Abstract
The purpose of this study was to analyze data according to gender, age, cause, number of traumatized teeth, time elapsed before treatment and type of tooth from the records of traumatized children. A retrospective study was conducted in the Department of Paediatric Dentistry at the University Dental Clinic in Zagreb. Croatia using the documentation of 128 patients (61 males and 67 females) aged 1 month to 6 years with injuries of primary teeth between February 2009 and January 2013. Trauma was seen in 217 primary teeth, which implies that the number of injured primary teeth was 1.69 per child. The maxillary central incisors were the most frequently affected teeth (81.1%), they were followed by maxillary lateral incisors, while the least affected were mandibular central incisors. Traumatic dental injuries involved periodontal tissue 2.82 times more frequently than hard dental and pulp tissue. The main cause of teeth injury was fall (67.2%) and the majority of injuries occurred at home (51.6%) (p<0.05). Of 128 patients who received treatment 71 (55.5%) also had soft-tissue injuries. The distribution of soft-tissue injuries by gender (35 males, 36 females) was not statistically significant. Comparing children with soft-tissue injuries and those without them, a statistically significant difference was found in the time of arrival (p<0.01). The results of this study showed the need of informing about preventive measures against falls at home and the methods of providing first aid in dental trauma injuries.
KEY WORDS: primary teeth, periodontal tissue, tooth injuries, soft-tissue injuries
INTRODUCTION
In preschool children head trauma accounts for 40% of injuries, and one-third of these lesions affect face [1]. Primary dentition is shown to suffer a higher prevalence of trauma with an average of 30% of children experiencing some dental trauma than children with permanent dentition [2-4]. Preschoolers showed a high prevalence of traumatic dental injuries (TDI) because of the lack of motor coordination [5] and underdevelopment in physical and emotional growth [6]. According to epidemiological studies from different countries, the frequency of primary tooth injuries ranges from 4% to 30% [7] and approximately 40% of children have their first contact with a dentist due to traumatic injuries [8]. Some of these values may be underestimated because many children with mild dental injuries do not seek care or do not receive an accurate diagnosis [9]. Dental trauma in primary teeth may cause pain and loss of function and may also affect the development of the middle third of the face, permanent teeth and occlusion, which may result in physical, emotional and behavioural problems in children and their parents or guardians [10, 11]. For a long time gender and age were considered the main risk factors for TDI in primary teeth but currently, as Glendor [2] states, other factors receive more attention, like the type of activity at the time of an accident and environmental, behavioural and socioeconomic factors. As there is no recent research on traumatic dental injuries of deciduous teeth in Zagreb, the purpose of this study is to analyse data according to gender, age, cause, number of traumatized teeth, time elapsed before treatment, type of tooth from the records of traumatized children referring to the University Dental Clinic in Zagreb, Croatia. Furthermore, the purpose is also to estimate the distribution and location of soft-tissue injuries and to determine if the presence of soft-tissue injuries influences the time elapsed between trauma and initial treatment.
MATERIALS AND METHODS
Patients
A retrospective study was conducted in the Department of Paediatric Dentistry at the University Dental Clinic in Zagreb, Croatia using the documentation of 128 patients (61 males and 67 females) aged 1 month to 6 years with injuries of primary teeth between February 2009 and January 2013.
Procedures
Trauma charts were written by a specialist of paediatric dentistry. Charts with incomplete medical information were excluded from this study. The information from trauma charts was organized by age, gender, place and source of trauma, hour and season of trauma, interval between injury and treatment, number of traumatized teeth, injured teeth, type of trauma and soft-tissue injuries. Radiographs were also used to classify hard and periodontal tissue damage. The type of trauma was classified according to Andreasen & Andreasen [12] classification: 1. Injuries to the hard tissue and the pulp: enamel fracture, enamel-dentin fracture without pulp exposure, enamel-dentin fracture with pulp exposure, crown-root fracture, root fracture and alveolar fracture; 2. Injuries to the periodontal tissue: concussion, subluxation, displacement, intrusion, extrusion and avulsion. Injuries of soft-tissue were divided into those of the upper and lower lip, tongue, gingiva and lip and gingiva injuries. TDI was classified according to the most serious damage if a specific tooth had more than one type of injury. Ethical approval for the study was obtained by the Ethical Committee of The Faculty of Dental Medicine, University of Zagreb, Croatia.
Statistical analysis
The statistical analysis was carried out by using descriptive statistics and Paerson’s chi-square test using Predictive Analytics SoftWare (PASW) for Windows version 17.0 (SPSS Inc, Chicago, IL, USA). The level of significance was set at 5%.
RESULTS
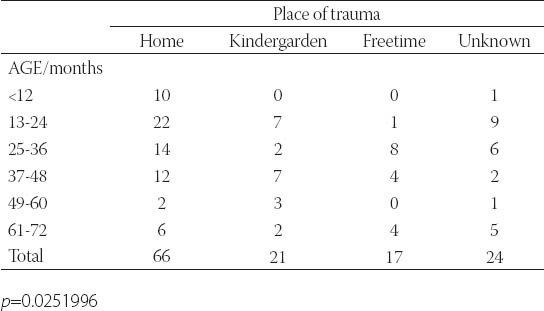
Of 128 patients attending the University Dental Clinic in Zagreb there were 52.3% females and 47.7% males, which is represented by female-male ratio of 1.1:1 and there is no statistical difference between genders. Ages were ranged from 1 month to 6 years (mean ± SD = 3.2111.48 years). The distribution of children suffering trauma in relation to age and gender is shown in Figure 1. Trauma was seen in 217 primary teeth, which implies that the number of injured primary teeth was 1.69 per child. Sixty-eight children (53.1%) had only one tooth traumatized, whereas sixty (46.9%) had more than one tooth traumatized. The maxillary central incisors were the most frequently affected teeth (81.1%), they were followed by maxillary lateral incisors (15.6%), while the least affected were mandibular central incisors (1%). TDI involved periodontal tissue 2.8 times more frequently than hard dental and pulp tissue. In primary dentition the most commonly observed TDI of dental hard tissue and pulp was enamel-dentin fracture without pulp exposure (11.1%), followed by enamel-dentin fracture with pulp exposure (9.7%) and enamel fracture (4.1%). In the analysis of the periodontal tissue injury, subluxation was the most common type (41.5%) and intrusion (17.9%) and avulsion (12.9%) were far behind. The main cause of teeth injury was fall (67.2%) (Figure 2) and the majority of injuries occurred at home (51.6%) (p<0.05) (Table 1).
FIGURE 1.
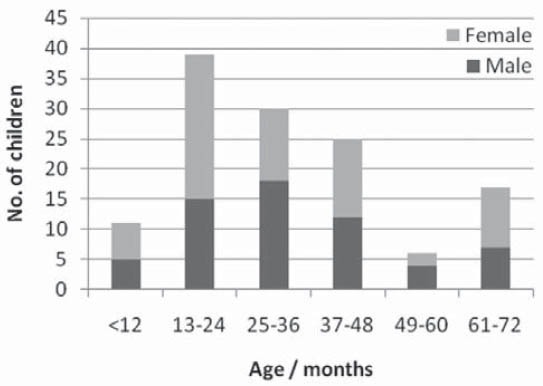
Distribution of traumatic dental injuries in relation to age and gender
FIGURE 2.
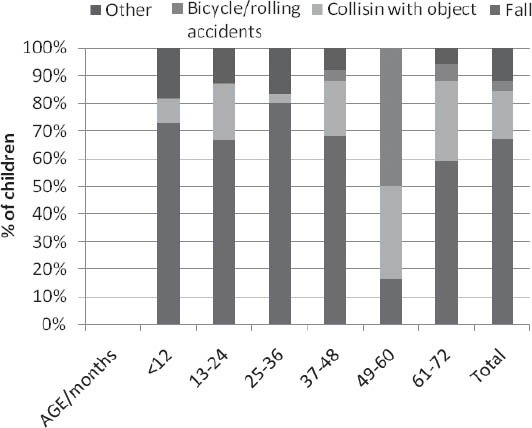
Distribution of TDIs according to cause of injury
TABLE 1.
Distribution of TDIs according to place of occurrence
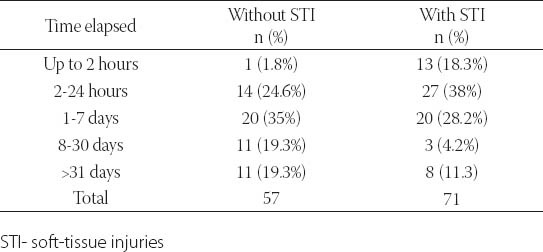
The highest dental trauma frequency was noted in spring and summer (39 cases, 30.5%), followed by autumn (33 cases, 25.8%) and winter (17 cases, 13.2%) and there was statistical difference in the seasonal distribution of TDI (p<0.05). Children (42.2%) in the age group between 1 month to 6 years had TDI in the interval from 4 to 7 p.m., while 71 (55.5%) of 128 patients who received treatment, also had soft-tissue injuries. The distribution of soft-tissue injuries by gender (35 males, 36 females) was not statistically significant (p=0.91). The highest percentage of preschoolers had soft-tissue injures at the age of 2 (25.4%). Of the total number of children 25% (31) had an injury of the upper lip, 17.2% (22) injured the upper lip and gingiva, 13.3% (17) injured gingiva and only one patient (0.8%) had a tongue injury. There was a statistically significant difference (p<0.001) among the distribution of soft-tissue injuries. Out of the group of children with injured primary tooth, 32% received treatment within 2-24 hours, followed by a group of children (31.3%) who received initial treatment in 1-7 days. The data about the time elapsed changed when soft-tissue injuries are included. Comparing children with soft-tissue injuries and those without them, a statistically significant difference was found in the time of arrival (p<0.01) (Table 2).
TABLE 2.
Distribution of elapsed time to treatment after injury with respect to presence of soft tissue injuries
DISCUSSION
TDI is currently seen as a public health problem because of its frequency and its wide occurrence among young patients during growth and development. Moreover, its treatment is often complex and expensive, and there may be an irreversible sequel, which will require treatment during the patient’s entire life [11-13]. Several studies found a greater prevalence of trauma among male patients [7, 14-17], however this study proved that girls show higher rates of TDI than boys. This is in agreement with Carvalho et al. [18]. It can be explained by the fact that both boys and girls aged 1 month to 6 years are exposed to similar risk factors and there is no difference among the games and sports they play. The present study showed that traumatic injuries to primary teeth were highest in 13-36 months (53.9%), which is in agreement with reviewed studies [5, 7, 11, 16]. At this age children are gaining mobility and independence, but still have little motor coordination. As demonstrated in studies [13, 19] a high number of TDI involved only one tooth, which may be explained by the fact that multiple dental injuries are, associated with sports, violence and traffic accidents, infrequent in this age group. The most commonly affected teeth are maxillary incisors [10, 17, 18, 20, 21] and our study findings confirm it. The reason for this is the fact that these teeth may have inadequate lip coverage and are frequently protruded. In this study TDI involved periodontal tissue almost three times more frequently than hard dental tissue and pulp, a result also found in other studies [7, 10, 20, 22, 23]. This may be explained by the resilience of the alveolar bone and the elasticity of periodontal ligament. The most frequent type of periodontal tissue trauma was subluxation, which was the same as in previous studies [7, 20, 24]. The predominant location where accidents occurred was home (51.6%), whereas falls (67.2%) were the most frequent cause of trauma, which are results similar to recent studies [7, 17, 20, 25]. Unlike other studies [14, 17, 20], which reported no statistically significant seasonal differences, the present study showed an increase in frequency of dental trauma in warmer seasons (spring and summer). One of the reasons for this can be that in warmer months children are outdoors and they participate in contact activities. Similar to Eyuboglu et al. [22], more than 50% of traumatized primary teeth were related to soft-tissue injuries; our result was 53%. As soft-tissue injuries include bleeding, it consequently motivates parents or guardians to seek earlier treatment [26]. This study showed that the time elapsed between an injury and initial treatment was shorter in bleeding than in non-bleeding injuries, which can be related to the fact that parents tend to be more anxious about bleeding injuries.
CONCLUSION
In conclusion, the present study revealed that girls suffered more often from traumatic dental injuries than boys, and injuries were more common in warmer months. Majority of injuries occurred between 1 and 3 years on the upper central incisors at home. Trauma of primary teeth were more associated with periodontal and soft-tissue than hard dental tissue and pulp. Initial treatment of soft-tissue injuries was conducted in earlier period of time. The prevalence of dental trauma has increased among preschool children during past few decades. The results of this study showed the need of informing about preventive measures against falls at home and about the methods of providing first aid in dental trauma injuries. Moreover, this study supports the necessity of education on prevention of dental injuries of all children caregivers. Further epidemiological studies are required in order to clarify the complexities of dental injury.
DECLARATION OF INTEREST
The authors declare that there are no conflicts of interest.
REFERENCES
- [1].Flores MT, Malmgren B, Andersson L, Andreasen JO, Bakland LK, Bamett F, et al. International Association of Dental Traumatology. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dent Traumatol. 2007;23(4):196–202. doi: 10.1111/j.1600-9657.2007.00627.x. [DOI] [PubMed] [Google Scholar]
- [2].Glendor U. Epidemiology of traumatic dental injuries--a 12 year review of the literature. Dent Traumatol. 2008;24(6):603–611. doi: 10.1111/j.1600-9657.2008.00696.x. [DOI] [PubMed] [Google Scholar]
- [3].Ferreira JM, Fernandes de Andrade EM, Katz CR, Rosenblatt A. Prevalence of dental trauma in deciduous teeth of Brazilian children. Dent Traumatol. 2009;25(2):219–223. doi: 10.1111/j.1600-9657.2008.00754.x. [DOI] [PubMed] [Google Scholar]
- [4].Cavalcanti AL, Bezerra PK, de Alencar CR, Moura C. Traumatic anterior dental injuries in 7- to 12-year-old Brazilian children. Dent Traumatol. 2009;25(2):198–202. doi: 10.1111/j.1600-9657.2008.00746.x. [DOI] [PubMed] [Google Scholar]
- [5].Cunha RF, Pugliesi DM, de Mello Vieira AE. Oral trauma in Brazilian patients aged 0-3 years. Dent Traumatol. 2001;17(5):210–212. doi: 10.1034/j.1600-9657.2001.170504.x. [DOI] [PubMed] [Google Scholar]
- [6].Andreasen JO. Challenges in clinical dental traumatology. Endod Dent Traumatol. 1985;1(2):45–55. doi: 10.1111/j.1600-9657.1985.tb00560.x. [DOI] [PubMed] [Google Scholar]
- [7].Avşar A, Topaloglu B. Traumatic tooth injuries to primary teeth of children aged 0-3 years (Turkey) Dent Traumatol. 2009;25(3):323–327. doi: 10.1111/j.1600-9657.2008.00695.x. [DOI] [PubMed] [Google Scholar]
- [8].Lygidakis NA, Marinou D, Katsaris N. Analysis of dental emergencies presenting to a community paediatric dentistry centre. Int J Paediatr Dent. 1998;8(3):181–190. doi: 10.1046/j.1365-263x.1998.00079.x. [DOI] [PubMed] [Google Scholar]
- [9].McTigue DJ. Diagnosis and management of dental injuries in children. Pediatr Clin North Am. 2000;47(5):1067–1084. doi: 10.1016/s0031-3955(05)70258-3. [DOI] [PubMed] [Google Scholar]
- [10].Sennhenn-Kirchner S, Jacobs HG. Traumatic injuries to the primary dentition and effects on the permanent successors - a clinical follow-up study. Dent Traumatol. 2006;22(5):237–241. doi: 10.1111/j.1600-9657.2006.00383.x. [DOI] [PubMed] [Google Scholar]
- [11].Altun C, Cehreli ZC, Güven G, Acikel C. Traumatic intrusion of primary teeth and its effects on the permanent successors: a clinical follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(4):493–498. doi: 10.1016/j.tripleo.2008.10.016. [DOI] [PubMed] [Google Scholar]
- [12].Andreasen JO, Andreasen FM. Textbook and color atlas of traumatic injuries to the teeth. 3rd edition. Copenhagen: Blackwell Munksgaard; 1994. Classification, etiology and epidemiology; pp. 151–180. [Google Scholar]
- [13].Kramer PF, Zembruski C, Ferreira SH, Feldens CA. Traumatic dental injuries in Brazilian preschool children. Dent Traumatol. 2003;19(6):299–303. doi: 10.1046/j.1600-9657.2003.00203.x. [DOI] [PubMed] [Google Scholar]
- [14].Chan YM, Williams S, Davidson LE, Drummond BK. Orofacial and dental trauma of young children in Dunedin, New Zealand. Dent Traumatol. 2011;27(3):199–202. doi: 10.1111/j.1600-9657.2011.00989.x. [DOI] [PubMed] [Google Scholar]
- [15].Wendt FP, Torriani DD, Assunção MC, Romano AR, Bonow ML, da Costa CT, et al. Traumatic dental injuries in primary dentition: epidemiological study among preschool children in South Brazil. Dent Traumatol. 2010;26(2):168–173. doi: 10.1111/j.1600-9657.2009.00852.x. [DOI] [PubMed] [Google Scholar]
- [16].Robson F, Ramos-Jorge ML, Bendo CB, Vale MP, Paiva SM, Pordeus IA. Prevalence and determining factors of traumatic injuries to primary teeth in preschool children. Dent Traumatol. 2009;25(1):118–122. doi: 10.1111/j.1600-9657.2008.00725.x. [DOI] [PubMed] [Google Scholar]
- [17].Choi SC, Park JH, Pae A, Kim JR. Retrospective study on traumatic dental injuries in preschool children at Kyung Hee Dental Hospital, Seoul, South Korea. Dent Traumatol. 2010;26(1):70–75. doi: 10.1111/j.1600-9657.2009.00840.x. [DOI] [PubMed] [Google Scholar]
- [18].Carvalho JC, Vinker F, Declerck D. Malocclusion, dental injuries and dental anomalies in the primary dentition of Belgian children. Int J Paediatr Dent. 1998;8(2):137–141. doi: 10.1046/j.1365-263x.1998.00070.x. [DOI] [PubMed] [Google Scholar]
- [19].Hargreaves JA, Cleaton-Jones PE, Roberts GJ, Williams S, Matejka JM. Trauma to primary teeth of South African pre-school children. Endod Dent Traumatol. 1999;15(2):73–76. doi: 10.1111/j.1600-9657.1999.tb00757.x. [DOI] [PubMed] [Google Scholar]
- [20].de Amorim Lde F, da Costa LR, Estrela C. Retrospective study of traumatic dental injuries in primary teeth in a Brazilian specialized pediatric practice. Dent Traumatol. 2011;27(5):368–373. doi: 10.1111/j.1600-9657.2011.01011.x. [DOI] [PubMed] [Google Scholar]
- [21].Saroglu I, Sönmez H. The prevalence of traumatic injuries treated in the pedodontic clinic of Ankara University, Turkey, during 18 months. Dent Traumatol. 2002;18(6):299–303. doi: 10.1034/j.1600-9657.2002.00093.x. [DOI] [PubMed] [Google Scholar]
- [22].Eyuboglu O, Yilmaz Y, Zehir C, Sahin H. A 6-year investigation into types of dental trauma treated in a paediatric dentistry clinic in Eastern Anatolia region, Turkey. Dent Traumatol. 2009;25(1):110–114. doi: 10.1111/j.1600-9657.2008.00668.x. [DOI] [PubMed] [Google Scholar]
- [23].Gábris K, Tarján I, Rózsa N. Dental trauma in children presenting for treatment at the Department of Dentistry for Children and Orthodontics, Budapest, 1985-1999. Dent Traumatol. 2001;17(3):103–108. doi: 10.1034/j.1600-9657.2001.017003103.x. [DOI] [PubMed] [Google Scholar]
- [24].Skaare AB, Jacobsen I. Primary tooth injuries in Norwegian children (1-8 years) Dent Traumatol. 2005;21(6):315–9. doi: 10.1111/j.1600-9657.2005.00362.x. [DOI] [PubMed] [Google Scholar]
- [25].Jorge KO, Moysés SJ, Ferreira e Ferreira E, Ramos-Jorge ML, de Araújo Zarzar PM. Prevalence and factors associated to dental trauma in infants 1-3 years of age. Dent Traumatol. 2009;25(2):185–189. doi: 10.1111/j.1600-9657.2008.00730.x. [DOI] [PubMed] [Google Scholar]
- [26].Garcia-Godoy F, Garcia-Godoy F, Garcia-Godoy FM. Reasons for seeking treatment after traumatic dental injuries. Endod Dent Traumatol. 1989;5(4):180–181. doi: 10.1111/j.1600-9657.1989.tb00356.x. [DOI] [PubMed] [Google Scholar]


