Abstract
Telocytes (TCs) are a peculiar type of interstitial cells with very long prolongations termed telopodes. TCs have previously been identified in different anatomic structures of the heart, and have also been isolated and cultured from heart tissues in vitro. TCs and fibroblasts, both located in the interstitial spaces of the heart, have different morphologies and functionality. However, other than microscopic observation, a reliable means to make differential diagnosis of cardiac TCs from fibroblasts remains unclear. In the present study, we isolated and cultured cardiac TCs and fibroblasts from heart tissues, and observed their different morphological features and immunophenotypes in primary culture. Morphologically, TCs had extremely long and thin telopodes with moniliform aspect, stretched away from cell bodies, while cell processes of fibroblasts were short, thick and cone shaped. Furthermore, cardiac TCs were positive for CD34/c-kit, CD34/vimentin, and CD34/PDGFR-β, while fibroblasts were only vimentin and PDGFR-β positive. In addition, TCs were also different from pericytes as TCs were CD34 positive and α-SMA weak positive while pericytes were CD34 negative but α-SMA positive. Besides that, we also showed cardiac TCs were homogenously positive for mesenchymal marker CD29 but negative for hematopoietic marker CD45, indicating that TCs could be a source of cardiac mesenchymal cells. The differences in morphological features and immunophenotypes between TCs and fibroblasts will provide more compelling evidence to differentiate cardiac TCs from fibroblasts.
Introduction
Telocytes (TCs), a distinctive type of interstitial cells, have firstly been identified by Popescu’s group [1]. TCs are characterized by a small cell body and extremely long and thin telopodes with alternation of dilations (podoms) and thin segments (podomeres) [2–7]. The presence of TCs has been demonstrated in almost all mammalian organs and tissues [8–26]. For example, TCs have been identified in different anatomic structures of the heart, including epicardium [2], endocardium [3], myocardium [20,27], and heart valves [28]. Also, TCs in primary culture from heart tissues have been documented [29,30]. It was proved that TC could form a three-dimensional (3D) interstitial network by connecting with a variety of cells [28,29,31–37], and might play potential but important roles in tissue homeostasis [27,38,39], intercellular communication [4,29,35,37] and tissue repair/remodeling [40–47].
To date, transmission electron microscopy (TEM) remains a golden standard method for identifying TCs, since not a single immunomarker can be considered specific for detecting TCs [48]. However, to use a set of double immunolabeling for TCs is of fundamental importance since it allows to explicit their presence and to distinguish them from other types of interstitial cells [49,50]. Discrimination between TCs and fibroblasts is an important subject in TC identification. In theory, distinction between TCs and fibroblasts is evident as they have different morphological characteristics and functions [48,51]. Moreover, differences of gene profiles [52,53], microRNA signatures [54], as well as proteome features [55] between TCs and fibroblasts have been described in heart or lung tissues. Morphologically, cell processes of fibroblasts are usually few, short and thick, which make it theoretically easy to distinguish them from TCs under light microscope. However, some of the cells tagged as “fibroblasts” in the literature have similar morphological features as TCs, thus probably leading to confusion when identifying these two cell types [48].
The aim of the present study was to observe different morphological features of cardiac TCs and fibroblasts in primary culture, and to determine their different immunophenotypes by using a set of double immunofluorescent staining for CD34/c-kit, CD34/vimentin, and CD34/PDGFR-β, which might provide more reliable means and evidence to discriminate between TCs and fibroblasts in heart tissues.
Materials and Methods
Animals
Male C57BL/6 mice, weighed 25–30 g (10–12 weeks), were purchased from the animal research center of Fudan University. Mice were housed in a temperature-controlled room on a 12 h light/dark cycle, with ad libitum access to food and water. All animal experiments were conducted under the guidelines on the use and care of laboratory animals for biomedical research published by National Institutes of Health (No. 85–23, revised 1996). This study was approved by the committee on the Ethics of Animal Experiments of Tongji Hospital (Permit Number: KYSB-2014–41). All surgery was perfomed under sodium pentobarbital anesthesia and all efforts have been made to mininmize suffering.
Isolation and primary culture of TCs and fibroblasts from heart tissues
After mice were anesthetized with 1% pentobarbital sodium, the hearts were isolated under sterile conditions and kept in Hank’s balanced salt solution (HBSS, R21–022-CV, Corning, NY, USA), supplemented with 100 U/ml penicillin and 100 μg/ml streptomycin (R30–002-CI, Corning) and 0.01 mM HEPES (H3375, Sigma, St. Louis, MO, USA). After transported to the cell culture room and rinsed again with fresh HBSS, the hearts were transferred into a sterile culture dish containing DMEM/F12 (12400–024, Gibco, New York, USA) supplemented with 0.25 mg/ml collagenase typeⅡ (17101–015, Invitrogen, Paisley, Renfrewshire, UK) and 0.01 mM HEPES. The hearts were then minced into 1 mm3 pieces, transferred into 50 mL centrifuge tube, and incubated on an orbital shaker at 37°C for 35 min with the collagenase solution as described above. After 25 mL ice-cold HBSS was added into the digest to inhibit collagenase activity, dispersed cells were separated from non-digested tissues by passing through a 40-μm-diameter cell strainer and collected with centrifugation at 1000 rpm for 5 min at 4°C. After washed once by centrifugation in HBSS, cells were resuspended with 10 mL DMEM/F12 supplemented with 10% fetal bovine serum (FBS, 16000–044, Gibco), 100 U/ml penicillin, and 100 μg/ml streptomycin, and seeded into sterile culture dishes. Cells were then cultured in a humidified atmosphere of 5% CO2 at 37°C for 2 h to purify the cell suspension with TCs by allowing fibroblasts attachment. The unattached cells (containing TCs) were collected and cultured in DMEM/F12 supplemented with 10% FBS, 100 U/ml penicillin, and 100 μg/ml streptomycin for 24 h and culture medium was changed. Cell cultures were examined using inverted biological microscope (BM-37XC, China), and TCs and fibroblasts were photographed under 200× magnification at 48 h, 72 h and 96 h after seeded.
Isolation and primary culture of pericytes from heart tissues
Pericytes were isolated and cultured as previously described [56]. Briefly, mice cardiac tissues freed from atria and upper portions of the ventricles were minced in HBSS, and treated with 0.25% trypsin in DMEM at 37°C for 15 min, followed by digestion in 0.1% collagenase type II, 0.05% deoxyribonuclease, and 25 μM CaCl2 until soft. After DMEM containing 1% BSA and 100μM CaCl2 was added into the digest to inhibit collagenase activity, dispersed cells were separated by 100-μm-diameter cell strainer and collected with centrifugation at 1500 rpm for 5 min at 4°C. After washed with DMEM containing 1% BSA and 500μM CaCl2 and layered over 5ml of DMEM containing 6% BSA, cells were centrifugated at 800 rpm for 10 min to separat a clear upper layer from a darker layer. Cells from the latter were cultured in DMEM/F12 supplemented with 10% FBS, 100 U/ml penicillin, and 100 μg/ml streptomycin.
Isolation and primary culture of bone marrow-derived mesenchymal stem cells (BMSC)
BMSCs were isolated and cultured as our previous described [57]. Briefly, primary BMSCs were harvested from tibias and femurs of 4-week-old Sprague-Dawley rats under aseptic conditions and then purified and passaged in DMEM/F12 supplemented with 10% fetal bovine serum, 100 U/ml penicillin, and 100 μg/ml streptomycin.
Double immunofluorescent staining for CD34/c-kit or vimentin or PDGFR-β or α-SMA in cell cultures
After washed with PBS for three times, cells were fixed in 4% paraformaldehyde for 30 min, washed with PBS, and permeabilized with 0.5% Triton X-100 for 30 min. Cells were then washed with PBS and blocked in 3% bovine serum albumin (BSA) for 1 h. After that, cells were incubated overnight at 4°C with rat monoclonal anti-CD34 (ab8158, Abcam, Cambridge, MA, USA) and rabbit polyclonal anti-c-kit (ab5506, Abcam) primary antibodies diluted by 1:100 in 1% BSA. After washed with PBS for three times, cells were incubated with goat anti-rat FITC-labelled (sc-2011, Santa Cruz, CA, USA) and goat anti-rabbit rhodamine-labelled (E031320, Earthox, San Francisco, CA, USA) secondary antibodies diluted by 1:200 in 3% BSA for 2 h, and then stained with DAPI (F36924, Life technology, Grand Island, NY, USA). Finally, cells were kept in fresh PBS at 4°C in dark before observation. The images were taken under a magnification of 200× with fluorescent inverted microscope (Leica DMI4000 B, Germany). Similar procedures were used for double immunofluorescent staining for CD34/vimentin (rabbit monoclonal anti-vimentin; 2707–1, Epitomics, Burlingame, CA, USA) or CD34/PDGFR-β (rabbit monoclonal anti-PDGFR-β; ab32570, Abcam) or CD34/α-SMA (rabbit polyclonal anti-α-SMA; ab137734, Abcam).
Flow cytometry analysis for cardiac TCs and BMSC
Cells were harvested by trypsinization and washed twice with cold PBS. TCs were stained with allophycocyanin-conjugated anti-mouse CD29 (17–0291, Ebioscence) and CD45 (17–0451, Ebioscence) while Rat-BMSCs were stained with FITC-conjugated anti-rat CD29 (561796, BD biosciences) and CD45 (561867, BD biosciences). As negative controls, cell aliquots were incubated with PBS under the same conditions. After incubation away from light for 30 min at 4°C, cells were analyzed by MoFlo XDP (Beckman Coulter) and FlowJo software (Tree Star).
Results
Different morphological features of cardiac TCs and fibroblasts in primary culture
Cardiac TCs in primary culture were purified from fibroblasts by using differential adhesion method. In the present study, fibroblast attachment occurred within 2 h after seeded, while TC attachment took 24 h. To observe the different morphological features of both cell types, cardiac TCs and fibroblasts were observed under light microscope and photographed at 48 h, 72 h and 96 h from the day of primary culture. As shown in Fig. 1, the prolongations of fibroblasts were relatively short, thick and cone shaped, while those of TCs were extremely long and thin, stretched away from cell bodies. Fig. 2 shows TCs with typical characteristics: small cell body and extremely thin and long telopode, and significant moniliform aspect with many dilations along telopode.
Fig 1. Light microscope shows cardiac telocytes (TCs, A-F) and fibroblasts (FB, G-L) in primary culture from heart tissues at 48 h, 72 h, and 96 h after the day of primary culture.
Arrows show typical TCs with long and thin telopodes in primary culture. Original magnification 200×; Scale bar = 50 μm.
Fig 2. Light microscope shows telocytes (TCs) with typical morphological features.
(A) A TC with small cell body and extremely thin and long telopode (Tp). (B) and (C) A TC with significant moniliform aspect: alternation of podoms-podomeres (enlarged in inset). (D-F) show more TCs with typical morphological features. Original magnification 200×; Scale bar = 50 μm.
Different immunophenotypes of cardiac TCs and fibroblasts in primary culture
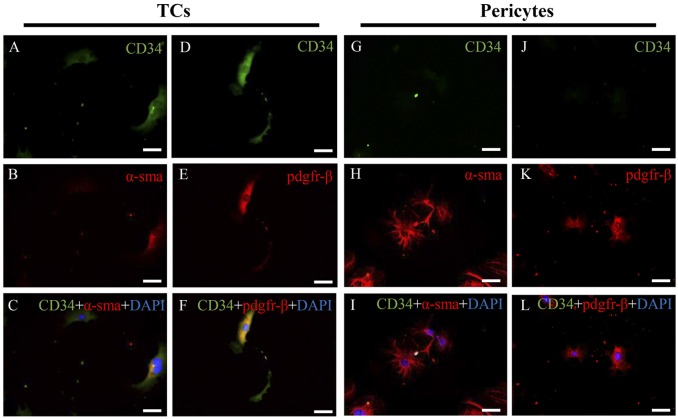
To identify different immunophenotypes of cardiac TCs and fibroblasts, three different double immunofluorescent methods (CD34 and c-kit, CD34 and vimentin, and CD34 and PDGFR-β) were used. As shown in Fig. 3, cardiac TCs were CD34/c-kit, CD34/vimentin and CD34/PDGFR-β positive, while cardiac fibroblasts were only vimentin and PDGFR-β positive, thus clearly demonstrating the different immunophenotypes of cardiac TC and fibroblasts in primary culture. As CD34 negative and vimentin positive cells in the culture may not all be fibroblasts, they could also be pericytes. We stained the fibroblast used in the present study and they were α-SMA negative (data not shown), indicating they were not pericytes. To futher compare the immunophenotypes of cardiac TCs and pericytes, we isolated pericytes and compared different immunophenotypes of cardiac TCs and fibroblasts. As indicated in Fig. 4, TCs were CD34 positive and α-SMA weak positive while pericytes were CD34 negative but α-SMA positive. In addition, TCs were CD34/PDGFR-β positive while pericytes were CD34 negative but PDGFR-β positive. These data indicated that TCs were different from pericytes.
Fig 3. Double immunofluorescent staining for CD34/c-kit, CD34/vimentin and CD34/PDGFR-β of cardiac telocytes (TCs) and fibroblasts (FB) in primary culture.

Fluorescent inverted microscope shows that TCs are positive for (A) CD34 (green) and (B) c-kit (red), while FBs are negative for (J) CD34 (green) and (K) c-kit (red). Co-localization of c-kit and CD34 (yellow) is significant in TCs (C), while absent in FBs (L). TCs are positive for (D) CD34 (green) and (E) vimentin (red). FBs are negative for (M) CD34 (green), but positive for (N) vimentin (red). Co-localization of vimentin and CD34 (yellow) is significant in TCs (F), while absent in FBs (O). TCs are positive for (G) CD34 (green) and (H) PDGFR-β (red). FBs are negative for (P) CD34 (green), but positive for (Q) PDGFR-β (red). Co-localization of PDGFR-β and CD34 (yellow) is significant in TCs (I), while absent in FBs (R). Nuclei are counterstained with DAPI (blue). Original magnification 200×; Scale bar = 50 μm. BF, bright field.
Fig 4. Double immunofluorescent staining for CD34/α-SMA and CD34/PDGFR-β of cardiac telocytes (TCs) and pericytes in primary culture.
Fluorescent inverted microscope shows that TCs are positive for (A) CD34 (green) and relatively weak positive for (B) α-SMA (red), while pericytes are negative for (G) CD34 (green) but strong positive for (H) PDGFR-β (red). Co-localization of α-SMA and CD34 (yellow) is extremely weak in TCs (C), while absent in pericytes (I). TCs are positive for (D) CD34 (green) and (E) PDGFR-β (red), while pericytes are negative for (J) CD34 (green), but positive for (K) PDGFR-β (red). Co-localization of PDGFR-β and CD34 (yellow) was significant in TCs (F), while absent in pericytes (L). Nuclei were counterstained with DAPI (blue). Original magnification 200×; Scale bar = 50 μm. BF, bright field.
Cell surface markers of cardiac telocytes (TCs) and BMSC
As shown in Fig. 5, flow cytometry analysis showed that cardiac TCs were homogenously positive for mesenchymal marker CD29 but negative for hematopoietic marker CD45, which is similar to BMSC. These data indicate that TCs could be a source of cardiac mesenchymal cells, supporting that and they might hold the potential to give rise to MSCs in culture.
Fig 5. Cell surface markers of cardiac telocytes (TCs) and bone marrow-derived mesenchymal stem cells (BMSC).
Cells collected are shown in A and D. Flow cytometry analysis show that cardiac TCs are homogenously positive for mesenchymal marker CD 29 (B) as BMSC (E), but negative for hematopoietic marker CD45 (C) as BMSC (F). Unlabeled cell (black) controls are included for comparison. FSC: forward scatter; SSC,side scatter.
Discussion
Cardiac TC and fibroblasts were isolated from heart tissues and their different morphological features were observed in primary culture. Meanwhile, we provided further evidence showing that cardiac TCs were positive for CD34/c-kit, CD34/vimentin, and CD34/PDGFR-β, while fibroblasts were only positive for vimentin and PDGFR-β, which clearly differentiated cardiac TCs from fibroblasts in primary culture.
Isolation and culture of TCs from a given organ is of great interest to study the peculiar morphological features and functionality of TCs [6,9–11,29,30,32,33,58]. TCs and fibroblasts, both located in the interstitium spaces, have different morphologies and functions [51]. Fibroblasts are mainly responsible for the production of collagen and some other extracellular matrix, whereas TCs are more functionally involved in intercellular communication via 3D network [51]. However, some cells labelled with “fibroblasts” or “fibroblast-like cells” in the literature are actually not real fibroblasts [48]. Thus, it is highly needed to discriminate between TCs and fibroblasts in virtual research. In the present study, we purified cardiac TCs from fibroblasts according to their different attachment time in primary culture. Actually, fibroblasts attached to culture dishes in less than 2 h after seeded, while cardiac TC attachment took much longer (2–24 h). When observed at 48 h, 72 h, and 96 h of primary culture, cell processes of fibroblasts were short, thick and cone shaped. While TCs extended very long and thin telopodes from cell bodies from 48 h of primary culture, coordinating with previous study [30]. Noteworthy, the alternation podoms-podomeres along telopodes clearly showed another typical morphological features of TCs.
Double immunolabeling is of great importance to make differential diagnosis of TCs from other cells in primary cultures or tissues [2,13,59]. In the present study, we performed double immunofluorescent staining for CD34/c-kit, CD34/vimentin, and CD34/PDGFR-β, which showed that cardiac TCs were positive for CD34, c-kit, vimentin and PDGFR-β, whereas fibroblasts were only positive for vimentin and PDGFR-β. Interestingly, similar to previous reports that not all TCs were CD34 and c-kit double positive [60], in TCs we isolated here, the proportion of CD34/c-kit double positive was 68.9%. It has previously been shown that pre-plating to remove fibroblasts from primary culture is not sufficient to completely clear fibroblasts, and that fibroblasts in primary culture express strongly vimentin but no CD34 [13,29]. However, immunolabeling for CD34 in combination with c-kit or vimentin still remains the best available approach to identify TCs from other cells [48]. In addition, PDGFR-β was also found positively expressed by TCs in heart valve, lung, skeletal muscle and liver samples [12,28,40,61,62]. The fibroblasts we isolated here were α-SMA negative, excluding the possibility of pericytes. Besides that, we also futher compared the immunophenotypes of TCs and pericytes. We found that TCs were CD34 positive and α-SMA weak positive while pericytes were CD34 negative but α-SMA positive, indicating that TCs were also different from pericytes. Anyway, the different immunophenotypes of cardiac TCs and fibroblasts by using double immunolabeling for CD34/c-kit, CD34/vimentin, and CD34/PDGFR-β, provides more compelling evidence to discriminate between cardiac TCs and fibroblasts.
It has been indicated that TCs could be a source of cardiac mesenchymal cells [63]. To address this point, using flow cytometry analysis, we showed that TCs were homogenously positive for mesenchymal marker CD29 but negative for hematopoietic marker CD45, which is similar to BMSC, supporting that they might hold the potential to give rise to MSCs in culture. In addition, as CD34+ cells may lose CD34 expression and acquire other marker expressions “in vivo” and “in vitro” [63], further studies over a longer period of culture to investigate whether the phenotype of the CD34+ cardiac TCs follows this behaviour.
In conclusion, the present study shows the different morphological features and immunophenotypes between cardiac TCs and fibroblasts in primary culture. Our results present here, as well as the comparison of gene profiles, microRNAs signatures and proteome features of these two cell types highly desirable to be determined in the future, will provide new lines of evidence to differentiate TCs from fibroblasts in heart tissues.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the grants from National Natural Science Foundation of China (81200169 to J. Xiao), Innovation Program of Shanghai Municipal Education Commission (13YZ014 to J. Xiao), Foundation for University Young Teachers by Shanghai Municipal Education Commission (year 2012, to J. Xiao), Innovation fund from Shanghai University (sdcx2012038 to J. Xiao), and Program for the integration of production, teaching and research for University Teachers supported by Shanghai Municipal Education Commission (year 2014, to J. Xiao).
References
- 1. Popescu LM, Faussone-Pellegrini M-S (2010) TELOCYTES—a case of serendipity: the winding way from Interstitial Cells of Cajal (ICC), via Interstitial Cajal-Like Cells (ICLC) to TELOCYTES. J Cell Mol Med 14:729–740. 10.1111/j.1582-4934.2010.01059.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Popescu LM, Manole CG, Gherghiceanu M, Ardelean A, Nicolescu MI, et al. (2010) Telocytes in human epicardium. J Cell Mol Med 14:2085–2093. 10.1111/j.1582-4934.2010.01129.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gherghiceanu M, Manole CG, Popescu LM (2010) Telocytes in endocardium: electron microscope evidence. J Cell Mol Med 14:2330–2334. 10.1111/j.1582-4934.2010.01133.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hinescu ME, Gherghiceanu M, Suciu L, Popescu LM (2011) Telocytes in pleura: two- and three-dimensional imaging by transmission electron microscopy. Cell Tissue Res 343:389–397. 10.1007/s00441-010-1095-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rusu MC, Jianu AM, Mirancea N, Didilescu AC, Mănoiu VS, et al. (2012) Tracheal telocytes. J Cell Mol Med 16:401–405. 10.1111/j.1582-4934.2011.01465.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zheng Y, Zhu T, Lin M, Wu D, Wang X (2012) Telocytes in the urinary system. J Transl Med 10:188 10.1186/1479-5876-10-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rusu MC, Mirancea N, Mănoiu VS, Vâlcu M, Nicolescu MI, et al. (2012) Skin telocytes. Ann Anat Anat Anz Off Organ Anat Ges 194:359–367. [DOI] [PubMed] [Google Scholar]
- 8. Chen X, Zheng Y, Manole CG, Wang X, Wang Q (2013) Telocytes in human oesophagus. J Cell Mol Med 17:1506–1512. 10.1111/jcmm.12149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zheng Y, Li H, Manole CG, Sun A, Ge J, et al. (2011) Telocytes in trachea and lungs. J Cell Mol Med 15:2262–2268. 10.1111/j.1582-4934.2011.01404.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Popescu LM, Manole E, Serboiu CS, Manole CG, Suciu LC, et al. (2011) Identification of telocytes in skeletal muscle interstitium: implication for muscle regeneration. J Cell Mol Med 15:1379–1392. 10.1111/j.1582-4934.2011.01330.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Qi G, Lin M, Xu M, Manole CG, Wang X, et al. (2012) Telocytes in the human kidney cortex. J Cell Mol Med 16:3116–3122. 10.1111/j.1582-4934.2012.01582.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xiao J, Wang F, Liu Z, Yang C (2013) Telocytes in liver: electron microscopic and immunofluorescent evidence. J Cell Mol Med 17:1537–1542. 10.1111/jcmm.12195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Suciu L, Popescu LM, Gherghiceanu M, Regalia T, Nicolescu MI, et al. (2010) Telocytes in human term placenta: morphology and phenotype. Cells Tissues Organs 192:325–339. 10.1159/000319467 [DOI] [PubMed] [Google Scholar]
- 14. Popescu BO, Gherghiceanu M, Kostin S, Ceafalan L, Popescu LM (2012) Telocytes in meninges and choroid plexus. Neurosci Lett 516:265–269. 10.1016/j.neulet.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 15. Cantarero Carmona I, Luesma Bartolomé MJ, Junquera Escribano C (2011) Identification of telocytes in the lamina propria of rat duodenum: transmission electron microscopy. J Cell Mol Med 15:26–30. 10.1111/j.1582-4934.2010.01207.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nicolescu MI, Popescu LM (2012) Telocytes in the interstitium of human exocrine pancreas: ultrastructural evidence. Pancreas 41:949–956. 10.1097/MPA.0b013e31823fbded [DOI] [PubMed] [Google Scholar]
- 17. Nicolescu MI, Bucur A, Dinca O, Rusu MC, Popescu LM (2012) Telocytes in parotid glands. Anat Rec Hoboken NJ 295:378–385. 10.1002/ar.21540 [DOI] [PubMed] [Google Scholar]
- 18. Corradi LS, Jesus MM, Fochi RA, Vilamaior PSL, Justulin LA Jr, et al. (2013) Structural and ultrastructural evidence for telocytes in prostate stroma. J Cell Mol Med 17:398–406. 10.1111/jcmm.12021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Luesma MJ, Gherghiceanu M, Popescu LM (2013) Telocytes and stem cells in limbus and uvea of mouse eye. J Cell Mol Med 17:1016–1024. 10.1111/jcmm.12111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kostin S (2010) Myocardial telocytes: a specific new cellular entity. J Cell Mol Med 14:1917–1921. 10.1111/j.1582-4934.2010.01111.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cantarero I, Luesma MJ, Junquera C (2011) The primary cilium of telocytes in the vasculature: electron microscope imaging. J Cell Mol Med 15:2594–2600. 10.1111/j.1582-4934.2011.01312.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li H, Lu S, Liu H, Ge J, Zhang H (2014) Scanning electron microscope evidence of telocytes in vasculature. J Cell Mol Med 18:975–978. 10.1111/jcmm.12337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rusu MC, Nicolescu MI, Jianu AM, Lighezan R, Mănoiu VS, et al. (2012) Esophageal telocytes and hybrid morphologies. Cell Biol Int 36:1079–1088. 10.1042/CBI20120007 [DOI] [PubMed] [Google Scholar]
- 24. Cretoiu D, Cretoiu SM, Simionescu AA, Popescu LM (2012) Telocytes, a distinct type of cell among the stromal cells present in the lamina propria of jejunum. Histol Histopathol 27:1067–1078. [DOI] [PubMed] [Google Scholar]
- 25. Rusu MC, Pop F, Hostiuc S, Dermengiu D, Lală AI, et al. (2011) The human trigeminal ganglion: c-kit positive neurons and interstitial cells. Ann Anat Anat Anz Off Organ Anat Ges 193:403–411. 10.1016/j.aanat.2011.06.005 [DOI] [PubMed] [Google Scholar]
- 26. Bosco C, Díaz E, Gutiérrez R, González J, Pérez J (2013) Ganglionar nervous cells and telocytes in the pancreas of Octodon degus: extra and intrapancreatic ganglionar cells and telocytes in the degus. Auton Neurosci Basic Clin 177:224–230. 10.1016/j.autneu.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 27. Faussone-Pellegrini M- S, Bani D (2010) Relationships between telocytes and cardiomyocytes during pre- and post-natal life. J Cell Mol Med 14:1061–1063. 10.1111/j.1582-4934.2010.01074.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang Y, Sun W, Wu SM, Xiao J, Kong X (2014) Telocytes in human heart valves. J Cell Mol Med 18:759–765. 10.1111/jcmm.12285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhou J, Zhang Y, Wen X, Cao J, Li D, et al. (2010) Telocytes accompanying cardiomyocyte in primary culture: two- and three-dimensional culture environment. J Cell Mol Med 14:2641–2645. 10.1111/j.1582-4934.2010.01186.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Suciu L, Nicolescu MI, Popescu LM (2010) Cardiac telocytes: serial dynamic images in cell culture. J Cell Mol Med 14:2687–2692. 10.1111/j.1582-4934.2010.01185.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Popescu LM, Gherghiceanu M, Suciu LC, Manole CG, Hinescu ME (2011) Telocytes and putative stem cells in the lungs: electron microscopy, electron tomography and laser scanning microscopy. Cell Tissue Res 345:391–403. 10.1007/s00441-011-1229-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bojin FM, Gavriliuc OI, Cristea MI, Tanasie G, Tatu CS, et al. (2011) Telocytes within human skeletal muscle stem cell niche. J Cell Mol Med 15:2269–2272. 10.1111/j.1582-4934.2011.01386.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hatta K, Huang M-L, Weisel RD, Li R-K (2012) Culture of rat endometrial telocytes. J Cell Mol Med 16:1392–1396. 10.1111/j.1582-4934.2012.01583.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ceafalan L, Gherghiceanu M, Popescu LM, Simionescu O (2012) Telocytes in human skin—are they involved in skin regeneration? J Cell Mol Med 16:1405–1420. 10.1111/j.1582-4934.2012.01580.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gherghiceanu M, Popescu LM (2012) Cardiac telocytes—their junctions and functional implications. Cell Tissue Res 348:265–279. 10.1007/s00441-012-1333-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gherghiceanu M, Popescu LM (2010) Cardiomyocyte precursors and telocytes in epicardial stem cell niche: electron microscope images. J Cell Mol Med 14:871–877. 10.1111/j.1582-4934.2010.01060.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gherghiceanu M, Popescu LM (2011) Heterocellular communication in the heart: electron tomography of telocyte-myocyte junctions. J Cell Mol Med 15: 1005–1011. 10.1111/j.1582-4934.2011.01299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bani D, Formigli L, Gherghiceanu M, Faussone-Pellegrini M- S (2010) Telocytes as supporting cells for myocardial tissue organization in developing and adult heart. J Cell Mol Med 14:2531–2538. 10.1111/j.1582-4934.2010.01119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Edelstein L, Smythies J (2014) The role of telocytes in morphogenetic bioelectrical signaling: once more unto the breach. Front Mol Neurosci 7:41 10.3389/fnmol.2014.00041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Suciu LC, Popescu BO, Kostin S, Popescu LM (2012) Platelet-derived growth factor receptor-β-positive telocytes in skeletal muscle interstitium. J Cell Mol Med 16:701–707. 10.1111/j.1582-4934.2011.01505.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Campeanu R-A, Radu BM, Cretoiu SM, Banciu DD, Banciu A, et al. (2014) Near-infrared low-level laser stimulation of telocytes from human myometrium. Lasers Med Sci 29: 1867–1874. 10.1007/s10103-014-1589-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Manetti M, Rosa I, Messerini L, Guiducci S, Matucci-Cerinic M, et al. (2014) A loss of telocytes accompanies fibrosis of multiple organs in systemic sclerosis. J Cell Mol Med 18:253–262. 10.1111/jcmm.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Manetti M, Guiducci S, Ruffo M, Rosa I, Faussone-Pellegrini MS, et al. (2013) Evidence for progressive reduction and loss of telocytes in the dermal cellular network of systemic sclerosis. J Cell Mol Med 17:482–496. 10.1111/jcmm.12028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li L, Lin M, Li L, Wang R, Zhang C, et al. (2014) Renal telocytes contribute to the repair of ischemically injured renal tubules. J Cell Mol Med 18:1144–1156. 10.1111/jcmm.12274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Manole CG, Cismaşiu V, Gherghiceanu M, Popescu LM (2011) Experimental acute myocardial infarction: telocytes involvement in neo-angiogenesis. J Cell Mol Med 15:2284–2296. 10.1111/j.1582-4934.2011.01449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhao B, Liao Z, Chen S, Yuan Z, Yilin C, et al. (2014) Intramyocardial transplantation of cardiac telocytes decreases myocardial infarction and improves post-infarcted cardiac function in rats. J Cell Mol Med 18:780–789. 10.1111/jcmm.12259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zhao B, Chen S, Liu J, Yuan Z, Qi X, et al. (2013) Cardiac telocytes were decreased during myocardial infarction and their therapeutic effects for ischaemic heart in rat. J Cell Mol Med 17:123–133. 10.1111/j.1582-4934.2012.01655.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pellegrini M-SF, Popescu LM (2011) Telocytes. Biomol Concepts 2:481–489. [DOI] [PubMed] [Google Scholar]
- 49. Milia AF, Ruffo M, Manetti M, Rosa I, Conte D, et al. (2013) Telocytes in Crohn’s disease. J Cell Mol Med 17:1525–1536. 10.1111/jcmm.12177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vannucchi M-G, Traini C, Manetti M, Ibba-Manneschi L, Faussone-Pellegrini M-S (2013) Telocytes express PDGFRα in the human gastrointestinal tract. J Cell Mol Med 17:1099–1108. 10.1111/jcmm.12134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Popescu LM, Nicolescu MI (2013) Telocytes and Stem Cells In: Goldenberg RC dos S, Carvalho ACC de, editors. Resid. Stem Cells Regen. Ther., Academic Press; pp. 205–231. [Google Scholar]
- 52. Zheng Y, Zhang M, Qian M, Wang L, Cismasiu VB, et al. (2013) Genetic comparison of mouse lung telocytes with mesenchymal stem cells and fibroblasts. J Cell Mol Med 17:567–577. 10.1111/jcmm.12052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sun X, Zheng M, Zhang M, Qian M, Zheng Y, et al. (2014) Differences in the expression of chromosome 1 genes between lung telocytes and other cells: mesenchymal stem cells, fibroblasts, alveolar type II cells, airway epithelial cells and lymphocytes. J Cell Mol Med 18:801–810. 10.1111/jcmm.12302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Cismasiu VB, Radu E, Popescu LM (2011) miR-193 expression differentiates telocytes from other stromal cells. J Cell Mol Med 15:1071–1074. 10.1111/j.1582-4934.2011.01325.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zheng Y, Cretoiu D, Yan G, Cretoiu SM, Popescu LM, et al. (2014) Comparative proteomic analysis of human lung telocytes with fibroblasts. J Cell Mol Med 18:568–589. 10.1111/jcmm.12290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. He Q, Spiro MJ. (1995) Isolation of rat heart endothelial cells and pericytes: evaluation of their role in the formation of extracellular matrix components. J Mol Cell Cardiol 27: 1173–1183. [DOI] [PubMed] [Google Scholar]
- 57. Chen L, Cui X, Wu Z, Yia L, Yu Y, et al. (2014) Transplantation of bone marrow mesenchymal stem cells pretreated with valproic acid in rats with an acute spinal cord injury. Biosci Trends 8: 111–119. [DOI] [PubMed] [Google Scholar]
- 58. Cretoiu SM, Cretoiu D, Marin A, Radu BM, Popescu LM (2013) Telocytes: ultrastructural, immunohistochemical and electrophysiological characteristics in human myometrium. Reprod Camb Engl 145:357–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhou Y, Pan P, Yao L, Su M, He P, et al. (2010) CD117-positive cells of the heart: progenitor cells or mast cells? J Histochem Cytochem Off J Histochem Soc 58:309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kostin S, Popescu LM. (2009) A distinct type of cell in myocardium: interstitial Cajal-like cells (ICLCs). J Cell Mol Med 13: 295–308. 10.1111/j.1582-4934.2008.00668.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Galiger C, Kostin S, Golec A, Ahlbrecht K, Becker S, et al. (2014) Phenotypical and ultrastructural features of Oct4-positive cells in the adult mouse lung. J Cell Mol Med 18: 1321–1333. 10.1111/jcmm.12295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang F, Song Y, Bei Y, Zhao Y, Xiao J, et al. (2014) Telocytes in liver regeneration: possible roles. J Cell Mol Med 18: 1720–1726. 10.1111/jcmm.12355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Díaz-Flores L, Gutiérrez R, García MP, Sáez FJ, Díaz-Flores L Jr, et al. (2014) CD34+ stromal cells/fibroblasts/fibrocytes/telocytes as a tissue reserve and a principal source of mesenchymal cells. Location, morphology, function and role in pathology. Histol Histopathol 29: 831–870. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.