Abstract
Gorham-Stout Syndrome (GSS) is a rare disease characterized by localized bone resorption. Any part of the skeleton may be affected; therefore, symptoms can vary depending on the site involved. Pathological analysis reveals lymphovascular proliferation and osteolysis in the affected lesion, but the etiology of the disease is poorly understood. When GSS occurs in the chest, chylothorax or respiratory failure may occur. Thus far, a standard treatment for GSS has not been established, and the prognosis remains unknown. The following case report describes a successfully treated case of GSS in a 16-year-old boy with an affected sternum and ribs.
Keywords: Sternum, Gorham-Stout Syndrome
CASE REPORT
A 16-year-old boy was referred to Gangnam Severance Hospital for a chest wall mass. During the preceding year, the patient occasionally experienced mild and diffuse chest pain. He had no family history of genetic or osteolytic disease. The patient was previously admitted to a local medical center for a lower extremity bone fracture. However, because he was also experiencing chest pain during admission, he was referred to Gangnam Severance Hospital. Chest computed tomography (CT) revealed a mass on the anterior chest wall of the sternum without mineralization (Fig. 1A). An ultrasound-guided biopsy was planned, but it failed because of the high vascularity within the mass. Magnetic resonance imaging revealed a highly vascular extensive extraosseous mass on the sternum (Fig. 1B). Additionally, the mass caused sternal destruction and anterior mediastinal extension. A malignant bone tumor such as Ewing’s sarcoma was suspected because the mass appeared to originate in the bone and invade the surrounding tissues. Whole-body bone scintigraphy was performed, and photon defects were observed in the sternum and the left first rib. In contrast, uptake was increased in the left second and third ribs (Fig. 1C). These findings suggested a destructive bone lesion because of a tumorous condition. To eliminate the possibility of a hemangioma, a red blood cell scan was performed; however, there was no scintigraphic evidence of a hemangioma. Positron emission tomography (PET) revealed a diffuse infiltrative lesion of the sternum with bony destruction and mild fluorodeoxyglucose uptake. No other hypermetabolic focus or distant metastasis was observed (Fig. 1D). As PET revealed that the disease was restricted to the sternum and the adjacent bones, an open bone biopsy was performed. A 3-cm incision was made along the midsternal line. The sternum was dissolved and reticulated (Fig. 2A), and a bloody effusion leaking from the posterior side of the sternum was noted. On the basis of the pathological results, it was suggested that the mass was characterized by angiomatosis without atypical cells. The clinical manifestations as well as radiological and pathological findings suggested a monocentric osteolytic bone disease such as Gorham-Stout syndrome (GSS).
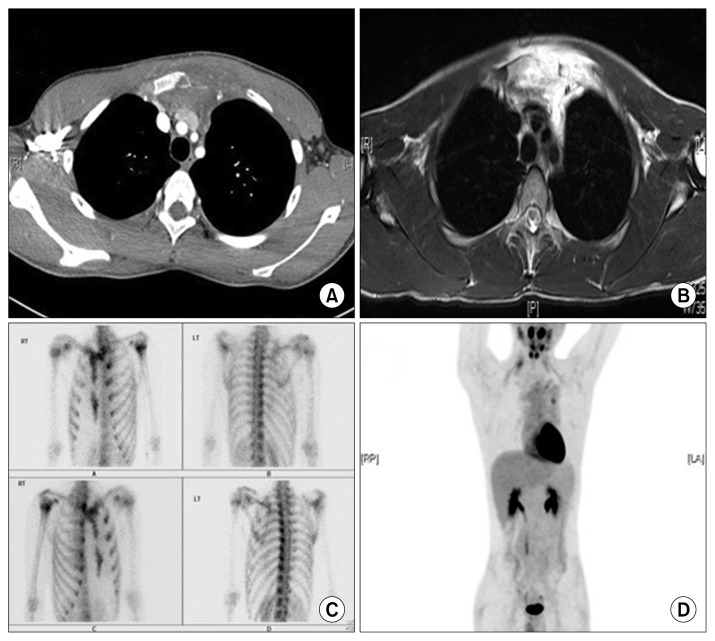
Fig. 1.
(A) A chest computed tomography (CT) scan illustrating a mass in the anterior chest wall without mineralization. (B) A magnetic resonance image displaying an extensive highly vascular extraosseous mass. (C) A whole-body bone scintigraphy image. (D) A positron emission tomography-CT scan showing a diffuse infiltrative lesion with bony destruction and mild uptake.
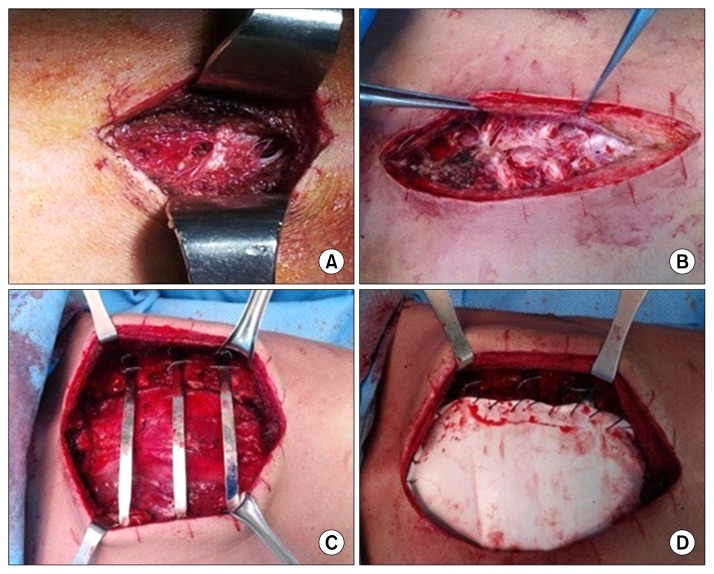
Fig. 2.
Operative findings. (A) Preoperative bone biopsy was performed. A 3-cm incision was made along the midsternal line. The sternum was dissolved and reticulated. (B) The manubrium and sternal body were almost dissolved, and the costal cartilages were attached. (C) The anterior chest wall was stabilized. (D) The defect of the bony thorax was covered with a Gore-tex membrane.
As there is no approved treatment for GSS, various treatment methods have been utilized on a case-by-case basis without proven principles. If the lesion is localized, then surgery is the principal treatment modality. However, surgery is not usually possible because of inadequate bone for fixation and extensive osteolysis [1]. In our case, extensive sternum involvement of GSS-induced sternum instability and the possibility of pathologic fracture could cause respiratory failure and incidental injury of the heart or lungs. Although the patient’s pain was not severe, aggressive treatments such as radiotherapy and immunotherapy were planned to suppress disease activity and decrease the extent of the osteolytic lesion. Consequently, radiotherapy (40 Gy) was delivered to the anterior chest wall including the sternum for 1 month. After radiotherapy, immunotherapy with interferon alpha (INF-α) was initiated. INF-α was infused twice a week, and its dose was gradually increased. CT performed 3 months after treatment (Fig. 3A) revealed that the size of the mass was slightly decreased and that the osteolytic lesion was localized. However, osteolytic lesions are not reversible in subjects with GSS. Therefore, sternal instability and the possibility of pathologic fracture remained. Therefore, we decided to resect the involved bone.
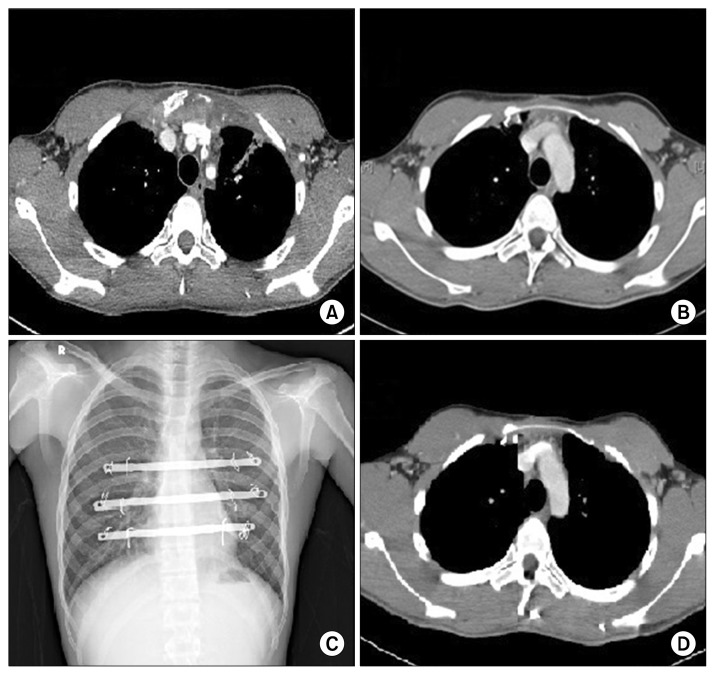
Fig. 3.
Postimmunotherapy and postoperative images. (A) Postimmunotherapy chest computed tomography (CT). The size of the mass was decreased. (B) The status of sternum resection and chest wall reconstruction was evaluated; no abnormal mass was observed on the postoperative chest CT scan. (C) No specific lesion was observed on the postoperative chest radiograph. (D) CT performed 1 year after surgery. There was no evidence of recurrence.
En bloc resection was performed. The sternum was exposed by making a midline incision on the anterior chest. The manubrium and the sternal body were involved, and they displayed a mesh-like appearance (Fig. 2B). The 2nd to 7th rib cartilages as well as the sternum and the manubrium were totally removed. The defect was reconstructed with 3 pectus bars and 2 Gore-Tex membranes (Fig. 2C, D). The pectus bars were fixed to the 3rd, 4th, and 5th ribs with wire. An artificial component was used to prevent recurrence instead of a bone graft. Flaps from both pectoralis major muscles were used to cover the artificial anterior chest wall. The patient recovered without any postoperative complications, and he was discharged 12 days after the operation. Chest CT (Fig. 3B) and chest radiograph (Fig. 3C) were performed 4 months after surgery, and the results did not reveal any signs of recurrence, nor did the patient experience any symptoms. The final chest CT (Fig. 3D) was performed 1 year after the operation, and the results remained unchanged.
DISCUSSION
Jackson first described GSS as ‘the boneless arm’ in 1838, and Gorham and Stout defined this disease entity in 1954. GSS is an extremely rare disease characterized by monocentric, idiopathic, and progressive osteolysis with resorption [1–3]. The pathophysiology of GSS is unknown; however, microscopic findings revealed vascular proliferation in the bone without malignant potency. The bone tissue is replaced by vascular tissue, but bone regeneration does not occur. Because the outside structure of the bone remains intact, gross deformity is not detected before a pathologic fracture occurs [3].
To diagnose this disease, clinical manifestations, radiological findings, histopathological features, and other osteolytic diseases should be considered. Exclusive diagnostic criteria were suggested by Heffez et al. [4] in 1983. GSS is difficult to diagnose because any part of the skeleton can be affected, including the skull, mandible, shoulder, vertebrae, and pelvic girdle [1,3]. The symptoms depend on the affected bone. Common symptoms include diffuse and slowly increasing pain, limitation of motion, and spontaneous fracture. Osteolytic lesions can occur in any bone of the body at any age without any associated clinical manifestations [1]. Histopathological analysis suggests the presence of angiomatous tissue in the osteolytic lesion without the presence of atypical cells [1,3]. Compared with other idiopathic osteolytic diseases, GSS is not hereditary or associated with nephropathy [1].
The prognosis of GSS is unpredictable owing to its unknown etiology. Extremity involvement causes minimal disabilities, and this syndrome is self-limiting in some cases. Conservative management such as pain control is effective and sufficient for treating GSS [3]. However, involvement of the thoracic cage, particularly the thoracic vertebrae, ribs, and sternum, may lead to a poor prognosis, as respiratory function is decreased because of chest wall weakness. When this disease invades the pleura, chylothorax occurs, leading to high mortality [5]. If a pathological fracture, one of the main clinical manifestations of GSS, has occurred, then surgery is the only available treatment option because the affected bone will not regenerate naturally [3]. Therefore, GSS with sternal involvement should be treated aggressively via a therapeutic plan including resection of the affected bone, radiotherapy, and medical treatment with INF-α or bisphosphonate [3]. Radiotherapy or treatment with INF-α or bisphosphonate has been found to suppress GSS effectively [2]; however, these are not confirmed treatments because only a few cases of GSS with sternal involvement have been reported, owing to the rarity of the disease.
In this case report, we presented a successfully treated case of GSS involving the sternum. In this specific case, no severe symptoms or pathologic sternal fractures existed, and the disease progression was not rapid. However, the sternum is an important chest wall component that protects the heart and lungs, and sternal weakness could lead to a life-threatening situation and progressive respiratory failure. Consequently, surgery was the definitive treatment in this case, and en bloc resection with sternum reconstruction was performed. However, unfortunately, surgery is not always possible because of the affected adjacent bones. When the disease progresses, the adjacent bones should be considered inadequate for fixation [1]. Although GSS presents many hurdles to resection and reconstruction, cases of GSS with fractures or fragile lesions should be treated via surgery.
The purpose of this case report was to highlight the role of surgery as a viable treatment option for GSS. This report describes the successful treatment of a case of GSS with sternum and rib involvement. Neoadjuvant radiotherapy and INF-α were used to suppress the disease, and resection of the sternum and the rib cartilage was performed to prevent recurrence.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Gondivkar SM, Gadbail AR. Gorham-Stout syndrome: a rare clinical entity and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e41–8. doi: 10.1016/j.tripleo.2009.08.043. [DOI] [PubMed] [Google Scholar]
- 2.Chong Ng L, Sell P. Gorham disease of the cervical spine-a case report and review of the literature. Spine (Phila Pa 1976) 2003;28:E355–8. doi: 10.1097/01.BRS.0000084557.38858.85. [DOI] [PubMed] [Google Scholar]
- 3.Ruggieri P, Montalti M, Angelini A, Alberghini M, Mercuri M. Gorham-Stout disease: the experience of the Rizzoli Institute and review of the literature. Skeletal Radiol. 2011;40:1391–7. doi: 10.1007/s00256-010-1051-9. [DOI] [PubMed] [Google Scholar]
- 4.Heffez L, Doku HC, Carter BL, Feeney JE. Perspectives on massive osteolysis: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1983;55:331–43. doi: 10.1016/0030-4220(83)90185-8. [DOI] [PubMed] [Google Scholar]
- 5.Brodszki N, Lansberg JK, Dictor M, et al. A novel treatment approach for paediatric Gorham-Stout syndrome with chylothorax. Acta Paediatr. 2011;100:1448–53. doi: 10.1111/j.1651-2227.2011.02361.x. [DOI] [PubMed] [Google Scholar]