Abstract
Pilonidal disease is a common chronic disorder mainly seen in the sacrococcygeal region, especially in young males. Many surgical treatment modalities have been suggested, but an ideal and widely accepted treatment has yet to be established. The aim of this study was to compare quality of life of patients treated with the sinotomy technique with quality of life of patients treated with surgical excision plus primary closure technique by means of quality of life questionnaire. The data of patients who had been treated for pilonidal sinus in our clinic from September 2010 to June 2012 were analyzed retrospectively. Forty patients were treated with sinotomy technique and 40 patients were treated with surgical excision plus primary closure technique. Time to return to work and to time to complete wound healing were evaluated. All patients were asked to fill the questionnaire after complete healing occurred. Postoperative complications were bleeding in 2.5%, infection in 3.75% and fever in 2.5% patients. There were no significant differences between the two groups in terms of complete healing (p=0.1) and sport times (p=0.1). There were significant differences between the groups in terms of length of hospital stay (p≤0.001), time off work (p≤0.001), times to sitting on toilet and walking without pain (p=0.002 and p≤0.001, respectively). The mean postoperative VAS scores were 5.2±3.2 and 2.8±2.2, respectively (p=0.02). The technique of sinotomy with good wound and surrounding skin care seems to be an ideal approach with high chance of cure. The patients returned to their routine in a short period of time.
KEY WORDS: pilonidal sinus, excision, quality of life, recurrence, sinotomy
INTRODUCTION
Pilonidal sinus (PS) is a common condition affecting young and middle-aged adults. It occurs more commonly in males. This disease has important economic impacts and is associated with frequent inability to work and discomfort. Men are thought to be at higher risk because of their more hirsute nature. The pathogenesis remains uncertainand, there are both congenital and acquired suggestions for the etiology of this condition [1]. Risk factors include adiposity, sedentary occupation - life style, local irritation-trauma, insufficient body hygiene, excessive hairiness and perspiration [2,3]. Many methods of surgical and nonsurgical treatment have been described in the literature [1], including: excision and lyingopen, excision and primary closure of the wound [1], rhombflap procedure [4,5]. However, midline excision and primary closure remains the most commonly adoptedtechnique worldwide [6]. The ideal approach for treating pilonidal disease should be simple, inflict minimal pain, have the best chance for a cure and the least local recurrence rate, avoid admission to the hospital, avoid general anesthesia, and require minimal wound care, inconvenience and time off work for the patient [7,8]. Maintaining the quality of life is the main goal for patients with pilonidal disease; it also minimizes the time off work, deviation from normal activity, and costs [9,10]. “Return to work period” should be as short as possible because of the economic impacts [11,12]. The procedure of incision and lying open (sinotomy) involves local excision of the midline sinuses, extending into the central cavity and laying open lateral tracts. Any hairs contained in the sinus are removed and wall of the cavity is scrapped free of granulations [13]. We aimed at comparing two techniques: the sinotomy technique with surgical excision and the primary closure technique (the most commonly used techniques in our clinic) in terms of the quality of life by means of a life quality questionnaire. For this purpose, we searched for a life quality questionnaire. SF-36 and other questionnaires were general, inadequate, and could not identify problems arising from the treatment of pilonidal disease. For this reason, we designed a questionnaire with 14 items, containing perioperative pain assessment as well as a visual analog scale (VAS).
MATERIALS AND METHODS
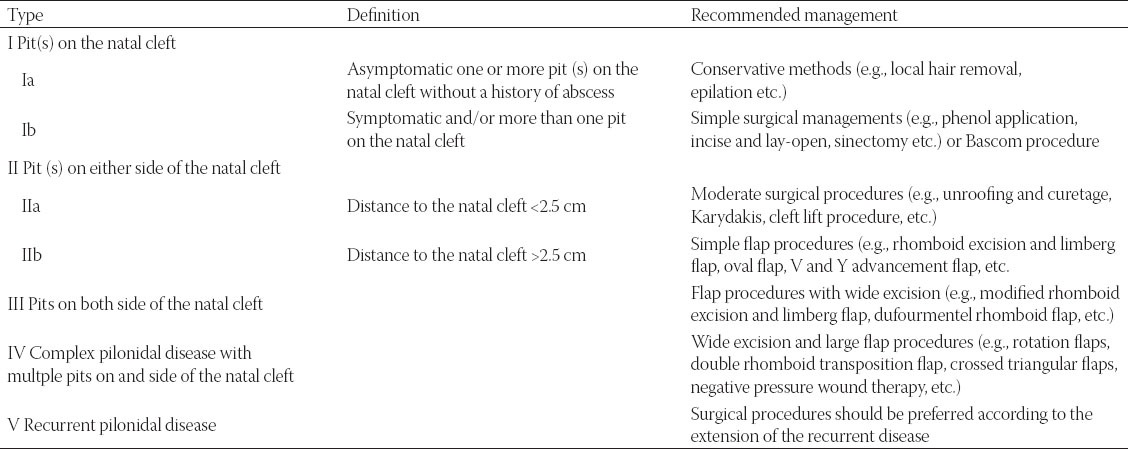
In our study we retrospectively evaluated 101 cases treated for pilonidal sinus disease from September 2010 to June 2012. Sinotomy technique was performed in 40 patients, and surgical excision as well as primary closure was done in 40 patients, all of them diagnosed with pilonidal disease. Exclusion criteria were previous pilonidal abscess surgery, diabetes mellitus, renal failure, immunosuppression, and age <16 years. All 80 patients fulfilling the criteria completed the study. We used Irkörücü and Adana Numune's classification [14] and treatment concept in sacrococcygeal pilonidal disease. Surgical techniques were used in types Ib, IIa, IIb, and some type III patients according to Irkörücü and Adana Numune's Classification and Treatment Concept (Table 1). Patients’ data (demographics and characteristics; age, gender, obesity, hirsute nature, positive family history) were extracted from the medical records. Excision surgery and the primary closure technique were carried out under general anesthesia with endotracheal intubation. The sinotomy procedure was performed under local anesthesia, with the patient lying prone. Povidone-iodine antiseptic solution was applied on the shaved skin of the buttocks, and sterile drapes were used to expose the sacrococygeal area. A small quantity of methylene blue was injected into the sinus opening in order to stain the diseased tissue and to identify the sinus extensions. The technique of sinotomy was performed as follows: 20 mL of 0.5% bupivacaine with 1:200,000 epinephrine was infiltrated in the sacrococcygeal area around pilonidal sinus, along with intravenous sedation using 1.5-3 mg of midazolam titrated slowly within five minutes to the desired effect. The main orifice was identified, cannulated with a suitably sized metal probe. This was followed by probing the main track and laying it open on the probe. Any cyst wall was dissected out and hair tufts removed. The cavity was then curetted to remove infected granulations and debris, followed by washing with hydrogen peroxide and diluted povidone-iodine solution, and finally, irrigated copiously with saline. Haemostasis and light packing were performed in the end of the operation. Postoperatively the patients had been observed for 15 minutes then discharged, with prescribed oral analgesics containing paracetamol and codeine. Sinus excision and primary closure was performed as a surgical treatment. All patients were admitted to the hospital the day before the surgery and operated under general anesthesia. The patients were placed in the prone jack-knife position on the operating table. The natal cleft was shaved just before the surgery. Excision and primaryclosure was carried out as recommended by Goligher [13]. No antibiotics were administered. The patients were instructed to return to normal daily activities as soon as they felt comfortable. All patients were checked weekly until the wound had healed and then every three months for one year. The patients were scheduled for wound inspection and removal of the sutures on day 7 and day 14 postoperatively. When no leakage from the wound and no dehiscence signs were observed, the last dressing was detached, and this was accepted as a complete healing. In order to evaluate quality of life and patient comfort, all patients were asked to fill the questionnaire after complete healing occurred (Supplementary material). Answers were documented and analyzed. Duration of incapacity for work was defined as the time from the very day of the surgery to the day on which the patient returned to normal activities including work and leisure activities. The pain level reported by patients was assessed in the pre-and post-treatment period with a visual analog scale (VAS) score. VAS scores were marked by patients on a horizontal scale, where “0” indicated painless condition and “10” denoted the worst pain.
TABLE 1.
Irkörücü and Adana Numune's classification and treatment concept in sacrococcygeal pilonidal disease
Statistical Analysis
All data are presented as mean ± standard deviation (SD) unless stated otherwise in the text. Continuous variableswere checked for the normal distribution assumption using the Kolmogorov–Smirnov statistics. Differences among the groups were analyzed by the Student's t-test and the Mann–Whitney U test for continuous variables and the chi-square test for categorical variables, as considered appropriate. The probabilities of less than 0.05 were accepted as significant. Data were analyzed using the SSPS 15.0 for Windows software (SPSS® Inc. Chicago IL).
RESULTS
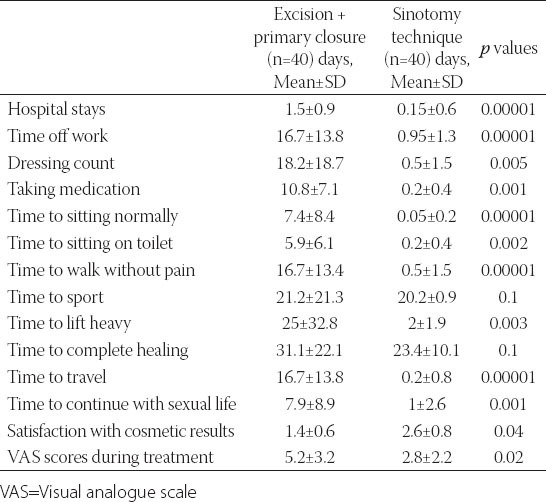
There were 46 men (57.5%) and 34 women (42.5%) participating in this study. Their ages ranged between 16 and 44 years with a mean of 25.7 years. The mean BMI of the study population was 27.2 (range 23.6 - 41.9), and 41.25% (33/80) of patients were hirsute in nature. As seen in Table 2, no significant differences between the two groups were observed in any of the patient characteristics in addition to age and gender. Postoperative complications were bleeding in 2.5%, infection in 3.75% and fever in 2.5%. Two patients experienced postoperative bleeding that required evaluation in the emergency department. Bleeding was controlled by external packing and application of local pressure and none required surgical haemostasis or blood transfusion. In a one year follow-up period, no patient suffered from recurrence of the disease. The clinical outcomes of both treatment modalities are listed in Table 3. There were significant differences between the two groups in terms of quality of life except for complete healing (p=0.1) and sport times (p=0.1). The mean postoperative Visual analogue scale scores were 5.2±3.2 and 2.8±2.2, respectively (p=0.02).
TABLE 2.
Patient demographics and characteristics
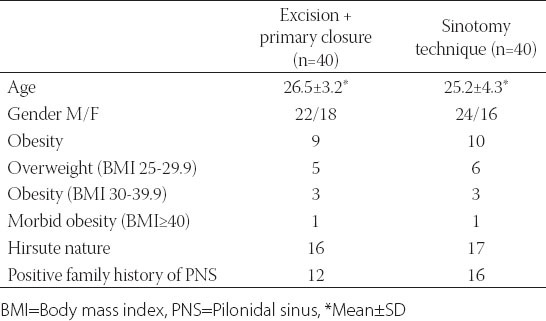
TABLE 3.
The clinical outcome of both treatment modalities
DISCUSSION
Various techniques are used currently in the treatment of pilonidal sinus disease [15]. Nevertheless, optimal treatment methods for each condition of pilonidal disease have yet to be established. An ideal surgical treatment of pilonidal disease should be simple, necessitate a short hospital stay, and have a low disease recurrence rate. In the literature, different surgical treatment options have been described for managing this condition. Most commonly, marsupialization, primary midline closure and skin flaps have been used as treatment modalities [16,17]. Different rates of morbidity, recurrence and hospitalization times have been reported for each technique [16,18]. Larger operations require longer healing times, sometimes several weeks. Surgery has a significant failure rate, with a high incidence of recurrence following the procedure [19,20]. Excision of the pilonidal sinus with primary closure has the advantage of rapid healing, but the recurrence rate is also relatively high - up to 38% [1,21]. Excision with primary closure obviates a large wound but in the process, the chances of wound infection; wound dehiscence and recurrence are very high [22]. Techniques involving closure by Z-plasty, rhomboid or myocutaneous advancement flaps require long operative time and hospital stay and are fraught with complications like loss of the graft or flap [23]. The usual mean for hospital stay in excision and primary closure techniques reported in previous studies was 4-5 days [24,25].
Incision and lying open (sinotomy) procedure involves local excision of the midline sinuses, extending into the central cavity and laying open lateral tracts. Any hairs contained in the sinus are removed and wall of the cavity is scrapped free of granulations [13]. However, it has been reported that the chances of infection are much bigger in the wounds created by excision and suturing [26]. Incidence rates of wound dehiscence followingexcision and primary repair are much bigger than previously considered [22,23]. These procedures also require a long hospital stay and long periods off work [13].
Al Naami reported his experience with the sinotomy technique [27]. The procedure was carried out under local anesthesia on an outpatient setting, with a complication rate of 3% and a recurrence rate of 2%. Yalcin [28] reported that sinotomy has the advantages of simplicity, the possibility to be performed under local anesthesia with excellent recurrence rate of 0% and complication rate of 1.69%. In sinotomy, however, as almost no tissue is excised, disfigurement is minimal and only a narrow short midline scar is left and recurrence, if occurs, could be managed by the same procedure [29]. Quality of life is the main goal for patients with pilonidal disease; it also minimizes the time off work, deviation from normal activities, and costs [9,10]. In a study evaluating the quality of life, Ertan et al. have reported that the Limberg flap technique used in pilonidal sinus surgery is better than primary closure [24]. Aydede et al. have reported that the excision and flap procedures seem to be successful in large pilonidal sinuses. However, in uncomplicated cases, excision and primary closure yields better results [30]. Ideal treatment for pilonidal disease should: be simple, need no hospitalization, minimize both: financial costs for the community, as well as costs for the patient; should not worsen the quality of life, and should be associated with a low complication rate and minimal pain [31,32].
CONCLUSION
The method described in this paper was found to be simple, cost-effective, and seems ideal with high chances of cure. The patients returned to their daily routine within a short period of time.
DECLARATION OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- [1].Allen-Mersh TG. Pilonidal-sinus: finding the right track for treatment. Br J Surg. 1990;77(2):123–32. doi: 10.1002/bjs.1800770203. doi:10.1002/bjs.1800770203. http://dx.doi.org/10.1002/bjs.1800770203 . [DOI] [PubMed] [Google Scholar]
- [2].Bendewald FP, Cima RR. Pilonidal disease. Clin Colon Rectal Surg. 2007;20(2):86–95. doi: 10.1055/s-2007-977486. http://dx.doi.org/10.1055/s-2007-977486 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010;40(8):757–62. doi: 10.1007/s00595-008-4098-7. Epub 2010 Jul 30. http://dx.doi.org/10.1007/s00595-008-4098-7 . [DOI] [PubMed] [Google Scholar]
- [4].Milito G, Cortese F, Casciani CU. Rhomboid flap procedure for pilonidal sinus: results from 67 cases. Int J Colorectal Dis. 1998;13(3):113–5. doi: 10.1007/s003840050146. http://dx.doi.org/10.1007/s003840050146 . [DOI] [PubMed] [Google Scholar]
- [5].Urhan MK, Kucukel F, Topgul K, Ozer I, Sari S. Rhomboid excision and Limberg flap for managing pilonidal sinus: results of 102 cases. Dis Colon Rectum. 2002;45(5):656–9. doi: 10.1007/s10350-004-6263-4. doi:10.1007/s10350-004-6263-4. http://dx.doi.org/10.1007/s10350-004-6263-4 . [DOI] [PubMed] [Google Scholar]
- [6].Al-Mulhim AS, Sultan MA, Ahmed HH. Pilonidal Sinus in Males: To preserve or obliterate the natal cleft. Saudi Med Journal. 2002;23(7):875–6. [PubMed] [Google Scholar]
- [7].Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002;82:1169–1185. doi: 10.1016/s0039-6109(02)00062-2. http://dx.doi.org/10.1016/S0039-6109(02)00062-2 . [DOI] [PubMed] [Google Scholar]
- [8].Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990;77:123–132. doi: 10.1002/bjs.1800770203. http://dx.doi.org/10.1002/bjs.1800770203 . [DOI] [PubMed] [Google Scholar]
- [9].Aygen E, Arslan K, Dogru O, Basbug M, Camci C. Crystallized phenol in nonoperative treatment of previously operated, recurrent pilonidal disease. Dis Colon Rectum. 2010;53(6):932–5. doi: 10.1007/DCR.0b013e3181d8283b. http://dx.doi.org/10.1007/DCR.0b013e3181d8283b . [DOI] [PubMed] [Google Scholar]
- [10].Spyridakis M, Christodoulidis G, Chatszitheofilou C, Symeonidis D, Tepetes C. The role of the platelet-rich plasma in accelerating the wound healing process and recovery in patients being operated for pilonidal sinus disease: preliminary results. World J Surg. 2009;33(8):1764–1769. doi: 10.1007/s00268-009-0046-y. http://dx.doi.org/10.1007/s00268-009-0046-y . [DOI] [PubMed] [Google Scholar]
- [11].Daphan C, Tekelioglu MH, Sayilgan C. Limberg flap repair for pilonidal sinus disease. Dis Colon Rectum. 2004;47(2):233–7. doi: 10.1007/s10350-003-0037-2. http://dx.doi.org/10.1007/s10350-003-0037-2 . [DOI] [PubMed] [Google Scholar]
- [12].Tocchi A, Mazzoni G, Bononi M, Fornasari V, Miccini M, Drumo A, et al. Outcome of chronic pilonidal disease treatment after ambulatory plain midline excision and primary suture. Am J Surg. 2008;196(1):28–33. doi: 10.1016/j.amjsurg.2007.05.051. Comment in: Am J Surg 2009; 197(5):693-4. http://dx.doi.org/10.1016/j.amjsurg.2007.05.051. [DOI] [PubMed] [Google Scholar]
- [13].Goligher J, Duthie H, Nixon H. Pilonidal sinus. In: Tindall B, editor. Surgery of the anus rectum and colon. 5th. London: 1992. pp. 230–233. [Google Scholar]
- [14].IrkörücüO Erdem H, Reyhan E. The best therapy for pilonidal disease: which management for which type? World J Surg. 2012;36:691–692. doi: 10.1007/s00268-011-1285-2. http://dx.doi.org/10.1007/s00268-011-1285-2 . [DOI] [PubMed] [Google Scholar]
- [15].daSilva JH. Pilonidal cyst: cause and treatment. Dis Colon Rectum. 2000;43(8):1146–56. doi: 10.1007/BF02236564. http://dx.doi.org/10.1007/BF02236564 . [DOI] [PubMed] [Google Scholar]
- [16].Bozkurt MK, Tezel E. Management of pilonidal sinus with the Limberg flap. Dis Colon Rectum. 1998;41(6):775–777. doi: 10.1007/BF02236268. http://dx.doi.org/10.1007/BF02236268 . [DOI] [PubMed] [Google Scholar]
- [17].Kapan M, Kapan S, Pekmezci S, Durgun V. Sacrococcygeal pilonidal sinus disease with Limberg flap repair. Tech Coloproctol. 2002;6(1):27–32. doi: 10.1007/s101510200005. doi: 10.1007/s101510200005 http://dx.doi.org/10.1007/s101510200005. [DOI] [PubMed] [Google Scholar]
- [18].Ozgultekin R, Ersan Y, Ozcan M. Die therapie des sinus pilonidalis mit dem transpositionslappen nach Limberg. Chirurg. 1995;66(3):192–195. [PubMed] [Google Scholar]
- [19].Bascom J, Bascom B. Failed pilonidal surgery: new paradigm and new operation leading to cures. Arch Surg. 2002;137(10):1146–50. doi: 10.1001/archsurg.137.10.1146. http://dx.doi.org/10.1001/archsurg.137.10.1146 . [DOI] [PubMed] [Google Scholar]
- [20].Iesalnieks I, Furst A, Rentsch M, Jauch KW. Primary midline closure after excision of a pilonidal sinus is associated with a high recurrence rate. Chirurg. 2003;74(5):461–8. doi: 10.1007/s00104-003-0616-8. doi: 10.1007/s00104-003-0616-8. http://dx.doi.org/10.1007/s00104-003-0616-8 . [DOI] [PubMed] [Google Scholar]
- [21].Rakinic J. Sacrococcygeal pilonidal sinus. In: Cameron JL, editor. Current surgical therapy. 8th. St. Louis, Missouri: Mosby; 1998. pp. 302–306. [Google Scholar]
- [22].Lee HC, Ho YH, Seow CF, Eu KW, Nyam D. Pilonidal disease in Singapore: clinical features and management. Aust N Z J Surg. 2000;70(3):196–198. doi: 10.1046/j.1440-1622.2000.01785.x. http://dx.doi.org/10.1046/j.1440-1622.2000.01785.x . [DOI] [PubMed] [Google Scholar]
- [23].Zieger K. Complications after surgery for pilonidal cyst. An introduction to a new debate on a “costly”disease. Ugeskr Laeger. 1999;161(44):6056–58. [PubMed] [Google Scholar]
- [24].Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005;190(3):388–92. doi: 10.1016/j.amjsurg.2004.08.068. http://dx.doi.org/10.1016/j.amjsurg.2004.08.068 . [DOI] [PubMed] [Google Scholar]
- [25].AbuGalala KH, Salam IM, Abu Samaan KR, El Ashaal YI, Chandran VP, Sabastian M, et al. Treatment of pilonidal sinus by primary closure with a transposed rhomboid flap compared with deep suturing: a prospective randomized clinical trial. Eur J Surg. 1999;165(5):468–72. doi: 10.1080/110241599750006721. http://dx.doi.org/10.1080/110241599750006721 . [DOI] [PubMed] [Google Scholar]
- [26].Miocinovic M, Horzic M, Bunoza D. The treatment of pilonidal disease of the sacrococcygeal region by the method of limited excision and open wound healing. Acta Med Croatica. 2000;54(1):27–31. [PubMed] [Google Scholar]
- [27].Al-Naami MY. Outpatient pilonidal sinotomy complemented with good wound and surrounding skin care. Saudi Med J. 2005;26(2):285–8. [PubMed] [Google Scholar]
- [28].Yalcin S, Ergul E. A. single-surgeon, single-institute experience of 59 sinotomies for sacrococcygeal pilonidal disease under local anesthesia. Bratisl Lek Listy. 2010;111(5):284–5. [PubMed] [Google Scholar]
- [29].Rabie ME, Al Refeidi AA, Al Haizaee A, Hilal S, Al Ajmi H, Al Amri AA. Sacrococcygeal pilonidal disease: sinotomy versus excisional surgery, a retrospective study. ANZ J Surg. 2007;77(3):177–80. doi: 10.1111/j.1445-2197.2006.04002.x. http://dx.doi.org/10.1111/j.1445-2197.2006.04002.x . [DOI] [PubMed] [Google Scholar]
- [30].Aydede H, Erhan Y, Sakarya A, Kumkumoglu Y. Comparison of three methods in surgical treatment of pilonidal disease. ANZ J Surg. 2001;71(6):362–364. http://dx.doi.org/10.1046/j.1440-1622.2001.02129.x . [PubMed] [Google Scholar]
- [31].Kayaalp C, Aydin C. Review of phenol treatment in sacrococcygeal pilon idal disease. Tech Coloproctol. 2009;13(3):189–193. doi: 10.1007/s10151-009-0519-x. http://dx.doi.org/10.1007/s10151-009-0519-x . [DOI] [PubMed] [Google Scholar]
- [32].Lee SL, Tejirian T, Abbas MA. Current management of adolescent pilonidal disease. J Pediatr Surg. 2008;43(6):1124–1127. doi: 10.1016/j.jpedsurg.2008.02.042. http://dx.doi.org/10.1016/j.jpedsurg.2008.02.042 . [DOI] [PubMed] [Google Scholar]


