Abstract
Idiopathic pulmonary arterial hypertension eventually leads to right-sided heart failure and sudden death. Its mortality rate in children is still high, despite improvements in pharmacological therapy, and therefore novel treatments are necessary. The Potts shunt, which creates an anastomosis between the left pulmonary artery and the descending aorta, has been proposed as a theoretically promising palliative surgical technique to decompress the right ventricle. We report the case of a 12-year-old girl with suprasystemic idiopathic pulmonary hypertension and right ventricular failure who underwent a Potts shunt for palliation with good short-term results.
Keywords: Shunts, Pulmonary hypertension
CASE REPORT
Idiopathic pulmonary arterial hypertension is a rare childhood disease with high mortality, eventually leading to right heart failure and sudden death. Despite the development of novel pharmacological agents, such as prostaglandin E1, endothelin receptor antagonists, and nitric oxide, the mortality rate is still high, especially in patients with recurrent syncope and severe right-sided heart failure, corresponding to New York Heart Association class IV [1]. The Potts shunt, a novel surgical approach that creates an anastomosis between the descending aorta and the left pulmonary artery, has been proposed to decompress the right side of the heart [2]. We report a case of suprasystemic primary pulmonary hypertension in a child with right heart failure refractory to medical treatment who underwent a Potts shunt as a palliative treatment and as a bridge to heart-lung transplantation.
A four-year-old girl was admitted to the clinic with respiratory difficulty, vomiting, and syncope, and was diagnosed with primary pulmonary arterial hypertension. There were no abnormal findings in her past medical history or in her familial history. A transthoracic Doppler echocardiogram showed dilated right atrial and right ventricular cavities with decreased right ventricular function. It showed moderate-to-severe tricuspid regurgitation with a pressure gradient of 100 mmHg. There was no evidence of pulmonary vein abnormalities. Her clinical condition improved and she was discharged after medical management involving dobutamine support and the application of sildenafil, digoxin, and diuretics.
For the following eight years, the patient was repeatedly admitted for dobutamine support due to refractory right ventricular failure despite combined therapy with bosentan, Viagra, Beraprost sodium, iloprost, digoxin, and diuretics. She experienced episodes of syncope four to five times a month and left-side chest pain two to three times a day. We put her on the list of heart-lung transplantation candidates, but she was at risk of sudden death. We decided to perform a Potts shunt as a palliative treatment and bridge to transplantation. Preoperative right cardiac catheterization showed suprasystemic precapillary pulmonary hypertension (systolic/diastolic/mean blood pressure of 130/56/87 mmHg, compared to descending thoracic aorta pressure of 105/66/83 mmHg).
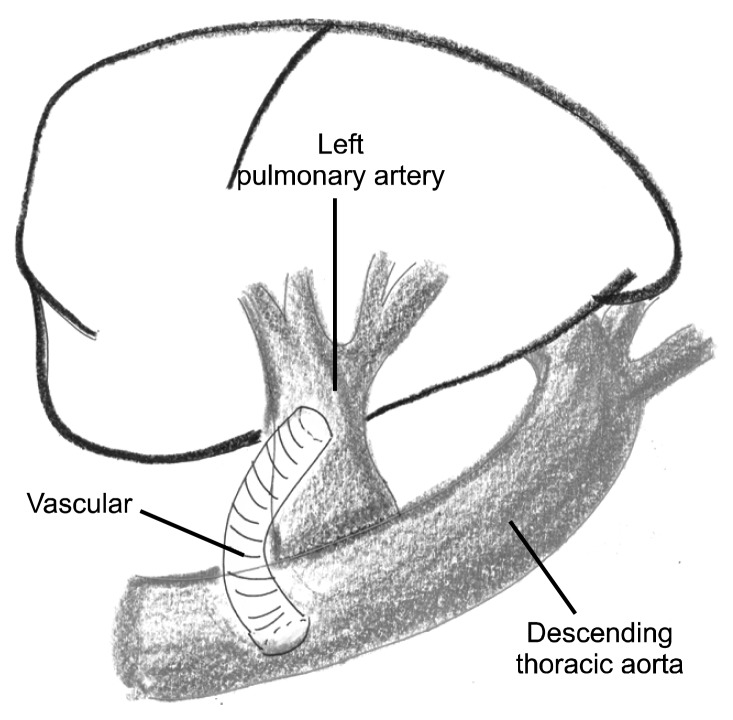
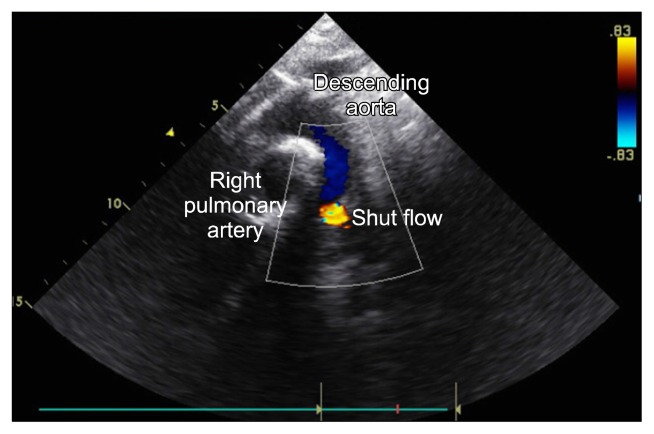
After a posterolateral thoracotomy via the left fourth intercostal space, the left pulmonary artery was anastomosed to the descending thoracic aorta with a 6 mm Gore-Tex vascular graft (Figs. 1, 2). The procedure was uneventful and the patient recovered without any significant postoperative events. The patient was extubated one day after the operation, and transferred to the general ward on postoperative day seven. She was discharged one month after surgery. She was in functional class III at discharge, and her oxygen saturation was 98% in the upper extremities and 74% in the lower extremities.
Fig. 1.
Schematic view of the Potts shunt procedure.
Fig. 2.
Echocardiographic view of the Potts shunt.
DISCUSSION
Idiopathic pulmonary arterial hypertension is a rare pediatric disease with a poor prognosis and high mortality rate due to progressive right heart failure and the risk of sudden death. Without treatment, the mean survival of children after diagnosis is less than one year [3]. Currently known factors associated with mortality are right atrial pressure, pulmonary artery pressure, and the cardiac index [3]. There has been significant improvement in pharmacological therapy for this condition, but nonetheless, some patients who are refractory to non-surgical treatment are at risk for sudden death and require bilateral lung or heart-lung transplantation as the final treatment option. Thus, there is a need for the development of novel therapeutic options in order to palliate patients with severe right heart failure, avoid sudden death, and provide a bridge to transplantation.
It is well known that patients with Eisenmenger physiology have better survival rates than patients with primary pulmonary hypertension who have an intact atrial septum [4]. Thus, percutaneous atrial septostomy has been implemented to convert normal cardiac physiology to the typical Eisenmenger physiology [3]. This allows a right-to-left shunt to decompress the right side of the heart, increasing systemic cardiac output and systemic oxygen transport, but decreasing systemic arterial oxygen saturation. In patients with severe right heart failure and markedly elevated pulmonary vascular resistance, atrial septostomy can be fatal due to insufficient pulmonary blood flow and subsequent severe hypoxemia. The procedure-related mortality of atrial septostomy in patients with severe pulmonary arterial hypertension and right heart failure has been reported to be 7.1% at 24 hours and 14.8% at one month after the procedure. The most common cause of death within 24 hours was refractory hypoxemia [5].
The Potts shunt is a novel alternative technique for decompressing the right ventricle without significant upper body cyanosis. It is a surgical technique in which a side-to-side anastomosis is created from the left pulmonary artery to the descending aorta, resulting in a right-to-left shunt. There have been several international case reports and case series reports of successful Potts shunts [2,6], but no case reports from Korea have yet been published. Thus, we present a successful case of a Potts shunt in a patient with severe idiopathic pulmonary hypertension and right heart failure refractory to medical treatment.
The current indications for a Potts shunt are limited to patients with suprasystemic refractory pulmonary hypertension. In patients with isosystemic pulmonary hypertension and exercise intolerance, a Potts shunt might allow right-to-left shunting during a suprasystemic pulmonary hypertensive crisis. However, further modifications of the Potts shunt, such as a unidirectional valved anastomosis, are needed to prevent left-to-right shunting during isosystemic or lower pulmonary arterial pressure at rest. Bui et al. [7] have reported successful results with unidirectional valved Potts anastomoses on pigs, using Gore-Tex patches mimicking the membrane of fossa ovalis. This modification could be adapted to patients with pulmonary arterial hypertension who are refractory to medical management in earlier stages of the disease.
In conclusion, despite recent improvements in pharmacological therapy, the mortality of idiopathic pulmonary arterial hypertension is still high, and the condition eventually leads to right heart failure and sudden death. The Potts shunt, which creates an anastomosis between the left pulmonary artery and the descending aorta, is theoretically advantageous in that it decompresses the failing right ventricle without causing upper body cyanosis. The Potts shunt may be an alternative option as a palliative treatment and bridge to transplantation in patients with idiopathic pulmonary hypertension and severe right heart failure refractory to medical management.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Thoele DG, Barst RJ, Gersony WM. Physiologic-based management of primary pulmonary hypertension in children and young adults. J Am Coll Cardiol. 1990;15:242A. doi: 10.1016/0735-1097(90)92680-Z. [DOI] [Google Scholar]
- 2.Blanc J, Vouhe P, Bonnet D. Potts shunt in patients with pulmonary hypertension. N Engl J Med. 2004;350:623. doi: 10.1056/NEJM200402053500623. [DOI] [PubMed] [Google Scholar]
- 3.Kerstein D, Levy PS, Hsu DT, Hordof AJ, Gersony WM, Barst RJ. Blade balloon atrial septostomy in patients with severe primary pulmonary hypertension. Circulation. 1995;91:2028–35. doi: 10.1161/01.CIR.91.7.2028. [DOI] [PubMed] [Google Scholar]
- 4.Hopkins WE, Ochoa LL, Richardson GW, Trulock EP. Comparison of the hemodynamics and survival of adults with severe primary pulmonary hypertension or Eisenmenger syndrome. J Heart Lung Transplant. 1996;15(1 Pt 1):100–5. [PubMed] [Google Scholar]
- 5.Keogh AM, Mayer E, Benza RL, et al. Interventional and surgical modalities of treatment in pulmonary hypertension. J Am Coll Cardiol. 2009;54(1 Suppl):S67–77. doi: 10.1016/j.jacc.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Zipes DP, Braunwald E, Libby P, Bonow RO Ralph Erskine Conrad Memorial Fund. Braunwald’s heart disease: a textbook of cardiovascular medicine. 7th ed. Philadelphia (PA): WB Saunders; 2005. [Google Scholar]
- 7.Bui MT, Grollmus O, Ly M, et al. Surgical palliation of primary pulmonary arterial hypertension by a unidirectional valved Potts anastomosis in an animal model. J Thorac Cardiovasc Surg. 2011;142:1223–8. doi: 10.1016/j.jtcvs.2010.10.060. [DOI] [PubMed] [Google Scholar]