Abstract
Background
Surgical enucleation is the treatment of choice for esophageal submucosal tumors (SMTs) with symptomatic, larger, or ill-defined lesions. The enucleation of SMTs has traditionally been performed via thoracotomy. However, minimally invasive approaches have recently been introduced and successfully applied. In this study, we present our experiences with the thoracotomic and thoracoscopic approaches to treating SMTs.
Methods
We retrospectively reviewed 53 patients with SMTs who underwent surgical enucleation between August 1996 and July 2013. Demographic and clinical features, tumor-related factors, the surgical approach, and outcomes were analyzed.
Results
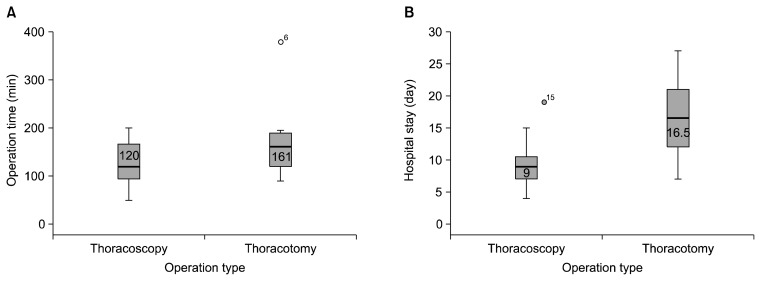
There were 36 males (67.9%) and 17 females (32.1%); the mean age was 49.2±11.8 years (range, 16 to 79 years). Histology revealed leiomyoma in 51 patients, a gastrointestinal stromal tumor in one patient, and schwannoma in one patient. Eighteen patients (34.0%) were symptomatic. Fourteen patients underwent a planned thoracotomic enucleation. Of the 39 patients for whom a thoracoscopic approach was planned, six patients required conversion to thoracotomy because of overly small tumors or poor visualization in five patients and accidental mucosal injury in one patient. No mortality or major postoperative complications occurred. Compared to thoracotomy, the thoracoscopic approach had a slightly shorter operation time, but this difference was not statistically significant (120.0±45.6 minutes vs. 161.5±71.1 minutes, p=0.08). A significant difference was found in the length of the hospital stay (9.0±3.2 days vs. 16.5±5.4 days, p<0.001).
Conclusion
The thoracoscopic enucleation of submucosal esophageal tumors is safe and is associated with a shorter length of hospital stay compared to thoracotomic approaches.
Keywords: Esophagus, surgery; Enucleation; Submucosal tumors of the esophagus; Thoracoscopy
INTRODUCTION
Esophageal submucosal tumors (SMTs) are rare, representing less than 1% of all esophageal tumors and showing a very heterogeneous composition. Leiomyoma is the most common benign esophageal tumor and accounts for 70% to 80% of esophageal SMTs. In contrast, gastrointestinal stromal tumors are less common in the esophagus than in the stomach [1,2]. Such lesions are mostly asymptomatic and are found incidentally in the course of upper gastrointestinal endoscopy. Although chest computed tomography and endoscopic ultrasonography (EUS) are performed as additional diagnostic tests, they have limitations in distinguishing various subtypes of esophageal SMTs. Ultimately, a definitive diagnosis is determined postoperatively through histopathological and immunohistochemical examinations [3]. Indications for thoracoscopic enucleation have not been established. Surgical therapy is usually indicated for patients with the presence of symptoms, a larger tumor size (>3 cm), and the need to obtain a pathological diagnosis to exclude malignancy [4].
Conventionally, the standard approach has been to perform enucleation through a thoracotomy. However, minimally invasive surgery using thoracoscopy and laparoscopy has recently been successfully applied and widely used. Few series of the thoracoscopic enucleation of esophageal SMTs have yet been reported, and therefore we investigated the results of the surgical enucleation of esophageal SMTs in our hospital and conducted a comparative analysis by dividing these cases into a thoracotomy group and a thoracoscopy group.
METHODS
From August 1996 to July 2013, 53 consecutive patients who underwent surgical enucleation of esophageal SMTs at the Chonnam National University Hospital were selected, and a retrospective analysis was conducted based on their medical records. Patients suspected to have SMTs based on the results of esophagoscopy (48 patients) or chest computed tomography (5 patients), performed either as part of a routine health screening or to evaluate gastrointestinal symptoms, were referred to our outpatient clinic. EUS was performed in 40 patients to characterize the SMTs. With the exception of early-stage patients, chest computed tomography was performed preoperatively on all patients to identify the tumor location and relationship with surrounding structures.
The main indications for the surgical enucleation of esophageal SMTs were the presence of tumor-related symptoms, tumors greater than 3 cm, evidence of an increase in tumor size, and the need to obtain a pathologic diagnosis to exclude malignancy. The surgical approach was determined based on the location and size of the tumors. In most patients, a right-side approach was chosen, except for two patients in whom a left-side approach was used to treat tumors located at the esophagogastric junction. A double-lumen endotracheal tube was inserted into all patients, and all surgeries were performed with the patient in the lateral decubitus position.
Since thoracoscopy was first introduced in our institution in 2006 for the enucleation of esophageal SMTs, it has been successfully applied and usually approached using four ports (two 5 mm ports and two 11 mm ports). After localization of the tumor, the mediastinal pleura were dissected, and a myotomy was performed at the level of the tumor. The tumor was carefully enucleated to preserve the vagal branches and to prevent mucosal damage. The muscular layer was closed with interrupted absorbable sutures. In case of suspected mucosal damage during enucleation or difficulty in identifying the location of the tumor, intraoperative esophagoscopy was performed to confirm mucosal integrity or to localize the tumor.
A postoperative esophagogram was usually performed on postoperative day three to five depending on the patient’s recovery status. The thoracic tube was removed once no abnormalities were found after enteral feeding. The length of hospital stay was defined as the number of days from surgery to discharge.
Descriptive data were expressed as mean±standard deviation for continuous variables with a normal distribution, and as median±standard deviation for non-normally distributed variables, while numbers and percentages were used for categorical variables. The chi-square test was used to compare categorical variables and the Student t-test or the Mann-Whitney U-test was used to compare differences between the two groups. p-values less than 0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA).
RESULTS
There were 36 males (67.9%) and 17 females (32.1%), with a mean age of 49.2 years (range, 16 to 79 years). Of these patients, 35 (66.0%) were asymptomatic and most of their tumors were detected incidentally during health screening examinations. Eighteen patients (34.0%) had tumor-related symptoms. Epigastric discomfort (n=5) was the most common symptom, followed by dysphagia (n=4), chest pain (n=4), dyspepsia (n=1), vomiting (n=1), and nonspecific gastrointestinal discomfort (n=3). The tumor was located in the upper thoracic esophagus in 18 patients, the middle thoracic esophagus in 21 patients, and the lower thoracic esophagus in 14 patients. The mean tumor size was 3.25±1.49 cm (range, 1 to 7 cm). The indications for surgical enucleation were a tumor greater than 3 cm or with increasing size in 17 patients, the presence of tumor-related symptoms in 18 patients, and the need to obtain a pathologic diagnosis in 17 patients. In one patient, an incidentally detected SMT was enucleated during a planned operation for esophageal achalasia.
Surgeries were mainly performed through a right-side approach, with the exception of two patients with tumors located at the esophagogastric junction and deviating to the left side of the esophagus. A planned thoracotomy was performed in 14 patients, and a thoracoscopy was performed in 39 patients. After 2006, when thoracoscopy was introduced in our institution for the enucleation of esophageal SMTs, a thoracoscopic approach was initially used on all patients, except for one patient with a 5 cm tumor that had unclear boundaries with the adjacent azygos vein and the descending thoracic aorta. Intraoperative esophagoscopy was performed in seven patients. In five cases, intraoperative esophagoscopy was performed to confirm the mucosal integrity, and in two cases to identify the location of a small tumor. There was no mucosal damage in the five patients who underwent intra-operative esophagoscopy due to suspicion of mucosal tearing. Mucosal injury occurred in only one patient, which was discovered in the course of thoracoscopic enucleation due to a large tumor (6 cm) with intensive adhesion to the mucosa. A primary repair was performed with conversion to a thoracotomy. Six patients (15.4%) required conversion to a thoracotomy during thoracoscopy. Of the six conversions, three were due to poor surgical visibility resulting from a pleural adhesion and a marked deviation of the esophagus to the left, two were due to difficulty in localizing very small tumors, and one was due to a mucosal injury, as mentioned above.
Histopathological examination identified 51 cases of leiomyoma, one case of a gastrointestinal stromal tumor, and one case of schwannoma. We determined that enucleation was sufficient treatment for the gastrointestinal stromal tumor because it was low-risk based on the mitotic index (less than five mitotic figures noted per 50 high-power fields), and there was no recurrence during a one-year follow-up period. There were no postoperative leakages or other major complications. There was also no perioperative mortality. The mean length of the hospital stay was 10.9±5.1 days (range, 4 to 27 days).
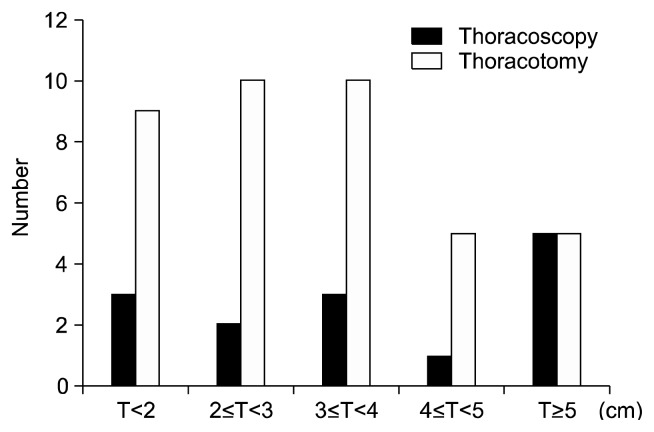
The results of a comparative analysis evaluating the effect of the surgical approach are presented in Table 1. There was no significant difference in age, gender ratio, tumor size, or presence of symptoms between the thoracotomy and thoracoscopy groups. The mean operation time was slightly shorter in the thoracoscopy group (120.0±45.6 minutes) compared the to thoracotomy group (161.5±71.1 minutes), but the difference was not statistically significant (p=0.08). The mean length of the hospital stay was significantly shorter in the thoracoscopy group (9.0±3.2 days vs. 16.5±5.4 days, p<0.001) (Fig. 1). The distribution of tumor size according to the surgical approach indicated that tumor size was not an inherent surgical limitation for thoracoscopic enucleation (Fig. 2). Tumors 5 cm or larger were enucleated successfully through the thoracoscopic approach in 4 patients (tumor size range, 5.0 to 5.8 cm), although one patient required conversion to thoracotomy because the tumor was too large (6 cm) and a mucosal injury had developed during enucleation.
Table 1.
Comparisons between thoracotomy and thoracoscopy
| Factors | Thoracotomy (n=14) | Thoracoscopy (n=39) | p-value |
|---|---|---|---|
| Age (yr)a) | 53.3±13.4 | 47.7±10.9 | 0.132 |
| Male:female (%) | 11 (78.6):3 (21.4) | 25 (64.1):14 (35.9) | 0.320 |
| Symptomatic (%) | 7 (50) | 11 (28.2) | 0.140 |
| Size (cm)b) | 3.65±1.8 | 3.0±1.4 | 0.312 |
| Operation time (min)b) | 161.5±71.1 | 120.0±45.6 | 0.080 |
| Hospital stay (day)b) | 16.5±5.4 | 9.0±3.2 | <0.001 |
Mean±standard deviation.
Median±standard deviation.
Fig. 1.
A graph showing the distribution of operation time and hospital stay for the thoracoscopy and thoracotomy groups. (A) The median operation time (min): 120.0±45.6 vs. 161.5±71.1, p=0.080. (B) The median length of hospital stay (day): 9.0±3.2 vs. 16.5±5.4, p<0.001.
Fig. 2.
Tumor size and distribution in the thoracoscopy and thoracotomy groups. T, tumor size.
DISCUSSION
Esophageal SMTs occur rarely, representing less than 1% of all esophageal tumors, and their composition is histologically heterogeneous. Even though they can cause symptoms such as dyspepsia, epigastric discomfort, and pain, they are frequently discovered incidentally without related symptoms. According to the results of the surgical enucleation of SMTs in 87 patients reported by Shin et al. [5], 66.7% of cases were asymptomatic and patients with symptoms had a significantly larger tumor size than asymptomatic patients. The definitive diagnosis of SMTs can only be made through a postoperative histological examination. Bonavina et al. [6] recommended against performing a preoperative endoscopic biopsy of the lesion. This is because endoscopic biopsy can lead to mucosal damage or inflammation, both of which increase the possibility of mucosal perforation during surgical enucleation. However, some recent reports have evaluated the use of esophagoscopy as a less invasive approach for enucleation using esophagoscopy. Guo et al. [7] reported their experience performing endoscopic enucleation on submucosal tumors smaller than 12 mm in 47 patients, and concluded that endoscopic enucleation facilitates the localized treatment of small SMTs with relatively few complications and is advantageous for histological diagnosis. We do not routinely perform endoscopic biopsies if submucosal tumors show benign patterns in computed tomography and EUS. However, in many cases, precisely differentiating between benign and malignant tumors through EUS can be difficult [8], and therefore endoscopic biopsies have been reported in the literature in cases where the morphologic appearance of a tumor does not exclude malignancy with a high probability. In this situation, the surgical enucleation of the tumor is usually postponed for two weeks in order to allow the mucosa to heal.
Esophageal SMTs can be treated with regular monitoring or surgery depending on the tumor size, location, morphology, and the presence of symptoms. Surgical treatment for asymptomatic patients remains controversial. Some authors have recommended regular monitoring for asymptomatic patients who show a small lesion with a benign pattern on EUS. However, surgical treatment has generally been embraced as the treatment of choice for SMTs, and many experts emphasize the necessity of surgery for the following reasons: (1) the possibility of a malignant or symptomatic transformation, (2) the need for a confirmatory histological diagnosis, and (3) the ability to exclude malignancy only by removal. There is also a consensus that enucleation is sufficient treatment for esophageal SMTs. Nonetheless, esophagectomy and reconstruction may be required for malignant gastrointestinal stromal tumors [9].
Surgical enucleation has traditionally been performed through thoracotomy, but minimally invasive surgery has become increasingly common since Everitt et al. [10] introduced thoracoscopic enucleation for the first time in 1992.
In most previous reports, thoracoscopic enucleation has been performed in the lateral decubitus position to anticipate possible conversion to a thoracotomy. Many reports have recently investigated the prone position during minimally invasive esophagectomy for esophageal carcinoma, focusing on how it may contribute to suitable surgical visibility and the reduction of postoperative complications. Claus et al. [11] reported the successful thoracoscopic enucleation of esophageal leiomyoma in the prone position with single-lumen endotracheal intubation in 10 patients, without any conversions [11]. We have also performed esophagectomy through a right thoracoscopy in the prone position, followed by laparoscopy and left cervicotomy in the supine position to treat upper thoracic esophageal carcinoma. However, the thoracoscopic enucleation of SMTs in our hospital is routinely performed in the lateral decubitus position because it is easy to convert to a thoracotomy if necessary.
Von Rahden et al. [4] conducted a comparative analysis of 12 cases of open thoracotomy and 133 cases in which a minimally invasive approach was employed. Their results were not subjected to a statistical analysis, but showed that the minimally invasive approach reduced pulmonary complications, duration of hospitalization, and postoperative pain compared to open surgery. Kent et al. [12] reported that minimally invasive resections of benign esophageal tumors were associated with a shorter length of stay compared to open approaches, and that the minimally invasive technique was technically safe although two patients required the repair of a mucosal injury during resection. Our study showed that minimally invasive surgery using thoracoscopy resulted in a significantly shorter hospital stay compared to open thoracotomy and a shorter operation time, although the latter finding was not statistically significant.
Several factors should be considered during minimally invasive surgery for esophageal SMTs. First, it can be difficult to identify the location of the tumor because a SMT cannot be directly palpated during thoracoscopy, unlike during thoracotomy. Second, there is the possibility of mucosal injury. Choi et al. [13] analyzed surgical outcomes by comparing the thoracotomic and thoracoscopic approaches for esophageal leiomyoma and concluded that the thoracoscopic approach should be considered the standard surgical method. They also suggested that regular monitoring should be considered in asymptomatic patients with tumors smaller than 1.5 cm, based on the high rate of conversion to thoracotomy found in their study (3 of 4 patients, 75%) and the difficulties found in localizing the tumor. However, tumor size itself has not been a contraindication for thoracoscopic enucleation in the case of large tumors if the surgeon has sufficient experience in thoracoscopic surgery. Jiang et al. [14] reported that thoracoscopic enucleation was the best choice for managing esophageal leiomyoma with diameters of 1 to 5 cm, whereas tumors larger than 5 cm can still be enucleated by thoracoscopy, although the likelihood of conversion to a thoracotomy increased along with the tumor’s size. In our study, thoracoscopic enucleation was attempted in five patients with tumors 5 cm or larger, and we successfully performed enucleation by thoracoscopy in four cases, while one case was converted to thoracotomy due to mucosal injury. Jeon et al. [15] reported that esophagoscopy was performed during thoracoscopic enucleation in all of the 17 patients with benign esophageal SMTs that were included in their study, and suggested that intraoperative esophagoscopy may be helpful in identifying the location of a tumor and in determining a suitable direction for the esophageal access incision. In our study, intraoperative esophagoscopy was not routinely performed in all patients, but was performed in seven patients for tumor localization and confirmation of mucosal integrity. Intraoperative esophagoscopy could enhance the accuracy and safety of the thoracoscopic enucleation of esophageal SMTs, despite being a time-consuming procedure.
Our study has some relevant limitations. First, this was a retrospective analysis based on medical records over a relatively long period. Second, we mostly employed the thoracotomic approach in the early period included in the study, whereas thoracoscopic enucleation has been the preferred approach since 2006. Therefore, accumulated surgical experience might have affected the results of this study.
In conclusion, the thoracoscopic enucleation of esophageal SMTs is a safe and feasible approach and is associated with a shorter hospital stay. Technical difficulties that may occur in the thoracoscopic procedure can be addressed by intraoperative esophagoscopy. The thoracoscopic approach is recommended as the standard procedure to treat esophageal SMTs in experienced centers.
ACKNOWLEDGMENTS
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund No. KTCS04-017).
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Seremetis MG, Lyons WS, deGuzman VC, Peabody JW., Jr Leiomyomata of the esophagus: an analysis of 838 cases. Cancer. 1976;38:2166–77. doi: 10.1002/1097-0142(197611)38:5<2166::AID-CNCR2820380547>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 2.Miettinen M, Sarlomo-Rikala M, Sobin LH, Lasota J. Esophageal stromal tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 17 cases and comparison with esophageal leiomyomas and leiomyosarcomas. Am J Surg Pathol. 2000;24:211–22. doi: 10.1097/00000478-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Blum MG, Bilimoria KY, Wayne JD, de Hoyos AL, Talamonti MS, Adley B. Surgical considerations for the management and resection of esophageal gastrointestinal stromal tumors. Ann Thorac Surg. 2007;84:1717–23. doi: 10.1016/j.athoracsur.2007.05.071. [DOI] [PubMed] [Google Scholar]
- 4.Von Rahden BH, Stein HJ, Feussner H, Siewert JR. Enucleation of submucosal tumors of the esophagus: minimally invasive versus open approach. Surg Endosc. 2004;18:924–30. doi: 10.1007/s00464-003-9130-9. [DOI] [PubMed] [Google Scholar]
- 5.Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J. Enucleation of esophageal submucosal tumors: a single institution’s experience. Ann Thorac Surg. 2014;97:454–9. doi: 10.1016/j.athoracsur.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 6.Bonavina L, Segalin A, Rosati R, Pavanello M, Peracchia A. Surgical therapy of esophageal leiomyoma. J Am Coll Surg. 1995;181:257–62. [PubMed] [Google Scholar]
- 7.Guo J, Liu Z, Sun S, Liu X, Wang S, Ge N. Ligation-assisted endoscopic enucleation for treatment of esophageal subepithelial lesions originating from the muscularis propria: a preliminary study. Dis Esophagus. 2014 Mar 4; doi: 10.1111/dote.12192. [Epub] http://dx.doi.org/10.1111/dote.12192. [DOI] [PubMed] [Google Scholar]
- 8.Chak A. EUS in submucosal tumors. Gastrointest Endosc. 2002;56(4 Suppl):S43–8. doi: 10.1016/S0016-5107(02)70085-0. [DOI] [PubMed] [Google Scholar]
- 9.Lee LS, Singhal S, Brinster CJ, et al. Current management of esophageal leiomyoma. J Am Coll Surg. 2004;198:136–46. doi: 10.1016/j.jamcollsurg.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Everitt NJ, Glinatsis M, McMahon MJ. Thoracoscopic enucleation of leiomyoma of the oesophagus. Br J Surg. 1992;79:643. doi: 10.1002/bjs.1800790715. [DOI] [PubMed] [Google Scholar]
- 11.Claus CM, Cury Filho AM, Boscardim PC, Andriguetto PC, Loureiro MP, Bonin EA. Thoracoscopic enucleation of esophageal leiomyoma in prone position and single lumen endotracheal intubation. Surg Endosc. 2013;27:3364–9. doi: 10.1007/s00464-013-2918-3. [DOI] [PubMed] [Google Scholar]
- 12.Kent M, d’Amato T, Nordman C, et al. Minimally invasive resection of benign esophageal tumors. J Thorac Cardiovasc Surg. 2007;134:176–81. doi: 10.1016/j.jtcvs.2006.10.082. [DOI] [PubMed] [Google Scholar]
- 13.Choi SH, Kim YT, Han KN, et al. Surgical management of the esophageal leiomyoma: lessons from a retrospective review. Dis Esophagus. 2010 Dec 10; doi: 10.1111/j.1442-2050.2010.01144.x. [Epub] http://dx.do-i.org/10.1111/j.1442-2050.2010.01144.x. [DOI] [PubMed] [Google Scholar]
- 14.Jiang G, Zhao H, Yang F, et al. Thoracoscopic enucleation of esophageal leiomyoma: a retrospective study on 40 cases. Dis Esophagus. 2009;22:279–83. doi: 10.1111/j.1442-2050.2008.00883.x. [DOI] [PubMed] [Google Scholar]
- 15.Jeon HW, Choi MG, Lim CH, Park JK, Sung SW. Intraoperative esophagoscopy provides accuracy and safety in video-assisted thoracoscopic enucleation of benign esophageal submucosal tumors. Dis Esophagus. 2014 Apr 9; doi: 10.1111/dote.12220. [Epub] http://dx.doi.org/10.1111/dote.12220. [DOI] [PubMed] [Google Scholar]