Abstract
Background
The present study was conducted to assess the preparedness of hepatopancreatobiliary (HPB) fellows upon entering fellowship, identify challenges encountered by HPB fellows during the initial part of their HPB training, and identify potential solutions to these challenges that can be applied during residency training.
Methods
A questionnaire was distributed to all HPB fellows in accredited HPB fellowship programmes in two consecutive academic years (n = 42). Reponses were then analysed.
Results
A total of 19 (45%) fellows responded. Prior to their fellowship, 10 (53%) were in surgical residency and the rest were in other surgical fellowships or surgical practice. Thirteen (68%) were graduates of university-based residency programmes. All fellows felt comfortable in performing basic laparoscopic procedures independently at the completion of residency and less comfortable in performing advanced laparoscopy. Eight (42%) fellows cited a combination of inadequate case volume and lack of autonomy during residency as the reasons for this lack of comfort. Thirteen (68%) identified inadequate preoperative workup and management as their biggest fear upon entering practice after general surgery training. A total of 17 (89%) fellows felt they were adequately prepared to enter HPB fellowship. Extra rotations in transplant, vascular or minimally invasive surgery were believed to be most helpful in preparing general surgery residents pursing HPB fellowships.
Conclusions
Overall, HPB fellows felt themselves to be adequately prepared for fellowship. Advanced laparoscopic procedures and the perioperative management of complex patients are two of the challenges facing HPB fellows. General surgery residents who plan to pursue an HPB fellowship may benefit from spending extra rotations on certain subspecialties. Focus on perioperative workup and management should be an integral part of residency and fellowship training.
Introduction
The preparedness of trainees for surgical practice has been questioned in the wake of certain changes in surgical practice and training. The effect of work hour restrictions on surgical training has also been a subject of ongoing debate.1 Objective evidence for this has been an increase in the rate of failure on the oral board examination from 15% in 2003 to 25% in 2013.2 Subjectively, a recent survey of Fellowship Council (FC) programme directors on the competency of their fellows demonstrated that nearly 43% of programme directors felt that an incoming fellow was unable to perform 30 min of a major procedure independently.3 Furthermore, 30% of programme directors felt their fellows were unable to perform a laparoscopic cholecystectomy without supervision. Similar opinions have been expressed by other leaders in surgical education.4–6
The lack of preparedness is also a concern of surgical residents. In a recent survey of senior general surgery residents, 25% felt unprepared for independent practice.7,8 As a result, over 80% of general surgery residents now pursue fellowship training for an additional 1–2 years.9 The duration of many of these fellowships is only 1 year, which results in a steep learning curve for the trainee. This highlights the importance of being sufficiently prepared on entering fellowship such that one can master complex skills in 1 year of additional training. Several studies have correlated the degree of preparedness of a trainee to the flattening of the learning curve.10,11 Trainees who do enter fellowship without being comfortable in basic open and laparoscopic techniques may not be able to master the complex procedures to which they are exposed during a 1-year fellowship.10,11
Hepatopancreatobiliary (HPB) surgery is a technically demanding field that requires expertise in advanced open and laparoscopic procedures. It also requires familiarity with vascular surgical principles and technique. The management of HPB diseases is also more complex than disease management in other specialties and is associated with a high rate of complications, including unique complications that are not typically seen in general surgery practice. For these reasons, HPB surgery fellowship is well suited to the study of preparedness in general surgery residents. The aim of this study is to identify challenges experienced by HPB fellows during the initial part of their HPB training and to put forward potential solutions to these challenges that can be integrated into the curriculum of general surgery residency training.
Materials and methods
An online questionnaire was designed by the present authors. Answer choices were congruent with a validated Likert scale. The questionnaire was distributed to the Americas Hepato-Pancreato-Biliary Association (AHPBA) subcommittee of HPB fellows in the class of 2012/2013 and was then revised according to the committee's recommendations. The final questionnaire consisted of 40 questions to evaluate five major categories of interest: the background of the fellow's residency training; the degree of independence achieved in performing general surgery procedures at the end of residency training; the challenges of entering independent practice after residency training; clinical and technical preparedness for an HPB fellowship, and proposed adjustment during residency to improve preparedness for HPB fellowships (Table 1). Although the reliability and reproducibility of the questions were not explicitly tested, the questions were based on those used in similar studies.
Table 1.
Outline of the electronically distributed questionnaire evaluating five major aspects of preparedness to enter a hepatopancreatobiliary (HPB) surgery fellowship
| Category | Questions | Answer choices |
|---|---|---|
| Fellow's prior training background | Setting prior to HPB fellowship | Residency, fellowship, or practice |
| Type of residency programme | University, community, hybrid, other | |
| Number of major cases performed during residency | <800, 800–999, 1000–1200, >1200a | |
| Pre-fellowship HPB experience: number of pancreatic, hepatic and biliary (excluding cholecystectomy) cases | <5, 5–10, >10a | |
| Degree of independence in performing general surgery procedures at the completion of residency training | Need for supervision in various basic and advanced open and laparoscopic procedures | No supervision, minimal supervision, full supervision |
| Challenges associated with entering independent practice after surgical residency | Reasons for lack of comfort in performing procedures independently | Work hour restriction, lack of autonomy, lack of time to prepare, lack of case volume (all during residency) |
| Areas of more concern and lack of comfort | Preoperative workup, performing procedures, complications, postoperative management | |
| Clinical and technical preparedness for HPB fellowship (during the first 3 months of fellowship) | Preparedness for handling: benign disease in pancreas; malignant disease in pancreas; hepatic disease; benign biliary disease, and malignant biliary disease | Poor, fair, adequate, excellent |
| Level of comfort in performing procedures with faculty supervision: open pancreas; MIS in pancreas; open liver surgery; MIS in liver, and biliary surgery | Comfortable with both anatomy and steps, comfortable with anatomy but not steps, comfortable with steps but not anatomy, uncomfortable with anatomy and steps | |
| Overall preparedness for HPB fellowship | Poor, fair, adequate, excellent | |
| Potential adjustments during residency to improve preparedness for HPB fellowship | Adjustments to improve preparedness for independent practice after residency | Operative autonomy, studying and didactic time, total training time, use of simulation |
| Surgical rotations that might prepare general surgery residents for HPB training | Vascular, transplant, bariatric, MIS, colorectal, general surgery |
Answer choices are based on the American Board of Surgery requirements for required experience for graduating residents.
MIS, minimally invasive surgery.
The questionnaire was electronically distributed to all fellows in FC-accredited HPB programmes in two consecutive academic years: 2012/2013 and 2013/2014. In the academic year of 2012/2013, both first- and second-year fellows in the 2-year programmes were targeted. Fellows' contact information was obtained through the FC and HPB fellowship programme directors. The survey was conducted anonymously and all collected data were de-identified. Survey results were tallied and significance testing was performed using Fisher's exact probability test. A P-value of <0.05 was considered to indicate statistical significance. Institutional review board approval was obtained.
Results
Questionnaires were sent to all 42 fellows, 19 (45%) of whom responded. Of these, 53% had entered their HPB fellowship as fresh graduates of general surgery residencies, 32% had been in other surgical fellowships, and 16% had been in surgical practice. University-based programmes constituted the majority (68%) of HPB fellows' residency training. Prior to their HPB fellowship, 63% of the fellows had performed more than 10 pancreas cases, and 47% had performed more than 10 liver cases and five to 10 biliary cases excluding cholecystectomy (Fig. 1).
Figure 1.
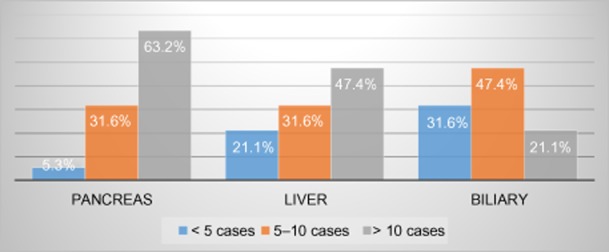
Hepatopancreatobiliary (HPB) cases performed by fellows prior to their HPB fellowship
When asked about need for supervision in performing certain surgical procedures at the completion of surgical residency training, 100% of the fellows reported that they felt comfortable in performing laparoscopic cholecystectomy without the need for supervision and 21% expressed a need for minimal supervision in performing open cholecystectomy. All fellows felt comfortable in performing open colon resection with no or minimal supervision, but 31% needed full supervision to perform the same procedure laparoscopically. Fellows felt more comfortable in performing more complex surgical procedures through an open approach; 84% expressed a need for full supervision in performing a laparoscopic Roux en-Y procedure, whereas only 16% required full supervision in an open approach. Totals of 32% and 53% of fellows indicated the need for full supervision in performing open gastrectomy and laparoscopic Nissen fundoplication, respectively (Fig. 2). Only 5% reported being able to perform an arteriovenous fistula without supervision. Of those who stated a requirement for full supervision, 47% cited lack of case volume as the reason and 42% attributed the need to lack of both case volume and intraoperative autonomy. A total of 90% of fellows cited ‘more time in the operating room’ as a factor that would make them feel better prepared to perform some of the complex procedures, rather than the use of simulators or more time to study. When asked about their biggest concern or fear upon entering practice after general surgery residency training, 47% referred to the ability to adequately assess patients preoperatively and 32% referred to the failure to recognize and manage postoperative complications. Only 21% cited technical ability as representing their greatest fear.
Figure 2.
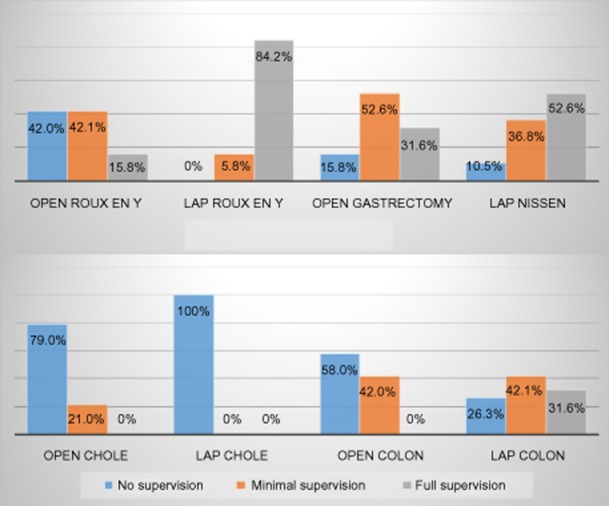
Level of comfort and independence of general surgery residency graduates in performing open and laparoscopic general surgery procedures. Chole, cholescystectomy; Colon, colon resection; Lap, laparoscopic
The majority of fellows felt well prepared to manage pancreatic and benign biliary disease upon entering fellowship. This sense of preparedness was lessened when it came to managing hepatic and malignant biliary disorders (Fig. 3). In the first 3 months of fellowship, fellows felt more comfortable in performing open pancreatic and liver procedures with faculty supervision than laparoscopic cases (Fig. 4). Overall, 89% of fellows felt well prepared for the fellowship. Transplant, vascular surgery and minimally invasive surgery (MIS) were cited as the most likely rotations to prepare residents for the technical aspects of an HPB fellowship (Fig. 5).
Figure 3.
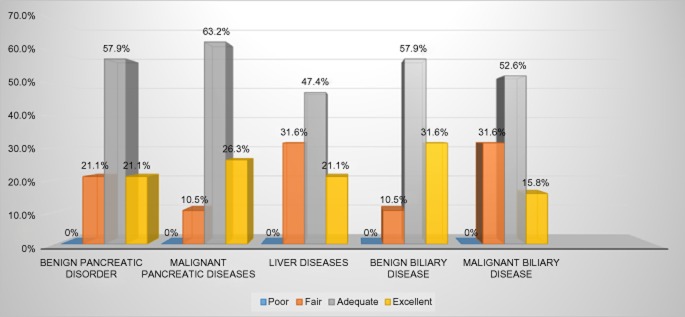
Preparedness of hepatopancreatobiliary (HPB) fellows to manage HPB disorders in the first 3 months of HPB fellowship
Figure 4.
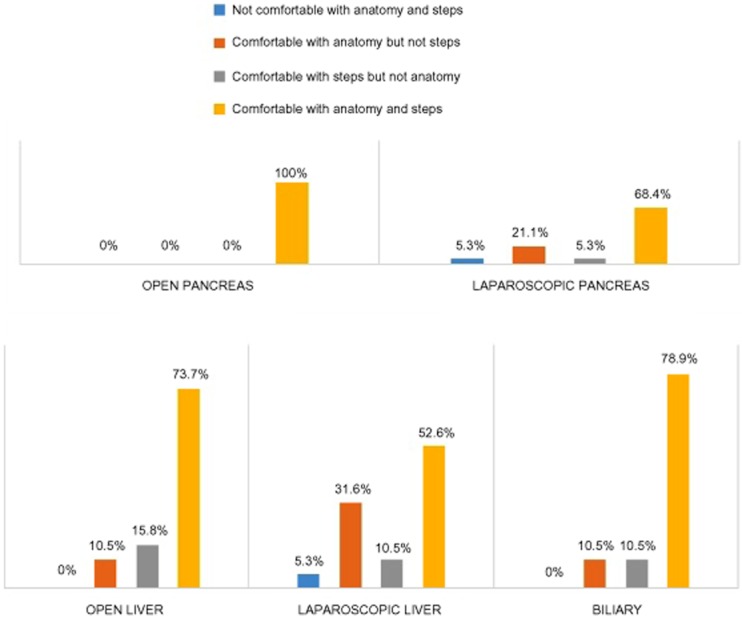
Hepatopancreatobiliary (HPB) fellows are more comfortable performing open than laparoscopic HPB cases in the first 3 months of an HPB fellowship
Figure 5.
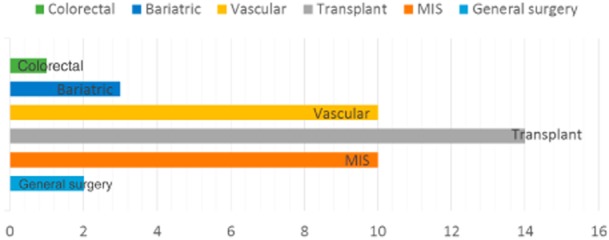
Transplant, vascular and minimally invasive surgery (MIS) rotations during residency training are likely to better prepare surgical residents for hepatopancreatobiliary fellowship
The responses from the nine fellows who were in surgical practice or surgical fellowship prior to HPB training were then analysed separately. Interestingly, the responses of this subgroup were very similar to those of the entire cohort. Overall, 67% and 44% of fellows in this subgroup had performed more than 10 pancreatic and liver cases, respectively, prior to their HPB fellowship; these proportions are similar to those in the entire cohort. All fellows in this subgroup felt comfortable in performing laparoscopic cholecystectomy and only one (11%) fellow reported a need for minimal supervision in performing open cholecystectomy, whereas 21% of the entire cohort did so. Of fellows with prior post-residency experience, 33% and 100% stated a requirement for full supervision in performing laparoscopic colon resection and laparoscopic Roux en-Y, respectively. Similarly to the entire cohort, 67% of fellows with post-residency surgical experience prior to fellowship cited inadequate preoperative workup and failure to recognize and manage postoperative complications as their biggest concerns after residency training. A total of 78% of this subgroup felt themselves to be adequately prepared for their HPB fellowship compared with 89% of the entire cohort and a similar trend towards a decreased level of comfort in performing laparoscopic HPB cases in the first 3 months of the fellowship emerged.
Discussion
This study examines the issue of preparedness from the perspective of the trainee in an HPB surgery fellowship. Trainees entering HPB fellowships seem to have robust experience with HPB operations. According to the present survey, 63% of fellows had performed more than 10 pancreatic cases prior to their fellowship and nearly half of all fellows had performed more than 10 liver cases. This exceeds the Accreditation Council for Graduate Medical Education (ACGME) requirements for graduating surgical residents. The fact that most of the fellows had trained at university-based programmes and perhaps the inherent interest in HPB surgery that caused trainees to seek out an HPB experience during residency can be argued as potential explanations for this finding. Interestingly, fellows with post-residency surgical experience in terms of other surgical fellowships or independent practice had HPB exposure similar to that of those who entered HPB fellowship straight after residency.
With regard to technical ability, all survey respondents felt comfortable in performing basic laparoscopic procedures independently, but a clear trend showing a decreasing level of comfort in line with the increasing complexity of laparoscopic procedures was apparent. This can be attributed to the steeper learning curve involved in such procedures and inadequate case volume or lack of autonomy in these complex cases during residency training. More alarming was the issue of preparedness in vascular surgery techniques as only 5% of respondents reported being able to perform an arteriovenous fistula without supervision. It is unclear why this number is so low as this is one of the most common operations performed in vascular surgery. This may reflect a lack of volume and/or exposure given the rise in vascular surgery residency tracts. The fellows' sense of their own ability to perform laparoscopic cholecystectomy unsupervised was shared by only 70% of programme directors in FC-accredited programmes.9 This discordance may be explained by the fact that the FC has multiple fellowship programmes, which include HPB, thoracic, bariatric and MIS fellowships, and all programme directors in these fellowships were queried, whereas only fellows in HPB programmes were targeted in this study. This can be also attributed to a possible disconnect between trainers and trainees in perceptions of preparedness. It is difficult to determine whose perception is more accurate using survey-based tools as they are all inherently biased.
The importance of technique and dexterity in surgical training is undisputed. Interestingly, however, when asked about their biggest fear upon entering practice after residency training, 68% of respondents cited a fear of failure in preoperative workup and in the recognition of postoperative complications. A decline in the number of surgeries performed by surgical residents was noted with the implementation of the 80-h week work rule in the early 2000s, but this has since rebounded. It is arguable whether the unchanged case volume, given the fixed amount of time per week, has come at the expense of outpatient clinic exposure or postoperative management of floor patients.
The management of HPB diseases requires both complex clinical decision making and a wide and deep array of technical skills. Preparedness for a career in HPB surgery is likely to differ from that in other subspecialties. Although transplant surgery is technically challenging, it does not require advanced laparoscopic and robotic surgery skills. Similarly, MIS does not provide the open surgery experience. Trainees in HPB surgery have understood these challenges, which explains why almost half of HPB surgery fellows in the present survey group were found to have come from practice or from another fellowship. Common fellowships prior to an HPB surgery fellowship include those in minimally invasive and transplant surgery. The slight discomfort experienced in managing hepatic and malignant biliary diseases in comparison with pancreatic and benign biliary disorders may be simply a product of the paucity of these conditions and lack of exposure during residency. This would further validate the need for HPB training for those who plan to manage such conditions in their practice. It was not surprising that transplant surgery, vascular surgery and MIS were voted as the most likely rotations to prepare general surgery residents for an upcoming HPB fellowship. Unlike HPB surgery, these rotations are readily available to surgical residents. Transplant surgery, specifically liver and pancreas transplant surgery, involves the organs that are targeted in an HPB fellowship and shares a similar level of patient complexity. The vascular technique is unquestionably of paramount importance to an HPB surgeon and minimally invasive surgery addresses the lack of comfort in advanced laparoscopic procedures that is clearly evident in this study.
The limitations of this study are those inherent to all survey-based studies and refer to the response rate and the potential for recall bias. Specific limitations of this study assessing the preparedness of general surgery residents entering HPB fellowship concern the fact that 48% of the fellows surveyed were in other surgical fellowships or surgical practice, which may further accentuate the potential recall bias. Finally, there may be some response bias that results in the overstatement of a fellow's true level of preparedness. Despite these limitations, the present findings provide insight into the composition of trainees who pursue HPB fellowships and their perceptions of their preparedness. Future steps include comparing the present results against the assessments of FC programme directors of HPB surgery fellowship programmes and tracking graduates of HPB fellowships into practice to better understand their preparedness from both a general surgery and an HPB surgery perspective.
Conclusions
Overall, HPB fellows felt themselves to be adequately prepared for fellowship. Advanced laparoscopic procedures and the perioperative management of complex patients represent two of the biggest challenges facing graduates of general surgery training. General surgery residents who plan to pursue HPB fellowships may benefit from spending extra rotations in certain subspecialties. Moreover, a focus on perioperative workup and management should be an essential part of residency and fellowship training.
Conflicts of interest
None declared.
References
- Durkin ET, McDonald R, Munoz A, Mahvi D. The impact of work hour restrictions on surgical resident education. J Surg Educ. 2008;65:54–60. doi: 10.1016/j.jsurg.2007.08.008. [DOI] [PubMed] [Google Scholar]
- American Board of Surgery. General Surgery Examination Statistics. Available at http://www.absurgery.org/default.jsp?statgeneral (last accessed 5 March 2014)
- Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258:440–449. doi: 10.1097/SLA.0b013e3182a191ca. [DOI] [PubMed] [Google Scholar]
- Debas HT. Surgery: a noble profession in a changing world. Ann Surg. 2002;236:263–269. doi: 10.1097/00000658-200209000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debas HT, Bass BL, Brennan MF, et al. American Surgical Association Blue Ribbon Committee report on surgical education: 2004. Ann Surg. 2005;241:1–8. doi: 10.1097/01.sla.0000150066.83563.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakayama DK, Taylor SM. SESC Practice Committee Survey: surgical practice in the duty-hour restriction era. Am Surg. 2013;79:711–715. [PubMed] [Google Scholar]
- Bucholz EM, Sue GR, Yeo H, Roman SA, Bell RH, Jr, Sosa JA. Our trainees' confidence: results from a national survey of 4136 US general surgery residents. Arch Surg. 2011;146:907–914. doi: 10.1001/archsurg.2011.178. [DOI] [PubMed] [Google Scholar]
- Coleman JJ, Esposito TJ, Rozycki GS, Feliciano DV. Early subspecialization and perceived competence in surgical training: are residents ready? J Am Coll Surg. 2013;216:764–773. doi: 10.1016/j.jamcollsurg.2012.12.045. [DOI] [PubMed] [Google Scholar]
- Kluger MD, Vigano L, Barroso R, Cherqui D. The learning curve in laparoscopic major liver resection. J Hepatobiliary Pancreat Sci. 2013;20:131–136. doi: 10.1007/s00534-012-0571-1. [DOI] [PubMed] [Google Scholar]
- El-Kadre L, Tinoco AC, Tinoco RC, Aguiar L, Santos T. Overcoming the learning curve of laparoscopic Roux-en-Y gastric bypass: a 12-year experience. Surg Obes Relat Dis. 2013;9:867–872. doi: 10.1016/j.soard.2013.01.020. [DOI] [PubMed] [Google Scholar]
- American College of Surgeons. June 2013 Bulletin. Available at http://www.facs.org/fellowsinfo/bulletin/bullet.html (last accessed 5 March 2014)


