Abstract
IN BRIEF Recent research has shown that high-intensity interval training (HIIT) can promote improvements in glucose control and cardiovascular health in individuals with type 2 diabetes. This article summarizes the evidence and highlights the ways in which HIIT might be safely implemented as an adjunct to more traditional exercise approaches.
Physical activity and exercise confer wide-ranging health benefits (1). Improvements in cardiovascular risk profile, energy balance, psychological well-being, immune function, strength, and flexibility make physical activity the most important means to improve overall health and well-being for all ages (2). Low cardiorespiratory fitness is a well-known risk factor for chronic diseases such as cardiovascular disease, type 2 diabetes, and obesity, among others (3). In addition, low cardiorespiratory fitness is a major predictor of mortality in individuals with diabetes (4,5). Exercise training is the most effective way to increase cardiorespiratory fitness, and individuals with type 2 diabetes clearly respond to exercise training with this expected adaptation (6). In the context of insulin resistance and type 2 diabetes, exercise provides additional benefits for blood glucose control and is established as an important therapy in the prevention, management, and treatment of type 2 diabetes and its associated complications (7).
The benefits of exercise for improving glucose control over a defined period of training often reflect those accumulated effects from each individual exercise session (1,8). Indeed, a single bout of exercise increases insulin sensitivity for up to 48 hours into recovery, and this is accompanied by improved glycemic control in individuals with type 2 diabetes (9,10). The intensity, duration, and type of exercise are likely to play a key role in the magnitude of the benefits attained. At present, the most effective exercise strategy for improving glucose control and reducing cardiometabolic risk in type 2 diabetes has not been defined. In this review, we will discuss recent evidence that highlights the potential for low-volume, high-intensity interval training (HIIT) to be safely implemented as a time-efficient exercise option for reducing blood glucose levels in individuals with, or at risk for, type 2 diabetes.
Traditional Exercise Approaches
Traditional exercise guidelines have focused on increasing low- to moderate- intensity physical activity in sedentary individuals. The American Diabetes Association (ADA) and American College of Sports Medicine (ACSM) guidelines for physical activity recommend a minimum of 150 minutes/week (or 30 minutes, 5 days/week) of moderate to vigorous physical activity (11). This includes activities such as walking, jogging, and cycling, or anything that causes a sustained increase in heart rate (∼40–60% of maximal aerobic capacity or ∼55–70% maximal heart rate [HRmax]). The guidelines also recommend that patients with type 2 diabetes undertake two to three sessions of resistance training per week and have no more than two consecutive days off between single bouts of exercise.
Both aerobic and resistance exercise have shown modest improvements in glycemic control (12,13), and although the combination may be more effective than either alone (14,15), there is evidence supporting potential added benefits of more vigorous exercise (16–19). For example, in a meta-analysis (6) examining the impact of exercise training on A1C in individuals with type 2 diabetes, exercise intensity was the stronger predictor of improvements in blood glucose control when compared to exercise volume.
It is likely that traditional exercise guidelines have focused on low- to moderate-intensity exercise because activities such as walking are easily achieved and relatively safe. However, such activities are the most common forms because they are the basis of a normal, active lifestyle (20), which does not describe the majority of individuals with type 2 diabetes (11). Such activities of daily living may not be able to provide an appropriate stimulus to increase cardiorespiratory fitness (21). This is particularly true for patients with type 2 diabetes, for whom there is evidence that a self-selected walking pace during exercise may be too low to achieve improvements in key health markers (22). Thus, supervised exercise training involving more vigorous exercise may be the most effective means to improve cardiorespiratory fitness and reduce hyperglycemia in type 2 diabetes.
What Is HIIT?
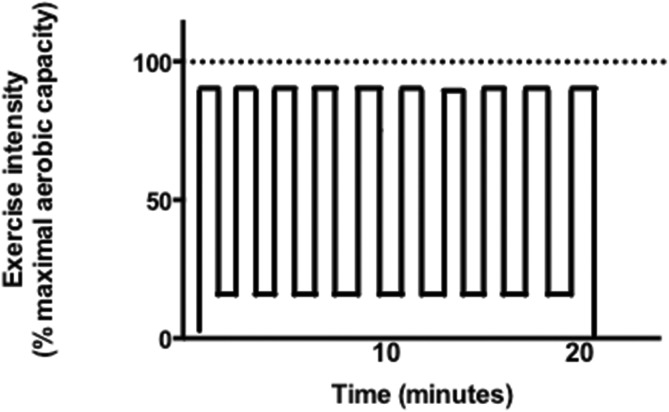
HIIT has attracted attention in the scientific and clinical communities and the popular press for its ability to robustly improve various aspects of cardiometabolic health. HIIT involves alternating between periods of vigorous exercise (which we will define as exercising at ≥70% maximal aerobic capacity) and periods of rest or recovery. Numerous different HIIT protocols have been employed in research studies, involving different numbers, intensity levels, and lengths of the vigorous-intensity portions and/or recovery periods. This makes comparison between HIIT studies inherently difficult. However, it is likely that the “on-off” pattern of exercise allows individuals to more readily perform vigorous exercise because break periods are naturally built in. HIIT may therefore represent an ideal strategy for implementing vigorous exercise in individuals who are unfit or unaccustomed to vigorous-intensity physical activity. Figure 1 graphically depicts the pattern of exercise in a typical HIIT session.
FIGURE 1.
Graphical representation of a typical HIIT protocol. Time is on the horizontal axis and exercise intensity, expressed relative to maximal aerobic capacity (dotted line), is on the vertical axis. The “on” portion of HIIT is typically >70% of maximal aerobic capacity, and these intervals can last from just a few seconds to several minutes. One protocol that has been shown to be feasible, time-efficient, and effective involves 10 × 1 minute at ∼90% maximal aerobic capacity separated by 1-minute rest periods. This protocol is depicted in the figure.
It is important to note that the intensity of the bursts of vigorous exercise that characterize HIIT is not standardized, but rather is based on the individual cardiorespiratory fitness of the exerciser. In this manner, the “on” portion of HIIT for a fit, healthy individual may involve running or sprint cycling, whereas the same relative intensity for the “on” portion for an overweight individual with type 2 diabetes may involve brisk or uphill walking. This is important to recognize because it means that HIIT can be individually tailored and does not have to involve all-out exercise.
Health Benefits of HIIT in People With Type 2 Diabetes
Numerous HIIT protocols have been tested on individuals with coronary artery disease, heart failure, chronic obstructive pulmonary disease, and metabolic syndrome and are reviewed elsewhere (23). Several studies have tested a HIIT protocol involving 4 × 4 minutes of uphill walking at ∼90–95% of maximal aerobic capacity, separated by 3-minute low-intensity walking rests. When compared to energy expenditure–matched, moderate-intensity walking at ∼65% of maximal aerobic capacity, HIIT has generally been found to offer superior cardiovascular benefits. A recent meta-analysis (24) of studies in participants with lifestyle-related metabolic disease reported that the increase in cardiorespiratory fitness after HIIT is approximately double the increase after moderate-intensity continuous training.
The clinical significance of these findings is highlighted by the fact that low cardiorespiratory fitness is an independent predictor of mortality in individuals with and without type 2 diabetes (3–5). Other added benefits of HIIT are improvements in endothelial function, insulin sensitivity, and blood pressure (24).
Studies directly comparing HIIT to traditional, moderate-intensity exercise in people with type 2 diabetes are less common. However, Karstoft et al. (25) recently reported superior effects of HIIT involving free-living interval walking compared to moderate-intensity continuous walking in patients with type 2 diabetes (∼60 years of age, ∼5 years since type 2 diabetes diagnosis, most treated with diet only or metformin, and no history of diabetes complications). Both groups trained for 60 minutes/day on 5 days/week for 16 weeks; therefore, training volume and time commitment were high. The interval walking was based on previous work conducted in older adults in Japan and involved 3-minute intervals at ∼70% of maximal aerobic capacity separated by 3 minutes of low-intensity walking (26), whereas the continuous walking group performed for 60 minutes at ∼55% of maximal aerobic capacity. After training, the interval walking group had greater improvements in body composition, aerobic fitness, and glucose control assessed by continuous glucose monitoring (CGM) (27).
Perhaps more intriguing are emerging data showing that low-volume HIIT can elicit rapid improvements in cardiovascular and metabolic health. Low-volume HIIT involves a substantially lower total exercise volume and time commitment and has therefore been touted as a time-efficient exercise option. Given that lack of time is the number-one reported barrier to regular exercise participation (28), it is possible that low-volume HIIT may be an attractive option for increasing physical activity levels.
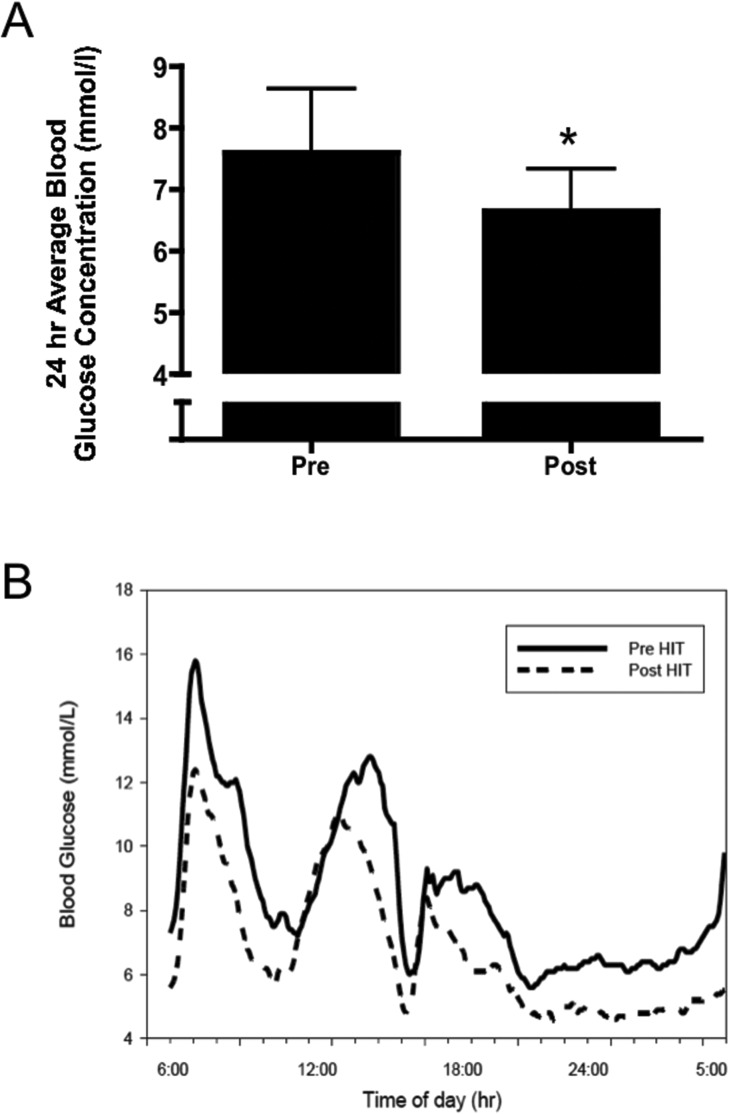
One low-volume HIIT protocol that has shown preliminary effectiveness in patients with type 2 diabetes involves 10 × 1-minute vigorous intensity efforts at ∼90% of maximal aerobic capacity interspersed with 1-minute rest periods. As little as 2 weeks of training in this manner three times per week (i.e., six total exercise sessions in 14 days) was effective for reducing 24-hour mean blood glucose in previously inactive participants with type 2 diabetes (29) (Figure 2). Participants in this study were ∼65 years of age, obese (BMI >30 kg/m2), not on exogenous insulin, and free of diabetes complications. Total exercise time was ∼30 minutes/week within a 75-minute weekly time commitment (including warm-up, cool-down, and rest periods), which is markedly lower than current guidelines.
FIGURE 2.
Low-volume HIIT leads to rapid improvements in glucose control in individuals with type 2 diabetes. A: Average 24-hour blood glucose asessed before (Pre) and after (Post) six sessions of HIIT involving 10 × 1 minute at ∼90% of maximal aerobic capacity over 2 weeks. B: A representative 24-hour continuous glucose monitoring curve from a participant assessed under standardized dietary conditions. Reprinted with permission from Ref. 29.
In another study, Shaban et al. (30) assessed an even lower-volume HIIT protocol involving 4 × 30 seconds at ∼100% of maximal aerobic capacity with 4-minute rest periods in nine patients with type 2 diabetes. Participants were on average ∼40 years of age, the majority (8/9) were taking exogenous insulin, and all were free of diabetes complications. The outcome measures in this small study were limited, but blood glucose was reduced immediately after each session, although there was no difference in fasting insulin or glucose after six sessions in 2 weeks. However, the authors noted that six of the nine participants did see improvements in insulin resistance assessed by fasting homeostasis model assessment scores and argued that this HIIT protocol may be effective for improving metabolic control.
Longer-term studies of low-volume HIIT in type 2 diabetes are limited. Mitranun et al. (31) investigated 12 weeks of HIIT or continuous exercise in 43 patients with type 2 diabetes aged 50–70 years who were on glucose-lowering medications but were not taking exogenous insulin and were free of diabetes complications. HIIT involved a progression to 6 × 1-minute intervals at 85% of maximal aerobic capacity with 4 minutes of low-intensity recovery and was compared to 30 minutes of continuous exercise (65% of maximal aerobic capacity) matched for exercise energy expenditure. Both low-volume HIIT and continuous training improved body fat mass, cardiorespiratory fitness, endothelial function, and fasting blood glucose; however, these benefits were greater in the HIIT group. Moreover, A1C only improved after HIIT.
As discussed above, many of the benefits of exercise for individuals with type 2 diabetes can be attributed to the acute effects of the most recent bout of exercise. A single session of HIIT involving 10 × 1 minute at ∼90% of maximal aerobic power has been shown to significantly reduce postprandial hyperglycemia assessed by CGM in type 2 diabetes patients aged ∼65 years (32). More recent studies have extended these findings to younger overweight or obese individuals at risk for type 2 diabetes and have demonstrated that HIIT may be superior to energy-matched, moderate-intensity continuous exercise for acutely improving glucose control (29). In patients with type 2 diabetes (aged 55–75 years and treated with metformin or combined metformin plus sitaglipin or sulfonylurea), Terada et al. (33) also found that HIIT, when compared to moderate-intensity continuous exercise, produced greater acute reductions in blood glucose assessed by fingerstick samples taken before and after each session during a 12-week training program.
The mechanism by which HIIT improves glucose control may lie in its ability to recruit more muscle fibers and rapidly deplete muscle glycogen levels, thereby promoting a greater increase in post-exercise muscle insulin sensitivity (34). Because the post-exercise increase in muscle insulin sensitivity lasts for ∼24–48 hours after a single bout of exercise, HIIT may be an effective strategy for improving glucose control acutely and over the longer term. Performing HIIT over a longer period of time (e.g., 12–16 weeks) may have the added bonuses of reducing abdominal adipose tissue (35) and increasing lower-body muscle mass (36).
Recent Advances: Less HIIT, Same Effect?
Despite the evidence that low-volume HIIT can improve several markers of health in individuals with or at risk for type 2 diabetes, the characteristics of the optimal HIIT session (e.g., interval number, length, and intensity) are not known. There is a growing trend in HIIT research to explore the minimal amount of exercise that is required to improve cardiometabolic health. In this regard, there is evidence that as little as 1 minute of vigorous exercise performed in a 10-minute training session (3 × 10–20 seconds) done thrice weekly for 6 weeks can improve glucose tolerance in overweight men (37). It remains to be determined whether all the benefits of traditional aerobic exercise can be achieved with such low-volume HIIT and whether this style of exercise is effective for individuals with type 2 diabetes.
Is HIIT Safe?
Because vigorous exercise has been associated with increased risk of acute cardiovascular events, there is concern regarding the safety of implementing HIIT in any clinical population. The ADA recommends 12-lead electrocardiogram (ECG) screening for patients with type 2 diabetes before engaging in any vigorous exercise (11), and, although there is no direct evidence that HIIT is equivalent to continuous vigorous exercise, this precaution is likely appropriate for those individuals interested in trying HIIT. A recent retrospective analysis of ∼5,000 patients over 7 years of supervised cardiac rehabilitation exercise reported a low risk of acute cardiovascular events with HIIT (38). Specifically, the authors reported an event rate of 1 nonfatal heart attack per 23,182 hours of HIIT (38).
More research is needed to directly assess the safety of HIIT in individuals with or at risk for type 2 diabetes. Because of its efficacy and time-efficiency, it would be important to determine whether the increased acute risk of cardiac events with continuous vigorous exercise (39) applies to HIIT, in which there are rest periods naturally built in and protocols can involve only a few seconds or minutes of vigorous exercise.
At this stage, it is advised that individuals with type 2 diabetes undergo an appropriate pre-exercise screening, a 12-lead ECG stress test, and physician clearance before engaging in HIIT, as they would with any vigorous exercise program. It is also recommended that a qualified exercise professional (e.g., ACSM-certified exercise specialist or Canadian Society for Exercise Physiology–certified exercise physiologist) supervise HIIT for individuals with type 2 diabetes. As with any exercise, an appropriate warm-up and cool-down period is important to help reduce the risk of cardiovascular events and musculoskeletal injury.
The majority of the studies examining HIIT in patients with type 2 diabetes have been of short duration (<6 months) and have typically involved individuals ∼60 years of age who were treated with metformin or metformin plus one other glucose-lowering drug, were free of coronary artery disease, and had been cleared for exercise with a 12-lead ECG stress test. Thus, the applicability of HIIT for different subgroups within the type 2 diabetes population (e.g., patients with concomitant heart disease, those who are insulin-treated, and those with peripheral neuropathy) is not known. In the only study to our knowledge to examine HIIT in type 2 diabetes patients with complications, Praet et al. (27) demonstrated that 10 weeks of HIIT (4–8 × 30 seconds of cycling sprints separated by 60 seconds of rest) when added to a resistance training program led to improvements in fitness and reductions in hyperglycemia and exogenous insulin requirements in a group of inactive males (∼60 years of age) with insulin-treated type 2 diabetes and diagnosed polyneuropathy. The authors of this small study reported one overuse injury that limited progression of training intensity, but it is not clear whether this was related to the HIIT or the resistance training. Certainly, more work is needed to examine the feasibility, impact, and safety of HIIT among different subgroups of the type 2 diabetic population.
Putting HIIT into Practice
HIIT could be a smart addition to any exercise program. Whether it is used in place of continuous moderate exercise when time is precious or added to traditional exercise approaches for variety, HIIT has the potential to provide additional health benefits. The most effective interval regimen is not known, but intervals ranging from 10 seconds to 4 minutes at intensities ≥70% of maximal aerobic capacity have been shown to be safe and effective in clinical populations. Depending on the initial fitness and experience of participants, it is advised to use a progression of interval duration, intensity, or number. This could be accomplished initially by adding just a few short periods of “picking up the pace” to a session of continuous moderate-intensity exercise (16).
It is important to reiterate that the intensity of the intervals is relative to participants’ level of fitness or tolerance. Thus, HIIT for a previously inactive older patient with type 2 diabetes might involve simply picking up the pace of walking for 30–60 seconds every few minutes during exercise, whereas an active patient who is already regularly exercising might need to walk uphill at a brisk pace to achieve the correct intensity.
Exercise intensity can be prescribed using a percentage of HRmax, which is assessed during a maximal exercise stress test or estimated as 220 minus age. For example, someone who is 50 years of age has a maximal heart rate of ∼170 bpm. Therefore, interval exercise at 85% HRmax would be at ∼145 bpm during the “on” portion. In our experience, it takes about three to four intervals (if they are 30–60 seconds in duration) to accurately determine whether the intensity of the interval is correct if you are trying to elicit ∼85% HRmax. Alternatively, the rating of perceived exertion (RPE) scale is effective and does not require any specialized equipment. The easiest scale for most people to understand is the Category Ratio-10 (CR-10) scale, which rates overall exertion on a scale from 0 to 10, with 10 being “very, very hard (maximal),” 7 being “very hard,” and 0 being “nothing at all” or resting. An intensity of ∼85% HRmax corresponds to ∼7–8 on the CR-10 scale (40), and we have found that 6–10 × 1-minute intervals at this RPE are well tolerated by participants with type 2 diabetes or prediabetes (16,29).
Most studies have used cycling or uphill walking to achieve the desired intensity. However, in practice, the intervals can be any type of movement, as long as the intensity during the “on” components is increased. Potential modalites of exercise to use for HIIT include walking, cycling, swimming, team sports such as football/soccer, circuit training, and resistance exercise. In the study by Francois et al. (16), an HIIT regimen involving 1-minute intervals that alternated between resistance band exercise and treadmill walking was just as effective as treadmill walking HIIT for reducing blood glucose assessed during the 24 hours after exercise. Interestingly, heart rate was lower during the resistance band exercises, but the RPE was higher. With the assistance of a trained exercise specialist, incorporation of adapted resistance band HIIT may increase the feasibility of HIIT for deconditioned patients or individuals with orthopedic limitations to exercise.
Conclusion
There is mounting evidence supporting the potential cardiometabolic benefits of HIIT in individuals with type 2 diabetes or prediabetes. It should be noted that most studies examining this type of exercise have involved a small number of participants and have been relatively short in duration. More research is needed to evaluate the safety and efficacy of HIIT before widespread adoption, but for individuals who are cleared for vigorous exercise participation, HIIT may be a valuable addition to a health-enhancing exercise program.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Thompson PD, Crouse SF, Goodpaster B, Kelley D, Moyna N, Pescatello L. The acute versus the chronic response to exercise. Med Sci Sports Exerc 2001;33:S438–S445 [DOI] [PubMed] [Google Scholar]
- 2.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol 2012;2:1143–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paffenbarger RS Jr, Lee I-M. Physical activity and fitness for health and longevity. Res Q Exerc Sport 1996;67:S11–S28 [DOI] [PubMed] [Google Scholar]
- 4.Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med 2000;132:605–611 [DOI] [PubMed] [Google Scholar]
- 5.Church TS, Cheng YJ, Earnest CP, et al. Exercise capacity and body composition as predictors of mortality among men with diabetes. Diabetes Care 2004;27:83–88 [DOI] [PubMed] [Google Scholar]
- 6.Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 2001;286:1218–1227 [DOI] [PubMed] [Google Scholar]
- 7.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care 2004;27:2518–2539 [DOI] [PubMed] [Google Scholar]
- 8.Horowitz JF. Exercise-induced alterations in muscle lipid metabolism improve insulin sensitivity. Exerc Sport Sci Rev 2007;35:192–196 [DOI] [PubMed] [Google Scholar]
- 9.Devlin JT, Hirshman M, Horton ED, Horton ES: Enhanced peripheral and splanchnic insulin sensitivity in NIDDM men after single bout of exercise. Diabetes 1987;36:434–439 [DOI] [PubMed] [Google Scholar]
- 10.Manders RJ, Van Dijk JW, van Loon LJ. Low-intensity exercise reduces the prevalence of hyperglycemia in type 2 diabetes. Med Sci Sports Exerc 2010;42:219–225 [DOI] [PubMed] [Google Scholar]
- 11.Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association joint position statement. Diabetes Care 2010;33:e147–e167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bacchi E, Negri C, Targher G, et al. Both resistance training and aerobic training reduce hepatic fat content in type 2 diabetic subjects with nonalcoholic fatty liver disease (the RAED2 randomized trial). Hepatology 2013;58:1287–1295 [DOI] [PubMed] [Google Scholar]
- 13.van Dijk JW, Manders RJF, Tummers K, et al. Both resistance-and endurance-type exercise reduce the prevalence of hyperglycaemia in individuals with impaired glucose tolerance and in insulin-treated and non-insulin-treated type 2 diabetic patients. Diabetologia 2011;55:1273–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuff DJ, Meneilly GS, Martin A, Ignaszewski A, Tildesley HD, Frohlich JJ. Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diabetes Care 2003;26:2977–2982 [DOI] [PubMed] [Google Scholar]
- 15.Sigal RJ, Kenny GP, Boulé NG, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med 2007;147:357–369 [DOI] [PubMed] [Google Scholar]
- 16.Francois ME, Baldi JC, Manning PJ, et al. ‘Exercise snacks’ before meals: a novel strategy to improve glycaemic control in individuals with insulin resistance. Diabetologia 2014;57:1437–1445 [DOI] [PubMed] [Google Scholar]
- 17.Helgerud J, Hoydal K, Wang E, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 2007;39:665–671 [DOI] [PubMed] [Google Scholar]
- 18.Little JP, Jung ME, Wright AE, Wright W, Manders RJ, Effects of high-intensity interval exercise versus continuous moderate-intensity exercise on postprandial glycemic control assessed by continuous glucose monitoring in obese adults. Appl Physiol Nutr Metab 2014;39:835–841 [DOI] [PubMed] [Google Scholar]
- 19.Tjønna AE, Lee SJ, Rognmo Ø, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome. Circulation 2008;118:346–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crespo CJ, Keteyian SJ, Heath GW, Sempos CT. Leisure-time physical activity among US adults: results from the Third National Health and Nutrition Examination Survey. Arch Intern Med 1996;156:93–98 [PubMed] [Google Scholar]
- 21.Winett RA, Carpinelli RN. Examining the validity of exercise guidelines for the prevention of morbidity and all-cause mortality. Ann Behav Med 2000;22:237–245 [DOI] [PubMed] [Google Scholar]
- 22.Johnson ST, Boule NG, Bell GJ, Bell RC. Walking: a matter of quantity and quality physical activity for type 2 diabetes management. Appl Physiol Nutr Metab 2008;33:797–801 [DOI] [PubMed] [Google Scholar]
- 23.Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med 2012;42:489–509 [DOI] [PubMed] [Google Scholar]
- 24.Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Brit J Sports Med 2014;48:1227–1234 [DOI] [PubMed] [Google Scholar]
- 25.Karstoft K, Winding K, Knudsen SH, et al. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: a randomized, controlled trial. Diabetes Care 2013;36:228–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nose H, Morikawa M, Yamazaki T, et al. Beyond epidemiology: field studies and the physiology laboratory as the whole world. J Physiol 2009;587:5569–5575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Praet SFE, Jonkers RAM, Schep G, et al. Long-standing, insulin-treated type 2 diabetes patients with complications respond well to short-term resistance and interval exercise training. Eur J Endocrinol 2008;158:163–172 [DOI] [PubMed] [Google Scholar]
- 28.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 2002;34:1996–2001 [DOI] [PubMed] [Google Scholar]
- 29.Little JP, Gillen JB, Percival M, et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol 2011;111:1554–1560 [DOI] [PubMed] [Google Scholar]
- 30.Shaban N, Kenno K, Milne K. The effects of a 2 week modified high intensity interval training program on the homeostatic model of insulin resistance (HOMA-IR) in adults with type 2 diabetes. J Sports Medicine Phys Fitness 2014;54:203–209 [PubMed] [Google Scholar]
- 31.Mitranun W, Deerochanawong C, Tanaka H, Suksom D. Continuous vs interval training on glycemic control and macro‐and microvascular reactivity in type 2 diabetic patients. Scand J Med Sci Sports 2014;24:69–76 [DOI] [PubMed] [Google Scholar]
- 32.Gillen JB, Little JP, Punthakee Z, Tarnopolsky MA, Riddell MC, Gibala MJ. Acute high-intensity interval exercise reduces the postprandial glucose response and prevalence of hyperglycaemia in patients with type 2 diabetes. Diabetes Obes Metab 2012;14:575–577 [DOI] [PubMed] [Google Scholar]
- 33.Terada T, Friesen A, Chahal BS, Bell GJ, McCargar LJ, Boule NG. Exploring the variability in acute glycemic responses to exercise in type 2 diabetes. J Diabetes Res 2013;2013:591574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts CK, Little JP, Thyfault JP. Modification of insulin sensitivity and glycemic control by activity and exercise. Med Sci Sports Exerc 2013;45:1868–1877 [DOI] [PubMed] [Google Scholar]
- 35.Boutcher SH: High-intensity intermittent exercise and fat loss. J Obes 2011;2011:868305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gillen JB, Percival ME, Ludzki A, Tarnopolsky MA, Gibala M. Interval training in the fed or fasted state improves body composition and muscle oxidative capacity in overweight women. Obesity 2013;21:2249–2255 [DOI] [PubMed] [Google Scholar]
- 37.Metcalfe RS, Babraj JA, Fawkner SG, Vollaard NB. Towards the minimal amount of exercise for improving metabolic health: beneficial effects of reduced-exertion high-intensity interval training. Eur J Appl Physiol 2012;112:2767–2775 [DOI] [PubMed] [Google Scholar]
- 38.Rognmo Ø, Moholdt T, Bakken H, et al. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation 2012;126:1436–1440 [DOI] [PubMed] [Google Scholar]
- 39.Thompson PD. The cardiovascular complications of vigorous physical activity. Arch Intern Med 1996;156:2297–2302 [PubMed] [Google Scholar]
- 40.Borg GA: Psychophysical basis of perceived exertion. Med Sci Sports Exerc 1982;14:377–381 [PubMed] [Google Scholar]