic and prognostic significance of NS1 and NS1-specific antibody detection107–109.
Dengue control and prevention strategies
A global strategy for dengue prevention and control was promulgated more than 10 years ago and comprises five major elements (BOX 2).
Box 2. The global strategy for dengue prevention and control.
Vector control, based on the principles of integrated vector management
Active disease surveillance based on a comprehensive health information system
Emergency preparedness
Capacity building and training
Vector control research
Efforts have since been made to focus on three fundamental aspects: surveillance for planning and response, reducing the disease burden and changing behaviours to improve vector control110. The 2002 World Health Assembly Resolution urged greater commitment among Member States and WHO to implement this strategy111. Of particular significance is the 2005 revision of the International Health Regulations112, which includes mention of DF (and yellow fever) as an example of a health ‘event that may constitute a public health emergency of international concern’ and which, under such circumstances, should be notified to WHO.
In recent years several new, improved or validated tools and strategies for dengue control and prevention have been developed and are available to public health practitioners and clinicians (BOX 3).
Box 3. Tools and resources for dengue control and prevention.
Rapid commercial diagnostic tests in use in endemic countries
Pocket Book of Hospital Care for Children (inclusion of dengue in the management of fever)137
An audiovisual guide and transcript for health care workers responding to outbreaks138
Guidelines for planning social mobilization and communication139
Global strategic framework for integrated vector management140
TDR–Wellcome Trust CD-ROM. Topics in International Health Series: dengue
Entomological survey to identify the most productive container habitats of the vector(s)116
Seven insecticide products evaluated by WHO as mosquito larvicides (five insect growth regulators and two bacterial larvicides), four of which are approved for use in drinking water and three for space spray applications to control mosquitoes
Advances in the development and operational deployment of DengueNet (http://apps.who.int/globalatlas/default.asp) for global dengue surveillance
International Health Regulations 2005 (REF. 112): voluntary compliance in effect
Planning Social Mobilization and Communication for Dengue Fever Prevention and Control: A Step-by-Step Guide139
Vector control
To reduce or prevent dengue virus transmission there is currently no alternative to vector control. Most endemic countries have a vector control component in their dengue control and prevention programmes but its delivery by public health practitioners is frequently insufficient, ineffective or both.
Given its behaviour and generally close association with humans, the principal vector A. aegypti requires the use of a combination of vector-control methods, notably environmental management methods and chemical control methods based on the application of larvicides and adulticide space sprays113. Chemical controls typically must be added to water stored for domestic use, including drinking water. The active ingredients of four larvicides have been assessed by the International Programme on Chemical Safety (IPCS) to determine their safety for use as mosquito larvicides in drinking water at dosages that are effective against Aedes spp. larvae. Since the early 1970s the organophosphate temephos has been widely used, but increasing levels of resistance114,115, householders’ rejection of the treatment of their drinking water, and difficulties in achieving high and regular levels of coverage are important technical and operational constraints.
Biological control agents, including larvivorous fish and copepods, have had a demonstrable role in controlling A. aegypti116,117, but operational difficulties — particularly the lack of facilities and expertise in mass rearing, and the need to frequently re-introduce these agents into some container habitats — have largely precluded their widespread use.
Environmental management is generally considered to be an essential component of dengue prevention and control, particularly when targeting the most productive container habitats of the vector118. Source reduction, ‘cleanup’ campaigns, regular container emptying and cleaning (targeting not only households but also public spaces such as cemeteries, green areas and schools), installation of water supply systems, solid waste management and urban planning all fall under the rubric of environmental management. However, huge investments in infrastructure are needed to increase access to safe and reliable water supplies and solid waste disposal systems. In addition to overall health gains, such provision would clearly have a major impact on vector ecology, although the relationship is complex. For instance, cost recovery mechanisms, such as the introduction of metered water, might actually encourage the household collection and storage of roof catchment rainwater, which can be harvested at no cost. Although not studied carefully, the construction of community water distribution services to rural townships and villages might be contributing to the rural spread of dengue in Southeast Asia and elsewhere by facilitating domestic water storage. When decisions on such infrastructure development are being made, the views of Ministers of Public Health and municipal health departments are seldom voiced loudly, even when the economic and public health burden of diseases linked to water and sanitation are recognized, including those associated with dengue.
Most efforts in vector control are centred at the household and community levels, but with few exceptions, the achievements to date have been largely unspectacular and there have been difficulties in scaling up from the project level119. Nevertheless, such community-based interventions are widely seen as the most promising way of improving delivery and achieving long-term control of the vector through behaviour change. Towards this end, a TDR/WHO guide for planning social mobilization and communication for dengue fever prevention and control has been developed113. Additionally, new ‘consumer-friendly’ tools such as window curtains and water container covers treated with long-lasting insecticide are being tested120 as well as controlled release larvicides that provide several months of control following a single application to targeted containers.
Products for personal and household protection have a huge potential for household pest control. Generally speaking, these commercial products tend to be used by consumers not so much in response to any perceived public health concerns, but to alleviate the nuisance of biting mosquitoes and in some settings households are prepared to spend substantial amounts of money on these products121.
With the increased political recognition of dengue as a public health problem and commitment to prevention and control, better organized control services using new tools and partnership strategies, based on the principles of integrated vector management, are likely to have a major impact on dengue transmission2.
Vaccine development
As a result of the failure of vector control, the continuing spread and increasing intensity of dengue has renewed interest and investment in dengue vaccine development, making a safe, effective and affordable tetravalent dengue vaccine a global public health priority122. Dengue vaccine development has been in progress for several decades, however the complex pathology of the illness, the need to control four virus serotypes simultaneously and insufficient investment by vaccine developers have hampered progress122.
The observation that DHF/DSS is associated with DENV secondary infection poses a special challenge to the development of a dengue vaccine, leading to a requirement that such vaccines should induce a robust immune response against the four serotypes in naive as well as previously immune individuals. Animal models are only partially useful for vaccine evaluation. The poor understanding of the mechanisms involved in inducing protective immunity against dengue infection poses additional challenges123. Finally, cases of DHF/DSS have recently been documented 20 or more years after primary dengue infection, which adds a new dimension to the problem25,44.
The available data suggest that neutralizing antibodies are the major contributors to protective immunity124,125, however the role of the cellular immune response requires further study123. In this context, clinical trials are crucial for vaccine development owing to the unique information they provide on immune responses and reactogenicity. Also, long-term observations of vaccinated populations will be required to demonstrate the absence of ADE or severe disease.
The ideal dengue vaccine should be free of important reactogenicity, induce life-long protection against infection with any of the four DENV serotypes and be affordable126,127. Vaccine candidates should be evaluated in population-based efficacy trials in several at-risk populations in different geographical settings including Asia and the Americas, which experience different patterns of dengue transmission intensity and dengue virus circulation122. Vaccine developers are working with the Pediatric Dengue Vaccine Initiative (PDVI) to establish suitable field sites. Developers are also working with the WHO Initiative for Vaccine Research (WHO/ IVR) to define the immunological correlates for protection and clinical trial design. Because of the important role of neutralizing antibodies as surrogates of protection, the validation of neutralization tests is a priority128. Current approaches to vaccine development involve using live attenuated viruses, inactivated viruses, subunit vaccines, DNA vaccines, cloned engineered viruses and chimeric viruses using yellow fever vaccine and attenuated dengue viruses as backbones129–134. TABLE 1 summarizes the most advanced vaccine candidates.
Table 1. Selected dengue vaccine candidates.
| Vaccine approach | Developer | Status |
|---|---|---|
| Live attenuated tetravalent chimeric YF–DEN vaccine | Sanofi Pasteur | Phase II |
| Live attenuated tetravalent viral isolate vaccine | WRAIR and GSK | Phase II |
| Live attenuated chimeric DEN2–DEN vaccine | CDC and Inviragen | Phase I |
| Recombinant E subunit vaccine | Merck | Phase I |
| Live attenuated tetravalent vaccine comprising 3′ deletion mutations and DEN–DEN chimeras | US NIH LID and NIAID | Phase I |
| Subunit recombinant antigen (domain III) vaccine | IPK/CIGB | Preclinical |
| Live attenuated chimeric YF–DEN vaccine | Oswaldo Cruz Foundation | Preclinical |
| Tetravalent DNA vaccine | US NMRC and GenPhar | Preclinical |
| Purified inactivated tetravalent vaccine | WRAIR and GSK | Preclinical |
CDC, Centers for Disease Control and Prevention; CIGB, Center for Genetic Engineering and Biotechnology; GSK, GlaxoSmithKline; IPK, Pedro Kouri Tropical Medicine Institute; NIAID, National Institute for Allergy and Infectious Diseases; US NIH LID, United States National Institutes of Health Laboratory of Infectious Diseases; US NMRC, United States Naval Medical Research Center; WRAIR, Walter Reed Army Institute of Research; YF, yellow fever.
Significant progress in the development of dengue vaccine candidates has been achieved lately135,136. An Acambis/Sanofi Pasteur yellow fever–dengue chimeric vaccine is in advanced Phase II testing in children in Thailand and others are in Phase 1 or advanced preclinical evaluation. It is expected that a licensed vaccine will be available in less than 10 years.
Conclusions
Dengue is now a global threat and is endemic or epidemic in almost every country located in the tropics. While we wait for new tools such as vaccines, antiviral drugs and improved diagnostics, better use should be made of the interventions that are currently available. The challenge that awaits us in the near future will be how to scale up to deploy these new tools.
In recent years, several partnerships such as the PDVI, the Innovative Vector Control Consortium, the Asia-Pacific Dengue Prevention Partnership and the European union’s DENFRAME and DENCO projects have come into existence, receiving funding from the Bill and Melinda Gates Foundation, regional Development Banks and the private sector. These partnerships are working with WHO and national governments to develop new tools and strategies to improve diagnostics and clinical treatments and to achieve a successful vaccine.
Acknowledgements
We thank Izabela Suder-Dayao for excellent secretarial assistance and Martine Guillerm for support.
References
- 1.WHO . WHO; Geneva, Switzerland: 2007. Scientific Working Group Report on Dengue. [online] < http://apps.who.int/tdr/publications/tdr-research-publications/swg-report-dengue/pdf/swg_dengue_2.pdf>. [Google Scholar]
- 2.TDR/WHO . Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. TDR/WHO; Geneva, Switzerland: 2009. [PubMed] [Google Scholar]
- 3.Guzman MG, Kouri G. Dengue: an update. Lancet Infect. Dis. 2002;2:33–42. doi: 10.1016/s1473-3099(01)00171-2. [DOI] [PubMed] [Google Scholar]
- 4.Gubler DJ. The changing epidemiology of yellow fever and dengue, 1900 to 2003: full circle? Comp. Immunol. Microbiol. Infect. Dis. 2004;27:319–330. doi: 10.1016/j.cimid.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Franco L, et al. Recent expansion of dengue virus serotype 3 in West Africa. Euro Surveill. 2010;15:19490. 9ii. [PubMed] [Google Scholar]
- 6.Wilder-Smith A. Dengue in travelers. New Engl. J. Med. 2005;353:924–932. doi: 10.1056/NEJMra041927. [DOI] [PubMed] [Google Scholar]
- 7.Freedman DO, et al. Spectrum of disease and relation to place of exposure among ill returned travelers. New Engl. J. Med. 2006;354:119–130. doi: 10.1056/NEJMoa051331. [DOI] [PubMed] [Google Scholar]
- 8.Wichmann O. Dengue antibody prevalence in German travelers. Emerg. Infect. Dis. 2005;11:762–765. doi: 10.3201/eid1105.050097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jelinek T. Dengue fever in international travelers. Clin. Infect. Dis. 2000;31:144–147. doi: 10.1086/313889. [DOI] [PubMed] [Google Scholar]
- 10.Gubler DJ, Meltzer M. Impact of dengue/dengue hemorrhagic fever on the developing world. Adv. Virus Res. 1999;53:35–70. doi: 10.1016/s0065-3527(08)60342-5. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez-Roche R, et al. Virus evolution during a severe dengue epidemic in Cuba, 1997. Virology. 2005;334:154–159. doi: 10.1016/j.virol.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 12.Wang E, et al. Evolutionary relationships of endemic/ epidemic and sylvatic dengue viruses. J. Virol. 2000;74:3227–3234. doi: 10.1128/jvi.74.7.3227-3234.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halstead SB. Dengue virus–mosquito interactions. Annu. Rev. Entomol. 2008;53:273–291. doi: 10.1146/annurev.ento.53.103106.093326. [DOI] [PubMed] [Google Scholar]
- 14.Watts DM, Burke DS, Harrison BA, Whitmire RE, Nisalak A. Effect of temperature on the vector efficiency of Aedes aegypti for dengue 2 virus. Am. J. Trop. Med. Hyg. 1987;36:143–152. doi: 10.4269/ajtmh.1987.36.143. [DOI] [PubMed] [Google Scholar]
- 15.Schneider BS, Soong L, Zeidner NS, Higgs S. Aedes aegypti salivary gland extracts modulate antiviral and TH1/TH2 cytokine responses to Sindbis virus infection. Viral Immunol. 2004;17:565–573. doi: 10.1089/vim.2004.17.565. [DOI] [PubMed] [Google Scholar]
- 16.Wu SJ, et al. Human skin Langerhans cells are targets of dengue virus infection. Nature Med. 2000;6:816–820. doi: 10.1038/77553. [DOI] [PubMed] [Google Scholar]
- 17.Jessie K, Fong MY, Devi S, Lam SK, Wong KT. Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J. Infect. Dis. 2004;189:1411–1418. doi: 10.1086/383043. [DOI] [PubMed] [Google Scholar]
- 18.Halstead SB, O’Rourke EJ. Dengue viruses and mononuclear phagocytes. I. Infection enhancement by non-neutralizing antibody. J. Exp. Med. 1977;146:201–217. doi: 10.1084/jem.146.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Halstead SB. In vivo enhancement of dengue virus infection in rhesus monkeys by passively transferred antibody. J. Infect. Dis. 1979;140:527–533. doi: 10.1093/infdis/140.4.527. [DOI] [PubMed] [Google Scholar]
- 20.Goncalvez AP, Engle RE, St. Claire M, Purcell RH, Lai CJ. Monoclonal antibody-mediated enhancement of dengue virus infection in vitro and in vivo and strategies for prevention. Proc. Natl Acad. Sci. USA. 2007;104:9422–9427. doi: 10.1073/pnas.0703498104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kliks SC, Nimmanitya S, Nisalak A, Burke DS. Evidence that maternal dengue antibodies are important in the development of dengue hemorrhagic fever in infants. Am. J. Trop. Med. Hyg. 1988;38:411–419. doi: 10.4269/ajtmh.1988.38.411. [DOI] [PubMed] [Google Scholar]
- 22.Cummings DAT, Schwartz IB, Billings L, Shaw LB, Burke DS. Dynamic effects of antibody-dependent enhancement on the fitness of viruses. Proc. Natl Acad. Sci. USA. 2005;102:15259–15264. doi: 10.1073/pnas.0507320102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guzman MG, et al. Dengue hemorrhagic fever in Cuba, 1981: a retrospective seroepidemiologic study. Am. J. Trop. Med. Hyg. 1990;42:179–184. doi: 10.4269/ajtmh.1990.42.179. [DOI] [PubMed] [Google Scholar]
- 24.Guzman MG, et al. Epidemiologic studies on Dengue in Santiago de Cuba, 1997. Am. J. Epidemiol. 2000;152:793–799. doi: 10.1093/aje/152.9.793. discussion 804. [DOI] [PubMed] [Google Scholar]
- 25.Alvarez M, et al. Dengue hemorrhagic fever caused by sequential dengue 1–3 virus infections over a long time interval: Havana epidemic, 2001–2002 Am. J. Trop. Med. Hyg. 2006;75:1113–1117. [PubMed] [Google Scholar]
- 26.Guzman MG, et al. Effect of age on outcome of secondary dengue 2 infections. Int. J. Infect. Dis. 2002;6:118–124. doi: 10.1016/s1201-9712(02)90072-x. [DOI] [PubMed] [Google Scholar]
- 27.Gamble J, et al. Age-related changes in microvascular permeability: a significant factor in the susceptibility of children to shock? Clin. Sci. 2000;98:211–216. [PubMed] [Google Scholar]
- 28.Kouri GP, Guzman MG, Bravo JR. Why dengue haemorrhagic fever in Cuba? 2. An integral analysis. Trans. R. Soc. Trop. Med. Hyg. 1987;81:821–823. doi: 10.1016/0035-9203(87)90042-3. [DOI] [PubMed] [Google Scholar]
- 29.Halstead SB, Nimmannitya S, Cohen SN. Observations related to pathogenesis of dengue hemorrhagic fever. IV. Relation of disease severity to antibody response and virus recovered. Yale J. Biol. Med. 1970;42:311–328. [PMC free article] [PubMed] [Google Scholar]
- 30.Lee MS, Hwang KP, Chen TC, Lu PL, Chen TP. Clinical characteristics of dengue and dengue hemorrhagic fever in a medical center of southern Taiwan during the 2002 epidemic. J. Microbiol. Immunol. Infect. 2006;39:121–129. [PubMed] [Google Scholar]
- 31.Stephens HA, et al. HLA-A and -B allele associations with secondary dengue virus infections correlate with disease severity and the infecting viral serotype in ethnic Thais. Tissue Antigens. 2002;60:309–318. doi: 10.1034/j.1399-0039.2002.600405.x. [DOI] [PubMed] [Google Scholar]
- 32.LaFleur C, et al. HLA-DR antigen frequencies in Mexican patients with dengue virus infection: HLA-DR4 as a possible genetic resistance factor for dengue hemorrhagic fever. Hum. Immunol. 2002;63:1039–1044. doi: 10.1016/s0198-8859(02)00682-1. [DOI] [PubMed] [Google Scholar]
- 33.Loke H, et al. Strong HLA class I-restricted T cell responses in dengue hemorrhagic fever: a double-edged sword? J. Infect. Dis. 2001;184:1369–1373. doi: 10.1086/324320. [DOI] [PubMed] [Google Scholar]
- 34.Sakuntabhai A, et al. A variant in the CD209 promoter is associated with severity of dengue disease. Nature Genet. 2005;37:507–513. doi: 10.1038/ng1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandez-Mestre MT, Gendzekhadze K, Rivas-Vetencourt P, Layrisse Z. TNF-α-308A allele, a possible severity risk factor of hemorrhagic manifestation in dengue fever patients. Tissue Antigens. 2004;64:469–472. doi: 10.1111/j.1399-0039.2004.00304.x. [DOI] [PubMed] [Google Scholar]
- 36.Kalayanarooj S, et al. Blood group AB is associated with increased risk for severe dengue disease in secondary infections. J. Infect. Dis. 2007;195:1014–1017. doi: 10.1086/512244. [DOI] [PubMed] [Google Scholar]
- 37.Bravo JR, Guzman MG, Kouri GP. Why dengue haemorrhagic fever in Cuba? 1. Individual risk factors for dengue haemorrhagic fever/dengue shock syndrome (DHF/DSS) Trans. R. Soc. Trop. Med. Hyg. 1987;81:816–820. doi: 10.1016/0035-9203(87)90041-1. [DOI] [PubMed] [Google Scholar]
- 38.Thisyakorn U, Nimmannitya S. Nutritional status of children with dengue hemorrhagic fever. Clin. Infect. Dis. 1993;16:295–297. doi: 10.1093/clind/16.2.295. [DOI] [PubMed] [Google Scholar]
- 39.Loke H, et al. Susceptibility to dengue hemorrhagic fever in vietnam: evidence of an association with variation in the vitamin D receptor and Fc gamma receptor IIa genes. Am. J. Trop. Med. Hyg. 2002;67:102–106. doi: 10.4269/ajtmh.2002.67.102. [DOI] [PubMed] [Google Scholar]
- 40.Sierra BD, et al. Ethnicity and difference in dengue virus-specific memory T cell responses in cuban individuals. Viral Immunol. 2006;19:662–668. doi: 10.1089/vim.2006.19.662. [DOI] [PubMed] [Google Scholar]
- 41.Sierra BD, Kouri G, Guzman MG. Race: a risk factor for dengue hemorrhagic fever. Arch. Virol. 2007;152:533–534. doi: 10.1007/s00705-006-0869-x. [DOI] [PubMed] [Google Scholar]
- 42.Halstead SB, et al. Haiti: absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. Am. J. Trop. Med. Hyg. 2001;65:180–183. doi: 10.4269/ajtmh.2001.65.180. [DOI] [PubMed] [Google Scholar]
- 43.Guzman MG, Kouri G, Halstead SB. Do escape mutants explain rapid increases in dengue case-fatality rates within epidemics? Lancet. 2000;355:1902–1903. doi: 10.1016/S0140-6736(00)02303-5. [DOI] [PubMed] [Google Scholar]
- 44.Guzman MG, et al. Enhanced severity of secondary dengue-2 infections: death rates in 1981 and 1997 Cuban outbreaks. Rev. Panam. Salud Pública. 2002;11:223–227. doi: 10.1590/s1020-49892002000400003. [DOI] [PubMed] [Google Scholar]
- 45.Chareonsirisuthigul T, Kalayanarooj S, Ubol S. Dengue virus (DENV) antibody-dependent enhancement of infection upregulates the production of anti-inflammatory cytokines, but suppresses anti-DENV free radical and pro-inflammatory cytokine production, in THP-1 cells. J. Gen. Virol. 2007;88:365–375. doi: 10.1099/vir.0.82537-0. [DOI] [PubMed] [Google Scholar]
- 46.Simmons CP, et al. Patterns of host genome-wide gene transcript abundance in the peripheral blood of patients with acute dengue hemorrhagic fever. J. Infect. Dis. 2007;195:1097–1107. doi: 10.1086/512162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Couvelard A, et al. Report of a fatal case of dengue infection with hepatitis: demonstration of dengue antigens in hepatocytes and liver apoptosis. Hum. Pathol. 1999;30:1106–1110. doi: 10.1016/s0046-8177(99)90230-7. [DOI] [PubMed] [Google Scholar]
- 48.Alcon-LePoder S, et al. The secreted form of dengue virus nonstructural protein NS1 is endocytosed by hepatocytes and accumulates in late endosomes: implications for viral infectivity. J. Virol. 2005;79:11403–11411. doi: 10.1128/JVI.79.17.11403-11411.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Malasit P. Complement and dengue haemorrhagic fever/shock syndrome. Southeast Asian J. Trop. Med. Pub. Health. 1987;18:316–320. [PubMed] [Google Scholar]
- 50.Avirutnan P, et al. Vascular leakage in severe dengue virus infections: a potential role for the nonstructural viral protein NS1 and complement. J. Infect. Dis. 2006;193:1078–1088. doi: 10.1086/500949. [DOI] [PubMed] [Google Scholar]
- 51.Mongkolsapaya J, et al. Original antigenic sin and apoptosis in the pathogenesis of dengue hemorrhagic fever. Nature Med. 2003;9:921–927. doi: 10.1038/nm887. [DOI] [PubMed] [Google Scholar]
- 52.Rico-Hesse R. Microevolution and virulence of dengue viruses. Adv. Virus Res. 2003;59:315–341. doi: 10.1016/s0065-3527(03)59009-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin CF, Wan SW, Cheng HJ, Lei HY, Lin YS. Autoimmune pathogenesis in dengue virus infection. Viral Immunol. 2006;19:127–132. doi: 10.1089/vim.2006.19.127. [DOI] [PubMed] [Google Scholar]
- 54.TDR/WHO . Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. TDR/WHO; Geneva, Switzerland: 2009. pp. 23–55. [PubMed] [Google Scholar]
- 55.PAHO . Dengue and Dengue Hemorrhagic Fever in the Americas: Guidelines for Prevention and Control. Pan American Health Organization; Washington, DC, USA: 1994. [Google Scholar]
- 56.Nimmannitya S. Clinical spectrum and management of dengue haemorrhagic fever. Southeast Asian J. Trop. Med. Pub. Health. 1987;18:392–397. [PubMed] [Google Scholar]
- 57.Martinez Torres E. Preventing deaths from dengue: a space and challenge for primary health care. Rev. Panam. Salud Pública. 2006;20:60–74. doi: 10.1590/s1020-49892006000700013. [DOI] [PubMed] [Google Scholar]
- 58.Bandyopadhyay S, Lum LC, Kroeger A. Classifying dengue: a review of the difficulties in using the WHO case classification for dengue haemorrhagic fever. Trop. Med. Int. Health. 2006;11:1238–1255. doi: 10.1111/j.1365-3156.2006.01678.x. [DOI] [PubMed] [Google Scholar]
- 59.Rigau-Perez JG. Severe dengue: the need for new case definitions. Lancet Infect. Dis. 2006;6:297–302. doi: 10.1016/S1473-3099(06)70465-0. [DOI] [PubMed] [Google Scholar]
- 60.Deen JL, et al. The WHO dengue classification and case definitions: time for a reassessment. Lancet. 2006;368:170–173. doi: 10.1016/S0140-6736(06)69006-5. [DOI] [PubMed] [Google Scholar]
- 61.Balmaseda A. Assessment of the World Health Organization scheme for classification of dengue severity in Nicaragua. Am. J. Trop. Med. Hyg. 2005;73:1059–1062. [PubMed] [Google Scholar]
- 62.Thangaratham PS, Tyagi BK. Indian perspective on the need for new case definitions of severe dengue. Lancet Infect. Dis. 2007;7:81–82. doi: 10.1016/S1473-3099(07)70005-1. [DOI] [PubMed] [Google Scholar]
- 63.Vorndam V, Kuno G. In: Dengue and Dengue Hemorrhagic Fever. Gubler DJ, Kuno G, editors. CAB International; New York, USA: 1997. pp. 313–333. [Google Scholar]
- 64.Guzman MG, Kouri G. Dengue diagnosis, advances and challenges. Int. J. Infect. Dis. 2004;8:69–80. doi: 10.1016/j.ijid.2003.03.003. [DOI] [PubMed] [Google Scholar]
- 65.Innis BL, et al. An enzyme-linked immunosorbent assay to characterize dengue infections where dengue and Japanese encephalitis co-circulate. Am. J. Trop. Med. Hyg. 1989;40:418–427. doi: 10.4269/ajtmh.1989.40.418. [DOI] [PubMed] [Google Scholar]
- 66.Chanama S, et al. Analysis of specific IgM responses in secondary dengue virus infections: levels and positive rates in comparison with primary infections. J. Clin. Virol. 2004;31:185–189. doi: 10.1016/j.jcv.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 67.Gubler DJ. Serologic diagnosis of dengue/dengue haemorrhagic fever. Dengue Bull. 1996;20:20–23. [Google Scholar]
- 68.Vazquez S, et al. Kinetics of antibodies in sera, saliva, and urine samples from adult patients with primary or secondary dengue 3 virus infections. Int. J. Infect. Dis. 2007;11:256–262. doi: 10.1016/j.ijid.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 69.Halstead SB, Rojanasuphot S, Sangkawibha N. Original antigenic sin in dengue. Am. J. Trop. Med. Hyg. 1983;32:154–156. doi: 10.4269/ajtmh.1983.32.154. [DOI] [PubMed] [Google Scholar]
- 70.Singh KRP, Paul SD. Multiplication of arboviruses in cell lines from Aedes albopictus and Aedes aegypti. Curr. Sci. 1968;37:65–67. [Google Scholar]
- 71.Race MW, Williams MC, Agostini CF. Dengue in the Caribbean: virus isolation in a mosquito (Aedes pseudoscutellaris) cell line. Trans. R. Soc. Trop. Med. Hyg. 1979;73:18–22. doi: 10.1016/0035-9203(79)90122-6. [DOI] [PubMed] [Google Scholar]
- 72.Henchal EA, McCown JM, Seguin MC, Gentry MK, Brandt WE. Rapid identification of dengue virus isolates by using monoclonal antibodies in an indirect immunofluorescence assay. Am. J. Trop. Med. Hyg. 1983;32:164–169. doi: 10.4269/ajtmh.1983.32.164. [DOI] [PubMed] [Google Scholar]
- 73.Kao CL, et al. Flow cytometry compared with indirect immunofluorescence for rapid detection of dengue virus type 1 after amplification in tissue culture. Clin. Microbiol. 2001;39:3672–3677. doi: 10.1128/JCM.39.10.3672-3677.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guzman MG, et al. Fatal dengue hemorrhagic fever in Cuba, 1997. Int. J. Infect. Dis. 1999;3:130–135. doi: 10.1016/s1201-9712(99)90033-4. [DOI] [PubMed] [Google Scholar]
- 75.Rosen L, Drouet MT, Deubel V. Detection of dengue virus RNA by reverse transcription-polymerase chain reaction in the liver and lymphoid organs but not in the brain in fatal human infection. Am. J. Trop. Med. Hyg. 1999;61:720–724. doi: 10.4269/ajtmh.1999.61.720. [DOI] [PubMed] [Google Scholar]
- 76.Cardosa MJ, Tio PH, Nimmannitya S, Nisalak A, Innis B. IgM capture ELISA for detection of IgM antibodies to dengue virus: comparison of 2 formats using hemagglutinins and cell culture derived antigens. Southeast Asian J. Trop. Med. Pub. Health. 1992;23:726–729. [PubMed] [Google Scholar]
- 77.Vazquez S, et al. Detection of IgM against the dengue virus in whole blood absorbed on filter paper. Rev. Panam. Salud Pública. 1998;3:174–178. doi: 10.1590/s1020-49891998000300005. [DOI] [PubMed] [Google Scholar]
- 78.Herrera RD, Cabrera MV, Garcia S, Gilart M. IgM antibodies to dengue virus in dried blood on filter paper. Clin. Chim. Acta. 2006;367:204–206. doi: 10.1016/j.cca.2005.12.042. [DOI] [PubMed] [Google Scholar]
- 79.Balmaseda A, et al. Diagnosis of dengue virus infection by detection of specific immunoglobulin M (IgM) and IgA antibodies in serum and saliva. Clin. Diagn. Lab. Immunol. 2003;10:317–322. doi: 10.1128/CDLI.10.2.317-322.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Blacksell SD, et al. The comparative accuracy of 8 commercial rapid immunochromatographic assays for the diagnosis of acute dengue virus infection. Clin. Infect. Dis. 2006;42:1127–1134. doi: 10.1086/501358. [DOI] [PubMed] [Google Scholar]
- 81.Blacksell SD, et al. Prospective study to determine accuracy of rapid serological assays for diagnosis of acute dengue virus infection in Laos. Clin. Vaccine Immunol. 2007;14:1458–1464. doi: 10.1128/CVI.00482-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hunsperger EA, et al. Evaluation of commercially available anti-dengue virus immunoglobulin M tests. Emerg. Infect. Dis. 2009;15:436–440. doi: 10.3201/eid1503.080923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vazquez S, Bravo JR, Perez AB, Guzman MG. Inhibition ELISA. Its utility for classifying a case of dengue. Rev. Cubana Med. Trop. 1997;49:108–112. [PubMed] [Google Scholar]
- 84.Falconar AK, de Plata E, Romero-Vivas CM. Altered enzyme-linked immunosorbent assay immunoglobulin M (IgM)/IgG optical density ratios can correctly classify all primary or secondary dengue virus infections 1 day after the onset of symptoms, when all of the viruses can be isolated. Clin. Vaccine Immunol. 2006;13:1044–1051. doi: 10.1128/CVI.00105-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cardosa MJ, Wang SM, Sum MS, Tio PH. Antibodies against prM protein distinguish between previous infection with dengue and Japanese encephalitis viruses. BMC Microbiol. 2002;2:9. doi: 10.1186/1471-2180-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wong SJ, et al. Immunoassay targeting nonstructural protein 5 to differentiate west nile virus infection from dengue and St. Louis encephalitis virus infections and from flavivirus vaccination. J. Clin. Microbiol. 2003;41:4217–4223. doi: 10.1128/JCM.41.9.4217-4223.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baretto dos Santos F, et al. Analysis of recombinant dengue virus polypeptides for dengue diagnosis and evaluation of the humoral immune response. Am. J. Trop. Med. Hyg. 2004;71:144–152. [PubMed] [Google Scholar]
- 88.Kuno G, Gomez I, Gubler DJ. An ELISA procedure for the diagnosis of dengue infections. J. Virol. Methods. 1991;33:101–113. doi: 10.1016/0166-0934(91)90011-n. [DOI] [PubMed] [Google Scholar]
- 89.Shu PY, et al. Comparison of capture immunoglobulin M (IgM) and IgG enzyme-linked immunosorbent assay (ELISA) and nonstructural protein NS1 serotype-specific IgG ELISA for differentiation of primary and secondary dengue virus infections. Clin. Diagn. Lab. Immunol. 2003;10:622–630. doi: 10.1128/CDLI.10.4.622-630.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Calisher CH, et al. Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. J. Gen. Virol. 1989;70:37–43. doi: 10.1099/0022-1317-70-1-37. [DOI] [PubMed] [Google Scholar]
- 91.Russell PK, Nisalak A. Dengue virus identification by the plaque reduction neutralization test. J. Immunol. 1967;99:291–296. [PubMed] [Google Scholar]
- 92.Morens DM, Halstead SB, Repik PM, Putvatana R, Raybourne N. Simplified plaque reduction neutralization assay for dengue viruses by semimicro methods in BHK-21 cells: comparison of the BHK suspension test with standard plaque reduction neutralization. J. Clin. Microbiol. 1985;22:250–254. doi: 10.1128/jcm.22.2.250-254.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thomas SJ, et al. Dengue plaque reduction neutralization test (PRNT) in primary and secondary dengue virus infections: how alterations in assay conditions impact performance. Am. J. Trop. Med. Hyg. 2009;81:825–833. doi: 10.4269/ajtmh.2009.08-0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Roehrig JT, et al. Guidelines for plaque-reduction neutralization testing of human antibodies to dengue viruses. Viral Immunol. 2008;21:123–132. doi: 10.1089/vim.2008.0007. [DOI] [PubMed] [Google Scholar]
- 95.Morita K, Tanaka M, Igarashi A. Rapid identification of dengue virus serotypes by using polymerase chain reaction. J. Clin. Microbiol. 1991;29:2107–2110. doi: 10.1128/jcm.29.10.2107-2110.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lanciotti RS, Calisher CH, Gubler DJ, Chang GJ, Vorndam AV. Rapid detection and typing of dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. J. Clin. Microbiol. 1992;30:545–551. doi: 10.1128/jcm.30.3.545-551.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Harris E, et al. Typing of dengue viruses in clinical specimens and mosquitoes by single-tube multiplex reverse transcriptase PCR. J. Clin. Microbiol. 1998;36:2634–2639. doi: 10.1128/jcm.36.9.2634-2639.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Raengsakulrach B, et al. Comparison of four reverse transcription-polymerase chain reaction procedures for the detection of dengue virus in clinical specimens. J. Virol. Methods. 2002;105:219–232. doi: 10.1016/s0166-0934(02)00104-0. [DOI] [PubMed] [Google Scholar]
- 99.Johnson BW, Russell BJ, Lanciotti RS. Serotype-specific detection of dengue viruses in a fourplex real-time reverse transcriptase PCR assay. J. Clin. Microbiol. 2005;43:4977–4983. doi: 10.1128/JCM.43.10.4977-4983.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chien LJ, et al. Development of real-time reverse transcriptase PCR assays to detect and serotype dengue viruses. J. Clin. Microbiol. 2006;44:1295–1304. doi: 10.1128/JCM.44.4.1295-1304.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kong YY, Thay CH, Tin TC, Devi S. Rapid detection, serotyping and quantification of dengue viruses by TaqMan real-time one-step RT-PCR. J. Virol. Methods. 2006;138:123–130. doi: 10.1016/j.jviromet.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 102.Vaughn DW, et al. Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity. J. Infect. Dis. 2000;181:2–9. doi: 10.1086/315215. [DOI] [PubMed] [Google Scholar]
- 103.Wu SJ, et al. Detection of dengue viral RNA using a nucleic acid sequence-based amplification assay. J. Clin. Microbiol. 2001;39:2794–2798. doi: 10.1128/JCM.39.8.2794-2798.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hall WC, et al. Demonstration of yellow fever and dengue antigens in formalin-fixed paraffin-embedded human liver by immunohistochemical analysis. Am. J. Trop. Med. Hyg. 1991;45:408–417. doi: 10.4269/ajtmh.1991.45.408. [DOI] [PubMed] [Google Scholar]
- 105.Pelegrino JL, et al. Standardization of immunohistochemical techniques for detecting dengue virus antigens in paraffin-embedded tissues. Rev. Cubana Med. Trop. 1997;49:100–107. [PubMed] [Google Scholar]
- 106.Limonta D, Capo V, Torres G, Perez AB, Guzman MG. Apoptosis in tissues from fatal dengue shock syndrome. J. Clin. Virol. 2007;40:50–54. doi: 10.1016/j.jcv.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 107.Shu PY, et al. Potential application of nonstructural protein NS1 serotype-specific immunoglobulin G. enzyme-linked immunosorbent assay in the seroepidemiologic study of dengue virus infection: correlation of results with those of the plaque reduction neutralization test. J. Clin. Microbiol. 2002;40:1840–1844. doi: 10.1128/JCM.40.5.1840-1844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xu H, et al. Serotype 1-specific monoclonal antibody-based antigen capture immunoassay for detection of circulating nonstructural protein NS1: implications for early diagnosis and serotyping of dengue virus infections. J. Clin. Microbiol. 2006;44:2872–2878. doi: 10.1128/JCM.00777-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Young PR, Hilditch PA, Bletchly C, Halloran W. An antigen capture enzyme-linked immunosorbent assay reveals high levels of the dengue virus protein NS1 in the sera of infected patients. J. Clin. Microbiol. 2000;38:1053–1057. doi: 10.1128/jcm.38.3.1053-1057.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.WHO Scientific working group on dengue; Meeting Report 3–5 April, 2000; Geneva, Switzerland: WHO; 2000. [online] < http://apps.who.int/tdr/publications/tdr-research-publications/swg-dengue/pdf/dengue-swg.pdf>. [Google Scholar]
- 111.WHO . World Health Assembly Resolution WHA55.17, adopted by the 55th World Health Assembly. WHO; Geneva, Switzerland: 2002. Dengue fever and dengue haemorrhagic fever prevention and control. [online] < http://www.who.int/gb/ebwha/pdf_files/WHA55/ewha5517.pdf>. [Google Scholar]
- 112.WHO . Revision of the International Health Regulations. World Health Assembly Resolution WHA58.3, adopted by the 58th World Health Assembly. WHO; Geneva, Switzerland: 2005. [online] < http://www.who.int/gb/ebwha/pdf_files/WHA58/WHA58_3-en.pdf>. [Google Scholar]
- 113.TDR/WHO . Dengue Guidelines for Diagnosis, Treatment, Prevention and Control. TDR/WHO; Geneva, Switzerland: 2009. pp. 111–133. [PubMed] [Google Scholar]
- 114.Rodriguez MM, Bisset JA, Fernandez D. Levels of insecticide resistance and resistance mechanisms in Aedes aegypti from some Latin American countries. J. Am. Mosq. Control Assoc. 2007;23:420–429. doi: 10.2987/5588.1. [DOI] [PubMed] [Google Scholar]
- 115.Brengues C, et al. Pyrethroid and DDT cross-resistance in Aedes aegypti is correlated with novel mutations in the voltage-gated sodium channel gene. Med. Vet. Entomol. 2003;17:87–94. doi: 10.1046/j.1365-2915.2003.00412.x. [DOI] [PubMed] [Google Scholar]
- 116.Nam VS, Yen NT, Holynska M, Reid JW, Kay BH. National progress in dengue vector control in Vietnam: survey for Mesocyclops (Copepoda), Micronecta (Corixidae), and fish as biological control agents. Am. J. Trop. Med. Hyg. 2000;62:5–10. doi: 10.4269/ajtmh.2000.62.5. [DOI] [PubMed] [Google Scholar]
- 117.Kay BH, et al. Control of Aedes vectors of dengue in three provinces of Vietnam by use of Mesocyclops (Copepoda) and community-based methods validated by entomologic, clinical, and serological surveillance. Am. J. Trop. Med. Hyg. 2002;66:40–48. doi: 10.4269/ajtmh.2002.66.40. [DOI] [PubMed] [Google Scholar]
- 118.Focks DA, Alexander N. Multicountry study of Aedes aegypti pupal productivity survey methodology: findings and recommendations. WHO/TDR; Geneva, Switzerland: 2006. [online] < http://apps.who.int/tdr/publications/tdr-research-publications/multicountry-study-aedes-aegypti/pdf/aedes_aegypti.pdf>. [Google Scholar]
- 119.Heintze C, Garrido MV, Kroeger A. What do community-based dengue control programmes achieve? A systematic review of published evaluations. Trans. R. Soc. Trop. Med. Hyg. 2007;101:317–325. doi: 10.1016/j.trstmh.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 120.Kroeger A, et al. Effective control of dengue vectors with curtains and water container covers treated with insecticide in Mexico and Venezuela: cluster randomised trials. Br. Med. J. 2006;332:1247–1252. doi: 10.1136/bmj.332.7552.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mulla MS, Thavara U, Tawatsin A, Kong-Ngamsuk W, Chompoosri J. Mosquito burden and impact on the poor: measures and costs for personal protection in some communities. J. Am. Mosq. Control Assoc. 2001;17:153–159. [PubMed] [Google Scholar]
- 122.Hombach J. Vaccines against dengue: a review of current candidate vaccines at advanced development stages. Rev. Panam. Salud Pública. 2007;21:254–260. doi: 10.1590/s1020-49892007000300011. [DOI] [PubMed] [Google Scholar]
- 123.Hombach J, Cardosa JM, Sabchareon A, Vaughn DW, Barrett ADT. Scientific consultation on immunological correlates of protection induced by dengue vaccines. Report from a meeting held at the World Health Organization 17–18 November 2005. Vaccine. 2007;25:4130–4139. doi: 10.1016/j.vaccine.2007.02.079. [DOI] [PubMed] [Google Scholar]
- 124.Bettramello M, et al. The human immune response to dengue virus is dominated by highly cross-reactive antibodies endowed with neutralizing and enhancing activity. Cell Host Microbe. 2010;8:271–283. doi: 10.1016/j.chom.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dejnirattisai W, et al. Cross-reacting antibodies enhance dengue virus infection in humans. Science. 2010;328:745–748. doi: 10.1126/science.1185181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Whitehead SS, Blaney JE, Durbin AP, Murphy BR. Prospects for a dengue virus vaccine. Nature Rev. Microbiol. 2007;5:518–528. doi: 10.1038/nrmicro1690. [DOI] [PubMed] [Google Scholar]
- 127.Rothman AL. Dengue: defining protective versus pathologic immunity. J. Clin. Invest. 2004;113:946–951. doi: 10.1172/JCI21512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Halstead SB, Heinz FX, Barrett AD, Roehrig JT. Dengue virus: molecular basis of cell entry and pathogenesis. Vaccine. 2005;23:849–856. doi: 10.1016/j.vaccine.2004.03.069. [DOI] [PubMed] [Google Scholar]
- 129.Guirakhoo F, et al. Live attenuated chimeric yellow fever dengue type 2 (ChimeriVax-DEN2) vaccine: Phase I clinical trial for safety and immunogenicity: effect of yellow fever pre-immunity in induction of cross neutralizing antibody responses to all 4 dengue serotypes. Hum. Vaccine. 2006;2:60–67. doi: 10.4161/hv.2.2.2555. [DOI] [PubMed] [Google Scholar]
- 130.Durbin AP, et al. rDEN4 Delta 30, a live attenuated dengue virus type 4 vaccine candidate, is safe, immunogenic, and highly infectious in healthy adult volunteers. J. Infect. Dis. 2005;191:710–718. doi: 10.1086/427780. [DOI] [PubMed] [Google Scholar]
- 131.Raviprakash K, et al. A chimeric tetravalent dengue DNA vaccine elicits neutralizing antibody to all four virus serotypes in rhesus macaques. Virology. 2006;353:166–173. doi: 10.1016/j.virol.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 132.Hermida L, et al. A recombinant fusion protein containing the domain III of the dengue-2 envelope protein is immunogenic and protective in nonhuman primates. Vaccine. 2006;24:3165–3171. doi: 10.1016/j.vaccine.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 133.Whitehead SS, et al. A live, attenuated dengue virus type 1 vaccine candidate with a 30-nucleotide deletion in the 3′ untranslated region is highly attenuated and immunogenic in monkeys. J. Virol. 2003;77:1653–1657. doi: 10.1128/JVI.77.2.1653-1657.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Edelman R, et al. Phase I trial of 16 formulations of a tetravalent live-attenuated dengue vaccine. Am. J. Trop. Med. Hyg. 2003;69:48–60. doi: 10.4269/ajtmh.2003.69.48. [DOI] [PubMed] [Google Scholar]
- 135.Wright PF, et al. Phase 1 trial of the dengue virus type 4 vaccine candidate rDEN4Δ30-4995 in healthy adult volunteers. Am. J. Trop. Med. Hyg. 2009;81:834–841. doi: 10.4269/ajtmh.2009.09-0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Morrison D, et al. A novel tetravalent dengue vaccine is well tolerated and immunogenic against all 4 serotypes in flavivirus-naive adults. J. Infect. Dis. 2010;201:370–377. doi: 10.1086/649916. [DOI] [PubMed] [Google Scholar]
- 137.WHO . Pocket book of hospital care for children. Guidelines for the management of common illnesses with limited resources. WHO; Geneva, Switzerland: 2005. [online] < http://whqlibdoc.who.int/publications/2005/9241546700.pdf>. [Google Scholar]
- 138.WHO . Dengue haemorrhagic fever: early recognition, diagnosis and hospital management. An audiovisual guide for health-care workers responding to outbreaks. WHO; Geneva, Switzerland: 2006. [online] < http://www.who.int/csr/don/archive/disease/dengue_fever/dengue.pdf>. [PubMed] [Google Scholar]
- 139.Parks W, Lloyd L. Planning social mobilization and communication for dengue fever prevention and control: a step-by-step guide. WHO; Geneva, Switzerland: 2004. [online] < http://apps.who.int/tdr/publications/training-guideline-publications/planning-social-mobilization-dengue-fever/pdf/planning_dengue.pdf>. [Google Scholar]
- 140.WHO . Global strategic framework for integrated vector management. WHO; Geneva, Switzerland: 2004. [online] < http://whqlibdoc.who.int/hq/2004/WHO_CDS_CPE_PVC_2004_10.pdf>. [Google Scholar]
- 141.Gubler DJ. Dengue and dengue haemorrhagic fever. Clin. Microbiol. Rev. 1998;11:480–496. doi: 10.1128/cmr.11.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]