Abstract
Children with special health care needs are believed to be susceptible to inequities in health and health care access. Within the group with special needs, there is a smaller group of children with medical complexity: children who require medical services beyond what is typically required by children with special health care needs. We describe health care inequities for the children with medical complexity compared to children with special health care needs but without medical complexity, based on a secondary analysis of the 2005–06 and 2009–10 National Survey of Children with Special Health Care Needs. The survey examines the prevalence, health care service use, and needs of children and youth with special care needs, as reported by their families. The inequities we examined were those based on race or ethnicity, primary language in the household, insurance type, and poverty status. We found that children with medical complexity were twice as likely to have at least one unmet need, compared to children without medical complexity. Among the children with medical complexity, uninsured status was associated with more unmet needs than privately insured status. We conclude that medical complexity itself can be a primary determinant of unmet needs.
Keywords: Chronic Care, Children's Health, Disparities, Maternal And Child Health
Children with medical complexity are the greatest users of health care services among children because of the presence of multiple chronic conditions, functional limitations, and family-identified service needs.[1,2] Children with medical complexity are increasingly recognized as a distinct subgroup within children and youth with special health care needs.[3] These children require medical services beyond those that are typically required because of a chronic medical condition.[4]
An example of a child with medical complexity is one who has a genetic syndrome and a developmental delay, depends on supplemental oxygen for adequate respiration and a feeding tube for nutrition, and receives chronic care from five subspecialists. Children with medical complexity are particularly distinguished by extraordinary family burden and unmet health care needs, even when compared to other children with special health care needs. In a national sample of families of children with medical complexity, over half reported that they had financial problems and that a family member had stopped working because of the child's health. Most of the families reported having at least ten physician visits and out-of-pocket health care costs of more than $1,000 annually.[5]
Children and youth with special health care needs in general are felt to be susceptible to inequities in health and health care access. This reflects social determinants of health such as poor housing or underperforming schools that favor specific social groups while leaving others at a disadvantage in many walks of life, including health outcomes.[6] Health inequities can be defined as systemic disparities in health resulting from social and economic policies that create barriers both to accessing health services and to healthy outcomes. The US government's Healthy People 2020 has the overarching goals of eliminating health disparities and achieving health equity among all groups in the United States, including those defined by disability status or special health care needs.[7]
Inequities in health care access remain prevalent among children generally.[8] Children and youth with special health care needs whose condition affects daily activities or who are either non-Hispanic black or Hispanic, reside in households where English is not the primary language, or have lower household income have higher unmet health care needs and are less likely to have access to a medical home, compared to children who are non-Hispanic white, reside in households where English is the primary language, and have higher household income.[9–11] Similar inequities in access to care are seen among non-Hispanic black children and youth with special health care needs who have chronic emotional and behavioral problems[12] and autism spectrum disorders.[13]
It is unknown how previously described health care inequities for children and youth with special health care needs may differ in the presence of additional medical complexity. Families of children and youth with special health care needs and disabilities report more unmet needs than families of such children and youth who do not have disabilities.[14] Greater condition severity among children and youth with special health care needs has been associated with reduced receipt of specialty care in families reporting a household income of 200–299 percent of the federal poverty level.[15]
Multiple societal factors likely determine health care inequities, and specific attention to the needs of underserved groups is necessary to achieve health equity.[6] Knowing if additional inequities in health care needs were associated with medical complexity, and how these inequities might affect family and health outcomes, would permit accurate, patient-centered design of care models for the highest users of pediatric resources.
The objective of this article is to determine the association between variables known to be associated with inequities in health care needs and the medical complexity status of children and youth with special health care needs. For this analysis, we defined medical complexity as having a need for medical care, having a multitude of needs across various health service domains, and having seen at least two specialists in the previous year. A slightly expanded definition appears in the Variables section.
The inequities in health care access we examined were those based on race or ethnicity, primary language spoken in the home, insurance type, and poverty status. We chose these characteristics based on the priorities in Healthy People 2020[7] and a literature review of inequities among children and youth generally and among those with special health care needs.[16–19]
We hypothesized that children with medical complexity would have more unmet needs, compared to children and youth with special health care needs but without medical complexity. We also hypothesized that—in contrast to children and youth with special health care needs but without medical complexity—a higher number of unmet needs would be associated with variables traditionally associated with health care inequities, both among children and youth generally and among those with special health care needs.
Study Data And Methods
Our study was a secondary data analysis of a combined data set containing information from the 2005–06 and the 2009–10 National Survey of Children with Special Health Care Needs. The survey is conducted by the National Center for Health Statistics, using random-digit dialing of landline telephone numbers supplemented with an independent sample of cell-phone numbers. The survey estimates the national- and state-level prevalence of children and youth with special health care needs, specific family-reported conditions, service use, and needs.
Parents first respond to questions regarding the special health care needs of each child in the household using the National Survey of Children with Special Health Care Needs Screener, a five-question instrument that identifies special needs.[20,21] The five items or domains on the screener are a need for prescription medication, a need for medical care, the presence of a functional limitation, a need for special therapies, and the presence of treatment or counseling for a developmental or behavioral problem.
Parents with a child “screening in” by having one or more positive responses then participate in the full National Survey of Children with Special Health Care Needs. In households with more than one child “screening in,” one child is selected at random to be the focus of the full survey's questions.
We combined the 2005–06 and 2009–10 surveys to increase the number of study subjects identified as having medical complexity. We limited our analyses to variables that were in both surveys. The only notable difference in the survey's administration between the two periods was the addition of a cell-phone sample in the 2009–10 survey. Findings generated from an analysis of the 2009–10 survey alone differed from those produced by an analysis of the combined surveys only with regard to statistical significance.
The National Survey of Children with Special Health Care Needs is publicly available and deidentified. Thus, the study was exempt from review by the Institutional Review Board at the University of Arkansas for Medical Sciences.
Variables
The main outcome of interest was the number of unmet health care needs. This measure is known to be elevated with an increased number of chronic conditions in children and has previously been shown to be associated with several determinants of health inequity among children generally and among children and youth with special health care needs—specifically, income, language, insurance, and race or ethnicity.[16–19]
The National Survey of Children with Special Health Care Needs lists fourteen possible health care needs that could be unmet. These are preventive care; specialist care; preventive dental care; other dental care; prescription medicine; occupational, physical, or speech therapy; mental health care; substance abuse (for children ages 8–17 only); home health care; eyeglasses or vision care; hearing aids or hearing care; mobility aids or devices; communication aids; and durable medical equipment. An unmet need was identified when the parent responding to the survey both answered “yes” to a question asking if a child needed a specific service and reported not receiving that service. We constructed an aggregated variable of total unmet needs for each child, with a range from 0 to 14.
The main predictor variable was medical complexity. We adapted a previously described method of using a combination of reported service needs to define medical complexity. The method, although not standardized, aligns the criteria for defining medical complexity with enrollment criteria for clinical services that target children with medical complexity.[5]
To meet the definition of a child with medical complexity, the child must meet all of the following criteria: a need for medical care, evidenced by a positive response to the medical care question on the National Survey of Children with Special Health Care Needs Screener; multiple needs across different domains, as evidenced by a positive response to at least three of the remaining four screener questions; and having seen at least two specialists in the previous year.
In the previously cited method that used data from the 2005–06 National Survey of Children with Special Health Care Needs, being dependent on medical technology or equipment was also a requirement for meeting the definition. However, the question asking about a need for medical supplies, which was a component of the previous method, was not asked in the 2009–10 survey. Thus, we eliminated that as a requirement. All children and youth with special health care needs who did not meet the criteria for medical complexity were defined as children without medical complexity.
Selected demographic characteristics associated with inequities in health and health care access for children and youth with special health care needs were used as covariates in the analytic model. The demographic variables were race/ethnicity, primary language spoken in household, income (as a percent of poverty), and insurance type. In all statistical models, results were also adjusted to account for the child's age and sex and for the number of children and adults residing in the household.
Analytic Plan
Weighted categorical percentages for the outcome, main predictor, and covariates for children with medical complexity and children without medical complexity are presented. Differences in the outcomes, main predictor, and covariates between children with medical complexity and those without it were determined by Rao-Scott chi-square tests of association at a significance level of α = 0.05.
Categorical differences of effect size within variables are presented using unadjusted odds ratios from logistic regression models, with medical complexity status as the outcome and each covariate in a separate model. The percentages of unmet needs by children without medical complexity and those with it, by inequity variable category, are also presented with Rao-Scott chi-square tests of association at a significance level of α = 0.05.
We were primarily interested in the three-way association between unmet needs, medical complexity status, and the sociodemographic covariates that are known to be associated with inequities in health. We also wanted to determine whether the association among those covariates was more highly associated with unmet needs in the case of children with medical complexity, compared to children without medical complexity. To investigate this question, we used a form of statistical regression stratification that models all parameters simultaneously. This produces common model fit parameters but separate regression parameters for children with medical complexity and those without it.
This mixture model was able to compare the parameters and incidence rate ratios (IRRs) across known classes that were assigned. The IRR is a measure that identifies how many more unmet needs were experienced for one variable category, compared to a reference category.
The number of unmet needs, ranging from 0 to 14, was the outcome variable, which was then modeled as a Poisson distributed count variable. A Poisson mixture regression model was fit with known class assignment (children with medical complexity and those without it). This model produced separate, but comparable, IRRs. The model was adjusted for all covariates and accounted for the complex survey design and weights.
Because of the highly skewed distribution of unmet needs, we also tested a negative binomial and a zero-inflated Poisson model. The findings were similar. Because of the lowest log-likelihood and Bayesian information criterion values, we report the findings of the Poisson regression model.
Descriptive results were obtained using SAS Enterprise Guide, version 4.3. The Poisson mixture regression model results were obtained using Mplus, version 7.11.[22]
Limitations
Our study had several limitations. Research supports the use of the National Survey of Children with Special Health Care Needs Screener to assess complexity.[21] However, identifying all children with medical complexity would require the use of a combination of administrative and survey data to address all domains that drive the use of health care resources.
There is likely variation in medical care needs for children without medical complexity that we did not account for in our analyses. Our definition of children with medical complexity requires reporting having seen two specialists, but this may not account for children who could not see necessary specialists because of access issues.
All of the data were survey-derived, which accounted for variance in the use of health care[23] but not for all variance. We had a relatively small sample of children with medical complexity, even after we combined the two National Surveys of Children with Special Health Care Needs. Thus, we may have had insufficient power to detect significant findings for some of our variables.
Our study findings were similar to findings based on the 2009–10 survey alone. However, there may be unmeasured differences between respondents to the two surveys.
Finally, the findings were limited to the reported fourteen unmet needs. It is possible that additional unmet needs with important sociodemographic relationships were not measured.
Study Results
We identified 481,739 children with medical complexity and 17,300,697 children without medical complexity from the combined 2005–06 and 2009–10 National Surveys of Children with Special Health Care Needs. Children with medical complexity were disproportionately younger than children without medical complexity: 33.0 percent of children with medical complexity were ages 0–5 years, compared to 21.0 percent of children without medical complexity (Exhibit 1). Compared to children without medical complexity, a smaller proportion of children with medical complexity were non-Hispanic black (10.7 percent versus 16.9 percent), and a larger proportion had Medicaid (42.5 percent versus 30.8 percent).
Exhibit 1. Children's Demographic Characteristics And Unmet Needs, By Medical Complexity.
| Characteristic | Children with medical complexity | Children without medical complexity | Odds ratio | ||
|---|---|---|---|---|---|
|
| |||||
| Number | Percent | Number | Percent | ||
| Age (years) | |||||
|
| |||||
| 0–5 | 489 | 33.0 | 12,038 | 21.0 | 2.18**** |
| 6–11 | 649 | 37.5 | 24,916 | 38.0 | 1.37 |
| 12–17 | 540 | 29.5 | 28,346 | 41.0 | Ref |
|
| |||||
| Sex | |||||
|
| |||||
| Male | 1,047 | 60.6 | 39,027 | 59.4 | 1.05 |
| Female | 631 | 39.4 | 26,273 | 40.6 | Ref |
|
| |||||
| Race/ethnicity | |||||
|
| |||||
| Non-Hispanic white | 1,231 | 65.3 | 47, 186 | 63.2 | Ref** |
| Non-Hispanicblack | 148 | 10.7 | 6,877 | 16.9 | 0.61 |
| Hispanic | 186 | 16.6 | 6,875 | 14.0 | 1.15 |
| Other | 113 | 7.5 | 4,362 | 5.9 | 1.22 |
|
| |||||
| Primary language | |||||
|
| |||||
| English | 1,607 | 91.1 | 63,274 | 94.9 | Ref*** |
| Other | 71 | 8.9 | 2,026 | 5.1 | 1.81 |
|
| |||||
| Insurance | |||||
|
| |||||
| Private | 557 | 30.7 | 40,590 | 56.2 | Ref**** |
| Medicaid | 627 | 42.5 | 16,546 | 30.8 | 2.52 |
| Uninsured | 21 | 1.0 | 1,978 | 3.3 | 0.56 |
| Other | 473 | 25.8 | 6, 186 | 9.7 | 4.86 |
|
| |||||
| Income (percent of federal poverty level) | |||||
|
| |||||
| Less than 200 | 738 | 51.2 | 23,095 | 42.1 | 1.67**** |
| 200–299 | 293 | 14.3 | 11,376 | 16.1 | 1.22 |
| 300–399 | 239 | 13.9 | 9,937 | 13.3 | 1.44 |
| 400 or more | 408 | 20.7 | 20,892 | 28.5 | Ref |
|
| |||||
| Number of unmet needs | |||||
|
| |||||
| 0 | 946 | 55.8 | 54,273 | 80.9 | Ref**** |
| 1 | 369 | 20.0 | 7,222 | 12.1 | 2.38 |
| 2 | 179 | 12.7 | 2,389 | 4.4 | 4.17 |
| 3 or more | 184 | 11.5 | 1,416 | 2.6 | 6.52 |
SOURCE Authors' analysis of data from the 2005–06 and 2009–10 National Survey of Children with Special Health Care Needs. NOTES There were 1,678 children with medical complexity (weighted number: 481,739) and 65,300 children without medical complexity (weighted number: 17,300,697). Significance indicators are results from Rao-Scott chi-square tests.
p < 0.05
p < 0.01
p < 0.001
At least one unmet need was reported by 44.2 percent of families of children with medical complexity, compared to 19.1 percent of families of children without medical complexity (Exhibit 1). Three or more unmet needs were reported by 11.5 percent of families of children with medical complexity, but by only 2.6 percent of families of children without medical complexity.
Overall, children with medical complexity had a higher percentage of unmet health care needs than children without medical complexity, regardless of race/ethnicity, insurance coverage, and household income in relation to poverty level (Exhibit 2). We found that children with medical complexity had disproportionately higher unmet needs than children without medical complexity across all categories of race and ethnicity. In families whose primary language was English, children with medical complexity had greater unmet needs than children without medical complexity. However, we found no significant difference in unmet needs between the two groups in families with a different primary language.
Exhibit 2. Number Of Children's Unmet Needs, By Medical Complexity And Variables Sensitive To Health Care Inequity.
| Category | Medical complexity | Number of unmet needs | |||
|---|---|---|---|---|---|
|
| |||||
| 0 | 1 | 2 | 3 or more | ||
| Race or ethnicity | |||||
|
| |||||
| Non-Hispanic white | Yes**** | 58.7% | 21.8% | 11.1% | 8.4% |
| No | 83.7 | 10.3 | 4.0 | 2.0 | |
| Non-Hispanic black | Yes**** | 52.0 | 17.7 | 13.2 | 17.0 |
| No | 76.7 | 14.6 | 5.6 | 3.1 | |
| Hispanic | Yes**** | 58.7 | 16.6 | 7.8 | 16.9 |
| No | 74.8 | 16.4 | 4.7 | 4.2 | |
| Other | Yes**** | 29.9 | 14.5 | 37.1 | 18.5 |
| No | 77.3 | 14.2 | 4.9 | 3.6 | |
|
| |||||
| Primary language | |||||
|
| |||||
| English | Yes**** | 55.4 | 19.9 | 12.9 | 11.9 |
| No | 81.3 | 11.9 | 4.4 | 2.5 | |
| Other | Yes | 60.4 | 21.1 | 10.7 | 7.8 |
| No | 74.1 | 16.2 | 5.6 | 4.2 | |
|
| |||||
| Insurance | |||||
|
| |||||
| Private | Yes**** | 62.2 | 16.4 | 10.7 | 10.7 |
| No | 87.0 | 8.8 | 2.9 | 1.2 | |
| Medicaid | Yes**** | 50.8 | 20.5 | 16.2 | 12.4 |
| No | 73.7 | 16.5 | 6.3 | 3.6 | |
| Uninsured | Yes*** | 24.3 | 17.9 | 8.6 | 49.2 |
| No | 49.6 | 21.7 | 10.9 | 17.8 | |
| Other | Yes**** | 57.7 | 23.4 | 9.5 | 9.5 |
| No | 78.8 | 14.3 | 4.9 | 2.0 | |
|
| |||||
| Income (percent of federal poverty level) | |||||
|
| |||||
| Less than 200 | Yes**** | 53.0 | 22.3 | 10.8 | 13.9 |
| No | 72.7 | 16.3 | 6.6 | 4.3 | |
| 200–299 | Yes**** | 62.6 | 18.9 | 13.1 | 5.5 |
| Non | 79.5 | 13.5 | 4.3 | 2.7 | |
| 300–399 | Yes**** | 50.8 | 12.9 | 22.8 | 13.5 |
| No | 86.1 | 9.4 | 3.1 | 1.4 | |
| 400 or more | Yes**** | 61.6 | 19.7 | 10.3 | 8.5 |
| No | 91.3 | 6.4 | 1.8 | 0.5 | |
SOURCE Authors' analysis of data from the 2005–06 and 2009–10 National Survey of Children with Special Health Care Needs. NOTES “Yes” is children with medical complexity. “No” is children without medical complexity. Significance indicators are results from Rao-Scott chi-square tests.
p < 0.01
p < 0.001
For all types of insurance, children with medical complexity had a greater number of unmet needs, compared to children without medical complexity who had the same insurance status (Exhibit 2). Of the children with medical complexity who were uninsured, 49.2 percent had three or more unmet needs.
Similarly, for all household income levels, children with medical complexity had a greater number of unmet needs, compared to children without medical complexity (Exhibit 2). Even at the highest income level (400 percent or more of poverty), only 61.6 percent of families of children with medical complexity reported that they had no unmet health care needs.
Among children without medical complexity, race/ethnicity, income (as a percentage of poverty), and insurance coverage were all associated with a higher number of unmet needs. Specifically, Hispanic families reported 27 percent more unmet needs (IRR: 1.27) and families in the “other” race or ethnicity category reported 29 percent more unmet needs (IRR: 1.29), compared to non-Hispanic white families (Exhibit 3). No significant difference in unmet needs was found when we compared non-Hispanic black families to non-Hispanic white families.
Exhibit 3. Incidence Rate Ratios Comparing The Number Of Unmet Needs, By Determinants Of Health Care Inequity For Children Without Medical Complexity.
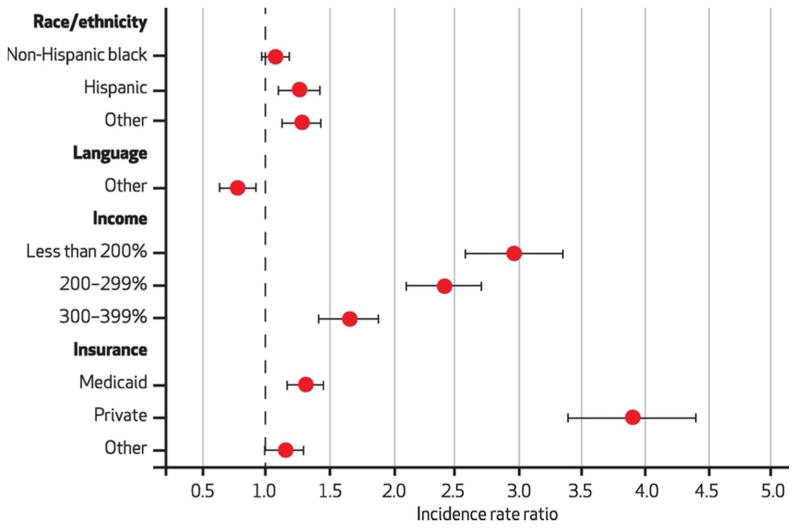
SOURCE Authors' analysis of data from the 2005–06 and 2009–10 National Survey of Children with Special Health Care Needs. NOTES The reference groups are the following: for race or ethnicity, non-Hispanic white; for primary language, English; for income (as percentage of the federal poverty level), 400 percent or more; for insurance, private. The whiskers denote 95% confidence intervals. An incidence rate ratio of 1 would indicate the same number of unmet needs that the reference group had. A ratio of greater than 1 indicates more unmet needs than the reference group had, and a ratio of less than 1 indicates fewer unmet needs.
For children without medical complexity, all families with lower income levels than the reference group (those with a household income of at least 400 percent of poverty) reported higher unmet needs. For example, families with a household income of less than 200 percent of poverty reported two and a half times the number of unmet needs (IRR: 2.97) as those reported by with families in the reference group (Exhibit 3). Compared with families who had private insurance, families with Medicaid reported 32 percent more unmet needs, and families who were uninsured reported almost four times the number of unmet needs. In contrast, having a primary language other than English was predictive of 22 percent fewer unmet needs.
For children with medical complexity, there were fewer significant differences in reports of unmet need according to race/ethnicity, primary language spoken in the household, income level, or insurance type. Hispanic families (IRR: 1.48) reported similar numbers of unmet needs compared to non-Hispanic white families. We found an increased number of unmet needs (IRR: 1.84) for children in the “other” race/ethnicity category, compared to non-Hispanic white children.
Primary language was not predictive of unmet needs among children with medical complexity, nor was income level or having Medicaid (Exhibit 4). However, being uninsured was.
Exhibit 4. Incidence Rate Ratios Comparing The Number Of Unmet Needs, By Determinants Of Health Care Inequity For Children With Medical Complexity.
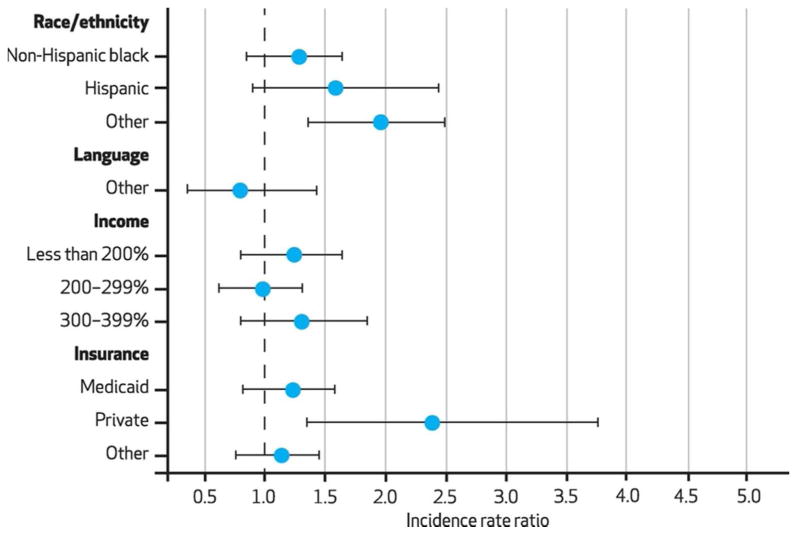
SOURCE Authors' analysis of data from the 2005–06 and 2009–10 National Survey of Children with Special Health Care Needs. NOTES The reference groups are the following: for race or ethnicity, non-Hispanic white; for primary language, English; for income (as percentage of the federal poverty level), 400 percent or more; for insurance, private. The whiskers denote 95% confidence intervals. For a description of incidence rate ratios, see the Notes to Exhibit 3.
Discussion
Almost half of the families of children with medical complexity reported at least one unmet health care need. Such families have previously reported a high number of unmet health care needs,[5] and our results confirmed these findings. However, we were surprised that our research revealed that several social determinants generally associated with inequities were not found when examining children with medical complexity. When we examined those children separately from other children and youth with special health care needs, we found that lower income, Hispanic ethnicity, and having Medicaid were not associated with higher unmet needs.
Our findings call attention to the role of medical complexity itself as a potential and important determinant of health care inequities. The overall level of unmet need was high even in children with medical complexity who had favorable social determinants. Children with medical complexity residing in households with incomes of at least 400 percent of poverty had more unmet need than children without medical complexity residing in households with incomes of less than 200 percent of poverty. Similarly, non-Hispanic white children with medical complexity had more unmet needs than non-Hispanic black children without medical complexity. For children and youth with special health care needs, medical complexity was a larger driver of inequity than race and income.
These findings are consistent with literature showing that families of children with medical complexity report a high prevalence of financial difficulties, employment instability, and stress.[5,24] This prevalence may be related to the high level of unmet health care needs.
Two of our findings deserve additional discussion. First, for uninsured children, the number of unmet needs was higher across both children with medical complexity and children without medical complexity, which suggests that a lack of insurance is a major driver of unmet needs.[25]
Second, we found no difference in reported unmet needs between the two groups of children when we analyzed families whose primary language was not English. Given the likely inequities in health status, our finding probably reflects differing recognitions of need, resulting from either reduced health care access or different interpretations of the need for health care.[26,27] However, we did not find a significant difference in unmet needs between non-English-speaking and English-speaking households of children with medical complexity. It is possible that previously reported differences in recognition of health care need among ethnic groups and households with different primary languages may not exist in the face of medical complexity, because complexity is the primary driver of health care inequity.
Our findings suggest that policies that target traditional determinants of health care inequities may be more appropriate for children without medical complexity than for children with medical complexity. This study has important policy implications by highlighting the need to focus on children with medical complexity across the socioeconomic spectrum as a distinct group with high levels of unmet need.
Ensuring health equity may require policies that focus on both medical and nonmedical determinants of health, such as living conditions, health promotion, and social acceptance.[19] Healthy People 2020 suggests that the health of people with disabilities, some of whom have medical complexity, should be addressed by improving conditions of daily life, increasing health care and opportunities for persons with disabilities, and raising public awareness about determinants of health for people with disabilities.[7]
There are several potential strategies to reduce inequities experienced by children with medical complexity that do not focus on the typical social determinants of health. The optimal care system for these children is believed to require coordination of care across the continuum.[2]
Both models of care that are community based[28] and those that are based on tertiary care centers have arisen to address the needs of children with medical complexity.[29] Efforts to reform health care policy are encouraging the expansion of medical homes based on primary care and of regional health homes to extend appropriately targeted services within communities.[1]
With appropriate up-front payment support, such as per member per month fees to support encounters that are not face to face, and with system integration that supports primary care within accountable care organizations,[30] comprehensive care frameworks such as the medical home[31] or additional tertiary care programs for children with medical complexity[2] may be able to focus on the needs of such children and address health inequities for all children in general.[32] In one sense, this is a return to the future, since the American Academy of Pediatrics called for a medical home for children, particularly those with a chronic condition, back in 1967.[33,34]
The Affordable Care Act, by prioritizing the development of patient-centered medical homes and health homes, emphasizes financial incentives for care coordination and population management of children with medical complexity. Comprehensive health insurance might also mitigate health care inequities.[32,35] Enhanced access to secondary health care coverage from public sources that provide wrap-around coverage to qualifying middle-income children with medical complexity may help address some of the unmet needs we found in this income group, by reducing underinsurance and increasing provider access.[36,37]
Additional research could focus on discovering effective treatments for complex medical conditions that could reduce the need for potentially preventable emergency department visits and hospitalizations.
Conclusion
Children with medical complexity are more likely to have more unmet needs than children without medical complexity. However, among children with medical complexity, we did not find inequity in unmet needs based on primary language, income level, or having Medicaid. Among children without medical complexity, there were numerous examples of inequity in unmet needs based on the same demographic and socioeconomic variables. Our findings suggest that medical complexity itself is a primary determinant of inequities, independent of the traditional social determinants of health.
Acknowledgments
The study findings were presented in part at the Pediatric Academic Societies Annual Meeting in Washington, D.C., May 5, 2013. Dennis Kuo and Anthony Goudie were supported by the National Center for Advancing Translational Sciences (Grant Nos. 8 KL2 TR000063-04 and 8 UL1 TR000039-04).
Contributor Information
Dennis Kuo, Email: dzkuo@uams.edu, University of Arkansas for Medical Sciences, in Little Rock.
Anthony Goudie, University of Arkansas for Medical Sciences.
Eyal Cohen, Hospital for Sick Children, University of Toronto, in Ontario.
Amy Houtrow, University of Pittsburgh, in Pennsylvania.
Rishi Agrawal, Ann and Robert H. Lurie Children's Hospital Northwestern University Feinberg School of Medicine, both in Chicago, Illinois.
Adam C. Carle, Cincinnati Children's Hospital Medical Center and the University of Cincinnati, in Ohio.
Nora Wells, Family Voices, Inc., working in Lexington, Massachusetts.
Notes
- 1.Berry JG, Agrawal RK, Cohen E, Kuo DZ. The landscape of medical care for children with medical complexity. Overland Park (KS): Children's Hospital Association; 2013. Jun, Internet. [cited 2014 Oct 6]. (Special Report). Available from: http://www.childrenshospitals.net/AM/Template.cfm?Section=Home3&Template=/CM/ContentDisplay.cfm&ContentlD=67046. [Google Scholar]
- 2.Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SKM, Simon TD, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–38. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry JG, Bloom S, Foley S, Palfrey JS. Health inequity in children and youth with chronic health conditions. Pediatrics. 2010;126(Suppl 3):S111–9. doi: 10.1542/peds.2010-1466D. [DOI] [PubMed] [Google Scholar]
- 4.McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck PW, et al. A new definition of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):137–40. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 5.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165(11):1020–6. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braveman PA. Monitoring equity in health and healthcare: a conceptual framework. J Health Popul Nutr. 2003;21(3):181–92. [PubMed] [Google Scholar]
- 7.HealthyPeople.gov. Disparities. Washington (DC): Department of Health and Human Services; Internet. [last updated 2014 Oct 6; cited 2014 Oct 6]. Available from: http://www.healthypeople.gov/2020/about/disparitiesAbout.aspx. [Google Scholar]
- 8.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(Suppl 3):S163–75. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- 9.Strickland BB, Singh GK, Kogan MD, Mann MY, van Dyck PC, Newacheck PW. Access to the medical home: new findings from the 2005–2006 National Survey of Children with Special Health Care Needs. Pediatrics. 2009;123(6):e996–1004. doi: 10.1542/peds.2008-2504. [DOI] [PubMed] [Google Scholar]
- 10.Newacheck PW, Hung YY, Wright KK. Racial and ethnic disparities in access to care for children with special health care needs. Ambul Pediatr. 2002;2(4):247–54. doi: 10.1367/1539-4409(2002)002<0247:raedia>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.Yu SM, Singh GK. Household language use and health care access, unmet need, and family impact among CSHCN. Pediatrics. 2009;124(Suppl 4):S414–9. doi: 10.1542/peds.2009-1255M. [DOI] [PubMed] [Google Scholar]
- 12.Inkelas M, Raghavan R, Larson K, Kuo AA, Ortega AN. Unmet mental health need and access to services for children with special health care needs and their families. Ambul Pediatr. 2007;7(6):431–8. doi: 10.1016/j.ambp.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Montes G, Halterman JS. White-black disparities in family-centered care among children with autism in the United States: evidence from the NS-CSHCN 2005–2006. Acad Pediatr. 2011;11(4):297–304. doi: 10.1016/j.acap.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Houtrow AJ, Okumura MJ, Hilton JF, Rehm RS. Profiling health and health-related services for children with special health care needs with and without disabilities. Acad Pediatr. 2011;11(6):508–16. doi: 10.1016/j.acap.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lykens KA, Fulda KG, Bae S, Singh KP. Differences in risk factors for children with special health care needs (CSHCN) receiving needed specialty care by socioeconomic status. BMC Pediatr. 2009;9:48. doi: 10.1186/1471-2431-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngui EM, Flores G. Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family-centered care. Pediatrics. 2006;117(4):1184–96. doi: 10.1542/peds.2005-1088. [DOI] [PubMed] [Google Scholar]
- 17.Derigne L, Porterfield S, Metz S. The influence of health insurance on parent's reports of children's unmet mental health needs. Matern Child Health J. 2009;13(2):176–86. doi: 10.1007/s10995-008-0346-0. [DOI] [PubMed] [Google Scholar]
- 18.Silver EJ, Stein RE. Access to care, unmet health needs, and poverty status among children with and without chronic conditions. Ambul Pediatr. 2001;1(6):314–20. doi: 10.1367/1539-4409(2001)001<0314:atcuhn>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 19.Braveman PA, Kumanyika S, Fielding J, LaVeist T, Borrell LN, Manderscheid R, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(Suppl 1):S149–55. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 21.Carle AC, Blumberg SJ, Poblenz C. Internal psychometric properties of the Children with Special Health Care Needs Screener. Acad Pediatr. 2011;11(2):128–35. doi: 10.1016/j.acap.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Muthén LK, Muthén BO. Mplus statistical analysis with latent variables: user's guide. 7th. Los Angeles (CA): Muthén and Muthén; 2012. Nov, Internet. [cited 2014 Oct 14]. Available from: http://www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r6_web.pdf. [Google Scholar]
- 23.Yu H, Dick AW. Risk-adjusted capitation rates for children: how useful are the survey-based measures? Health Serv Res. 2010;45(6 Pt 2):1948–62. doi: 10.1111/j.1475-6773.2010.01165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuo DZ, Robbins JM, Lyle RE, Barrett KW, Burns KH, Casey PH. Parent-reported outcomes of comprehensive care for children with medical complexity. Farn Syst Health. 2013;31(2):132–41. doi: 10.1037/a0032341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Honberg LE, Kogan MD, Allen D, Strickland BB, Newacheck PW. Progress in ensuring adequate health insurance for children with special health care needs. Pediatrics. 2009;124(5):1273–80. doi: 10.1542/peds.2009-0372. [DOI] [PubMed] [Google Scholar]
- 26.Yeh M, McCabe K, Hough RL, Dupuis D, Hazen A. Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Ment Health Serv Res. 2003;5(2):65–77. doi: 10.1023/a:1023286210205. [DOI] [PubMed] [Google Scholar]
- 27.Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: has anything changed over the years? Int J Equity Health. 2013;12:10. doi: 10.1186/1475-9276-12-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palfrey JS, Sofis LA, Davidson EJ, Liu J, Freeman L, Ganz ML. The Pediatric Alliance for Coordinated Care: evaluation of a medical home model. Pediatrics. 2004;113(5 Suppl):1507–16. [PubMed] [Google Scholar]
- 29.Berry JG, Agrawal R, Kuo DZ, Cohen E, Risko W, Hall M, et al. Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. J Pediatr. 2011;159(2):284–90. doi: 10.1016/j.jpeds.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards ST, Abrams MK, Baron RJ, Berenson RA, Rich EC, Rosenthal GE, et al. Structuring payment to medical homes after the Affordable Care Act. J Gen Intern Med. 2014;29(10):1410–3. doi: 10.1007/s11606-014-2848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medical Home Initiatives for Children with Special Needs Project Advisory Committee. American Academy of Pediatrics. The medical home. Pediatrics. 2002;110(1 Pt 1):184–6. [PubMed] [Google Scholar]
- 32.Shone LP, Dick AW, Klein JD, Zwanziger J, Szilagyi PG. Reduction in racial and ethnic disparities after enrollment in the State Children's Health Insurance Program. Pediatrics. 2005;115(6):e697–705. doi: 10.1542/peds.2004-1726. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics, Council on Pediatric Practice. Council on Pediatric Practice Standards of child health care. Evanston (IL): American Academy of Pediatrics; 1967. Pediatric records and a “medical home.”; pp. 77–9. [Google Scholar]
- 34.Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113(5 Suppl):1473–8. [PubMed] [Google Scholar]
- 35.Rose RA, Parish SL, Yoo J, Grady MD, Powell SE, Hicks-Sangster TK. Suppression of racial disparities for children with special health care needs among families receiving Medicaid. Soc Sci Med. 2010;70(9):1263–70. doi: 10.1016/j.socscimed.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 36.Kogan MD, Newacheck PW, Blumberg SJ, Ghandour RM, Singh GK, Strickland BB, et al. Underinsurance among children in the United States. N Engl J Med. 2010;363(9):841–51. doi: 10.1056/NEJMsa0909994. [DOI] [PubMed] [Google Scholar]
- 37.Wells N, Krauss MW, Anderson B, Gulley S, Leiter V, O'Neil M, et al. Your voice counts!! The Family Partners Project report to families. 2nd. Boston (MA): Family Voices at the Federation for Children with Special Health Care Needs; 2000. Apr, What do families say about health care for children with special heatlh care needs? Internet. [cited 2014 Oct 14]. Available from: http://www.familyvoices.org/admin/miscdocs/files/National-Famrpt-1.pdf. [Google Scholar]


