Abstract
Purpose:
To study the impact of adjuvant trastuzumab among patients achieving a pathologic complete response (pCR) after trastuzumab-based neoadjuvant systemic therapy (NST).
Patients and methods:
Patients with primary HER2-positive breast cancer treated with trastuzumab-based NST were categorised according to adjuvant trastuzumab administration and pCR status. Adjuvant trastuzumab became standard of care in 2006, this was the main reason patients in our cohort did not receive adjuvant trastuzumab. Kaplan–Meier was used to estimate survival. A test for interaction between adjuvant trastuzumab and pCR was completed.
Findings:
Of 589 patients, 203 (34.5%) achieved a pCR. After surgery, 109 (18.5%) patients in the entire cohort did not receive adjuvant trastuzumab. Among patients achieving a pCR, 31.3% received adjuvant trastuzumab compared with 68.8% among those who did not achieve a pCR (P=0.0006). Among patients achieving pCR, adjuvant trastuzumab did not further improve overall survival (OS) or relapse-free survival (RFS) (P=0.35 and P=0.93, respectively). Any benefit of adjuvant trastuzumab in OS and RFS among patients without a pCR did not achieve statistical significance (P=0.3 and P=0.44, respectively).
Conclusions:
In this cohort, patients treated with trastuzumab-based NST who achieved a pCR have excellent outcome regardless of whether they received adjuvant trastuzumab.
Keywords: trastuzumab, neoadjuvant therapy, pathologic complete response, adjuvant therapy, survival
Neoadjuvant systemic therapy (NST) is commonly used to downstage the primary tumour and regional lymph nodes preoperatively, in order to increase operability and enable breast-conserving surgery in patients with large primary tumours or locally advanced disease (Fisher et al, 1998; Gralow et al, 2008). NST also allows the assessment of the effectiveness of the systemic treatment by pathologic evaluation of the breast and nodes removed at surgery (Gralow et al, 2008; Cortazar et al, 2014). A pathologic complete response (pCR) in the breast and nodes is associated with favourable survival outcomes. However, this association is stronger among patients with highly proliferative, HER2-positive breast cancers (Untch et al, 2011; Kim et al, 2013; Cortazar et al, 2014).
HER2 is overexpressed in approximately 15–25% of primary breast cancers (Wolff et al, 2013). In the neoadjuvant setting, randomised trials have shown that the use of trastuzumab-based NST increases pCR rates compared with chemotherapy alone (Buzdar et al, 2005; Gianni et al, 2014), and recent data demonstrated that dual anti-HER2 therapy combined with chemotherapy further increases pCR rates as compared with trastuzumab-based chemotherapy (Baselga et al, 2012; Gianni et al, 2012).
Although 1 year of trastuzumab therapy is considered the standard of care today, several studies have been designed to look at shorter or longer treatment times (Goldhirsch et al, 2013; Pivot et al, 2013). A recent randomised trial comparing 6 months of adjuvant trastuzumab therapy vs 1 year failed to show that 6 months of adjuvant trastuzumab treatment was non-inferior to 12 months (Pivot et al, 2013). The impact of adjuvant trastuzumab among patients achieving a pCR after trastuzumab-based NST is unknown. We therefore, aimed to evaluate the impact of completion of adjuvant trastuzumab according to pCR status.
Patients and methods
A retrospective review of the Breast Medical Oncology Institutional database at The University of Texas MD Anderson Cancer Center was performed. Women with HER2-positive primary invasive breast cancer who received trastuzumab-based NST from 2001 to 2012 were identified. Adjuvant trastuzumab became standard of care in 2006; this was the main reason patients in our cohort did not receive adjuvant trastuzumab in earlier years. Patients were classified according to whether they had received adjuvant trastuzumab or not. Data were extracted on relevant prognostic factors including year of diagnosis, age, menopausal status, race, histology, grade, lymphovascular invasion (LVI), oestrogen receptor status, progesterone receptor status, adjuvant radiation, and adjuvant endocrine therapy. pCR was defined as no evidence of invasive cancer in the breast and lymph nodes (yT0/is,N0).
Patient characteristics were tabulated and compared between the adjuvant trastuzumab vs no adjuvant trastuzumab groups using Chi-square test. Overall survival (OS) was measured from the date of diagnosis to the date of death or lost to follow-up. Relapse-free survival (RFS) was measured from the date of diagnosis to the date of first documented local or distant recurrence. Patients who died before experiencing the relevant events were considered censored for RFS at their dates of last follow-up. The Kaplan–Meier product limit method was used to estimate the 5-year OS and RFS with 95% confidence intervals (CIs) of all patients, and compared using the log-rank statistic. Cox proportional hazards models were fit to determine the association of patient and clinical characteristics with survival outcomes. Initially, a Cox proportional hazard model that included pCR, adjuvant trastuzumab and the interaction between both covariates was tested. Because of rare events in one of the groups defined by the two variables, Firth's penalised likelihood approach was applied to obtain a finite estimate for the coefficient (Firth, 1993). The profile-likelihood confidence limits for the hazard ratios (HR) are presented. Variables were included in the final Cox multivariate model based on both statistical significance and clinical relevance including adjuvant trastuzumab, pCR, race, clinical stage at presentation, hormone receptor status, and LVI, year of diagnosis and adjuvant endocrine therapy. Results are expressed in HR and 95% CIs. P values less than 0.05 were considered statistically significant; all tests were two-sided. Statistical analyses were carried out using SAS 9.3 (SAS Institute, Cary, NC, USA) and S-Plus 8.2 (TIBCO Software Inc., Houston, TX, USA).
Results
A total of 589 women with HER2-positive breast cancer diagnosed between 2001 and 2012 were identified. Patients received NST with either PH-FECH (paclitaxel 80 mg m−2 intravenously weekly for 12 weeks or paclitaxel 225 mg m−2 intravenously over 24 h every 3 weeks, followed by 4 cycles of FEC-75 (5-fluorouracil 500 mg m−2, epirubicin 75 mg m−2, and cyclophosphamide 500 mg m−2) intravenously on day 1, every 3 weeks. A loading dose of 4 mg kg−1 intravenously trastuzumab was given on day 1 followed by 2 mg kg−1 weekly, during the 24 weeks of NST). After surgery, 109 (18.5%) patients did not receive adjuvant trastuzumab, and 480 (81.5%) patients received adjuvant trastuzumab for 6 months to complete 1 year of therapy. Patient characteristics by adjuvant trastuzumab therapy are presented in Table 1. There were no significant differences amongst clinical and pathologic factors. A total of 203 patients (34.55) achieved a pCR. Among them, 73.9% of the patients received adjuvant trastuzumab compared with 85.5% of patients not achieving a pCR (P=0.0006).
Table 1. Patient and tumour characteristics.
|
All patients (N=589) |
No adjuvant trastuzumab (N=109) |
Adjuvant trastuzumab (N=480) |
|
|||
|---|---|---|---|---|---|---|
| N (%) | N | % | N | % | P-value | |
|
Year of diagnosis | ||||||
| 2001–2006 | 142 (24.1%) | 80 | 73.4 | 62 | 12.9 | |
| 2007–2012 |
447 (75.9%) |
29 |
26.6 |
418 |
87.1 |
<0.0001 |
|
Age (years) | ||||||
| Age≤50 | 293 (49.7%) | 52 | 47.7 | 241 | 50.2 | |
| Age>50 |
296 (50.3%) |
57 |
52.3 |
239 |
49.8 |
0.64 |
|
Race/ethnicity | ||||||
| White | 344 (58.4%) | 66 | 60.6 | 278 | 57.9 | |
| Black | 73 (12.4%) | 15 | 13.8 | 58 | 12.1 | |
| Hispanic | 116 (19.7%) | 20 | 18.3 | 96 | 20.0 | |
| Other |
56 (9.5%) |
8 |
7.3 |
48 |
10.0 |
0.78 |
|
Clinical stage | ||||||
| I | 8 (1.4%) | 2 | 1.9 | 6 | 1.3 | |
| II | 293 (50.3%) | 59 | 54.6 | 234 | 49.3 | |
| III |
282 (48.4%) |
47 |
43.5 |
235 |
49.5 |
0.50 |
|
Histology | ||||||
| Ductal | 543 (92.2%) | 102 | 93.6 | 441 | 91.9 | |
| Other |
46 (7.8%) |
7 |
6.4 |
39 |
8.1 |
0.55 |
|
Nuclear grade | ||||||
| 1–2 | 123 (21.4%) | 86 | 78.9 | 366 | 78.5 | |
| 3 |
452 (78.6%) |
23 |
21.1 |
100 |
21.5 |
0.93 |
|
Lymphovascular invasion | ||||||
| Negative | 479 (81.3%) | 92 | 84.4 | 387 | 80.6 | |
| Positive |
110 (18.7%) |
17 |
15.6 |
93 |
19.4 |
0.36 |
|
Hormone receptor status | ||||||
| Negative | 236 (40.4%) | 51 | 46.8 | 185 | 38.9 | |
| Positive |
348 (59.6%) |
58 |
53.2 |
290 |
61.1 |
0.13 |
|
Pathologic complete response | ||||||
| No | 386 (65.5%) | 56 | 51.4 | 330 | 68.8 | |
| Yes |
203 (34.5%) |
53 |
48.6 |
150 |
31.3 |
0.0006 |
|
Adjuvant radiation | ||||||
| No | 125 (21.2%) | 24 | 22.0 | 101 | 21.0 | |
| Yes |
464 (78.8%) |
85 |
78.0 |
379 |
79.0 |
0.82 |
|
Adjuvant endocrine therapy | ||||||
| No | 301 (51.1%) | 59 | 54.1 | 242 | 50.4 | |
| Yes | 288 (48.9%) | 50 | 45.9 | 238 | 49.6 | 0.48 |
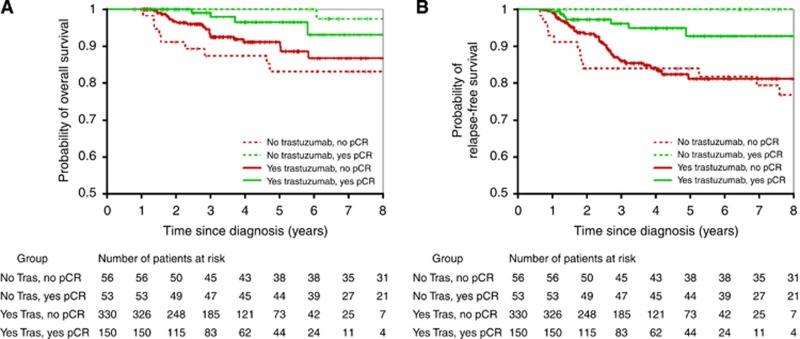
At a median follow-up of 45 months, (range, 9–144 months), 38 patients (6.5%) had died, and 61 (10.4%) had experienced a recurrence. Table 2 summarises the 5-year OS and RFS estimates by patient and tumour characteristics. For the overall cohort, 5-year OS and RFS were 93% and 87%, respectively. The 5-year OS estimates were 91% and 93% for patients who did not or did receive adjuvant trastuzumab (P=0.97); and the 5-year RFS estimates were 92% and 85% for patients who did not or did receive adjuvant trastuzumab (P=0.33), respectively. When comparing patients who did not or did achieve a pCR after NST, the 5-year OS estimates were 90% and 98% (P=0.002), respectively; and the 5-year RFS estimates were 83% and 95% (P<0.0001), respectively. The Kaplan–Meier estimates of OS and RFS stratified by adjuvant trastuzumab and pCR status are presented in Figure 1.
Table 2. Survival estimates by patient characteristics.
| N Patients | N Events | 5-year overall survival estimate (95% CI) | P-value | N Events | 5-year relapse-tree survival estimate (95% CI) | P-value | |
|---|---|---|---|---|---|---|---|
| All patients |
589 |
38 |
0.93 (0.9, 0.95) |
|
61 |
0.87 (0.84, 0.9) |
|
|
Year of diagnosis | |||||||
| 2001–2006 | 142 | 14 | 0.92 (0.86, 0.96) | 19 | 0.88 (0.82, 0.93) | ||
| 2007–2012 |
447 |
24 |
0.93 (0.89, 0.95) |
0.60 |
42 |
0.86 (0.8, 0.9) |
0.64 |
|
Age (years) | |||||||
| Age≤50 | 293 | 19 | 0.93 (0.88, 0.96) | 30 | 0.87 (0.82, 0.91) | ||
| Age>50 |
296 |
19 |
0.92 (0.88, 0.95) |
0.78 |
31 |
0.87 (0.82, 0.91) |
0.80 |
|
Race/ethnicity | |||||||
| White | 344 | 23 | 0.92 (0.88, 0.95) | 33 | 0.89 (0.85, 0.92) | ||
| Black | 73 | 6 | 0.89 (0.77, 0.95) | 13 | 0.72 (0.55, 0.84) | ||
| Hispanic | 116 | 4 | 0.98 (0.92, 0.99) | 7 | 0.92 (0.83, 0.96) | ||
| Other |
56 |
5 |
0.87 (0.71, 0.95) |
0.39 |
8 |
0.84 (0.71, 0.92) |
0.03 |
|
Clinical stage | |||||||
| I–II | 301 | 17 | 0.93 (0.89, 0.96) | 22 | 0.9 (0.85, 0.94) | ||
| III |
282 |
20 |
0.92 (0.87, 0.95) |
0.42 |
38 |
0.84 (0.79, 0.88) |
0.01 |
|
Histology | |||||||
| Ductal | 543 | 34 | 0.93 (0.9, 0.95) | 54 | 0.88 (0.84, 0.91) | ||
| Other |
46 |
4 |
0.91 (0.74, 0.97) |
0.56 |
7 |
0.82 (0.64, 0.92) |
0.26 |
|
Nuclear grade | |||||||
| 1–2 | 123 | 7 | 0.93 (0.84, 0.97) | 14 | 0.86 (0.76, 0.92) | ||
| 3 |
452 |
30 |
0.93 (0.89, 0.95) |
0.57 |
45 |
0.88 (0.84, 0.91) |
0.71 |
|
Lymphovascular invasion | |||||||
| Negative | 479 | 24 | 0.94 (0.91, 0.96) | 37 | 0.9 (0.87, 0.93) | ||
| Positive |
110 |
14 |
0.86 (0.76, 0.92) |
0.002 |
24 |
0.72 (0.6, 0.81) |
<0.0001 |
|
Hormone receptor status | |||||||
| Negative | 236 | 18 | 0.92 (0.86, 0.95) | 24 | 0.88 (0.82, 0.92) | ||
| Positive |
348 |
20 |
0.93 (0.89, 0.96) |
0.53 |
36 |
0.87 (0.82, 0.91) |
0.77 |
|
Pathologic complete response | |||||||
| No | 386 | 33 | 0.9 (0.85, 0.93) | 54 | 0.83 (0.78, 0.87) | ||
| Yes |
203 |
5 |
0.98 (0.93, 0.99) |
0.002 |
7 |
0.95 (0.9, 0.98) |
<0.0001 |
|
Adjuvant trastuzumab | |||||||
| No | 109 | 11 | 0.91 (0.84, 0.95) | 12 | 0.92 (0.85, 0.96) | ||
| Yes |
480 |
27 |
0.93 (0.9, 0.95) |
0.97 |
49 |
0.85 (0.8, 0.89) |
0.33 |
|
Adjuvant radiation | |||||||
| No | 125 | 8 | 0.94 (0.86, 0.97) | 10 | 0.89 (0.79, 0.95) | ||
| Yes |
464 |
30 |
0.92 (0.89, 0.95) |
0.69 |
51 |
0.87 (0.83, 0.9) |
0.63 |
|
Adjuvant endocrine therapy | |||||||
| No | 301 | 23 | 0.91 (0.87, 0.94) | 31 | 0.87 (0.82, 0.91) | ||
| Yes | 288 | 15 | 0.94 (0.89, 0.96) | 0.17 | 30 | 0.87 (0.82, 0.91) | 0.84 |
Abbreviation: CI=confidence interval.
Figure 1.
Kaplan–Meier OS estimates (A) and RFS estimates (B) according to adjuvant trastuzumab use and pCR status.
On multivariate analysis, there was no significant interaction between adjuvant trastuzumab and pCR on OS (P=0.32) or RFS (P=0.15). After adjustment for year of diagnosis, pCR, race, clinical stage at presentation, hormone receptor status, LVI and adjuvant endocrine therapy, adjuvant trastuzumab had no significant impact on OS (HR=0.75; 95% CI=0.31–1.78; P=0.51) or RFS (HR=1.10; 95% CI=0.52–2.33; P=0.81). As expected, patients who achieved a pCR had a decreased risk of death (HR=0.23; 95% CI=0.08–0.60; P=0.003) and recurrence (HR=0.22; 95% CI=0.1–0.49; P=0.0002). In addition, black race (HR=2.07; 95% CI=1.11–3.87; P=0.022), clinical stage III disease at diagnosis (HR=2.28; 95% CI=1.3–3.99; P=0.004), and the presence of LVI (HR=2.28; 95% CI=1.33–3.93; P=0.003) were associated with an increased risk of recurrence (Table 3).
Table 3. Multivariable Cox proportional hazards models.
|
Overall survival |
Relapse-free survival |
|||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | P-value | Hazard ratio | 95% CI | P-value | |
| Adjuvant trastuzumab vs no |
0.75 |
0.31–1.78 |
0.51 |
1.1 |
0.52–2.33 |
0.81 |
| Year of diagnosis: 2001–2006 vs 2007–2012 |
0.78 |
0.34–1.79 |
0.56 |
1.13 |
0.59–2.17 |
0.72 |
| pCR vs no |
0.23 |
0.08–0.6 |
0.003 |
0.22 |
0.1–0.49 |
0.0002 |
| Back race vs other |
1.37 |
0.56–3.33 |
0.49 |
2.07 |
1.11–3.87 |
0.022 |
| Clinical stage III vs I and II |
1.42 |
0.71–2.84 |
0.32 |
2.28 |
1.3–3.99 |
0.004 |
| Hormone receptor positive vs negative. |
1.48 |
0.54–4.05 |
0.45 |
1.45 |
0.63–3.33 |
0.38 |
| Lymphovascular invasion vs no |
2.17 |
1.06–4.45 |
0.034 |
2.28 |
1.33–3.93 |
0.003 |
| Adjuvant endocrine therapy vs no | 0.37 | 0.14–1.02 | 0.05 | 0.57 | 0.25–1.28 | 0.17 |
Abbreviation: CI=confidence interval.
Discussion
This study was undertaken to evaluate the impact of completion of adjuvant trastuzumab in patients with HER2-positive disease treated at our institution according to pCR status. In this cohort of patients treated with trastuzumab-based NST, those who achieved a pCR had an excellent outcome regardless of whether they received adjuvant trastuzumab or not.
In our initial trastuzumab-based neoadjuvant study, patients received trastuzumab for only 24 weeks during chemotherapy and did not receive adjuvant trastuzumab following local therapy because adjuvant trastuzumab was, at the time, not part of the standard of care (Buzdar et al, 2007). This practice was continued until trastuzumab was approved in the adjuvant setting with the recommended duration of 1 year of treatment. To our knowledge, this is the only cohort of patients available to evaluate the impact of adjuvant trastuzumab among patients who achieved a pCR. A recently published retrospective study evaluating the outcomes of patients with HER2-positive breast cancer reported that 65 (8.4%) of the 776 patients in the study did not receive adjuvant trastuzumab, however, outcomes in this group were not discussed (Takada et al, 2014).
Although the test for interaction in the analysis of our patient cohort was negative, we applied a Firth's penalised likelihood approach to obtain a finite estimate for the coefficients and the profile-likelihood confidence limits for the HR in the multivariable analysis to compensate for our limited sample size before commit to our conclusions (Firth, 1993).
Currently, there is compelling evidence from large phase III randomised clinical trials including approximately 12 000 patients supporting the standard use of adjuvant trastuzumab for 1 year. On the basis of the results of the FinHER study (Joensuu et al, 2009), shorter adjuvant trastuzumab regimens are being evaluated (9 weeks, 3 months, and 6 months), but only one has been fully reported. Results from the PHARE trial failed to show that 6 months of trastuzumab is non-inferior to 12 months. Nevertheless, the cardiac safety profile was more favourable for the shorter treatment (Pivot et al, 2013). The results of other on-going or recently completed studies are not expected before 2015, at which time they might be less relevant given that dual anti-HER2 therapy with pertuzumab and trastuzumab is now part of the new standard of care.
As our treatment armamentarium increases, we continue to struggle to find biomarkers capable of identifying those patients with HER2-positive breast cancer who need less extensive or less complex therapies, and pCR after adequate NST may be a good surrogate. All anti-HER2-based NST studies have shown that patients who achieved a pCR at the time of surgery have an excellent prognosis and the majority are probably cured (Buzdar et al, 2007; Untch et al, 2011; Baselga et al, 2012; Bayraktar et al, 2012; Gianni et al, 2012; Buzdar et al, 2013; Cortazar et al, 2014; Gianni et al, 2014). The use of maintenance trastuzumab to complete a year of therapy is considered standard, and no data are available to support the use of pertuzumab, T-DM1, or lapatinib in the adjuvant setting; further, the neoadjuvant studies adding lapatinib and pertuzumab only used these targeted therapies in the pre-operative portion of the treatment (Baselga et al, 2012; Gianni et al, 2012). Our work is limited by its retrospective nature and limited sample size; despite including in the multivariable model important clinical variables, residual confounding cannot be excluded. Furthermore, selection bias is a potential concern because we do not have specific information on the reason a patient was prescribed further adjuvant trastuzumab or not. Our results are hypothesis-generating and need to be interpreted with caution, but they support the concept that patients achieving a pCR may not receive further benefit from adjuvant anti-HER2 therapy and therefore, toxicities may be avoided. Furthermore, if patients achieving a pCR do not receive further benefit from adjuvant trastuzumab, this could have important implications associated with resource optimisation. This is particularly relevant as the use of double anti-HER2 blockade becomes standard in the neoadjuvant setting and we increase the rates of pCR. Further prospective studies are needed to evaluate the impact of continued HER2 therapy among patients with a pCR. In addition, ongoing prospective studies evaluating the benefit of adjuvant anti-HER2 therapies after a pCR would be ideal to answer this important question and an opportunity for comparative effectiveness research, particularly as we incorporate newer targeted therapies into the care of our patients (Pritchard, 2010).
Acknowledgments
This work was supported in part by American Cancer Society Research Scholar Grant 121329-RSG-11-187-01-TBG (AMG) and The Commonwealth Foundation for Cancer Research (AMG). DHHS–NIH–National Cancer Institute: 2P30 CA016672 (PP-RP6) Cancer Center Support grant to MD Anderson Cancer Center. The MD Anderson Breast Cancer Management is supported in part by the Nelly B. Connally Breast Cancer Research Fund.
GNH, VV, and AMG have received research funding from Genentech and GSK. All remaining authors have declared no conflicts of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Results of this study were presented in part at the 2014 American Society of Clinical Oncology, Chicago, IL, June, 2014.
References
- Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, Gómez H, Dinh P, Fauria K, Van Dooren V, Aktan G, Goldhirsch A, Chang TW, Horváth Z, Coccia-Portugal M, Domont J, Tseng LM, Kunz G, Sohn JH, Semiglazov V, Lerzo G, Palacova M, Probachai V, Pusztai L, Untch M, Gelber RD, Piccart-Gebhart M, NeoALTTO Study Team Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379 (9816:633–640. doi: 10.1016/S0140-6736(11)61847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayraktar S, Gonzalez-Angulo AM, Lei X, Buzdar AU, Valero V, Melhem-Bertrandt A, Kuerer HM, Hortobagyi GN, Sahin AA, Meric-Bernstam F. Efficacy of neoadjuvant therapy with trastuzumab concurrent with anthracycline- and nonanthracycline-based regimens for HER2-positive breast cancer. Cancer. 2012;118 (9:2385–2393. doi: 10.1002/cncr.26555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzdar AU, Ibrahim NK, Francis D, Booser DJ, Thomas ES, Theriault RL, Pusztai L, Green MC, Arun BK, Giordano SH, Cristofanilli M, Frye DK, Smith TL, Hunt KK, Singletary SE, Sahin AA, Ewer MS, Buchholz TA, Berry D, Hortobagyi GN. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23 (16:3676–3685. doi: 10.1200/JCO.2005.07.032. [DOI] [PubMed] [Google Scholar]
- Buzdar AU, Suman VJ, Meric-Bernstam F, Leitch AM, Ellis MJ, Boughey JC, Unzeitig G, Royce M, McCall LM, Ewer MS, Hunt KK, American College of Surgeons Oncology Group, investigators Fluorouracil, epirubicin, and cyclophosphamide (FEC-75) followed by paclitaxel plus trastuzumab versus paclitaxel plus trastuzumab followed by FEC-75 plus trastuzumab as neoadjuvant treatment for patients with HER2-positive breast cancer (Z1041): a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14 (13:1317–1325. doi: 10.1016/S1470-2045(13)70502-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzdar AU, Valero V, Ibrahim NK, Francis D, Broglio KR, Theriault RL, Pusztai L, Green MC, Singletary SE, Hunt KK, Sahin AA, Esteva F, Symmans WF, Ewer MS, Buchholz TA, Hortobagyi GN. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomized study population and data of additional patients treated with the same regimen. Clin Cancer Res. 2007;13 (1:228–233. doi: 10.1158/1078-0432.CCR-06-1345. [DOI] [PubMed] [Google Scholar]
- Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, Wickerham DL, Bogaerts J, Baselga J, Perou C, Blumenthal G, Blohmer J, Mamounas EP, Bergh J, Semiglazov V, Justice R, Eidtmann H, Paik S, Piccart M, Sridhara R, Fasching PA, Slaets L, Tang S, Gerber B, Geyer CE, Jr, Pazdur R, Ditsch N, Rastogi P, Eiermann W, von Minckwitz G. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384 (9938:164–172. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80 (1:27–38. [Google Scholar]
- Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER, Wickerham DL, Begovic M, DeCillis A, Robidoux A, Margolese RG, Cruz AB, Jr, Hoehn JL, Lees AW, Dimitrov NV, Bear HD. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 1998;16 (8:2672–2685. doi: 10.1200/JCO.1998.16.8.2672. [DOI] [PubMed] [Google Scholar]
- Gianni L, Eiermann W, Semiglazov V, Lluch A, Tjulandin S, Zambetti M, Moliterni A, Vazquez F, Byakhov MJ, Lichinitser M, Climent MA, Ciruelos E, Ojeda B, Mansutti M, Bozhok A, Magazzù D, Heinzmann D, Steinseifer J, Valagussa P, Baselga J. Neoadjuvant and adjuvant trastuzumab in patients with HER2-positive locally advanced breast cancer (NOAH): follow-up of a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet Oncol. 2014;15 (6:640–647. doi: 10.1016/S1470-2045(14)70080-4. [DOI] [PubMed] [Google Scholar]
- Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, Lluch A, Staroslawska E, de la Haba-Rodriguez J, Im SA, Pedrini JL, Poirier B, Morandi P, Semiglazov V, Srimuninnimit V, Bianchi G, Szado T, Ratnayake J, Ross G, Valagussa P. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13 (1:25–32. doi: 10.1016/S1470-2045(11)70336-9. [DOI] [PubMed] [Google Scholar]
- Goldhirsch A, Gelber RD, Piccart-Gebhart MJ, de Azambuja E, Procter M, Suter TM, Jackisch C, Cameron D, Weber HA, Heinzmann D, Dal Lago L, McFadden E, Dowsett M, Untch M, Gianni L, Bell R, Köhne CH, Vindevoghel A, Andersson M, Brunt AM, Otero-Reyes D, Song S, Smith I, Leyland-Jones B, Baselga J, Herceptin Adjuvant Trial Study Team 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet. 2013;382 (9897:1021–1028. doi: 10.1016/S0140-6736(13)61094-6. [DOI] [PubMed] [Google Scholar]
- Gralow JR, Burstein HJ, Wood W, Hortobagyi GN, Gianni L, von Minckwitz G, Buzdar AU, Smith IE, Symmans WF, Singh B, Winer EP. Preoperative therapy in invasive breast cancer: pathologic assessment and systemic therapy issues in operable disease. J Clin Oncol. 2008;26 (5:814–819. doi: 10.1200/JCO.2007.15.3510. [DOI] [PubMed] [Google Scholar]
- Joensuu H, Bono P, Kataja V, Alanko T, Kokko R, Asola R, Utriainen T, Turpeenniemi-Hujanen T, Jyrkkiö S, Möykkynen K, Helle L, Ingalsuo S, Pajunen M, Huusko M, Salminen T, Auvinen P, Leinonen H, Leinonen M, Isola J, Kellokumpu-Lehtinen PL. Fluorouracil, epirubicin, and cyclophosphamide with either docetaxel or vinorelbine, with or without trastuzumab, as adjuvant treatments of breast cancer: final results of the FinHer Trial. J Clin Oncol. 2009;27 (34:5685–5692. doi: 10.1200/JCO.2008.21.4577. [DOI] [PubMed] [Google Scholar]
- Kim MM, Allen P, Gonzalez-Angulo AM, Woodward WA, Meric-Bernstam F, Buzdar AU, Hunt KK, Kuerer HM, Litton JK, Hortobagyi GN, Buchholz TA, Mittendorf EA. Pathologic complete response to neoadjuvant chemotherapy with trastuzumab predicts for improved survival in women with HER2-overexpressing breast cancer. Ann Oncol. 2013;24 (8:1999–2004. doi: 10.1093/annonc/mdt131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivot X, Romieu G, Debled M, Pierga JY, Kerbrat P, Bachelot T, Lortholary A, Espié M, Fumoleau P, Serin D, Jacquin JP, Jouannaud C, Rios M, Abadie-Lacourtoisie S, Tubiana-Mathieu N, Cany L, Catala S, Khayat D, Pauporté I, Kramar A, PHARE trial investigators 6 months versus 12 months of adjuvant trastuzumab for patients with HER2-positive early breast cancer (PHARE): a randomised phase 3 trial. Lancet Oncol. 2013;14 (8:741–748. doi: 10.1016/S1470-2045(13)70225-0. [DOI] [PubMed] [Google Scholar]
- Pritchard KI. Optimizing the delivery of targeted research: an opportunity for comparative effectiveness research. J Clin Oncol. 2010;28 (7:1089–1091. doi: 10.1200/JCO.2009.25.2205. [DOI] [PubMed] [Google Scholar]
- Takada M, Ishiguro H, Nagai S, Ohtani S, Kawabata H, Yanagita Y, Hozumi Y, Shimizu C, Takao S, Sato N, Kosaka Y, Sagara Y, Iwata H, Ohno S, Kuroi K, Masuda N, Yamashiro H, Sugimoto M, Kondo M, Naito Y, Sasano H, Inamoto T, Morita S, Toi M. Survival of HER2-positive primary breast cancer patients treated by neoadjuvant chemotherapy plus trastuzumab: a multicenter retrospective observational study (JBCRG-C03 study) Breast Cancer Res Treat. 2014;145 (1:143–153. doi: 10.1007/s10549-014-2907-9. [DOI] [PubMed] [Google Scholar]
- Untch M, Fasching PA, Konecny GE, Hasmuller S, Lebeau A, Kreienberg R, Camara O, Müller V, du Bois A, Kühn T, Stickeler E, Harbeck N, Höss C, Kahlert S, Beck T, Fett W, Mehta KM, von Minckwitz G, Loibl S. Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol. 2011;29 (25:3351–3357. doi: 10.1200/JCO.2010.31.4930. [DOI] [PubMed] [Google Scholar]
- Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF, American Society of Clinical Oncology; College of American Pathologists Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31 (31:3997–4013. doi: 10.1200/JCO.2013.50.9984. [DOI] [PubMed] [Google Scholar]