Abstract
Signs of hypertensive retinopathy are common and are correlated with elevated blood pressure. Patients who have swelling of both optic discs and very high blood pressure (i.e., malignant retinopathy) need urgent antihypertensive treatment. A patient was reported with malignant hypertensive retinopathy who recovered promptly following single intravitreal bevacizumab injection. Intravitreal bevacizumab (1.25 mg/0.05 mL) was injected in two eyes of a patient having malignant hypertensive retinopathy with optic disc edema, macular edema, and retinal exudates. A complete ophthalmic examination, including the best-corrected visual acuity (BCVA), central macular thickness on optical coherence tomography (OCT), and fluorescein angiography (FAG), was performed before and after the treatments. Two eyes in a patient received a single intravitreal injection of bevacizumab had improvement of macular edema on OCT at 1 month and decreased fluorescein leakage on FAG 3 months after the treatment, which led to improvements in the BCVA both eyes. The results suggest that intravitreal bevacizumab injections might be a useful and safe adjunctive treatment of malignant hypertensive retinopathy, in addition to proper medical management of malignant hypertension.
Keywords: Bevacizumab (avastin), hypertensive retinopathy, optic disc edema
Introduction
Hypertensive retinopathy was first described by Gunn in the 19th century in a series of patients with hypertension and renal disease.[1] Hypertensive retinopathy is characterized by the presence of retinal vascular signs in patients with elevated blood pressure. It is well known that the retinal circulation shares anatomical, physiological, and embryologic features with the cerebral circulation. An autopsy study of patients with stroke showed a close similarity between retinal and cerebral arteriolar findings which indicates an evidence of the association between the risk of stroke and hypertensive retinopathy.[2] There are infrequent data regarding the association of hypertensive retinopathy and the risk of coronary heart disease.[3] According to the Joint National Committee (JNC) criteria, the presence of retinopathy may be an indication for starting antihypertensive treatment, even in patients with stage 1 hypertension (blood pressure, 140-159/90-99 mm Hg) who have no other proof of target-organ damage.[4] The evidence in support of the JNC guidelines on retinal findings in hypertension is based on earlier studies that may not have a direct connection to current clinical practice.[1,5,6,7]
Bevacizumab (avastin), an antibody against vascular endothelial growth factor (VEGF) (anti-VEGF), has been injected intravitreally in various retinal diseases that have increased vascular permeability and edema.[8] Researchers using preclinical models have shown that anti-VEGF agents such as bevacizumab may work by causing several changes in blood vessels. Next to interfering with vessel growth and neovascularization, they help a regression of existing microvessels and stimulate “normalization” of surviving mature vasculature, stabilize the vessel, and prevent leakage.[9]
This study reports a patient with malignant hypertensive retinopathy who presented with visual impairment and severe exudative retinal changes, but recovered quickly following a single intravitreal bevacizumab injection.
Case Report
A 32-year-old woman was referred because of blurred vision in both eyes for 1 week. She had been taking medication to treat hypertension for 2 years with poor control of blood pressure. Her best-corrected visual acuity was counting fingers 5 feet both eyes. The anterior segment examination of both eyes was unremarkable. Fundoscopic examination showed bilateral optic disc swelling, peripapillary retinal edema involving the macula and peripapillary flame-shaped hemorrhages with multiple hard exudates more with the right eye [Figure 1a]. Fluorescein angiography (FAG) showed extensive fluorescein leakage from the optic disc and diffuse capillary leakage along the vascular arcades in both eyes [Figure 2a]. Optical coherence tomography (OCT) revealed bilateral marked macular edema and neurosensory detachment [Figure 3a]. Her blood pressure was 160/100 mm Hg. Cardiology, nephrology, and neurology consultations were obtained and showed renal impairment. This patient was treated with single intravitreal injections of bevacizumab (1.25 mg/0.05 mL) in both eyes. One month after the treatment, visual acuity was 20/400 and 20/100 in her right and left eyes, respectively, and the bilateral optic disc edema and macular edema had resolved [Figures 1b and 3b]. Three months after the treatment, much of the hard exudates surrounding the fovea bilaterally were absorbed on fundus examination [Figure 1c]. FAG showed minimal leakage from the optic discs bilaterally with macular area of nonperfusion of the right eye which might explain decreased right eye vision [Figure 2b]. Although she showed resolution of the bilateral macular edema, atrophic thinning of the fovea in both eyes was detected on OCT [Figure 3c].
Figure 1.
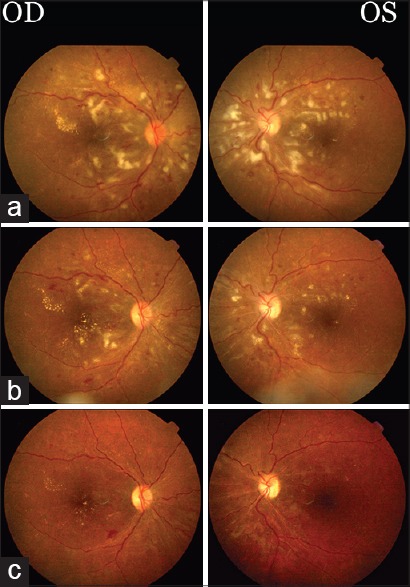
Fundus findings before and after intravitreal bevacizumab injection. At presentation, optic discs welling, macular edema, and peripapillary flame-shaped hemorrhages and hard exudates were present in both eyes (a). One month after intravitreal bevacizumab injection, the bilateral optic disc swelling and hard exudates were decreased (b). Three months (c). after the treatment, the optic disc swelling, macular edema and hard exudates decreased both eyes
Figure 2.
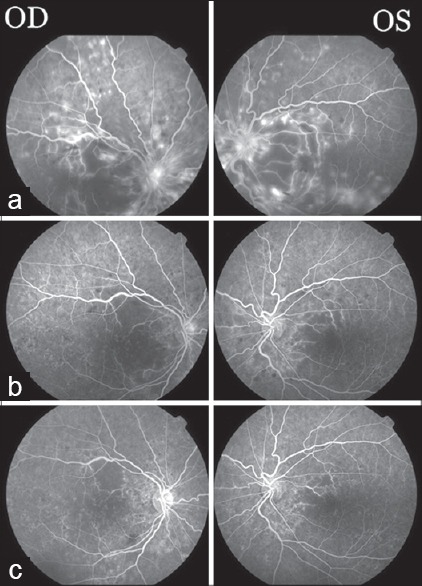
Fluorescein angiography findings before and after intravitreal bevacizumab injection. At presentation, profuse fluorescein leakage from the optic disc and diffuse leakage from the capillaries along the vascular arcades were present in both eyes (a). One month after intravitreal bevacizumab injection, decreased leakage from the optic discs and the retinal vessels (b). Three months after the treatment, minimal fluorescein leakage occurred from the optic disc both eyes with macular area of nonperfusion of the right eye (c)
Figure 3.
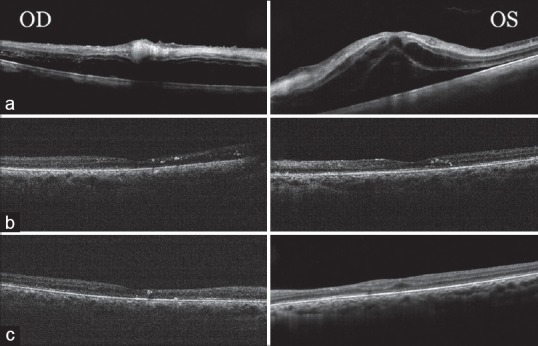
Optical coherence tomography findings before and after intravitreal bevacizumab injection. At presentation, macular edema and subfoveal neurosensory detachments were noted both eyes. The central macular thickness (CMT) was 392 mm in the right eye and 874 mm in the left eye (a). One month after the treatment, CMT decreased to 193 mm in the right eye and 194 mm in the left eye (b). The CMT reduced to 144 mm in right eye and 193 mm in left eye with atrophic thinning of the fovea 3 months after the (c)
Discussion
The retinal circulation suffers a series of pathophysiological changes in reply to elevated blood pressure.[10] The retinal signs are generalized and focal arteriolar narrowing, arteriovenous nicking, flame-shaped and blot-shaped retinal hemorrhages, cotton-wool spots, and swelling of the optic disc some experimental studies[11,12] and clinical trials[13,14] have demonstrated that clinical findings of hypertensive retinopathy regress with the control of blood pressure, although spontaneous resolution of these findings in the presence of high blood pressure has also been reported.[15] It is unclear whether antihypertensive medications that are expected to have direct useful result on the microvascular structure (e.g., angiotensin-converting enzyme inhibitors) would decrease the injury of retinopathy beyond the reduction effected by lowered blood pressure. According to Chen et al.,[16] 11 of 14 patients with malignant hypertensive retinopathy had an acceptable visual prognosis when the blood pressure was controlled, whereas three patients, who had longer durations of high blood pressure and other retinal comorbidities, such as central artery occlusion and anterior ischemic optic neuropathy still, had bad vision. Salman[17] did not find a significant relation between severity of hypertension and degree of drop in initial visual acuity or extent of retinopathy. However, Browning et al.[18] who found that the worst visual prognosis was associated with the highest presented blood pressure, the worst visual acuity at presentation, and the longest duration of symptoms. The use of intravitreal anti-VEGF therapy has expanded tremendously in recent years, and intravitreal anti-VEGF agents are now used to handle complications of various diseases of the posterior segment.[7] In an exudative stage of hypertensive retinopathy, in which there is a disruption of the blood retinal barrier, necrosis of the smooth muscles and endothelial cells, exudation of blood and lipids, and retinal ischemia. These changes are manifested in the retina as microaneurysms, hemorrhages, hard exudates, and cotton-wool spots. Swelling of the optic disc may occur at this time and usually indicates severely elevated blood pressure (i.e., malignant hypertension).[19,20]
The intravitreal injection of anti-VEGF agents can accelerate the resolution of macular edema with exudative retinal detachment and improve the visual outcome.
In the current case, intravitreal bevacizumab injection in a patient with exudative stage of malignant hypertensive retinopathy resulted in rapid resolution of the macular edema and optic disc edema. Kim et al.[21] reported same results in two cases. This result and previous results suggest that intravitreal bevacizumab injection might be recommended as effective therapeutic modality for treating exudative stage of hypertensive retinopathy, in addition to lowering blood pressure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gunn RM. Ophthalmoscopic evidence of (1) arterial changes associated with chronic renal diseases and (2) of increased arterial tension. Trans Ophthalmol Soc UK. 1892;12:124–5. [Google Scholar]
- 2.Goto I, Katsuki S, Ikui H, Kimoto K, Mimatsu T. Pathological studies on the intracerebral and retinal arteries in cerebrovascular and noncerebrovascular diseases. Stroke. 1975;6:263–9. doi: 10.1161/01.str.6.3.263. [DOI] [PubMed] [Google Scholar]
- 3.Walsh JB. Hypertensive retinopathy. Description, classification, and prognosis. Ophthalmology. 1982;89:1127–31. [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 5.Breslin DJ, Gifford RW, Jr, Fairbairn JF, 2nd, Kearns TP. Prognostic importance of ophthalmoscopic findings in essential hypertension. JAMA. 1966;195:335–8. [PubMed] [Google Scholar]
- 6.Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: Their course and prognosis. Am J Med Sci. 1939;197:332–43. doi: 10.1097/00000441-197412000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Nicholson BP, Schachat AP. A review of clinical trials of anti-VEGF agents for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2010;248:915–30. doi: 10.1007/s00417-010-1315-z. [DOI] [PubMed] [Google Scholar]
- 8.Gulati N, Forooghian F, Lieberman R, Jabs DA. Vascular endothelial growth factor inhibition in uveitis: A systematic review. Br J Ophthalmol. 2011;95:162–5. doi: 10.1136/bjo.2009.177279. [DOI] [PubMed] [Google Scholar]
- 9.Ferrara N, Houck KA, Jakeman LB, Winer J, Leung DW. The vascular endothelial growth factor family of polypeptides. J Cell Biochem. 1991;47:211–8. doi: 10.1002/jcb.240470305. [DOI] [PubMed] [Google Scholar]
- 10.Tso MO, Jampol LM. Pathophysiology of hypertensive retinopathy. Ophthalmology. 1982;89:1132–45. doi: 10.1016/s0161-6420(82)34663-1. [DOI] [PubMed] [Google Scholar]
- 11.Hamada Y, Niisato E, Otori T, Chikugo TA, Ohta Y, Suzuki T, et al. Ocular fundus changes in malignant or precocious stroke-prone spontaneously hypertensive rats after administration of antihypertensive drugs. Clin Exp Pharmacol Physiol Suppl. 1995;22:S132–3. doi: 10.1111/j.1440-1681.1995.tb02851.x. [DOI] [PubMed] [Google Scholar]
- 12.Morishita R, Higaki J, Nakamura F, Tomita N, Yu H, Nagano M, et al. Regression of hypertension-induced vascular hypertrophy by an ACE inhibitor and calcium antagonist in the spontaneously hypertensive rat. Blood Press Suppl. 1992;3:41–7. [PubMed] [Google Scholar]
- 13.Bock KD. Regression of retinal vascular changes by antihypertensive therapy. Hypertension. 1984;6:III158–62. doi: 10.1161/01.hyp.6.6_pt_2.iii158. [DOI] [PubMed] [Google Scholar]
- 14.Dahlöf B, Stenkula S, Hansson L. Hypertensive retinal vascular changes: Relationship to left ventricular hypertrophy and arteriolar changes before and after treatment. Blood Press. 1992;1:35–44. doi: 10.3109/08037059209065122. [DOI] [PubMed] [Google Scholar]
- 15.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 16.Chen YH, Kuo HK, Kao ML. Malignant hypertensive retinopathy-clinical and fundus manifestations in patients with new onset or acute exacerbation of chronic hypertension. Chang Gung Med J. 2003;26:669–77. [PubMed] [Google Scholar]
- 17.Salman AG. Intravitreal bevacizumab in persistent retinopathy secondary to malignant hypertension. Saudi J Ophthalmol. 2013;27:25–9. doi: 10.1016/j.sjopt.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Browning AC, Mengher LS, Gregson RM, Amoaku WM. Visual outcome of malignant hypertension in young people. Arch Dis Child. 2001;85:401–3. doi: 10.1136/adc.85.5.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004;351:2310–7. doi: 10.1056/NEJMra032865. [DOI] [PubMed] [Google Scholar]
- 20.DellaCroce JT, Vitale AT. Hypertension and the eye. Curr Opin Ophthalmol. 2008;19:493–8. doi: 10.1097/ICU.0b013e3283129779. [DOI] [PubMed] [Google Scholar]
- 21.Kim EY, Lew HM, Song JH. Effect of intravitreal bevacizumab (Avastin(®)) therapy in malignant hypertensive retinopathy: A report of two cases. J Ocul Pharmacol Ther. 2012;28:318–22. doi: 10.1089/jop.2011.0113. [DOI] [PubMed] [Google Scholar]


