Abstract
Keratoconus (KC) is the most common ectasia of the cornea and is a common reason for corneal transplant. Therapeutic strategies that can arrest the progression of this disease and modify the underlying pathogenesis are getting more and more popularity among scientists. Cumulating data represent strong evidence of a genetic role in the pathogenesis of KC. Different loci have been identified, and certain mutations have also been mapped for this disease. Moreover, Biophysical properties of the cornea create an appropriate candidate of this tissue for gene therapy. Immune privilege, transparency and ex vivo stability are among these properties. Recent advantage in vectors, besides the ability to modulate the corneal milieu for accepting the target gene for a longer period and fruitful translation, make a big hope for stupendous results reasonable.
Keywords: Cornea, gene therapy, genetics, keratoconus
Introduction
Keratoconus (KC) is a progressive noninflammatory etatic disease of the cornea. It, usually, begins in puberty and its advance is predictably arrested in the 3rd or 4th decades of life.[1] KC is regarded as the most common corneal ectasia[2] with its estimated incidence in different society ranges from 5 to 20 in 10,000 persons and a prevalence of 54 in 100,000 is reported according to different studies.[3,4] KC is considered to have a genetic basis. Many genes including visual system homeobox 1 (VSX1) gene, superoxide dismutase 1 (SOD1) gene and lysyl oxidase (LOX), and genetic mutations are associated with KC in several studies. Linkage studies in familial KC, genome-wide association studies and twin studies also found that there is a genetic predisposition to KC.[5,6,7,8,9,10] These findings envisage gene therapy as a possible treatment option for KC.
Method of Literature Review
We searched the National Library of Medicine's PubMed database and Elsevier Scopus database with a subsequent review of the accompanying references. The major search words and word combinations included: Genetic of KC; gene therapy of KC, genetic treatment of KC, the perspective of KC, molecular studies of KC, management and treatment options of KC, diagnosis of KC.
In addition, the citations from the above searches were also included. Cases from the non-English literature were not included. All identified documents were examined, and those that were relevant were retrieved for inclusion in the review.
Pathogenesis
The exact pathophysiology of KC till now is not well established. Interaction between environmental and genetic factors seem to play a role. In susceptible patients environmental factors such as trauma, ultraviolet or atopy trigger an inflammatory cascade leading to degeneration of the corneal stroma.[11]
Imbalances between pro-inflammatory agents and anti-inflammatory agents have been found. On the corneal keratinocytes of KC patient, Interleukin 1 receptors are presented four times more than normal keratinocytes. This cytokine induces keratinocytes apoptosis and regulates keratinocyte proliferation and differentiation.[12,13] Intercellular adhesion molecule-1, Vascular cell adhesion molecule-1 and interleukin 6 are even expressed as much as 40 times, whereas expressions of anti-inflammatory agents like interleukin 10 are markedly reduced.[14]
It is suggested that interleukin 1 has a role in modulating the expression of metalloproteinase.[13] Disparities between proteinase and proteinase inhibitor activity have also been postulated[15] and can lead to the corneal stromal degradation; as the core pathological finding in KC. It has been found that in the keratoconic eyes proteinase inhibitors levels such as α2-macroglobulin and α1-antiprotease are significantly less than normal eyes[16] and a higher activity of lysosomal and catabolic enzymes like proteinase has been reported.[17]
Collagen alignment and components are also of significant importance.[18] Researchers found differences in certain collagen types between normal and keratoconic eyes and retard in the wound healing process could be attributed to these differences.[19]
Diagnosis
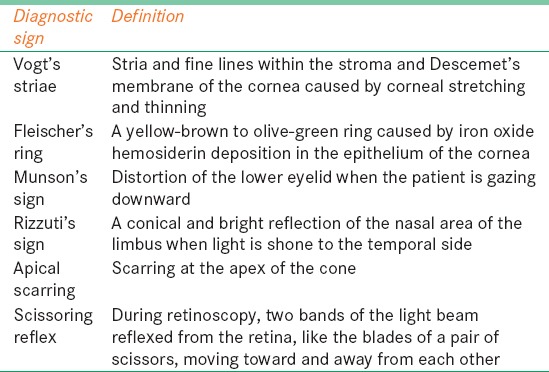
Diagnosis of KC is based on slit-lamp clinical examination or corneal topography imaging. On slit-lamp examination conical protrusion of the cornea, Vogt's striae, Fleischer's ring, Munson's sign, Rizzuti's sign, corneal scars and scissoring reflex by retinoscopy might be visible [Table 1].
Table 1.
Definition of keratoconus diagnostic signs
Management
In the very early phase, spectacles can be applied but contact lenses are the first choice of therapy for more than 90% of the patients. Soft contact lenses are used in the early phases, but with progressions of the disease rigid gas permeable lenses are more functional. Patients with severe KC or those who do not tolerate a contact lens, surgery are the next step. Penetrating keratoplasty, in which the full thickness of the cornea is removed enjoys from the most popularity. Deep anterior lamellar keratoplasty, photorefractive keratectomy, intrastromal corneal ring segment implantation and implantation of intraocular lens are other surgical maneuvers that are applied solely or in combination with other techniques.[20,21,22]
Genetic Background
Reports of identical twins that progressed KC in the literature brought up the possibility of the genetic basis for this disease. This hypothesis got stronger by the positive family history in almost 10% of these patients.[23] The rate has got a significant rise by the introduction of corneal topography in this field and approximates >50%. Moreover, clustering of KC in two or three generations in a family was another supportive finding.[24,25,26,27,28]
The suggested mode of inheritance in most papers is autosomal dominant with variable expression.[29,30] In a study by Himmerstien in 1974 on 52 families, the degree of penetrance was postulated to be about 20%.[26] Other researchers who reported a higher rate included subclinical or fruste types as well as high degrees of astigmatism as an incomplete expression of KC gene defining variable expression in this mode of inheritance.[27] Nevertheless, other modes of inheritance are also proposed, and it does not seem that a fixed Mendelian model can express the genetic influence in all the cases.[31]
Concordance of KC with certain systemic disorders like: Trisomy 21.[32] or connective tissue diseases such as osteogenesis imperfecta,[33] Ehlers-Danlos syndrome[4,31] and Leber congenital amaurosis[34] are another clues for the genetic role.
Predominance of certain human leukocyte antigens in keratoconic patients has also been investigated by some researchers to clarify the hereditary background.[35] These hard attempts to find a possible genetic basis for KC were aimed to find the guilty gene(s)and open a new prospect for the future treatment.
Keratoconus and Genetic Bases
Despite the familial form of the disease that mostly follows the autosomal dominant mode of inheritance; most cases of KC appear sporadically in a polygenic fashion.[23] Complex genetic phenomena and interaction make the identification of the causative gene difficult. One of the strategies to allocate the contributing gene is linkage analysis. In this approach, multiple families in more than one generation become recruited. Both affected and unaffected members undergo genetic analysis. Chromosomal regions that are distributed equally between affected and unaffected members are not likely to be the causative genes. After defining the chromosomal region, the mapped gene with that region gets clarified. Phenocopy, which is an individual who is not genetically vulnerable but probably under the effect of environmental factors show the disease phenotype, along with penetration, which is the ratio of positive genotypes, who show the phenotype of the disease and genetic heterogeneity especially locus heterogeneity, same phenotype as a result of different causative loci mutation, are important genetic phenomena that influence the linkage analysis and limit the consequent result.[36,37,38,39]
Several studies, especially in recent years have isolated the causative loci using this strategy.[36,37,38,40,41] In a study that was conducted in Australia, no chromosomal linkage but two loci were found (1p36.23–36.21 and 8q13.1–q21.11).[42] In a study on Ecuadorian society, researchers found a mutation at 13q32.[43] This locus is very proximal to the gene coding for collagen type IV, α1 and collagen type IV, α2. This neighborhood brought up the hypothesis of a possible mutation in these genes. The investigation, which put this hypothesis into practice, found no new mutations.[43] Further studies in other nations found other causative regions. And chromosomal regions like 3p14-q13, 5q14-q21, 15q22-q24, 16q22-q23 and 9q34 were represented in different studies.[36,38,40,41,44,45]
However, other scientists could replicate none of these regions and their exact role in the different ethnical group remains blurred. In a study by Saee-Rad et al.,[8] six previously described loci (2p, 3p, 5q, 15q, 16q, and 20q) underwent haplotype analysis and no linkage was associated with KC in the recruited families.
Like other complex diseases, gene-gene interaction is another defining genetic event that should be considered. How different genes under the effect of environmental factors interact with each other to form the subsequent phenotype has only barely been investigated. Burdon et al.[42] also found in their study that single locus analysis resulted in less LOD score (logarithm (base 10) of odds) than analyzing two regions concurrently and this finding bolds these important interactions.
These complexities in interpreting gene analyses have restricted defining new loci and were partly responsible for the unproductive investigation in finding blameworthy gene(s)
Of these very few genes, VSX1 is especially popular. First described in 2002,[46] VSX1 is a homeobox gene that binds to the control region of red/green visual pigment gene cluster and is likely to regulate the expression of cone opsin. Different mutations of this gene were identified in some with anomalous development of endothelium along with a few families with KC and posterior corneal dystrophy.[46,47,48,49] In a study by Bisceglia et al.[50] on 80 keratoconic eyes, VSX1 was concluded to be an important gene in autosomal dominant KC and four different defining mutations were found.
Other studies reported other mutations and proposed their likely pathological effect.[51,52,53] Complete code region of VSX1 underwent analyze, and two non-synonymous mutations (H244R and R166W) were established. H244R was only found in affected people, and healthy individuals did not carry this mutation.[8] Another researcher has already suggested a pathological role for this mutation.[54] On the other hand, there are cumulating amount of data that brings the role of VSX1 gene and its mutations into question.[55,56] and in a recent study by Stabuc-Silih et al.[57] on 113 Slovenian patients, no disease causing mutation was found.
Another candidate gene that was appealing for researchers in the pathogenesis of KC is the SOD1 on chromosome 21.[58] Fewer studies than VSX1 have investigated this gene in keratoconic eyes. After complete sequencing of all five exons of the gene, Udar et al. found a unique genomic deletion within intron 2 close to the 5’ splice junction of the SOD1 in three patients with KC[58] a mutation that was not observed in normal individuals. This finding was not confirmed in other studies.[45,57] Other genes, especially those of collagen, the major protein of the cornea drew the attention of some scientists.[39]
Cornea, a Good Candidate for Gene Therapy Past and Future
Corneal gene therapy as a powerful method that can modify the ultrastructure of the cell protein is potentially helpful in many of hereditary and acquired corneal abnormalities.
In 1994, Mashhour et al. transferred successfully gene to the cornea with the application of adenovirus as a vector.[59] Since then, new aspects were recognized for this apparatus. Transferring cytokines, growth factors and enzymes to the cornea in a sustained concentration that is hardly if at all achievable with systemic administration along with knock down of defective genes and inducing the functional genes are only part of the presumed advantages.[60,61]
In preclinical studies, outstanding results for this method have been obtained. Researchers found promising results in the prevention and treatment of major corneal issues like herpetic stromal keratitis (HSK), corneal graft rejection, neovascularization and haze.[61,62,63,64,65,66] This method has also been postulated for other corneal abnormality like KC[67] and corneal dystrophies.[68,69]
There are lots of intrinsic characters that make the cornea an ideal candidate for gene therapy. One of these important characters is the exceptional policy of the immune system towards this tissue in comparison to others, the so-called immune privilege.
Excessive inflammation that is considered to be a very useful strategy against microorganism and is one of the routine immune response to combat the offending enemy is extremely harmful to cornea. This inflammation easily causes opacities in the cornea that affects the vision significantly.
The margination of the inflammatory cells is restricted by a blood ocular barrier. Even after entrance the activity of these cells becomes suspiciously inhibited. Endothelial cells express molecules that inhibit complement activation and subsequently the opsonization and destructive effect of the complement cascade. Presenting the antigens to immune cells is also modified in this tissue and corneal cells express comparatively lower histocompatibility complex of both classes (I and II). Lymphatic drainage as a pathway to present the antigens to dendritic cells in lymph nodes are lacking as well and fas ligands that are presented on the surface of the corneal cells induce apoptosis in activated T cells And for reasons that are poorly understood, presenting B cells do not secrete complement fixating immunoglobulins M and immunoglobulins G2.[70,71]
These features give a unique property to the cornea for accommodating the gene vectors without consequent immunogenicity and thus will guarantees longer gene expression.
Other properties like the stability ex vivo are particularly of significant importance.[64,72] This feature makes the successful manipulation for gene therapy out of the body possible.
Easily accessible[64,72,73,74] and anesthetized[75] along with transparency,[64,65,72] which makes direct observation of the procedure progress effortless, are other technical facilities that this tissue offers to ophthalmologists.
Technique
Basics of the techniques are the same as gene therapy in other tissues. Gene that its downstream products are desirable is transferred to an appropriate vector. The vector is then injected into the tissue in a particular way to obtain and enter the target cell and with the application of the protein synthesis machinery of the cell, gene translation starts.
An optimal vector must suit for the purpose of the gene therapy and a property that is essential for one vector might be useless and even harmful for another. However as a rule, the less immunogenic be a vector, the better. Besides, vectors that can carry larger sequence are often preferred under equal condition, and the ability to express both in proliferative and non-proliferative cells is another functional feature.
At the present time, there are viral and non-viral vectors. Adenovirus, Herpes simplex virus, Lentiviruses, Retroviruses and Adeno-associated virus is among the most popular viral vectors[76,77,78,79,80,81] and Naked DNA, Cationic liposomes, Minimalistic immunologically defined gene expression vectors as well as Polyethylenimines and Polyamidoamine dendrimers are among the non-viral biologic methods.[81,82,83]
Physical methods have also moved forward and progressed in recent years. Electroporation, Sonoporation and Gene gun have been utilized with real success.[84,85,86,87,88]
Details of vectors and physical methods are beyond the scope of this paper.
Conclusion
Excessive body of documents indicates the role of genes in the pathogenesis of KC and further investigations are to complete this complex puzzle. As discussed above, despite a very comprehensive genetic analysis, no single gene was discovered as the disease causing gene. And to the time of finding the gene (s), despite progress in gene delivery and control of the microenvironment of the cornea, the application of gene therapy in the treatment of the KC remains in future prospect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: A review. Cont Lens Anterior Eye. 2010;33:157–66. doi: 10.1016/j.clae.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Hofstetter HW. A keratoscopic survey of 13,395 eyes. Am J Optom Arch Am Acad Optom. 1959;36:3–11. doi: 10.1097/00006324-195901000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101:267–73. doi: 10.1016/0002-9394(86)90817-2. [DOI] [PubMed] [Google Scholar]
- 5.Karimian F, Aramesh S, Rabei HM, Javadi MA, Rafati N. Topographic evaluation of relatives of patients with keratoconus. Cornea. 2008;27:874–8. doi: 10.1097/ICO.0b013e31816f5edc. [DOI] [PubMed] [Google Scholar]
- 6.Kaya V, Utine CA, Altunsoy M, Oral D, Yilmaz OF. Evaluation of corneal topography with Orbscan II in first-degree relatives of patients with keratoconus. Cornea. 2008;27:531–4. doi: 10.1097/ICO.0b013e318165d110. [DOI] [PubMed] [Google Scholar]
- 7.Wheeler J, Hauser MA, Afshari NA, Allingham RR, Liu Y. The Genetics of Keratoconus: A Review. Reprod Syst Sex Disord. 2012 doi: 10.4172/2161-038X.S6-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saee-Rad S, Hashemi H, Miraftab M, Noori-Daloii MR, Chaleshtori MH, Raoofian R, et al. Mutation analysis of VSX1 and SOD1 in Iranian patients with keratoconus. Mol Vis. 2011;17:3128–36. [PMC free article] [PubMed] [Google Scholar]
- 9.Bykhovskaya Y, Li X, Epifantseva I, Haritunians T, Siscovick D, Aldave A, et al. Variation in the lysyl oxidase (LOX) gene is associated with keratoconus in family-based and case-control studies. Invest Ophthalmol Vis Sci. 2012;53:4152–7. doi: 10.1167/iovs.11-9268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burdon KP, Vincent AL. Insights into keratoconus from a genetic perspective. Clin Exp Optom. 2013;96:146–54. doi: 10.1111/cxo.12024. [DOI] [PubMed] [Google Scholar]
- 11.Cristina Kenney M, Brown DJ. The cascade hypothesis of keratoconus. Cont Lens Anterior Eye. 2003;26:139–46. doi: 10.1016/S1367-0484(03)00022-5. [DOI] [PubMed] [Google Scholar]
- 12.Wilson SE, He YG, Weng J, Li Q, McDowall AW, Vital M, et al. Epithelial injury induces keratocyte apoptosis: Hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Exp Eye Res. 1996;62:325–7. doi: 10.1006/exer.1996.0038. [DOI] [PubMed] [Google Scholar]
- 13.Bureau J, Fabre EJ, Hecquet C, Pouliquen Y, Lorans G. Modification of prostaglandin E2 and collagen synthesis in keratoconus fibroblasts, associated with an increase of interleukin 1 alpha receptor number. C R Acad Sci III. 1993;316:425–30. [PubMed] [Google Scholar]
- 14.Lema I, Durán JA, Ruiz C, Díez-Feijoo E, Acera A, Merayo J. Inflammatory response to contact lenses in patients with keratoconus compared with myopic subjects. Cornea. 2008;27:758–63. doi: 10.1097/ICO.0b013e31816a3591. [DOI] [PubMed] [Google Scholar]
- 15.Sawaguchi S, Yue BY, Sugar J, Gilboy JE. Lysosomal enzyme abnormalities in keratoconus. Arch Ophthalmol. 1989;107:1507–10. doi: 10.1001/archopht.1989.01070020581044. [DOI] [PubMed] [Google Scholar]
- 16.Sawaguchi S, Twining SS, Yue BY, Chang SH, Zhou X, Loushin G, et al. Alpha 2-macroglobulin levels in normal human and keratoconus corneas. Invest Ophthalmol Vis Sci. 1994;35:4008–14. [PubMed] [Google Scholar]
- 17.Godel V, Blumenthal M, Iaina A. Congenital Leber amaurosis, keratoconus, and mental retardation in familial juvenile nephronophtisis. J Pediatr Ophthalmol Strabismus. 1978;15:89–91. doi: 10.3928/0191-3913-19780301-09. [DOI] [PubMed] [Google Scholar]
- 18.Smolin G, Thoft RA. 1st ed. Boston: Little Brown; 1983. The Cornea. Scientific Foundations and Clinical Practice; pp. 21–5. [Google Scholar]
- 19.Zimmermann DR, Fischer RW, Winterhalter KH, Witmer R, Vaughan L. Comparative studies of collagens in normal and keratoconus corneas. Exp Eye Res. 1988;46:431–42. doi: 10.1016/s0014-4835(88)80031-9. [DOI] [PubMed] [Google Scholar]
- 20.Gordon MO, Steger-May K, Szczotka-Flynn L, Riley C, Joslin CE, Weissman BA, et al. Baseline factors predictive of incident penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2006;142:923–30. doi: 10.1016/j.ajo.2006.07.026. [DOI] [PubMed] [Google Scholar]
- 21.Watson SL, Ramsay A, Dart JK, Bunce C, Craig E. Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology. 2004;111:1676–82. doi: 10.1016/j.ophtha.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 22.Sray WA, Cohen EJ, Rapuano CJ, Laibson PR. Factors associated with the need for penetrating keratoplasty in keratoconus. Cornea. 2002;21:784–6. doi: 10.1097/00003226-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Chang HY, Chodosh J. The genetics of keratoconus. Semin Ophthalmol. 2013;28:275–80. doi: 10.3109/08820538.2013.825295. [DOI] [PubMed] [Google Scholar]
- 24.Etzine S. Conical cornea in identical twins. S Afr Med J. 1954;28:154–5. [PubMed] [Google Scholar]
- 25.Gonzalez V, McDonnell PJ. Computer-assisted corneal topography in parents of patients with keratoconus. Arch Ophthalmol. 1992;110:1413–4. doi: 10.1001/archopht.1992.01080220074024. [DOI] [PubMed] [Google Scholar]
- 26.Hammerstein W. Genetics of conical cornea (author's transl) Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1974;190:293–308. doi: 10.1007/BF00407890. [DOI] [PubMed] [Google Scholar]
- 27.Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 28.Parker J, Ko WW, Pavlopoulos G, Wolfe PJ, Rabinowitz YS, Feldman ST. Videokeratography of keratoconus in monozygotic twins. J Refract Surg. 1996;12:180–3. doi: 10.3928/1081-597X-19960101-31. [DOI] [PubMed] [Google Scholar]
- 29.Falls HF, Allen AW. Dominantly inherited keratoconus. J Genet Hum. 1969;17:317–24. [PubMed] [Google Scholar]
- 30.Ihalainen A. Clinical and epidemiological features of keratoconus genetic and external factors in the pathogenesis of the disease. Acta Ophthalmol Suppl. 1986;178:1–64. [PubMed] [Google Scholar]
- 31.Redmond KB. The role of heredity in keratoconus. Trans Ophthalmol Soc Aust. 1968;27:52–4. [PubMed] [Google Scholar]
- 32.Cullen JF, Butler HG. Mongolism (down's syndrome) and keratoconus. Br J Ophthalmol. 1963;47:321–30. doi: 10.1136/bjo.47.6.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beckh U, Schönherr U, Naumann GO. Autosomal dominant keratoconus as the chief ocular symptom in Lobstein osteogenesis imperfecta tarda. Klin Monbl Augenheilkd. 1995;206:268–72. doi: 10.1055/s-2008-1035438. [DOI] [PubMed] [Google Scholar]
- 34.Elder MJ. Leber congenital amaurosis and its association with keratoconus and keratoglobus. J Pediatr Ophthalmol Strabismus. 1994;31:38–40. doi: 10.3928/0191-3913-19940101-08. [DOI] [PubMed] [Google Scholar]
- 35.Wachtmeister L, Ingemansson SO, Möller E. Atopy and HLA antigens in patients with keratoconus. Acta Ophthalmol (Copenh) 1982;60:113–22. doi: 10.1111/j.1755-3768.1982.tb05787.x. [DOI] [PubMed] [Google Scholar]
- 36.Brancati F, Valente EM, Sarkozy A, Fehèr J, Castori M, Del Duca P, et al. A locus for autosomal dominant keratoconus maps to human chromosome 3p14-q13. J Med Genet. 2004;41:188–92. doi: 10.1136/jmg.2003.012872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gajecka M, Radhakrishna U, Winters D, Nath SK, Rydzanicz M, Ratnamala U, et al. Localization of a gene for keratoconus to a 5.6-Mb interval on 13q32. Invest Ophthalmol Vis Sci. 2009;50:1531–9. doi: 10.1167/iovs.08-2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hutchings H, Ginisty H, Le Gallo M, Levy D, Stoësser F, Rouland JF, et al. Identification of a new locus for isolated familial keratoconus at 2p24. J Med Genet. 2005;42:88–94. doi: 10.1136/jmg.2004.022103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nowak DM, Gajecka M. The genetics of keratoconus. Middle East Afr J Ophthalmol. 2011;18:2–6. doi: 10.4103/0974-9233.75876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tang YG, Rabinowitz YS, Taylor KD, Li X, Hu M, Picornell Y, et al. Genomewide linkage scan in a multigeneration Caucasian pedigree identifies a novel locus for keratoconus on chromosome 5q14.3-q21.1. Genet Med. 2005;7:397–405. doi: 10.1097/01.gim.0000170772.41860.54. [DOI] [PubMed] [Google Scholar]
- 41.Tyynismaa H, Sistonen P, Tuupanen S, Tervo T, Dammert A, Latvala T, et al. A locus for autosomal dominant keratoconus: Linkage to 16q22.3-q23.1 in Finnish families. Invest Ophthalmol Vis Sci. 2002;43:3160–4. [PubMed] [Google Scholar]
- 42.Burdon KP, Coster DJ, Charlesworth JC, Mills RA, Laurie KJ, Giunta C, et al. Apparent autosomal dominant keratoconus in a large Australian pedigree accounted for by digenic inheritance of two novel loci. Hum Genet. 2008;124:379–86. doi: 10.1007/s00439-008-0555-z. [DOI] [PubMed] [Google Scholar]
- 43.Karolak JA, Kulinska K, Nowak DM, Pitarque JA, Molinari A, Rydzanicz M, et al. Sequence variants in COL4A1 and COL4A2 genes in Ecuadorian families with keratoconus. Mol Vis. 2011;17:827–43. [PMC free article] [PubMed] [Google Scholar]
- 44.Hughes AE, Dash DP, Jackson AJ, Frazer DG, Silvestri G. Familial keratoconus with cataract: Linkage to the long arm of chromosome 15 and exclusion of candidate genes. Invest Ophthalmol Vis Sci. 2003;44:5063–6. doi: 10.1167/iovs.03-0399. [DOI] [PubMed] [Google Scholar]
- 45.Semina EV, Mintz-Hittner HA, Murray JC. Isolation and characterization of a novel human paired-like homeodomain-containing transcription factor gene, VSX1, expressed in ocular tissues. Genomics. 2000;63:289–93. doi: 10.1006/geno.1999.6093. [DOI] [PubMed] [Google Scholar]
- 46.Héon E, Greenberg A, Kopp KK, Rootman D, Vincent AL, Billingsley G, et al. VSX1: A gene for posterior polymorphous dystrophy and keratoconus. Hum Mol Genet. 2002;11:1029–36. doi: 10.1093/hmg/11.9.1029. [DOI] [PubMed] [Google Scholar]
- 47.Eran P, Almogit A, David Z, Wolf HR, Hana G, Yaniv B, et al. The D144E substitution in the VSX1 gene: A non-pathogenic variant or a disease causing mutation? Ophthalmic Genet. 2008;29:53–9. doi: 10.1080/13816810802008242. [DOI] [PubMed] [Google Scholar]
- 48.Mintz-Hittner HA, Semina EV, Frishman LJ, Prager TC, Murray JC. VSX1 (RINX) mutation with craniofacial anomalies, empty sella, corneal endothelial changes, and abnormal retinal and auditory bipolar cells. Ophthalmology. 2004;111:828–36. doi: 10.1016/j.ophtha.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 49.Mok JW, Baek SJ, Joo CK. VSX1 gene variants are associated with keratoconus in unrelated Korean patients. J Hum Genet. 2008;53:842–9. doi: 10.1007/s10038-008-0319-6. [DOI] [PubMed] [Google Scholar]
- 50.Bisceglia L, Ciaschetti M, De Bonis P, Campo PA, Pizzicoli C, Scala C, et al. VSX1 mutational analysis in a series of Italian patients affected by keratoconus: Detection of a novel mutation. Invest Ophthalmol Vis Sci. 2005;46:39–45. doi: 10.1167/iovs.04-0533. [DOI] [PubMed] [Google Scholar]
- 51.Abu-Amero KK, Kalantan H, Al-Muammar AM. Analysis of the VSX1 gene in keratoconus patients from Saudi Arabia. Mol Vis. 2011;17:667–72. [PMC free article] [PubMed] [Google Scholar]
- 52.Grünauer-Kloevekorn C, Duncker GI. Keratoconus: Epidemiology, risk factors and diagnosis. Klin Monbl Augenheilkd. 2006;223:493–502. doi: 10.1055/s-2005-859021. [DOI] [PubMed] [Google Scholar]
- 53.Tanwar M, Kumar M, Nayak B, Pathak D, Sharma N, Titiyal JS, et al. VSX1 gene analysis in keratoconus. Mol Vis. 2010;16:2395–401. [PMC free article] [PubMed] [Google Scholar]
- 54.Valleix S, Nedelec B, Rigaudiere F, Dighiero P, Pouliquen Y, Renard G, et al. H244R VSX1 is associated with selective cone ON bipolar cell dysfunction and macular degeneration in a PPCD family. Invest Ophthalmol Vis Sci. 2006;47:48–54. doi: 10.1167/iovs.05-0479. [DOI] [PubMed] [Google Scholar]
- 55.Aldave AJ, Yellore VS, Salem AK, Yoo GL, Rayner SA, Yang H, et al. No VSX1 gene mutations associated with keratoconus. Invest Ophthalmol Vis Sci. 2006;47:2820–2. doi: 10.1167/iovs.05-1530. [DOI] [PubMed] [Google Scholar]
- 56.Tang YG, Picornell Y, Su X, Li X, Yang H, Rabinowitz YS. Three VSX1 gene mutations, L159M, R166W, and H244R, are not associated with keratoconus. Cornea. 2008;27:189–92. doi: 10.1097/ICO.0b013e31815a50e7. [DOI] [PubMed] [Google Scholar]
- 57.Stabuc-Silih M, Strazisar M, Hawlina M, Glavac D. Absence of pathogenic mutations in VSX1 and SOD1 genes in patients with keratoconus. Cornea. 2010;29:172–6. doi: 10.1097/ICO.0b013e3181aebf7a. [DOI] [PubMed] [Google Scholar]
- 58.Udar N, Atilano SR, Brown DJ, Holguin B, Small K, Nesburn AB, et al. SOD1: A candidate gene for keratoconus. Invest Ophthalmol Vis Sci. 2006;47:3345–51. doi: 10.1167/iovs.05-1500. [DOI] [PubMed] [Google Scholar]
- 59.Mashhour B, Couton D, Perricaudet M, Briand P. In vivo adenovirus-mediated gene transfer into ocular tissues. Gene Ther. 1994;1:122–6. [PubMed] [Google Scholar]
- 60.Sakamoto T, Oshima Y, Nakagawa K, Ishibashi T, Inomata H, Sueishi K. Target gene transfer of tissue plasminogen activator to cornea by electric pulse inhibits intracameral fibrin formation and corneal cloudiness. Hum Gene Ther. 1999;10:2551–7. doi: 10.1089/10430349950016889. [DOI] [PubMed] [Google Scholar]
- 61.Klebe S, Sykes PJ, Coster DJ, Krishnan R, Williams KA. Prolongation of sheep corneal allograft survival by ex vivo transfer of the gene encoding interleukin-10. Transplantation. 2001;71:1214–20. doi: 10.1097/00007890-200105150-00006. [DOI] [PubMed] [Google Scholar]
- 62.Lai CM, Brankov M, Zaknich T, Lai YK, Shen WY, Constable IJ, et al. Inhibition of angiogenesis by adenovirus-mediated sFlt-1 expression in a rat model of corneal neovascularization. Hum Gene Ther. 2001;12:1299–310. doi: 10.1089/104303401750270959. [DOI] [PubMed] [Google Scholar]
- 63.Lai YK, Shen WY, Brankov M, Lai CM, Constable IJ, Rakoczy PE. Potential long-term inhibition of ocular neovascularisation by recombinant adeno-associated virus-mediated secretion gene therapy. Gene Ther. 2002;9:804–13. doi: 10.1038/sj.gt.3301695. [DOI] [PubMed] [Google Scholar]
- 64.Pleyer U, Bertelmann E, Rieck P, Hartmann C, Volk HD, Ritter T. Survival of corneal allografts following adenovirus-mediated gene transfer of interleukin-4. Graefes Arch Clin Exp Ophthalmol. 2000;238:531–6. doi: 10.1007/pl00007896. [DOI] [PubMed] [Google Scholar]
- 65.Gong N, Pleyer U, Yang J, Vogt K, Hill M, Anegon I, et al. Influence of local and systemic CTLA4Ig gene transfer on corneal allograft survival. J Gene Med. 2006;8:459–67. doi: 10.1002/jgm.876. [DOI] [PubMed] [Google Scholar]
- 66.Koelle DM, Ghiasi H. Prospects for developing an effective vaccine against ocular herpes simplex virus infection. Curr Eye Res. 2005;30:929–42. doi: 10.1080/02713680500313153. [DOI] [PubMed] [Google Scholar]
- 67.Jun AS, Larkin DF. Prospects for gene therapy in corneal disease. Eye (Lond) 2003;17:906–11. doi: 10.1038/sj.eye.6700565. [DOI] [PubMed] [Google Scholar]
- 68.Yeh P, Colby C. Corneal endothelial dystrophies. In: Foster C, Azar DT, Dohlman CH, editors. Cornea: Scientific Foundations and Clinical Practice. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 849–73. [Google Scholar]
- 69.Nishida T. Cornea. In: Krachmer J, Mannis MJ, Holland EJ, editors. Cornea. Vol. 1. Philadelphia: Elsevier Mosby; 2005. pp. 3–26. [Google Scholar]
- 70.Bouchard C. The ocular immune response. In: Krachmer J, Mannis MJ, Holland EJ, editors. Cornea. Vol. 1. Philadelphia: Elsevier Mosby; 2005. pp. 59–93. [Google Scholar]
- 71.Foster C, Streilein JW. Basic immunology. In: Foster C, Azar DT, Dohlman CH, editors. The Cornea: Scientific Foundations and Clinical Practice. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 59–102. [Google Scholar]
- 72.Larkin DF, Oral HB, Ring CJ, Lemoine NR, George AJ. Adenovirus-mediated gene delivery to the corneal endothelium. Transplantation. 1996;61:363–70. doi: 10.1097/00007890-199602150-00005. [DOI] [PubMed] [Google Scholar]
- 73.Zhou R, Dean DA. Gene transfer of interleukin 10 to the murine cornea using electroporation. Exp Biol Med (Maywood) 2007;232:362–9. [PMC free article] [PubMed] [Google Scholar]
- 74.Toropainen E, Hornof M, Kaarniranta K, Johansson P, Urtti A. Corneal epithelium as a platform for secretion of transgene products after transfection with liposomal gene eyedrops. J Gene Med. 2007;9:208–16. doi: 10.1002/jgm.1011. [DOI] [PubMed] [Google Scholar]
- 75.Stechschulte SU, Joussen AM, von Recum HA, Poulaki V, Moromizato Y, Yuan J, et al. Rapid ocular angiogenic control via naked DNA delivery to cornea. Invest Ophthalmol Vis Sci. 2001;42:1975–9. [PubMed] [Google Scholar]
- 76.Lundstrom K. Gene therapy applications of viral vectors. Technol Cancer Res Treat. 2004;3:467–77. doi: 10.1177/153303460400300508. [DOI] [PubMed] [Google Scholar]
- 77.Lundstrom K, Boulikas T. Viral and non-viral vectors in gene therapy: Technology development and clinical trials. Technol Cancer Res Treat. 2003;2:471–86. doi: 10.1177/153303460300200513. [DOI] [PubMed] [Google Scholar]
- 78.Young LS, Searle PF, Onion D, Mautner V. Viral gene therapy strategies: From basic science to clinical application. J Pathol. 2006;208:299–318. doi: 10.1002/path.1896. [DOI] [PubMed] [Google Scholar]
- 79.Latchman DS. Herpes simplex virus-based vectors for the treatment of cancer and neurodegenerative disease. Curr Opin Mol Ther. 2005;7:415–8. [PubMed] [Google Scholar]
- 80.Argnani R, Lufino M, Manservigi M, Manservigi R. Replication-competent herpes simplex vectors: Design and applications. Gene Ther. 2005;12(Suppl 1):S170–7. doi: 10.1038/sj.gt.3302622. [DOI] [PubMed] [Google Scholar]
- 81.Nishikawa M, Takakura Y, Hashida M. Pharmacokinetics of Plasmid DNA-Based Non-viral Gene Medicine. Adv Genet. 2005;53PA:47–68. doi: 10.1016/S0065-2660(05)53003-7. [DOI] [PubMed] [Google Scholar]
- 82.Zhang EP, Franke J, Schroff M, Junghans C, Wittig B, Hoffmann F. Ballistic CTLA4 and IL-4 gene transfer into the lower lid prolongs orthotopic corneal graft survival in mice. Graefes Arch Clin Exp Ophthalmol. 2003;241:921–6. doi: 10.1007/s00417-003-0763-0. [DOI] [PubMed] [Google Scholar]
- 83.Müller A, Zhang EP, Schroff M, Wittig B, Hoffmann F. Influence of ballistic gene transfer on antigen-presenting cells in murine corneas. Graefes Arch Clin Exp Ophthalmol. 2002;240:851–9. doi: 10.1007/s00417-002-0536-1. [DOI] [PubMed] [Google Scholar]
- 84.Wells DJ. Gene therapy progress and prospects: Electroporation and other physical methods. Gene Ther. 2004;11:1363–9. doi: 10.1038/sj.gt.3302337. [DOI] [PubMed] [Google Scholar]
- 85.Mehier-Humbert S, Guy RH. Physical methods for gene transfer: Improving the kinetics of gene delivery into cells. Adv Drug Deliv Rev. 2005;57:733–53. doi: 10.1016/j.addr.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 86.Tanelian DL, Barry MA, Johnston SA, Le T, Smith G. Controlled gene gun delivery and expression of DNA within the cornea. Biotechniques. 1997;23:484–8. doi: 10.2144/97233st06. [DOI] [PubMed] [Google Scholar]
- 87.Sonoda S, Tachibana K, Uchino E, Okubo A, Yamamoto M, Sakoda K, et al. Gene transfer to corneal epithelium and keratocytes mediated by ultrasound with microbubbles. Invest Ophthalmol Vis Sci. 2006;47:558–64. doi: 10.1167/iovs.05-0889. [DOI] [PubMed] [Google Scholar]
- 88.Gardlík R, Pálffy R, Hodosy J, Lukács J, Turna J, Celec P. Vectors and delivery systems in gene therapy. Med Sci Monit. 2005;11:RA110–21. [PubMed] [Google Scholar]


