Abstract
Background:
Prostate cancer is the sixth most common cancer worldwide and will include about 30% of all malignancies in men. Since the initial report of the anatomic radical prostatectomy, refinements in the surgical technique have been made. Several studies show that bladder neck preservation (BNP) during radical prostatectomy makes improve early return of urinary continence, erectile function or both. However, some clinical trials have suggested little difference between the return of continence while using modifications. In this study, we compared outcomes of BNP and bladder neck reconstruction (BNR) during radical retropubic prostatectomy (RRP).
Materials and Methods:
This prospective study was performed on 60 patients at a referral university hospital from March 2010 to March 2012. Study population was all patients candidate for RRP (RRP in this period. All patients divided into two groups, A and B (30 patients in each group). Group A (n = 30) who preserved bladder neck (BNP) and Group B (n = 30) who had BNR. Prostate specific antigen (PSA) before and at 2, 6, 9, 12 and18 months after surgery, anastomotic stricture symptoms, positive bladder neck margin, Gleason score and urine incontinence were compared between two groups. Also, we compared bladder neck contracture, urinary continence and positive surgical margin rates after BNP and BNR while retropubic prostatectomy in 24 months period follow-up.
Results:
The mean age of the patients was 61.81 ± 7.15 years (range, 50-74 years). After a follow-up period of 24 months, the PSA rising was not different between the two groups. After 2 months, 19 (63.33%) of patients in A group and the same number in B group were continent (P = 0.78). Stricture of the bladder neck at the anastomosis site requiring transurethral dilation occurred in 7 (23.33%) and 3 (10.0%) patients in groups A and B, respectively (P = 0.04).
Conclusion:
Although there was no difference in prevalence and duration of return of urinary continence after the operation between two groups, but results of our study showed that stenosis of the bladder neck was lower in BNP. Hence in the group of BNP, need for further operation and overflow incontinency due to the obstruction of urinary tract will be less likely than BNR and patients have better long time (24 months) urinary continence.
Keywords: Bladder neck preservation, bladder neck reconstruction, prostate cancer, prostatectomy, urinary incontinenc
INTRODUCTION
Prostate cancer is the sixth most common cancer worldwide and will include about 30% of all malignancies in men.[1,2] The standard treatments for prostate cancer without clinical evidence of distant metastases are radical prostatectomy surgery, radiotherapy, brachytherapyand are active surveillance.[2] Among these methods, radical prostatectomy is an effective treatment for localized prostate cancer and it is based on long-term control of the disease.[3,4,5,6] However, this method is likely to cause injury to the urinary sphincter. Urinary incontinence has always been associated with serious complications and it's trying to obtain the best results which improve the condition and the choice of surgical technique in this field. Since the initial report of the anatomic radical prostatectomy, refinements in the surgical technique have been made. Some studies show modifications of radical retropubic prostatectomy (RRP) have minimized the short-term and long-term morbidity of the procedure or the oncologic outcome and have been incorporated into the classic operation;[7,8,9] others have demonstrated no or minimal measurable benefit or negative benefit and have been abandoned.[10,11]
Several studies show that bladder neck preservation (BNP) during radical prostatectomy makes improve early return of urinary continence, erectile function or both. These studies have focused on the function of the bladder neck in urinary control, dissection around the seminal vesicles.[12,13,14,15,16] Walsh has found that with intussusceptions of the bladder neck, 80% of men are pad free at 3 months and 98% at 1 year.[17]
On the other hand, some clinical trials have suggested little difference between the return of continence in the short-term (3-6 months after surgery) and long-term (1 year after surgery) while using modifications.[14,18,19] At the same time preserved positive margin at the bladder neck in many cases makes the effectiveness of this method questionable.[16]
Since previous studies on compare of effects of BNP and bladder neck reconstruction (BNR) techniques on urinary incontinence after radical prostatectomy are controversial, we performed a study on the outcomes of BNP during RRP considering post-operative urinary continence and stenosis of the bladder neck.
MATERIALS AND METHODS
This randomized clinical trial was performed at Al zahra Hospital of Isfahan from March 2010 to March 2012 (research project number 78633). Study population was all patients candidate for RRP in this period. Inclusion criteria included the candidacy of radical prostatectomy for retro pubic prostate cancer surgery (prostate specific antigen [PSA] <20, Gleason score <8 and clinical stage ≤T2b), no history of previous surgery on the prostate and bladder neck and had no history of urinary incontinence and consent to participate in the study. Exclusion criteria included candidates for other treatments other than RRP.
After reading method, explained benefits and risks of treatment, for patients with inclusion criteria and obtaining their informed consent, all patients operated by one surgeon.
Pre-operative demographic data recorded in age, pre-operative clinical factors, including PSA levels and pathological findings recorded in the presence of a previous biopsy.
All patients divided randomized into two groups with simple randomization method, A and B. Group A who preserved bladder neck BNP and Group B who had bladder neck reconstruction BNR.
In both methods of surgery after lower midline incision by extra peritoneal approach and ligation of dorsal vein, apex of the prostate was divided from the urethra. Then by saving of neurovascular bundle, prostate was separated from rectum up to the bladder.
In BNP technique prostate was divided from the bladder in the border between the bladder and prostate without disturbing bladder neck anatomy. But in BNR technique, prostate and bladder neck were separated from the bladder and then bladder neck was reconstructed by tennis racquet technique. Finally bladder was anastomosed to the urethra in both methods.[12,13]
In total, 60 patients (30 in each group) studied. BNR in Group B was a classic Tennis racket closure. Other technical considerations during surgery (BNR and BNP) were also recorded. At 2 months after surgery, the serum PSA measured and every 3 month for the 1st year and then in the absence of recurrence every 6 month.
Recurrence was considered to increase in serum PSA >0.4 ng/ml measured on 2 times during follow-up after surgery.
Patients who came with obstructive symptoms or urinary retention and confirmed by cystourethroscopy considered as an anastomotic site stricture. Furthermore anastomotic stricture symptoms of lower urinary tract symptoms (irritative symptoms such as dysuria and frequency, obstructive symptoms such as hesitancy, dribbling and reduced force and caliber), urinary retention and other symptoms recorded. Other variables reviewed, include ratings Gleason (Gleason score) based on pathology reports.[14,15] Incontinence of urine defined to use the pad to control urinary leakage if it is needed. The pad test is a non-invasive diagnostic tool for urinary incontinence. It is an easy to perform, inexpensive test with utilization in both the daily patient care and clinical research and it is clear value in initial diagnosis, selection of treatment and follow-up evaluation.[16] Urinary incontinence recovery time and improvement of recovery investigated. For statistical analysis, we used independent t-test and for qualitative variables used Chi-square or Fisher exact test. All data analyzed with Statistical Package for the Social Science (SPSS) software version 20 (SPSS Inc., Chicago, IL, USA).
RESULTS
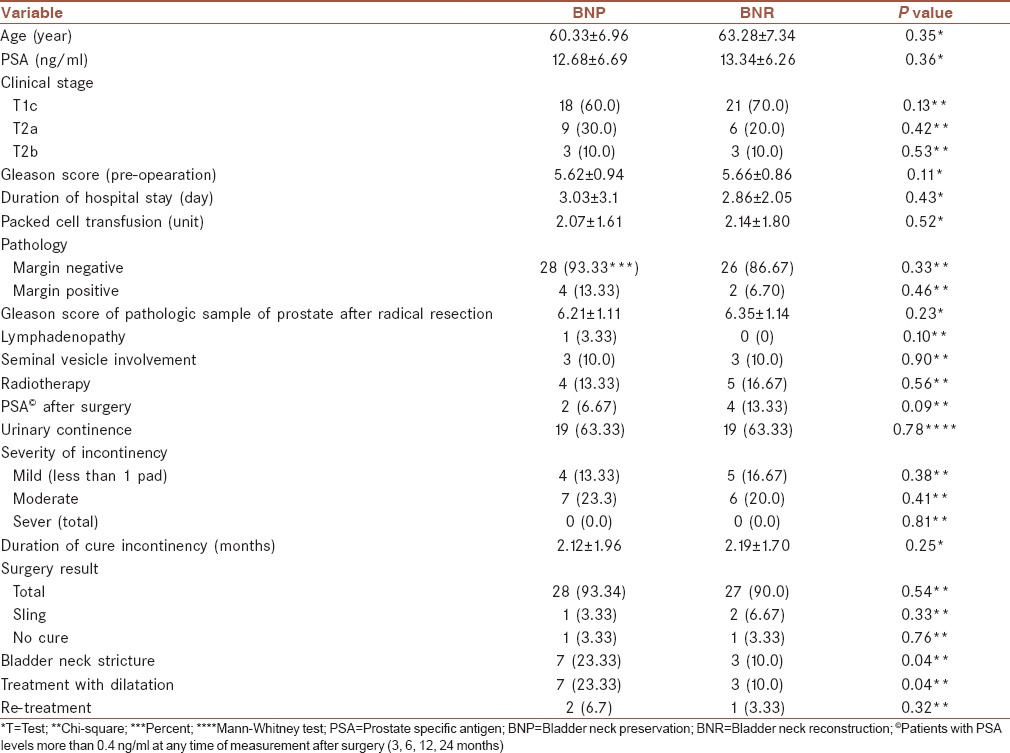
The mean age of the patients was 61.81 ± 7.15 years (range, 50-74 years). 30 patients had RRP with BNP (Group A) and 30 had undergone the same operation with BNR (Group B). There were no differences in characteristics of the patients between the two groups [Table 1]. After a follow-up period of 24 months, the PSA rising was not different between the two groups [Table 1]. 19 (63.33%) of patients in Group A and the same number in Group B were continent after catheter removal in first visit and difference between two groups was not significant (P = 0.78) and ultimate consequence after 18 months was 28 (93.34) versus 27 (90.0) total continent in BNP and BNR respectively with no significant difference (P = 0.54). Stricture of the bladder neck at the anastomosis site requiring transurethral dilation occurred in 7 (23.33%) and 3 (10.0%) patients in Groups A and B, respectively and difference between two groups was 1.
Table 1.
Patient's characteristics outcome of BNP compared with BNR
DISCUSSION
In the present study, we compared bladder neck contracture, urinary continence and positive surgical margin rates after BNP and BNR while retro pubic prostatectomy after 24 months period follow-up. We found that there is no difference between two group in achieving urinary continence and duration of this achievement.
Several studies show that BNP during radical prostatectomy makes improve early return of urinary continence, erectile function, or both. These studies have focused on the function of the bladder neck in urinary control, dissection around the seminal vesicles.[17,18,19,20,21]
Walsh has found that with intussusceptions of the bladder neck, 80% of men are pad free at 3 months and 98% at 1 year.[22]
On the other hand, some clinical trials have suggested little difference between the return of continence in the short-term (3-6 months after surgery) and long-term (1 year after surgery) while using modifications.[19,23,24] At the same time preserved positive margin at the bladder neck in many cases makes the effectiveness of this method questionable.[21]
Klein was the first to suggest that modification of the bladder neck resection and reconstruction at the time of RRP might influence urinary control.[17]
In a retrospective study of Razi et al. on 103 patients into two groups of BNP (51 patients) and BNR (52 patients) who had undergone RRP, they found BNP during RRP may improve long-term results of urinary continence and be effective in eradicating prostate cancer without increasing the recurrence rate. They also found there were no significant differences in the frequency of biochemical failure and bladder neck stricture that required dilation between the two groups of patients.[25]
Nevertheless, in a study of Poon et al. found no statistically significant differences in return of urinary continence, bladder neck contracture rates or positive margins between BNP and excision. They also found continence rates at 1 year were 93% for BNP, 96% for tennis racket reconstruction and 97% for anterior bladder tube reconstruction, which was not significant and in this study positive margin rates were 27.4% with BNP versus 30.5% with excision, which was not significantly different.[23]
Results of other study showed that BNP may aid in an earlier return of continence following radical prostatectomy and reduces anastomotic strictures. Study of Braslis et al. suggested that preservation of the bladder neck during radical prostatectomy does not appear to compromise the efficacy of the procedure.[26]
Strictures are a common, but easily managed complication of RRP for prostate cancer. In a review article, 456 patients with an adequate follow-up to determine stricture formation, 82.5% had no strictures, 6.8% required a single dilation, 3.7% required two dilations, 3.1% required three dilations and 3.9% required more than three dilations. Of these patients, 80.1% required no pads, 8.1% required 1-2 pads a day, 6.6% required 3-5 pads a day and 5.2% were totally incontinent 1 year or more after surgery. Urinary incontinence was closely associated with post-operative urinary urgency.[27]
In our study, BNP patients who placed under the bladder neck stenosis were less than BNR patients were this problem could be less in patients who are not bladder reconstruction) because this did not manipulate the neck of the bladder and its natural).
On the other hand, during reconstruction of the bladder neck (using a tennis racket method) tension and pressure on the bladder neck tissue due to suture and the absence of normal anatomic neck reconstruction can cause an increase in the bladder neck stenosis in this group.
Although there was no difference in prevalence and duration of return of urinary continence after the operation between two groups, but results of our study showed that stenosis of the bladder neck was lower in BNP. So in the group of BNP, need for further operation and overflow incontinency due to the obstruction of urinary tract will be less likely than BNR and patients have better long time urinary continence and this method does not increase the recurrence of prostate cancer. However, in the studies conducted, patients were not followed in long period and association of BNP with urinary incontinence is still not well defined, so, further studies are necessary to clarify the role of BNP during RRP.
Limitation of the study: Small number of patients.
AUTHOR'S CONTRIBUTIONS
MHI contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. RH contributed in the conception of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MHKh contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MRN contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MMS contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. FA contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
Footnotes
Source of Support: Isfahan University of Medical Science.
Conflict of Interest: None declared.
REFERENCES
- 1.Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177:2106–31. doi: 10.1016/j.juro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 2.National comprehensive cancer network (NCCN) guidelines. [Last accessed: 2/17/2013]. Available from: http://www.nccn.org/professionals/physician_gls/default.asp .
- 3.Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD. Contemporary update of prostate cancer staging nomograms (partin tables) for the new millennium. Urology. 2001;58:843–8. doi: 10.1016/s0090-4295(01)01441-8. [DOI] [PubMed] [Google Scholar]
- 4.O’Hara JF, Jr, Sprung J, Klein EA, Dilger JA, Domen RE, Piedmonte MR. Use of preoperative autologous blood donation in patients undergoing radical retropubic prostatectomy. Urology. 1999;54:130–4. doi: 10.1016/s0090-4295(99)00042-4. [DOI] [PubMed] [Google Scholar]
- 5.Steiner MS. The puboprostatic ligament and the male urethral suspensory mechanism: An anatomic study. Urology. 1994;44:530–4. doi: 10.1016/s0090-4295(94)80052-9. [DOI] [PubMed] [Google Scholar]
- 6.Lowe BA. Preservation of the anterior urethral ligamentous attachments in maintaining post-prostatectomy urinary continence: A comparative study. J Urol. 1997;158:2137–41. doi: 10.1016/s0022-5347(01)68180-1. [DOI] [PubMed] [Google Scholar]
- 7.Rogers CG, Trock BP, Walsh PC. Preservation of accessory pudendal arteries during radical retropubic prostatectomy: Surgical technique and results. Urology. 2004;64:148–51. doi: 10.1016/j.urology.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 8.Walsh PC. Radical prostatectomy for localized prostate cancer provides durable cancer control with excellent quality of life: A structured debate. J Urol. 2000;163:1802–7. [PubMed] [Google Scholar]
- 9.Walsh PC. Nerve grafts are rarely necessary and are unlikely to improve sexual function in men undergoing anatomic radical prostatectomy. Urology. 2001;57:1020–4. doi: 10.1016/s0090-4295(01)00987-6. [DOI] [PubMed] [Google Scholar]
- 10.Steiner MS, Burnett AL, Brooks JD, Brendler CB, Stutzman RE, Carter HB. Tubularized neourethra following radical retropubic prostatectomy. J Urol. 1993;150:407–9. doi: 10.1016/s0022-5347(17)35494-0. [DOI] [PubMed] [Google Scholar]
- 11.Parsons JK, Marschke P, Maples P, Walsh PC. Effect of methylprednisolone on return of sexual function after nerve-sparing radical retropubic prostatectomy. Urology. 2004;64:987–90. doi: 10.1016/j.urology.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 12.Brunocilla E, Borghesi M, Schiavina R, Pultrone CV, Martorana G. Re: Impact of complete bladder neck preservation on urinary continence, quality of life and surgical margins after radical prostatectomy: A randomized, controlled, single blind trial. Eur Urol. 2013;64:338–9. doi: 10.1016/j.eururo.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 13.Nyarangi-Dix JN, Radtke JP, Hadaschik B, Pahernik S, Hohenfellner M. Impact of complete bladder neck preservation on urinary continence, quality of life and surgical margins after radical prostatectomy: A randomized, controlled, single blind trial. J Urol. 2013;189:891–8. doi: 10.1016/j.juro.2012.09.082. [DOI] [PubMed] [Google Scholar]
- 14.Egevad L, Granfors T, Karlberg L, Bergh A, Stattin P. Prognostic value of the Gleason score in prostate cancer. BJU Int. 2002;89:538–42. doi: 10.1046/j.1464-410x.2002.02669.x. [DOI] [PubMed] [Google Scholar]
- 15.Josefsson A, Wikström P, Granfors T, Egevad L, Karlberg L, Stattin P, et al. Tumor size, vascular density and proliferation as prognostic markers in GS 6 and GS 7 prostate tumors in patients with long follow-up and non-curative treatment. Eur Urol. 2005;48:577–83. doi: 10.1016/j.eururo.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 16.Krhut J, Zachoval R, Smith PP, Rosier PF, Valanský L, Martan A, et al. Pad weight testing in the evaluation of urinary incontinence. Neurourol Urodyn. 2013 Jun 24; doi: 10.1002/nau.22436. doi: 10.1002/nau.22436. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Klein EA. Early continence after radical prostatectomy. J Urol. 1992;148:92–5. doi: 10.1016/s0022-5347(17)36519-9. [DOI] [PubMed] [Google Scholar]
- 18.Licht MR, Klein EA, Tuason L, Levin H. Impact of bladder neck preservation during radical prostatectomy on continence and cancer control. Urology. 1994;44:883–7. doi: 10.1016/s0090-4295(94)80175-4. [DOI] [PubMed] [Google Scholar]
- 19.Shelfo SW, Obek C, Soloway MS. Update on bladder neck preservation during radical retropubic prostatectomy: Impact on pathologic outcome, anastomotic strictures and continence. Urology. 1998;51:73–8. doi: 10.1016/s0090-4295(97)00463-9. [DOI] [PubMed] [Google Scholar]
- 20.Soloway MS, Neulander E. Bladder-neck preservation during radical retropubic prostatectomy. Semin Urol Oncol. 2000;18:51–6. [PubMed] [Google Scholar]
- 21.Srougi M, Nesrallah LJ, Kauffmann JR, Nesrallah A, Leite KR. Urinary continence and pathological outcome after bladder neck preservation during radical retropubic prostatectomy: A randomized prospective trial. J Urol. 2001;165:815–8. [PubMed] [Google Scholar]
- 22.Walsh PC, Marschke PL. Intussusception of the reconstructed bladder neck leads to earlier continence after radical prostatectomy. Urology. 2002;59:934–8. doi: 10.1016/s0090-4295(02)01596-0. [DOI] [PubMed] [Google Scholar]
- 23.Poon M, Ruckle H, Bamshad BR, Tsai C, Webster R, Lui P. Radical retropubic prostatectomy: Bladder neck preservation versus reconstruction. J Urol. 2000;163:194–8. doi: 10.1016/s0022-5347(05)68003-2. [DOI] [PubMed] [Google Scholar]
- 24.Deliveliotis C, Protogerou V, Alargof E, Varkarakis J. Radical prostatectomy: Bladder neck preservation and puboprostatic ligament sparing — Effects on continence and positive margins. Urology. 2002;60:855–8. doi: 10.1016/s0090-4295(02)01956-8. [DOI] [PubMed] [Google Scholar]
- 25.Razi A, Yahyazadeh SR, Sedighi Gilani MA, Kazemeyni SM. Bladder neck preservation during radical retropubic prostatectomy and postoperative urinary continence. Urol J. 2009;6:23–6. [PubMed] [Google Scholar]
- 26.Braslis KG, Petsch M, Lim A, Civantos F, Soloway MS. Bladder neck preservation following radical prostatectomy: Continence and margins. Eur Urol. 1995;28:202–8. doi: 10.1159/000475052. [DOI] [PubMed] [Google Scholar]
- 27.Geary ES, Dendinger TE, Freiha FS, Stamey TA. Incontinence and vesical neck strictures following radical retropubic prostatectomy. Urology. 1995;45:1000–6. doi: 10.1016/s0090-4295(99)80121-6. [DOI] [PubMed] [Google Scholar]


