Abstract
Background:
Different approaches to treat myasthenia gravis showed variable outcomes probably because of remained ectopic thymic tissue. The aim of this study is to determine incidence of thymic tissue in cases without any thymic disease.
Materials and Methods:
Seventy-two patients scheduled for open heart surgery during 2000 and 2007 without thymic disease that were enrolled in the study at Chamran Hospital. Intraoperative biopsies were taken form aortopulmonary window, aortocaval groove and left and right pericardiophrenic regions. Finally, the distribution of ectopic thymic tissue was evaluated in above regions.
Results:
Thymic tissue was found overall in 70.85% of patients. The most common sites for thymic tissue were left pericardiophrenic (50%) and right pericardiophrenic (31.9%) regions. Frequencies of ectopic thymus in aortopulmonary window and aortocaval groove were 19.4% and 12.5%, respectively.
Conclusion:
Because of high incidence of ectopic thymic tissue in mediastinum in patients without thymic disease, we recommend wide excision of thymus gland and all of adipose tissue in patients with myasthenia gravis.
Keywords: Ectopic thymic tissue, mediastinum, myasthenia gravis
INTRODUCTION
Thymus buds migrate from elongated ventral part to third pharyngeal pouch bilaterally. Then, they descend and come together in midline and form thymus gland in superior anterior mediastinum. Although thymus is considered as a one unit, it has a bi component architectural origin. Thymus, as well as parathyroid glands, loses its connection to pharynx.[1] Accidently, some islands of thymus tissue may be left in unrelated anatomical regions due to defects during descending of thymic buds. This residual tissue may be the cause of developing some disorders such as thymic cyst, cervical thymoma, and ectopic thymus tissue.[2,3,4,5,6]
Recently, several studies were done on the frequency of ectopic tissue in the mediastinum and the neck of the patients with myashtenia gravis. Our previous study showed frequency of cervical ectopic thymic tissue in people without thymic diseases.[7] It was an issue for our surgical department that no study was performed to evaluate ectopic thymus within mediastinal region in patients without thymic disease. The aim of the present study is to determine the frequency of ectopic thymic tissue in mediastinum among patients without any thymic diseases.
MATERIALS AND METHODS
We enrolled 72 eligible patients who were scheduled for open heart surgery due to any cause during 2000 and 2007 at Chamran Hospital in Esfahan. None of them had history or symptoms of thymic disease. After sternotomy, from each of the four different parts of mediastinum (aortopulmonary window, aortocaval groove, left, and right pericaridophrenic regions) which were more likely to find ectopic thymus, a 1 × 1-cm biopsy was taken. Then, specimens were fixed in formalin and processed and stained with Hematoxylin and Eosin. Finally, slides were reviewed by an expert pathologist and considered positive if Hassal Corpuscle was observed in the background of lymphoid tissue. After gathering the data, SPSS v16 was used to analyze them.
RESULTS
Our subjects comprised 21 females (29.2%) and 51 males (70.8%) from the age of 6-75. In this study 228 slides and 864 sections were reviewed for presence of the thymic tissue. Thymic tissue was found in 70.85% of patients. This study showed ectopic thymic tissue were frequently located in different parts of the mediastinum which were left pericardiophrenic 50%, right pericardiophrenic 31.9%, aortopulmonary window 19.4% and aortocaval groove 12.5% [Figure 1].
Figure 1.
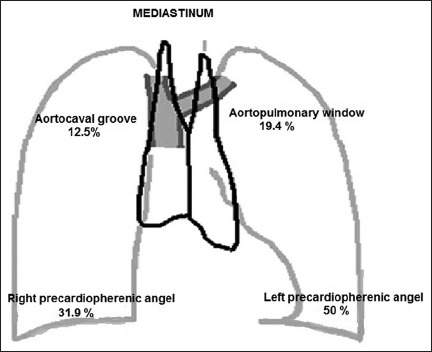
Distribution of ectopic thymic tissue in population of 72 patients
DISCUSSION
In our literature review, it was an interesting fact that this study was the only one done on patients without any thymic disease. In study done by Zielinski et al. overall incidence of proven and suspicious cases were as followed: Aortopulmonary window 25.9%, aortocaval groove 17.2%, left pericardiophrenic fat 22.4%, right pericardiophrenic fat 24.1%, perithymic fat 22.4%, cervical 12.1% and all of the aforementioned localizations 56.9% in patients with myasthenia gravis.[8] Fukai outlined frequency of thymic tissue in anterior mediastinal fat and para-aortic fat were 44.4% and 7.4%, respectively.[9] In study of Jaretzki and Wolf, incidence of ectopic thymic tissue was 32% in the neck and 98% in the mediastinum.[10] Another study showed that the incidence of ectopic thymic tissue in mediastinum of myasthenia gravis patients was up to 72.2%.[11] The newest studies which were done by Amergi V and Mineo TC, revealed the incidence of ectopic thymic tissue in mediastinum was 67% and 80%, respectively.[12,13]
Furthermore, the outcomes of this study revealed that the frequency of mediastinal ectopic thymic tissue is surprisingly high in candidates who did not have myasthenia gravis or thymic disease. So, the analysis of the high incidence of anatomical findings of mediastinal ectopic thymic tissue of this study in patients without thymic disease, proves the likelihood of the high frequency of ectopic thymic tissue in myasthenia gravis patients. Several medical treatments are used during these years, but, due to high incidence of mediastinal ectopic thymic tissue in the aforementioned studies, majority of the thoracic surgeons recommend extended thymectomy which is the removal of the thymus and all adipose tissue in anterior mediastinum.
CONCLUSIONS
Understanding the anatomy of thymic and ectopic tissue is very important for management of the myasthenia gravis. Incomplete resections of thymus or leaving ectopic tissue are the two main factors of recurrence of the disease. All in all, this study states that the high frequency of mediastinal ectopic thymus tissue in patients without thymic disease validates the evidence of high distribution of mediastinal ectopic thymic tissue among myasthenia gravis patients. So, we recommend wide excision of thymus gland and all of the adipose tissue from diaphragm to the thymic corn and laterally to phrenic nerves by full median sternotomy in myasthenia gravis patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Moore KL, Persaud TV. Clinically Oriented Embryology. 9th ed. Philadelphia: WB Saunders Company; 2011. The developing human; pp. 167–173. [Google Scholar]
- 2.Fukuda T, Itami M, Sawa H, Furukawa T, Fukakusa S, Tsuchihashi N, et al. A case of thymoma arising from undescended thymus. High uptake of Thallium-201 chloride. Eur J Nucl Med. 1980;5:465–8. doi: 10.1007/BF00261793. [DOI] [PubMed] [Google Scholar]
- 3.Miller WT, Jr, Gefter WB, Miller WT. Thymoma mimicking a thyroid mass. Radiology. 1992;184:75–6. doi: 10.1148/radiology.184.1.1609105. [DOI] [PubMed] [Google Scholar]
- 4.Kiyosue H, Miyake H, Komatsu E, Mori H. MRI of cervical masses of thymic origin. J Comput Assist Tomogr. 1994;18:206–8. doi: 10.1097/00004728-199403000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita H, Murakami N, Noguchi S, Noguchi A, Yokoyama S, Moriuchi A, et al. Cervical thymoma and incidence of cervical thymus. Acta Pathol Jpn. 1983;33:189–94. doi: 10.1111/j.1440-1827.1983.tb02113.x. [DOI] [PubMed] [Google Scholar]
- 6.Khariwala SS, Nicollas R, Triglia JM, Garabedian EN, Marianowski R, Van Den Abbeele T, et al. Cervical presentations of thymic anomalies in children. Int J Pediatr Otorhinolaryngol. 2004;68:909–14. doi: 10.1016/j.ijporl.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Tabatabaie SA, Hashemi SM, Sanei B, Sanei MH. The frequency of ectopic thymic tissue in the necks of patients without any thymic disease. Med Sci Monit. 2007;13:CR283–5. [PubMed] [Google Scholar]
- 8.Zieliński M, Kuzdzal J, Szlubowski A, Soja J. Comparison of late results of basic transsternal and extended transsternal thymectomies in the treatment of myasthenia gravis. Ann Thorac Surg. 2004;78:253–8. doi: 10.1016/j.athoracsur.2003.11.040. [DOI] [PubMed] [Google Scholar]
- 9.Fukai I, Funato Y, Mizuno T, Hashimoto T, Masaoka A. Distribution of thymic tissue in the mediastinal adipose tissue. J Thorac Cardiovasc Surg. 1991;101:1099–102. [PubMed] [Google Scholar]
- 10.Jaretzki A, 3rd, Wolff M. “Maximal“ thymectomy for myasthenia gravis. Surgical anatomy and operative technique. J Thorac Cardiovasc Surg. 1988;96:711–6. [PubMed] [Google Scholar]
- 11.Masaoka A, Yamakawa Y, Niwa H, Fukai I, Kondo S, Kobayashi M, et al. Extended thymectmy for myasthenia gravis patients: A 20-year review. Ann Thorac Surg. 1996;62:853–9. doi: 10.1016/s0003-4975(96)00376-1. [DOI] [PubMed] [Google Scholar]
- 12.Ambrogi V, Mineo TC. Active ectopic thymus predicts poor outcome after thymectomy in class III myasthenia gravis. J Thorac Cardiovasc Surg. 2012;143:601–6. doi: 10.1016/j.jtcvs.2011.04.050. [DOI] [PubMed] [Google Scholar]
- 13.Mineo TC, Ambrogi V. Outcomes after thymectomy in class I myasthenia gravis. J Thorac Cardiovasc Surg. 2013;145:1319–24. doi: 10.1016/j.jtcvs.2012.12.053. [DOI] [PubMed] [Google Scholar]


