CASE PRESENTATION
An 85-year-old female nursing home resident presented with a medical history of dementia, stroke, hypertension, gastroesophageal reflux disease and cholethiasis. The patient was referred because of four episodes of coffee-ground emesis and symptoms of right upper quadrant abdominal pain, with no issues with bowel movements. There was limited other information available due to the underlying history of dementia. The patient’s vital signs were stable. Physical examination revealed normal cardiorespiratory parameters. The abdominal examination revealed a tender right upper quadrant, with no palpable mass and the presence of bowel sounds. Laboratory investigations revealed a white blood cell count of 18.4×109/L (normal 4.0×109/L to 11.0×109/L), alkaline phosphatase level of 131 U/L (normal 40 U/L to 120 U/L) and gamma-glutamyl transferase level of 116 U/L (normal <37 U/L). The remaining laboratory investigations were unremarkable. An abdominal x-ray revealed a large, rounded, lamellated calcification in the epigastric region measuring approximately 4.5 cm × 3.3 cm (Figure 1). The patient underwent a computed tomography scan, which revealed gastric outlet obstruction secondary to an impacted gallstone within the duodenum, a cholecystoduodenal fistula and a collpased gallbladder, with thickening of the gallbladder wall and air within the gallbladder (Figure 2). The patient was initially managed with intravenous fluids, nasogastric tube, antiemetics and antibiotics. An urgent endoscopy was arranged by gastroenterology, revealing a stone impacted in the duodenal cap (Figure 3). Attempts to push or bypass the stone were unsuccessful, followed by attempts at retrieval with snare, basket, pronged grasper and Roth net, all of which were also unsuccessful. Additional attempts by another gastroenterologist and surgeon using endoscopic therapy to disimpact the stone were unsuccessful. The surgeon then suggested operative management for the patient; however, due to the patient’s deteriorating medical condition, the palliative team involved in her care and the family elected to proceed with palliation instead of surgery. After a three-week hospital stay, the patient was transferred to a hospice care facility where she died within one week.
Figure 1).
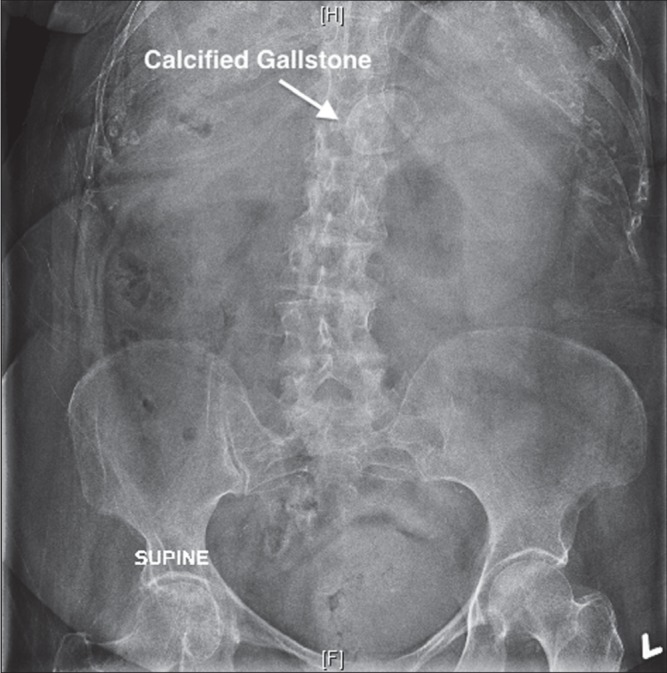
Abdominal x-ray. Ectopic calcified gallstone
Figure 2).
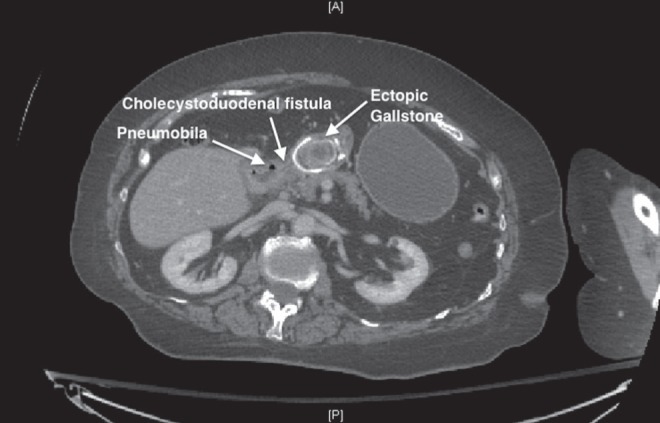
Computed tomography scan. Gallstone in the duodenum, cholecystoduodenal fistula and pneumobilia
Figure 3).
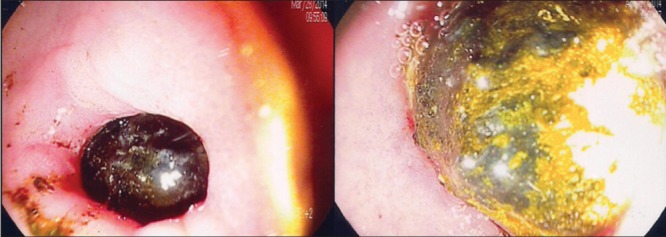
Endoscopy showing gallstone impacted in the duodenum
DISCUSSION
In 1896, the first two cases of gastric outlet obstruction from an impacted gallstone were reported by Leon Bouveret (1,2). Generally, 1% to 4% of intestinal obstruction are caused by gallstone ileus and, of these, 1% to 3% are caused by Bouveret syndrome (3,4). It is known to occur in elderly women due to the high incidence of gallstones and can cause significant morbidity and mortality, especially in patients with multiple comorbidities (5). To diagnose Bouveret syndrome, the Rigler triad of small-bowel obstruction, pneumobilia and ectopic gallstone is virtually pathognomonic; however, in conventional radiographs, it is present in only 30% to 35% of cases and is more readily apparent on computed tomography scan (2,6,7). The pathophysiology of this syndrome stems from increases in intraluminal pressure caused by obstruction, which leads to local ischemia and necrosis, enabling the gallstone to perforate the walls and pass into the intestines (4). Stones <2.5 cm in size usually pass into the small bowel while larger gallstones usually become impacted within the gastric outlet (3). Because the syndrome is common in elderly patients with comorbidities and higher perioperative surgical risk, an endoscopic approach is usually the first-line intervention (8). Despite many available endoscopic techniques, including mechanical lithotripsy, net extraction, electrohydraulic lithotripsy, intracorporeal laser lithotripsy or combinations thereof, endoscopic treatment has a success rate of only 9% (9). If endoscopy is unsuccessful, patients undergo surgery for stone extraction. The most commonly performed surgical procedures are enterolithotomy or gastrostomy with or without cholecystectomy, and fistula repair (5). Postoperative mortality rates in the early 2000s were as high as 30%; however, due to earlier diagnoses made possible by endoscopy and the advent of more minimally invasive techniques, the mortality rate has fallen to 12% (9,10). There are multiple case reports describing postoperative complications including death (2,11,12).
CONCLUSION
The patient described in our case was an elderly woman with multiple comorbidities who belonged to a high-risk group. The patient’s diagnostic imaging confirmed Rigler’s triad. She underwent three unsuccessful therapeutic endoscopic attempts to retrieve an impacted stone – an approach with a reported success rate of only 9%. The patient deteriorated rapidly during her hospital stay, which necessitated palliative management because the surgical approach was considered to be high risk. Our region has no electrohydraulic or intracorporeal laser lithotripsy facilities, which may have been a helpful endoscopic intervention. The patient died within four weeks of presentation, which reaffirms that Bouveret syndrome can cause significant morbidity and mortality.
The Canadian Journal of Gastroenterology & Hepatology is considering a limited number of submissions for IMAGE OF THE MONTH. These are based on endoscopic, histological, radiological and/or patient images, which must be anonymous with no identifying features visible. The patient must consent to publication and the consent must be submitted with the manuscript. All manuscripts should be practical and relevant to clinical practice, and not simply a case report of an esoteric condition. The text should be brief, structured as CASE PRESENTATION and DISCUSSION, and not more than 700 words in length. A maximum of three images can be submitted and the number of references should not exceed five. The submission may be edited by our editorial team.
REFERENCES
- 1.Bouveret L. Stenose du pylore adhérent à la vesicule. Rev Med (Paris) 1896;16:1–16. [Google Scholar]
- 2.Cappell MS, Davis M. Characterization of Bouveret’s syndrome: A comprehensive review of 128 cases. Am J Gastroenterol. 2006;101:2139–46. doi: 10.1111/j.1572-0241.2006.00645.x. [DOI] [PubMed] [Google Scholar]
- 3.Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77:737–42. doi: 10.1002/bjs.1800770707. [DOI] [PubMed] [Google Scholar]
- 4.Langhorst J, Schumacher B, Deselaers T, Neuhaus H. Successful endoscopic therapy of a gastric outlet obstruction due to a gallstone with intracorporeal laser lithotripsy: A case of Bouveret’s syndrome. Gastrointest Endosc. 2000;51:209–13. doi: 10.1016/s0016-5107(00)70421-4. [DOI] [PubMed] [Google Scholar]
- 5.Koulaouzidis A, Moschos J. Bouveret’s syndrome. Narrative review. Ann Hepatol. 2007;6:89–91. [PubMed] [Google Scholar]
- 6.Lassandro F, Romano S, Ragozzino A, et al. Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR. 2005;185:1159–65. doi: 10.2214/AJR.04.1371. [DOI] [PubMed] [Google Scholar]
- 7.Pickhardt PJ, Bhalla S, Balfe DM. Acquired gastrointestinal fistulas: Classification, etiologies, and imaging evaluation. Radiology. 2002;224:9–23. doi: 10.1148/radiol.2241011185. [DOI] [PubMed] [Google Scholar]
- 8.Keller M, Epp C, Meyenberger C, et al. Unspecified abdominal symptoms and pneumobilia: A rare case of gastrointestinal obstruction. Case Rep Gastroenterol. 2014;8:216–20. doi: 10.1159/000364818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret’s syndrome): A review of the literature. Endoscopy. 2005;37:82–7. doi: 10.1055/s-2004-826100. [DOI] [PubMed] [Google Scholar]
- 10.Halabi W, Kang CY, Ketana N, et al. Surgery for gallstone ileus: A nationwide comparison of trends and outcomes. Ann Surg. 2014;259:329–35. doi: 10.1097/SLA.0b013e31827eefed. [DOI] [PubMed] [Google Scholar]
- 11.Gajendran M, Muniraj T, Gelrud A, et al. A challenging case of gastric outlet obstruction (Bouveret’s syndrome): A case report. J Med Case Rep. 2011;5:497. doi: 10.1186/1752-1947-5-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neill C, Colquhoun P, Schlachta CM, Etemad-Rezai R, Jayaraman S. Gastric outlet obstruction secondary to biliary calculi: 2 cases of Bouveret syndrome. Can J Surg. 2009;52:E16–8. [PMC free article] [PubMed] [Google Scholar]


