Abstract
Objective
Evaluate the utility of a computer-based, interactive, and individualized intervention for promoting well-being in US surgeons.
Background
Distress and burnout are common among US surgeons. Surgeons experiencing distress are unlikely to seek help on their own initiative. A belief that distress and burnout are a normal part of being a physician and lack of awareness of distress level relative to colleagues may contribute to this problem.
Methods
Surgeons who were members of the American College of Surgeons were invited to participate in an intervention study. Participating surgeons completed a 3-step, interactive, electronic intervention. First, surgeons subjectively assessed their well-being relative to colleagues. Second, surgeons completed the 7-item Mayo Clinic Physician Well-Being Index and received objective, individualized feedback about their well-being relative to national physician norms. Third, surgeons evaluated the usefulness of the feedback and whether they intended to make specific changes as a result.
Results
A total of 1150 US surgeons volunteered to participate in the study. Surgeons’ subjective assessment of their well-being relative to colleagues was poor. A majority of surgeons (89.2%) believed that their well-being was at or above average, including 70.5% with scores in the bottom 30% relative to national norms. After receiving objective, individualized feedback based on the Mayo Clinic Physician Well-Being Index score, 46.6% of surgeons indicated that they intended to make specific changes as a result. Surgeons with lower well-being scores were more likely to make changes in each dimension assessed (all Ps < 0.001).
Conclusions
US surgeons do not reliably calibrate their level of distress. After self-assessment and individualized feedback using the Mayo Clinic Physician Well-Being Index, half of participating surgeons reported that they were contemplating behavioral changes to improve personal well-being.
Keywords: behavioral change, burnout, intervention, Physician Well-Being Index, physician
Studies during the last decade have demonstrated high rates of distress and burnout among US physicians.1–4 Physician distress may manifest itself in a variety of ways, including stress, depression, fatigue, and low career satisfaction.5,6 Burnout appears to be one of the most common manifestations of distress, with recent studies indicating that 30% to 45% of US physicians are experiencing burnout.2–5,7,8 Burnout is a syndrome of emotional exhaustion and depersonalization that leads to decreased effectiveness at work.9 In addition to potential personal consequences, physician distress can affect physicians’ satisfaction with their work and the quality of medical care they provide.10–15
A series of studies conducted by the American College of Surgeons (ACS) since 2008 have provided insight into the experience and repercussions of distress among US surgeons.2,15–24 This effort has characterized the prevalence of burnout and distress among US surgeons2 and explored correlations with work hours,16 area of subspecialization,21,25 malpractice suits,26 and practice setting.2,25 These studies have also identified potential personal consequences of distress among surgeons, including problematic alcohol use,23 strained personal relationships,17,20 and suicidal ideation.27 From a professional standpoint, surgeon distress seems both to contribute to medical errors15 and to cause surgeons to consider reducing their clinical workload and/or to pursue early retirement.3,28
Other than descriptive information on the habits and self-care strategies of thriving surgeons,24 there is limited information on what steps surgeons can take to reduce distress. Like other physicians,29 surgeons experiencing distress are unlikely to seek help of their own initiative.27 A variety of factors likely contribute to this fact, including concerns about repercussions for licensure, the belief that distress and burnout are normal parts of being a physician, and a professional culture that minimizes distress until it reaches dangerous levels.27,29,30
Several barriers have also prevented proactive screening for physician distress, including the lack of a brief screening instrument that evaluates the relevant dimensions of distress, the complex scoring systems required for the available tools, a lack of physician-specific normative data, and no information regarding what level of distress results in clinically relevant outcomes. Through a 5-year iterative process, we developed and validated a brief 7-item self-assessment tool [Mayo Clinic Physician Well-Being Index (MPWBI) Table 1] to evaluate the dimensions of distress commonly experienced by physicians.31–33 A recent validation study among approximately 7000 US physicians confirmed the utility of the MPWBI and indicated that the index was able to stratify an individual physician’s risk of experiencing adverse personal and professional consequences (eg, makeing medical error, intent to leave practice, suicidal ideation).31
TABLE 1.
Mayo Clinic Physician Well-Being Index*
| During the past month… |
| have you felt burned out from your work? |
| have you worried that your work is hardening you emotionally? |
| have you often been bothered by feeling down, depressed, or hopeless? |
| have you fallen asleep while stopped in traffic or driving? |
| have you felt that all the things you had to do were piling up so high that you could not overcome them? |
| have you been bothered by emotional problems (such as feeling anxious, depressed, or irritable)? |
| has your physical health interfered with your ability to do your daily work at home and/or away from home? |
Each question is answered using a yes/no scale. Basic scoring systems and weighted scoring approaches that may improve sensitivity and specificity for predicting specific outcomes (eg, mental quality of life; suicidal ideation) are reviewed in reference 31.
Although the best strategy to help individuals improve their well-being is unknown, computer-based, interactive, and individualized interventions have been shown to be an effective approach to promote behavioral change.34,35 In this study, conducted as part of the ongoing ACS effort to promote surgeon well-being, we tested the utility of an interactive and individualized intervention based on the MPWBI in approximately 1100 US surgeons. After answering baseline questions regarding how they believed their well-being compared with their colleagues, participating surgeons completed an online version of the MPWBI after which they received immediate, individualized feedback. Surgeons were then asked a series of follow-up questions regarding the utility of the feedback and whether they planned to make specific changes based on the information provided.
METHODS
Participants
Study eligibility and the electronic participation process were similar to our 2008 and 2010 ACS studies.2,15–24 A random sample of 8000 surgeons who were members of the ACS, had an e-mail address on file with the ACS, and permitted their e-mail to be used for correspondence with the ACS were notified of the study. Participation was voluntary, and all responses were anonymous. The ACS Governor’s Committee on Physician Competency and Health commissioned the study, and institutional review board oversight for protection of human subjects was provided by the Mayo Clinic institutional review board. Surgeons received 2 e-mails notifying them of the study and inviting them to participate. Surgeons who volunteered to participate completed the study electronically in March to April 2013.
Physician Well-Being Index
The 7-itemMPWBI evaluates the dimensions of distress commonly experienced by physicians [eg, burnout (emotional exhaustion, depersonalization), depression, fatigue, mental quality of life, physical quality of life]. The robust, iterative process to develop and validate the MPWBI is described in previous publications.31–33 After initial development and validation in medical students,32,33 the MPWBI was subsequently adapted and tested in a national sample of approximately 7000 US physicians.31 That study confirmed the utility of the MPWBI for assessing multiple dimensions of physician distress, defined the normative scores for US physicians,31 and indicated that the index is associated with clinically relevant personal and professional endpoints (eg, medical errors,15 intent to leave practice,22 suicidal ideation36). For the present study, a Web-based version of the MPWBI was created along with automated scoring reports that provided immediate, individualized feedback based on the MPWBI score. This feedback informed physicians how their level of distress compared with national physician norms31 and also provided dashboards that gave participating surgeons specific data on how their degree of distress may impact them personally and professionally in 6 dimensions. The feedback to all participants also included the phone number for the National Suicide Prevention hotline.
Intervention and Data Collection
It should be emphasized that this study was not a survey but a multistep electronic intervention. The cover letter stated that the purpose of the study was to evaluate the utility of a validated online self-assessment tool that would provide individualized feedback on the individual’s well-being relative to that of other physicians/surgeons. Although the entire process was designed to take 5 minutes or less, the intervention had 3 phases. First, surgeons provided baseline information regarding demographic characteristics (age, sex, practice setting, years in practice) and their assessment of personal well-being relative to other physicians. Response options for this latter question included: “poor” (bottom 30% of physicians), “below average” (31st–40th percentile), “average” (41st–60th percentile), “above average” (61st–70th percentile), and “excellent” (top 30% of physicians). These options were designed to represent an intuitive distribution and allow assessment of the accuracy of self-calibration relative to actual objective benchmarking using the MPWBI (scores of 0 represent the top 27.4% of physicians nationally; scores ≥4 represent the bottom 29.3% of physicians nationally).31
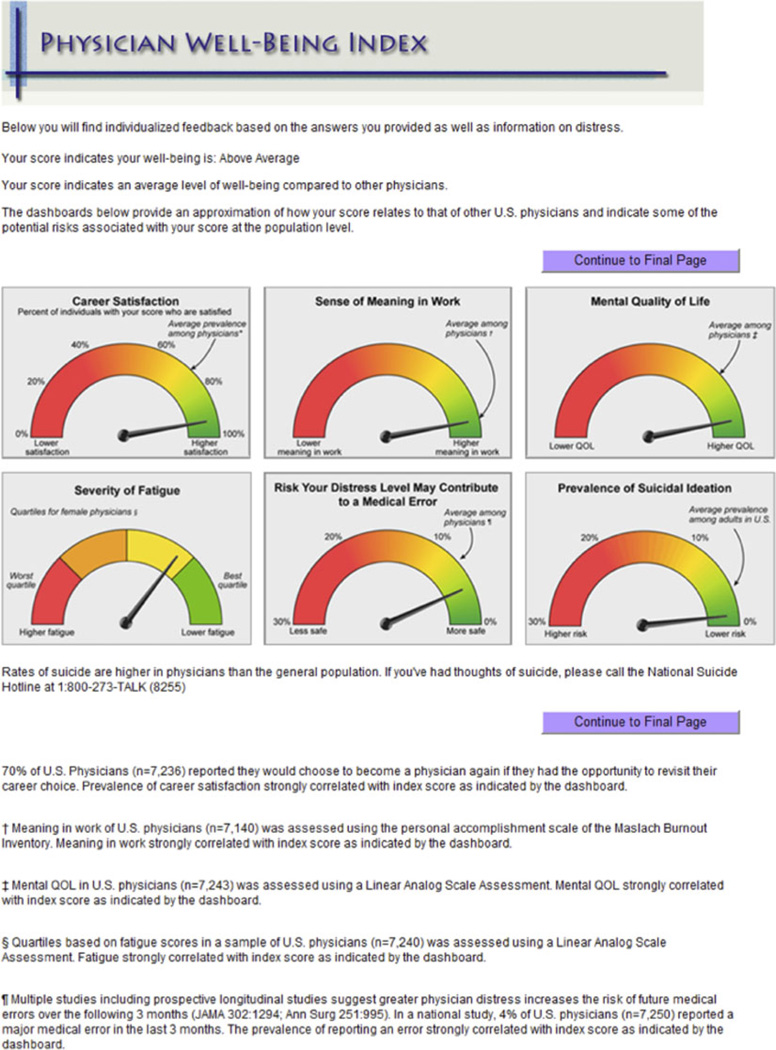
Second, surgeons completed the 7-item MPWBI and subsequently received immediate, individualized feedback (Fig. 1). This feedback informed the participants how their well-being compared with national physician norms31 and provided information on risk in 6 specific dimensions (fatigue, career satisfaction, meaning in work, risk of suicidal ideation, risk degree of distress may contribute to errors, and mental quality of life). Third, surgeons answered follow-up questions evaluating the usefulness of the information provided and indicating whether they intended to make any specific changes “as a result of reviewing the feedback” to (i) reduce burnout, (ii) reduce fatigue, (iii) promote work-life balance, or (iv) promote career satisfaction.
FIGURE 1.
Example of individualized feedback provided to surgeons completing the online self-assessment using the MPWBI. QOL indicates quality of life.
Statistical Analysis
Standard descriptive statistics were used to characterize responding surgeons. Associations between variables were evaluated using the Kruskal-Wallis test (continuous variables) or χ2 test (categorical variables) as appropriate. All tests were 2-sided, with type I error rates of 0.05. All analyses were done using SAS, version 9 (SAS Institute, Inc, Cary, NC).
RESULTS
Of the 8000 fellows and associate fellows of the ACS notified of the study by e-mail, 1150 volunteered to participate. The basic demographic and practice characteristics of study participants are shown in Table 2. The median age of volunteers was 53 years, and 84.2%were men. Participating surgeons had been in practice amedian of 20 years, and most were in either private practice (46.7%) or academic practice (36.7%). When asked to subjectively assess their well-being relative to other physicians, 993 surgeons (89.2%) believed that theirwell-beingwas at or above average.Only 25 surgeons (2.2%) believed that their well-being was in the bottom 30% relative to other physicians (Table 2).
TABLE 2.
Demographic and Practice Characteristics
| Age, yr | |
| Median | 53 (10.6) |
| <40 | 120 (11.3%) |
| 40–49 | 288 (27.2%) |
| 50–59 | 369 (34.8%) |
| 60+ | 283 (26.7%) |
| Missing | 90 |
| Sex | |
| Women | 176 (15.8%) |
| Men | 937 (84.2%) |
| Missing | 37 |
| Years in practice | |
| Median | 20 |
| <10 | 215 (20.8%) |
| 10–19 | 290 (28.0%) |
| ≥20 | 530 (51.2%) |
| Missing | 115 |
| Practice setting | |
| Private practice | 520 (46.7%) |
| Academic practice | 408 (36.7%) |
| Military | 18 (1.6%) |
| Veterans | 15 (1.4%) |
| Other* | 152 (9.7%) |
| How do you think your well-being compares with other physicians? | |
| Poor (bottom 30% of physicians) | 25 (2.2%) |
| Below average (31st–40th percentile) | 95 (8.5%) |
| Average (41st–60th percentile) | 329 (29.6%) |
| Above average (61st–70th percentile) | 325 (29.2%) |
| Excellent (top 30% of physicians) | 339 (30.5%) |
| Missing | 37 |
Values given are number (percentage) unless indicated otherwise.
Other category includes those working in other practice settings, other areas (eg, industry), or retired.
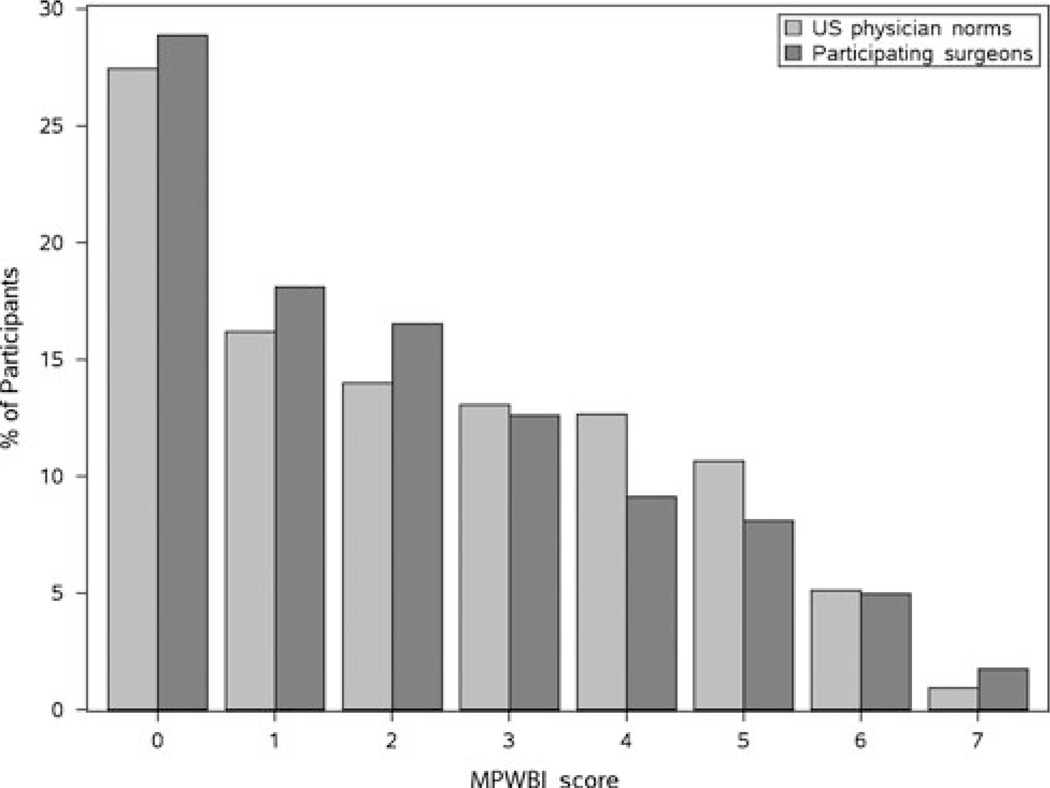
The distribution of scores on the MPWBI is shown in Figure 2. Scores of participating surgeons were consistent with that expected on the basis of national physician normative data, with 28.9% of surgeons scoring into the top 30% relative to national norms and 24% scoring in the bottom 30% relative to national norms.31
FIGURE 2.
Distribution of MPWBI scores. The figure shows the distribution of MPWBI scores (x axis) of the participating surgeons (dark gray bars; n=1150) relative to a normative sample of approximately 7000 US physicians (light gray bars).31 Higher scores indicate greater levels of distress. MPWBI indicates Mayo Physician Well-Being Index.
Surgeons’ ability to subjectively assess their own well-being relative to other physicians was poor. Among the 275 surgeons with an MPWBI score of 4 or more (eg, in the bottom ~30% relative to national physician norms), 194 (70.5%) believed that their well-being was at or above average, including 66 (24.0%) who believed that their well-being was above average relative to other physicians. Similarly, among the 332 surgeons with an MPWBI score of 0 (eg, top ~30% relative to national physician norms), 40 (13.6%) believed that their well-being was at or below average.
Surgeons were next asked to subjectively “indicate whether the individualized feedback from the online self-assessment tool was helpful for calibrating personal well-being relative to your colleagues” (Table 3). Collectively, 546 surgeons (49.5%) rated the feedback “somewhat” to “extremely” helpful (highest 3 choices on a 5-point scale), 257 (23.3%) reported that the information was only slightly helpful, and 301 (27.3%) reported that the feedback was not helpful. Surgeons with better well-being scores on the MPWBI were as or more likely to report that they found the feedback helpful as those with lower well-being scores (Table 3).
TABLE 3.
Subjective Assessment of Feedback Utility and Intent to Make Changes as a Direct Result of the Feedback
| Proportion of Surgeons Rating Feedback “Somewhat” to “Extremely Helpful” |
|
|---|---|
| MPWBI score* | |
| 0 | 65.0% |
| 1 | 49.0% |
| 2 | 43.6% |
| 3 | 41.0% |
| 4 | 36.5% |
| ≥5 | 44.6% |
| Proportion of surgeons reporting they were considering making a change as a direct result of feedback to: | N = 1150 |
| Reduce burnout | 296 (26.7%) |
| Reduce fatigue | 302 (27.3%) |
| Promote work-life balance | 437 (39.2%) |
| Promote career satisfaction | 380 (34.2%) |
| ≥1 of above | 529 (46.6%) |
Lower scores indicate less distress and higher well-being.
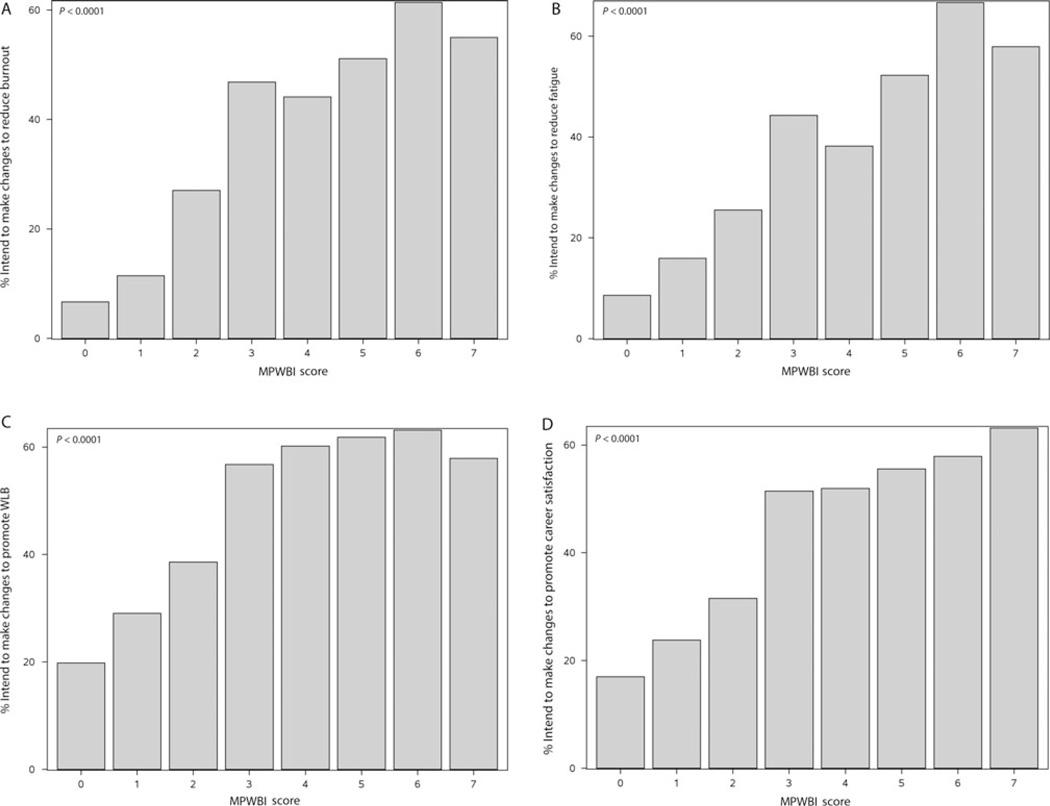
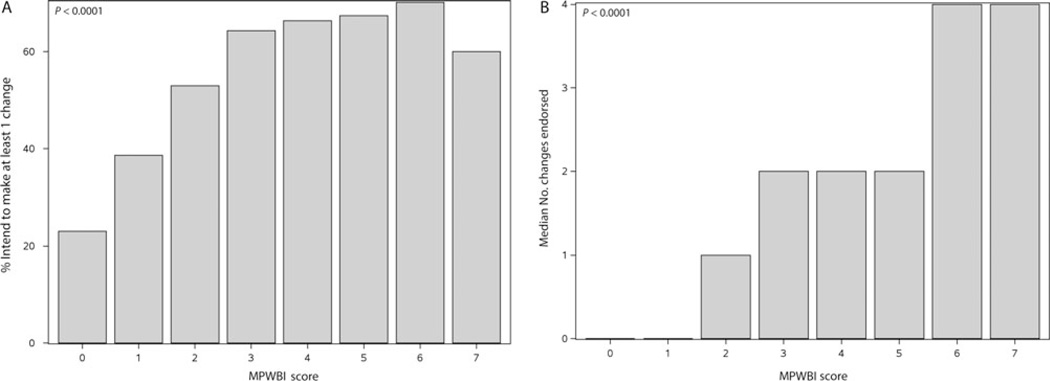
Finally, surgeons were asked whether they were considering making a change in any of 4 specific dimensions (eg, to reduce burnout, to reduce fatigue, to promote work-life balance, and to promote career satisfaction) as a direct result of the feedback on how their well-being compared with other physicians (Table 3). As a direct result of the individualized feedback, 296 participants (26.7%) reported that they intended to make changes to reduce burnout, 302 (27.3%) to reduce fatigue, 437 (39.2%) to promote work-life balance, and 380 (34.2%) to promote career satisfaction. Collectively, 529 (46.6%) indicated that they were considering making a change in at least 1 of these dimensions as a result of the individualized feedback. A strong dose-response relationship was observed between feedback that an individual’s well-being was lower than physician norms and intent to make a change. In each of the 4 dimensions evaluated, surgeons having lower well-being were more likely to be considering making a change (Figs. 3A–D). The proportion of surgeons considering making at least 1 change (Fig. 4A) and the number of changes being considered (Fig. 4B) also increased on the basis of the feedback surgeon’s received regarding how their well-being compared with physician norms on the MPWBI.
FIGURE 3.
Feedback regarding well-being relative other physicians and intent to make changes to promote well-being. MPWBI scores are shown on the x axis (higher scores indicate greater levels of distress). The proportion of surgeons who indicated they were considering making changes to reduce burnout (A), reduce fatigue (B), promote work-life balance (C), and promote career satisfaction (D) as a direct result of the individualized feedback received is shown on the y axis of each figure. Feedback of higher levels of distress relative to physician norms was correlated with higher likelihood of considering making changes in each dimension. MPWBI indicates Mayo Physician Well-Being Index; WLB, work-life balance.
FIGURE 4.
MPWBI score and intent to make changes. MPWBI scores are shown on the x axis (higher scores indicate greater levels of distress) of each figure. A, The proportion of surgeons who indicated they were considering making changes in at least 1 of the 4 dimensions assessed (Fig. 3) as a direct result of the individualized feedback they received is shown on the y axis. B, The median number of changes (range = 1–4) being considered is shown on the y axis. MPWBI indicates Mayo Physician Well-Being Index.
DISCUSSION
Despite the high prevalence of distress among US physicians, few physicians seek help of their own initiative.27,29,30 In the present study of more than 1000 US surgeons, physicians’ ability to reliably calibrate their level of distress relative to colleagues was poor. The high prevalence of burnout among physicians may lead some individuals with severe distress to believe that their experience is simply a normal part of being a physician. Likewise, physicians may compare their experience with a limited circle of colleagues they interact with regularly but who may not be a representative sample. Among surgeons whose well-being was in the lowest 30% relative to national physician norms, the majority (>70%) believed that their well-being was at or above average, including approximately 25% who believed that their well-being was above average. These findings illustrate poor calibration and lack of awareness—both of which may be important barriers to physicians taking steps to promote personal health and well-being.
Behavioral change is believed to be a multistep process characterized by at least 6 phases: precontemplation (no intent to make changes; may not be aware of the need for change), contemplation (aware of the need for a change and considering making a change in near future), preparation (ready to take action and have begun making plans to change), action (have taken action and changed their behavior), maintenance (sustain new habits avoid regression to old ways), and termination (certainty that able to preserve healthy approaches rather than reverting to old unhealthy habits).34 The poor self-calibration of well-being likely results in many surgeons being at the precontemplation stage of this process, unaware of the need for a change to promote resilience and improve career satisfaction.
The intervention phase of this study provides encouraging results. When surgeons received objective, individualized feedback on how their well-being compared with normative samples of physicians and potential personal and professional risks (Fig. 1), they recognized the need for a change. Nearly half of the study participants indicated that they were considering making at least 1 change to reduce burnout, reduce fatigue, promote work-life balance, or promote career satisfaction as a direct result of the individualized feedback. Strikingly, the individualized feedback on distress level as stratified by the MPWBI was strongly associated with intent to make a change in each of the 4 dimensions assessed. Those with greater distress were also considering a greater number of changes as a result of the feedback. Because physicians have reached their standing by being high achievers, feedback to those in distress on how their well-being relates to peers may leverage their competitive nature and desire to be successful to help promote changes to improve well-being.
These observations provide evidence that the specific feedback provided to those most in need of a change helped them progress from the precontemplation phase to the contemplation phase. The graded, incremental increase in the proportion intending to make a change and the number of changes they were considering as distress level increased also indicates that the feedback effectively conveyed stratified information to participating surgeons. Surgeons whose well-being was only slightly below average planned to make more limited adjustments in a fewer number of domains, suggesting that the feedback may have helped these individuals promote early intervention and prevention before more severe distress developed. Notably, although physicians with the highest levels of well-being were appropriately less likely to report that they were considering making changes, they were as or more likely to report that they found the individualized feedback helpful. This observation may indicate that physicians’ confidence in the accuracy of their self-calibration is low (although they think that their well-being is above average they are not certain) and that the objective information helped affirm and reassure those with high well-being. Collectively, these findings suggest that periodic assessment and feedback may have relatively universal benefit for physicians because it seems to provide useful information both to those who are doing well (affirmation and reassurance) and to encourage behavioral change to those who are struggling.
Our study is subject to several limitations. Considering making a change to promote well-being is one step in the process of behavioral change and will not result in an actual change in many cases. Nonetheless, the intervention tested helped a large proportion of surgeons move from the precontemplation phase of behavioral change to the contemplation phase, which is the necessary first step to a meaningful change. Longitudinal studies are needed to see how many physicians proceed to the preparation and action phases. Combining the interactive electronic intervention tested here in conjunction with follow-up initiatives may increase the proportion of physicians proceeding to the action phase.34 For example, applying an interactive version of the MPWBI to assess well-being and provide individualized feedback may be a useful first step that helps bring physicians to the point they are ready to consider a change. Physicians could then be offered a menu of specific activities to reduce burnout and fatigue or to promote work-life balance and career satisfaction.34,35 Several publications have reviewed strategies surgeons can take to promote their well-being.5,24,37–40
It is unknown whether the study participants are representative of surgeons in general. Although the sample size was large and study volunteers were drawn from a random, national sample of surgeons who are members of the ACS, only approximately 14% of those notified about the study volunteered to participate. Participation rates are a well-recognized problem in medical research trials in the United States.41,42 The age, sex, practice setting, and years in practice of volunteers seem similar to surgeons in prior studies of the ACS membership,2,23 suggesting that the participating surgeons are likely representative. Nonetheless, replication of these findings in other samples will be important.
CONCLUSIONS
US surgeons do not reliably calibrate their level of distress. After interactive, self-assessment with individualized feedback based on the MPWBI, nearly half of surgeons reported that they were contemplating behavioral changes to improve personal well-being. Surgeons with greater distress were more likely to be considering making changes to promote well-being and to be contemplating changes in a greater number of dimensions. The interactive electronic intervention tested here seems to provide useful information to surgeons and to help those with greater degrees of distress move from the precontemplation phase to the contemplation phase of making changes to promote personal well-being.
Acknowledgments
Supported by funding from the National Institutes of Health (ACOSOG CCOP U10 CA149950), the American College of Surgeons, and the Mayo Clinic Department of Medicine Program on Physician Well-Being.
Footnotes
Disclosure: T. Shanafelt and L. Dyrbye developed both the Medical Student Well-Being Index and Mayo Clinic Physician Well-Being Index. Mayo Clinic holds the copyright on these technologies and accordingly Mayo Clinic and Drs Shanafelt and Dyrbye have a potential financial interest in these technologies. The Medical Student Well-Being Index has been licensed to a commercial entity, although no royalties have been received to date. To obtain permission to use the index, please contact the corresponding author.
The authors declare no conflicts of interest.
REFERENCES
- 1.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–1385. 1–9. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 3.Campbell DA, Jr, Sonnad SS, Eckhauser FE, et al. Burnout among American surgeons. Surgery. 2001;130:696–702. doi: 10.1067/msy.2001.116676. discussion 702–705. [DOI] [PubMed] [Google Scholar]
- 4.Kuerer HM, Eberlein TJ, Pollock RE, et al. Career satisfaction, practice patterns and burnout among surgical oncologists: report on the quality of life of members of the Society of Surgical Oncology. Ann Surg Oncol. 2007;14:3043–3053. doi: 10.1245/s10434-007-9579-1. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt T, Sloan J, Habermann T. The well-being of physicians. Am J Med. 2003;114:513–517. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 6.Dyrbye LN, Harper W, Durning S, et al. Patterns of distress in US medical students. Med Teach. 2011;33:834–839. doi: 10.3109/0142159X.2010.531158. [DOI] [PubMed] [Google Scholar]
- 7.Bertges Yost W, Eshelman A, Raoufi M, et al. A national study of burnout among American transplant surgeons. Transplant Proc. 2005;37:1399–1401. doi: 10.1016/j.transproceed.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 8.Allegra C, Hall R, Yothers G. Prevalence of burnout in the U.S. oncology community: results of a 2003 survey. J Oncol Pract. 2005;1:140–147. doi: 10.1200/jop.2005.1.4.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 10.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 11.Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- 12.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 13.West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 14.Williams ES, Manwell LB, Konrad TR, et al. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32:203–212. doi: 10.1097/01.HMR.0000281626.28363.59. [DOI] [PubMed] [Google Scholar]
- 15.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 16.Balch CM, Shanafelt TD, Dyrbye L, et al. Surgeon distress as calibrated by hours worked and nights on call. J Am Coll Surg. 2010;211:609–619. doi: 10.1016/j.jamcollsurg.2010.06.393. [DOI] [PubMed] [Google Scholar]
- 17.Dyrbye LN, Shanafelt TD, Balch CM, et al. Physicians married or partnered to physicians: a comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211:663–671. doi: 10.1016/j.jamcollsurg.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 18.Balch CM, Shanafelt TD. Burnout among surgeons: whether specialty makes a difference. Arch Surg. 2011;146:385–386. doi: 10.1001/archsurg.2011.53. [DOI] [PubMed] [Google Scholar]
- 19.Balch CH, Oreskovich MR, Dyrbye LN, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213:657–667. doi: 10.1016/j.jamcollsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Dyrbye LN, Shanafelt TD, Balch CM, et al. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146:211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 21.Balch CM, Shanafelt TD, Sloan J, et al. Burnout and career satisfaction among surgical oncologists compared with other surgical specialties. Ann Surg Oncol. 2011;18:16–25. doi: 10.1245/s10434-010-1369-5. [DOI] [PubMed] [Google Scholar]
- 22.Shanafelt T, Sloan J, Satele D, et al. Why do surgeons consider leaving practice? J Am Coll Surg. 2011;212:421–422. doi: 10.1016/j.jamcollsurg.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 24.Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg. 2012;255:625–633. doi: 10.1097/SLA.0b013e31824b2fa0. [DOI] [PubMed] [Google Scholar]
- 25.Balch CM, Shanafelt TD, Sloan JA, et al. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254:558–568. doi: 10.1097/SLA.0b013e318230097e. [DOI] [PubMed] [Google Scholar]
- 26.Balch CM, Oreskovich MR, Dyrbye LN, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213:657–667. doi: 10.1016/j.jamcollsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Shanafelt TD, Balch C, Dyrbye LN, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 28.Kent GG, Johnson AG. Conflicting demands in surgical practice. Ann R Coll Surg Engl. 1995;77:235–238. [PubMed] [Google Scholar]
- 29.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289:3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 30.Balch CM, Shanafelt TS. Dynamic tension between success in a surgical career and personal wellness: how can we succeed in a stressful environment and a “culture of bravado”? Ann Surg Oncol. 2011;18:1213–1216. doi: 10.1245/s10434-011-1629-z. [DOI] [PubMed] [Google Scholar]
- 31.Dyrbye LN, Satele D, Sloan J, et al. Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med. 2013;28:421–427. doi: 10.1007/s11606-012-2252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dyrbye LN, Szydlo DW, Downing SM, et al. Development and preliminary psychometric properties of a well-being index for medical students. BMC Med Educ. 2010;10:8. doi: 10.1186/1472-6920-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dyrbye LN, Schwartz A, Downing SM, et al. Efficacy of a brief screening tool to identify medical students in distress. Acad Med. 2011;86:907–914. doi: 10.1097/ACM.0b013e31821da615. [DOI] [PubMed] [Google Scholar]
- 34.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 35.Velicer WF, Prochaska JO, Bellis JM, et al. An expert system intervention for smoking cessation. Addict Behav. 1993;18:269–290. doi: 10.1016/0306-4603(93)90029-9. [DOI] [PubMed] [Google Scholar]
- 36.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 37.Balch CM, Shanafelt T. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29–47. doi: 10.1016/j.yasu.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 38.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144:371–376. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 39.Shanafelt T. A career in surgical oncology: finding meaning, balance, and personal satisfaction. Ann Surg Oncol. 2008;15:400–406. doi: 10.1245/s10434-007-9725-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuerer HM, Breslin T, Shanafelt TD, et al. Road map for maintaining career satisfaction and balance in surgical oncology. J Am Coll Surg. 2008;207:435–442. doi: 10.1016/j.jamcollsurg.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 41.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 42.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]