Abstract
Objective
We examined the impact of parental psychological stress on body mass index (BMI) in pre-adolescent children over four years of follow-up.
Methods
We included 4,078 children aged 5–10 years (90% were between 5.5 and 7.5 years) at study entry (2002–2003) into the Children's Health Study, a prospective cohort study in southern California. A multi-level linear model simultaneously examined the effect of parental stress at study entry on the attained BMI at age 10 and the slope of change across annual measures of BMI during follow-up, controlled for the child's age and sex. Body mass index was calculated based on objective measurements of height and weight by trained technicians following a standardized procedure.
Results
A two standard deviation increase in parental stress at study entry was associated with an increase in predicted BMI attained by age 10 of 0.287 kg/m2 (95% confidence interval 0.016-0.558; a 2% increase at this age for a participant of average attained BMI). The same increase in parental stress was also associated with an increased trajectory of weight gain over follow-up, with the slope of change in BMI increased by 0.054 kg/m2 (95% confidence interval 0.007-0.100; a 7% increase in the slope of change for a participant of average BMI trajectory).
Conclusions
We prospectively demonstrated a small effect of parental stress on BMI at age 10 and weight gain earlier in life than reported previously. Interventions to address the burden of childhood obesity should address the role of parental stress in children.
Keywords: Parental stress, psychological stress, obesity, weight gain, pre-adolescents, children, prospective cohort
Introduction
Rates of childhood and adult obesity have increased dramatically in North America and elsewhere since the mid-1970s [1, 2]. Childhood is a critical period for determinants of energy balance, including biological programming and cognitive-social development that can influence the adoption of relevant health behaviours [3, 4]. Identifying factors that influence how obese phenotypes are determined during early life can facilitate prevention earlier in the life course. While research into behavioural determinants has focused on physical inactivity and unhealthy diets [5], psychological stress experienced by parents can also contribute to risk for obesity during childhood [6].
Although the role of psychological stress in parents in the etiology of childhood overweight remains unclear, plausible pathways leading to positive energy balance in children include: parenting changes that directly lead to positive energy balance in children [7, 8] (e.g., preparation of convenient but unhealthy meals in an effort to help manage their own time [9]); the indication of parental obesity due to lifestyle and/or physiological dysfunction, which influences related attitudes and behaviours of children [10, 11]; and a role for stress experienced by children of stressed parents [12].
There has been little study of the relationship between parental stress and obesity outcomes in children (e.g., [6]), and apparently no prospective assessment of the effects of parental stress on weight gain in children. We examined the relationship between perceived psychological stress in parents and attained body mass index (BMI) at age 10 and BMI trajectory over four years in pre-adolescent schoolchildren in the Children's Health Study, which provides data on a variety of factors that might confound associations between parental stress and obesity in children. Study participants included males and females ages 5-10 at study entry, and the majority of children were either of Hispanic ethnicity or non-Hispanic white race.
Methods
Study population
The Children's Health Study is a prospective cohort study of air pollution and respiratory health [13]. Details on the study design are reported elsewhere [13]. Enrollment was carried out in 45 participating schools located in 13 southern California communities in 2002 and 2003, as previously described [13]. Written informed consent was obtained from parents or guardians at baseline, and the study was approved by the University of Southern California Institutional Review Board.
This secondary analysis includes data from baseline and annual follow-up visits over a four year period. Although all students in kindergarten and first grade were invited to participate, 5349 (65%) returned valid baseline questionnaires [14, 15]. This analysis was restricted to 4550 children followed up for at least one year (i.e., two or more measurements of height and weight). These participants had an average of 3.9 BMI measurements and there was complete follow-up (i.e., no missing measurements of BMI for any participants) before they were censored (i.e., 2.9 years of follow-up on average). Children were excluded from this analysis if they were missing data describing parental stress (n=472). Therefore, the study population for this analysis included 4078 children (76% of all respondents).
Assessment of body mass index, parental stress and covariates
Body mass index was calculated based on objective measurements of height and weight during annual follow-up visits (see online supplement for details). Baseline and follow-up questionnaires were completed by parents (74% mothers), including information about demographic and family characteristics, respiratory health, parental stress at baseline, physical activity, characteristics of homes and other relevant covariates.
Perceived stress was assessed in the responding parent using the 4-item version of the Perceived Stress Scale (PSS), which is a widely used measure of the degree to which respondents believe their lives are unpredictable, uncontrollable, or overwhelming [16]. A single measure of this scale has been validated as a measure of manifestations including negative affective states and physical symptoms of stress [17, 18]. Scores ranged from 0 to 16, and a representative U.S. sample found an overall mean and standard deviation of 4.49 and 2.96, respectively [16].
Other covariates from the baseline questionnaire and describing the built environment were identified as potential confounders of any of the pathways identified between parental stress and BMI trajectory of children based on prior evidence of a plausible relationship and a statistically significant unadjusted association with the slope of change in BMI in our cohort (α=0.05; see online supplement for rationale). Questionnaire measures included age, sex, race or Hispanic ethnicity, use of a Spanish language questionnaire, medical insurance coverage, parental educational attainment (an indicator of socioeconomic position), exercise classes, lessons or special programs outside of school in which the child participated during the last 12 months [19], and presence of a daily smoker of cigarettes, cigars or pipes in the home (which may reflect exposure in utero [20]. Measures of the residential built environment at baseline included: two walkability measures, including connectivity of the street network and household exposure to non-freeway sources of NOX from traffic on local roads; proximity to food outlets; green cover based on the normalized difference vegetation index (NDVI); and population density (population per square mile) (see [14, 21] for more detail on how these variables were compiled).
Statistical methods
Our mixed-effects modeling approach properly adjusts for age- and sex- specific effects on BMI growth in children, and provides a proper mechanism for assessing effects of risk factors on BMI growth. Letting c, i and j denote the study community, child and year of measurement, respectively, the following two-level linear model was used to examine the effect of parental stress at study baseline, Sci, both on BMI, Ycij:
| (1) |
| (2) |
| (3) |
where tcij denotes age of participants at time of BMI measurements (centered at 10 years of age), Ac denotes town specific intercepts, and Z1,...,Zq denote adjustment factors such as sex, and race/ethnicity categories. Our results were obtained by combining equations (1-3) to fit the following unified mixed effects model:
| (4) |
In Eqn (4), β1 and β2 correspend to the simultaneously estimated effects of parental stress on BMI level attained at age 10 (i.e., examining the main effect between individuals) and also the yearly slope of change in BMI during the follow-up period [22], respectively.
In our models, we required subjects to have at least two measurements of BMI to enable the conceptual subject-specific linear growth framework. Body mass index trajectory between measurements within the same individuals, and the effect of stress on BMI trajectory, were assumed to be linear over the four-year average age change from 6 - 10 years.
The basic model included a set of design variables as fixed effects on BMI trajectory; namely, age, BMI and community of residence at baseline, sex, and racial/ethnic group. Additional confounders (as described above) were then considered in the final model using a manual forward stepwise approach. Potential confounders were entered into the model only if controlling for them individually changed the BMI trajectory coefficient of parental stress by at least 10%. This subset of potential confounders was then entered into a final model in order of greatest negative impact on the effect of parental stress on BMI trajectory. Indicators of missing data for confounders were also included in models adjusted for these covariates to allow all 4078 subjects into these models [23].
Interaction terms were added to the final model to test whether effects on attained BMI at age 10 or BMI trajectory were different by sex, Hispanic ethnicity, and all other confounders entered into the final model (α=0.05), except for after-school exercise activity because the interaction model did not converge in that case. All analyses were conducted by using the SAS and R statistical software packages.
Results
The full age range at study entry was 5-10 years; however, 90% of participants were aged between 5.5 and 7.5 years with a mean of 6.7 years. The mean PSS among parents (i.e. parental stress) was 4.0 with a standard deviation of 2.9. Approximately half of participants were male (50.5%) and the majority were of Hispanic ethnicity (54.1%). Around one-third of participants were Non-Hispanic whites (32.2%), and the remainder was Asian (3.2%), African American (2.7%) or another race/ethnicity (7.9%). One-quarter of parents used a Spanish-language questionnaire (24.9%). Only 12% of participants were not medically insured, while 21.8% lived with a parent without a high school diploma. Other characteristics of participants’ families and their neighborhood built environment are shown in Table 1.
Table 1.
Participant characteristics at baseline
| Variables | N (%)* | Mean (SD): range |
|---|---|---|
| Dependent Variable | ||
| Parental stress (Perceived Stress Scale) | 4.0 (2.9): 0-16 | |
| Design Variables | ||
| Age (years) | 6.7 (0.7): 4.5-10.4 | |
| Male sex | 2297 (50.5) | |
| Race/Ethnicity | ||
| Hispanic ethnicity | 2462 (54.1) | |
| African-American race | 122 (2.7) | |
| Asian race | 145 (3.2) | |
| White Non-Hispanic race | 1464 (32.2) | |
| Other race | 357 (7.9) | |
| Body mass index at baseline (kg/m2) | 16.7 (2.7): 11.5-34.9 | |
| Gender- and age-specific body mass index percentile** | ||
| Normal (BMI <85th pct) | 3201 (70.4) | |
| Overweight (≥85th pct BMI <95th pct) | 660 (14.5) | |
| Obese (≥95th pct BMI) | 684 (15.1) | |
| Other Covariates | ||
| Number of after-school exercise activities in last 12 months? | ||
| 0 | 2913 (70.9) | |
| 1 | 1000 (24.3) | |
| 2+ | 198 (4.8) | |
| Parental education | ||
| Did not finish high school | 905 (21.8) | |
| High school diploma or some college | 2364 (56.8) | |
| College diploma or greater | 892 (21.4) | |
| Medical insurance coverage | 3689 (88.3) | |
| Spanish language questionnaire | 1133 (24.9) | |
| Any daily smoker inside home | 309 (7.2) | |
| Any pets in home | 3232 (76.1) | |
| Residential traffic-related pollution (ppm) | 6.7 (6.1): 0-69 | |
| Residence in a food desert neighborhood | 2137 (51.9) | |
| Neighborhood green space (NDVI) | 0.09 (0.10): 0-0.50 | |
| Neighborhood connectivity index | 0.40 (0.06): 0-0.66 | |
| Neighborhood population density (per km2) | 1703.9 (1426.7): 3.8-13978.3 | |
Numbers do not always add up to 4550 due to missing values.
Body mass index percentile based on Centers for Disease Control and Prevention reference values for the year 2000.
After controlling for age and sex of participants, perceived stress in parents at baseline was positively associated with attained BMI at age 10 as well as BMI trajectory over a 4-year period (Table 2). In a model adjusted only for design variables, an increase in parental stress across two standard deviations of PSS was associated with 0.443 kg/m2 higher BMI at baseline (95% confidence interval 0.025-0.860). In this model, the slope of change in BMI over the study period was increased by 0.093 kg/m2 (95% confidence interval 0.078-0.108) across the same contrast (Model 1 in Table 2).
Table 2.
Associations of parental stress at baseline with attained BMI at age 10, slope of BMI change over a four-year period
| Effect | Model 1 | Model 2 |
|---|---|---|
| Attained BMI coefficient (95% CI) | 0.443 (0.025-0.860) | 0.287 (0.016-0.558) |
| Slope of BMI change coefficient (95% CI) | 0.093 (0.078-0.108) | 0.054 (0.007-0.100) |
Model 1 includes adjustment for age, sex, racial/ethnic group and community of residence at baseline. Model 2 additionally adjusts for exposure to traffic-related pollution at the home, participant's level of extra-curricular exercise activity, residence in a “food desert” and parental education. Effects of stress scaled across 2 SD of PSS (2.9 units).
Although adjusting for possible confounders led to large reductions in the size of effects on attained BMI and BMI trajectory, both effects remained statistically significant (Model 2 in Table 2). After further adjusting for confounders including exposure to traffic-related pollution at the home, extra-curricular exercise activity, proximity to food outlets and parental education, we observed a 0.287 kg/m2 increase in attained BMI at age 10 across the interquartile range of parental stress (95% confidence interval 0.016-0.558). Across the same contrast, the slope of change in BMI was increased by 0.054 kg/m2 (95% confidence interval 0.007-0.100). These coefficients translate into roughly 2% and 7% increases in the attained BMI and BMI trajectory (respectively) for every two standard deviation increase in parental stress for participants of average attained BMI (16.7 kg/m2) and average increase in attained BMI during follow-up (0.77 kg/m2).
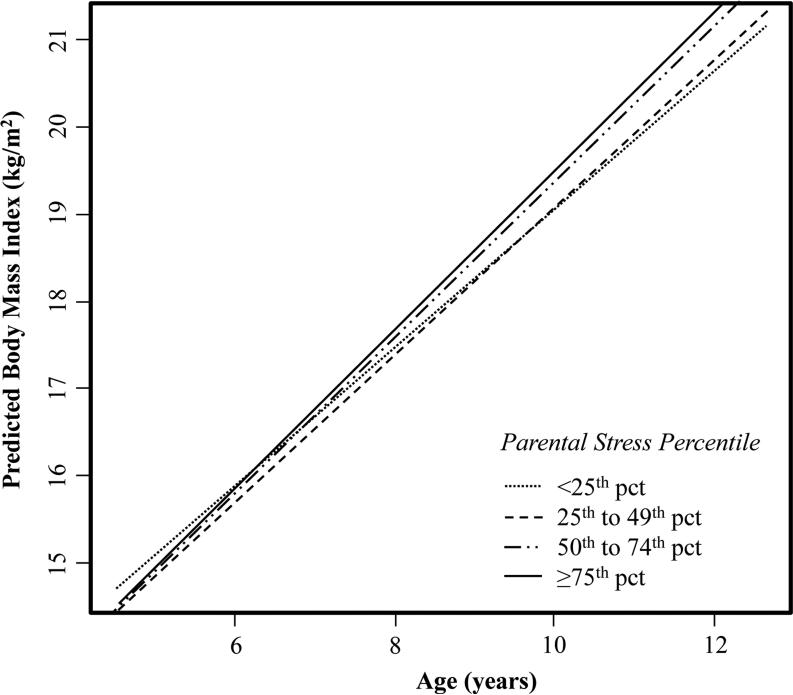
Figure 1 displays BMI trajectory across the age range available in the cohort (5 to 13 years) predicted by data from annual follow-up visits, applied, which has been stratified by parental stress quartile, based on the final model (Model 2 in Table 2). This figure indicates that there was a graded increase in the slope of change across increasing levels of parental stress, as well as a particularly large increase above (versus below) the 50th percentile. Model results were also highlighted by considering the change in overweight and obesity rates at age 10 (120.5 months) based on gender-specific 85th and 95th percentiles of BMI from the Centers for Disease Control growth charts if all children in the sample were to have commensurate parental stress at the lower end of the 2 standard deviation range. Under this scenario, 2.7% of boys would move from overweight to normal, and approximately 1.2% would move from obese to overweight; for girls, the comparable shifts are 1.2% and 1.4%.
Figure 1.
Predicted adjusted body mass index across increasing quartiles of parental stress Figure 1 Footnote Parental Stress Scale: 25th pct = 2, 50th pct = 4, 75th pct = 6. BMI trajectory is predicted by data from annual follow-up visits, applied to the age range available in the cohort from 5 to 13 years by parental stress quartile, based on the final model (Model 2 in Table 2).
Effects of stress on attained BMI and the slope of change were stronger among children of Hispanic ethnicity (p-value for interaction < 0.05). Coefficients for both of these BMI outcomes were approximately 2.5 times larger in Hispanics than effects noted for the total population in Table 2; whereas these coefficients were diminished and not statistically significant among non-Hispanic children. Effects of parental stress did not differ for boys and girls in our cohort, nor by other covariates included in the final model that were tested.
Discussion
This is the first prospective study to demonstrate an association of parental stress with increased weight gain in pre-adolescents. This relationship was not fully explained by socioeconomic, lifestyle and environmental factors available for this analysis. Our results support studies indicating a cross-sectional positive relationship between parental stress with overweight and obesity in children (e.g., [6]).
Rates of obesity, and other components of the metabolic syndrome have increased over the last 20 years, and it is possible that increasing stress in parents over this period contributed to weight gain in children [24]. There are several plausible pathways; although we did not have data available to test their salience.
Parental stress may be associated with parenting behaviours causing positive energy balance in children, e.g., provision of an insecure food environment with under-nutritious food [7-9]. Parental stress may also reflect obesity in parents, which could explain obesity in children due to shared genetic vulnerability [11], and the potential for lifestyle factors related to energy balance (i.e., diet and exercise) to be inefluenced by the conditions (e.g., nutrition environment; [10]) and social models [25] that parents offer children. Since parental stress was associated with other likely household-level stressors (e.g., low income, residence in an apartment versus house) in our cohort [26], it may act as a marker for psychosocial stress in children [12, 27-30], which has been associated with weight gain [31, 32] and metabolic syndrome [33, 34] in adolescents.
Although the strength of the relationship of parental stress with both BMI outcomes was substantially reduced by controlling for confounders, several of these confounders reflect variables that may lie on the causal pathway, including level of exercise activity, as well as parental education, which could reflect a scarcity of resources to cope with stress effectively or residence in an environment with a scarcity of healthy, affordable food or that is activity unfriendly. Thus, the true stress effects may be larger than indicated by coefficients in the fully adjusted model in Table 2.
There was a wide age range among participants at baseline (5-10 years), although 90% of participants were between the ages of 5.5 and 7.5. A sensitivity analysis restricted to the narrower age group showed a similar pattern of effects of stress, so it is unlikely that the overall effect of stress on BMI is masking distinct effects of parental stress on participants of particularly old or young age at baseline. Pubertal stage, which can influence appetite control and weight gain through changes in levels of the hormone leptin, was not measured in this study [35]. Therefore, if changes in pubertal stage lead to changes in parental stress, then the association between parental stress and weight gain in children may be spurious. We only assessed parental stress at study baseline, and parents’ experience of stress may have changed during follow-up. This would likely lead to non-differential misclassification and some attenuation of the size of the effect on BMI outcomes.
Beyond the pre-adolescent age range of our participants, the generalizability of these results is potentially limited based on the sociodemographic profile of the participants; namely, the unique racial and ethnic composition of our study population (mainly Hispanic and White, non-Hispanic schoolchildren) given that genetic and social factors help determine diet, weight gain and obesity. Given the importance of cultural, economic, political and other factors in determining parental and child stress and obesity, these results may be specific to U.S. children.
The effects of stress on BMI were greater among Hispanic children in our cohort. The average BMI at baseline of Hispanic children was 0.5 kg/m2 greater than children of other racial or ethnic backgrounds (data not shown), which is consistent with other studies that have observed a higher prevalence of overweight and obesity among Hispanic American children compared to other American children (e.g., [2]), and others that indicate that Hispanic children may be particularly vulnerable to parent stress for obesity [9]. Some evidence indicates that obesity in Hispanic children may reflect genetic phenotypes characterized by behavioural (i.e., hyperphagia and sedentary lifestyle) and biological (i.e., promotion of adiposity) predispositions for positive energy balance [36, 37]. We cannot rule out the possibility that effects of stress reflect confounding by such genetic factors, or gene-stress interactions. Hispanic participants may also be more likely to experience stress related to immigration or acculturation. Hispanic children who used a Spanish language questionnaire in our survey also had higher stress [26], and acculturation stress has been associated with higher waist circumference in Mexican-American adults [38]. However, the coefficient of stress on BMI among Hispanics in this analysis was not altered by limiting the sample to participants who used a Spanish language questionnaire (data not shown), so stress related to a history of immigration or low acculturation does not explain the larger effect in Hispanic children. Future research should consider other reasons that Hispanic children are more susceptible to parental stress, including differences in how Hispanic parents respond to stress or how Hispanic children perceive stressors or cope with stress. Policies and other interventions (as described below) should be targeted in design to Hispanic communities.
Some participants were excluded from the analysis due to missing data on parental stress. These individuals were more likely to be of “other” race/ethnicity (i.e., not Hispanic, African-American, Asian or White Non-Hispanic; 28% versus 5%), more likely to be of Hispanic ethnicity (55% versus 50%), and slightly older (1.5 months); P<0.05. Since the effect of parental stress on attained BMI and BMI trajectory was stronger for Hispanic participants, if these participants were more likely to have high parental stress, then effects reported in Table 2 may be biased towards the null; although there were only very weak positive associations between Hispanic ethnicity or use of a Spanish language questionnaire and parental stress, so this bias is unlikely to be very strong. Also, although we did not observe any effect of parental stress among children of “other” race/ethnicity (data not shown) and thus, do not expect any bias associated with their exclusion, our study may have been under-powered to detect effects in this small subgroup to the small sample size. Finally, the age difference was very minor between participants with and without stress information; therefore, bias in observed effects of stress due to these differences in excluded participants was unlikely.
This study links increased attained BMI at age 10 and increased BMI trajectory with parental stress in a population of pre-adolescents. Although the precise role of parental stress in children's energy balance remains unclear, the consistency of the relationship between chronic stress and BMI across a range of age groups suggests that interventions to reduce chronic household stress and stressful environmental conditions, and to increase resources for families to coping with stress, might help reduce obesity in children and its metabolic consequences [39]. Family-level psychological, social and educational support for those experiencing chronic stress might help promote healthy diet and exercise behaviors in children (e.g., [40]). Improved food security (e.g., [41]) and policies that provide a strong social safety net could lead to healthier eating habits and less obesity in families experiencing stressful conditions such as poverty or joblessness [42, 43].
Supplementary Material
Acknowledgements
This work was supported by National Institute of Environmental Health Sciences [grant numbers 5R03ES014046, 1R01ES016535, 5P01ES009581, 5P01ES011627, 5P30ES007048]; U.S. Environmental Protection Agency [grant numbers R831845, RD831861, R826708]; the Eunice Kennedy Shriver National Institute of Child Health and Human Development [R01 HD061968]; National Cancer Institute [grant number 1U54CA116848- 01]; and the Hastings Foundation. We thank Ernest Shen for his assistance in completing this work.
Footnotes
None of the authors have conflicts of interest to declare.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307(5):483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauer AM, Boyce WT. Prophecies of childhood: how children's social environments and biological propensities affect the health of populations. Int J Behav Med. 2004;11(3):164–75. doi: 10.1207/s15327558ijbm1103_5. [DOI] [PubMed] [Google Scholar]
- 4.Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–73. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- 5.Singh AS, Vik FN, Chinapaw MJ, et al. Test-retest reliability and construct validity of the ENERGY-child questionnaire on energy balance-related behaviours and their potential determinants: the ENERGY-project. Int J Behav Nutr Phys Act. 2011;8:136. doi: 10.1186/1479-5868-8-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koch FS, Sepa A, Ludvigsson J. Psychological stress and obesity. J Pediatr. 2008;153(6):839–44. doi: 10.1016/j.jpeds.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Francis DD, Meaney MJ. Maternal care and the development of stress responses. Curr Opin Neurobiol. 1999;9(1):128–34. doi: 10.1016/s0959-4388(99)80016-6. [DOI] [PubMed] [Google Scholar]
- 8.Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes. 2011;6(2-2):e12–27. doi: 10.3109/17477166.2011.566339. [DOI] [PubMed] [Google Scholar]
- 9.Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012;130(5):e1096–104. doi: 10.1542/peds.2012-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am J Health Promot. 2005;19(5):330–3. ii. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- 11.Tsiotra PC, Koukourava A, Kaltezioti V, et al. Compound heterozygosity of a frameshift mutation in the coding region and a single base substitution in the promoter of the ACTH receptor gene in a family with isolated glucocorticoid deficiency. J Pediatr Endocrinol Metab. 2006;19(9):1157–66. doi: 10.1515/jpem.2006.19.9.1157. [DOI] [PubMed] [Google Scholar]
- 12.Alpern L, Lyons-Ruth K. Preschool children at social risk: Chronicity and timing of maternal depressive symptoms and child behavior problems at school and at home. Dev Psychopathol. 1993;5:371–387. [Google Scholar]
- 13.McConnell R, Berhane K, Yao L, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–72. doi: 10.1289/ehp.8594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jerrett M, McConnell R, Chang CC, et al. Automobile traffic around the home and attained body mass index: a longitudinal cohort study of children aged 10-18 years. Prev Med. 2010;50(Suppl 1):S50–8. doi: 10.1016/j.ypmed.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shankardass K, McConnell R, Jerrett M, Milam J, Richardson J, Berhane K. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. Proc Natl Acad Sci U S A. 2009;106(30):12406–11. doi: 10.1073/pnas.0812910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage; Newbury Park, CA.: 1988. pp. 31–67. [Google Scholar]
- 17.Hewitt PL, Flett GL, Mosher SW. The Perceived Stress Scale: Factor Structure and Relation to Depression Symptoms in a Psychiatric Sample. Journal of Psychopathology and Behavioral Assessment. 1992;14(3):247–57. [Google Scholar]
- 18.Pbert L, Doerfler LA, DeCosimo D. An Evaluation of the Perceived Stress Scale in Two Clinical Populations. Journal of Psychopathology and Behavioral Assessment. 1992;14(4):363–75. [Google Scholar]
- 19.Dunton G, McConnell R, Jerrett M, et al. Organized physical activity in young school children and subsequent 4-year change in body mass index. Arch Pediatr Adolesc Med. 2012;166(8):713–8. doi: 10.1001/archpediatrics.2012.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al Mamun A, Lawlor DA, Alati R, O'Callaghan MJ, Williams GM, Najman JM. Does maternal smoking during pregnancy have a direct effect on future offspring obesity? Evidence from a prospective birth cohort study. Am J Epidemiol. 2006;164(4):317–25. doi: 10.1093/aje/kwj209. [DOI] [PubMed] [Google Scholar]
- 21.Maziak W, Ward KD, Stockton MB. Childhood obesity: are we missing the big picture? Obes Rev. 2008;9(1):35–42. doi: 10.1111/j.1467-789X.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 22.Berhane K, Gauderman WJ, Stram DO, Thomas DC. Statistical Issues in Studies of the Long-Term Effects of Air Pollution: The Southern California Children's Health Study. Statist Sci. 2004;19(3):414–449. [Google Scholar]
- 23.White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med. 2005;24(7):993–1007. doi: 10.1002/sim.1981. [DOI] [PubMed] [Google Scholar]
- 24.Moriarty DG, Zack MM, Holt JB, Chapman DP, Safran MA. Geographic patterns of frequent mental distress: U.S. adults, 1993-2001 and 2003-2006. Am J Prev Med. 2009;36(6):497–505. doi: 10.1016/j.amepre.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 25.Cullen KW, Baranowski T, Rittenberry L, Olvera N. Social-environmental influences on children's diets: results from focus groups with African-, Euro- and Mexican-American children and their parents. Health Educ Res. 2000;15(5):581–90. doi: 10.1093/her/15.5.581. [DOI] [PubMed] [Google Scholar]
- 26.Islam T, Urman R, Gauderman WJ, et al. Parental stress increases the detrimental effect of traffic exposure on children's lung function. Am J Respir Crit Care Med. 2011;184(7):822–7. doi: 10.1164/rccm.201104-0720OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conger RD, Conger KJ, Elder GH, Jr., Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Dev. 1992;63(3):526–41. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- 28.Hodges WF, London J, Colwell JB. Stress in parents and late elementary age children in divorced and intact families and child adjustment. J Divorce Remarriage. 1990;14:63–80. [Google Scholar]
- 29.Compas BE, Howell DC, Phares V, Williams RA, Giunta CT. Risk factors for emotional/behavioral problems in young adolescents: a prospective analysis of adolescent and parental stress and symptoms. J Consult Clin Psychol. 1989;57(6):732–40. doi: 10.1037//0022-006x.57.6.732. [DOI] [PubMed] [Google Scholar]
- 30.Puder JJ, Munsch S. Psychological correlates of childhood obesity. Int J Obes (Lond) 2010;34(Suppl 2):S37–43. doi: 10.1038/ijo.2010.238. [DOI] [PubMed] [Google Scholar]
- 31.Tomiyama AJ, Puterman E, Epel ES, Rehkopf DH, Laraia BA. Chronic Psychological Stress and Racial Disparities in Body Mass Index Change Between Black and White Girls Aged 10-19. Ann Behav Med. 2012 doi: 10.1007/s12160-012-9398-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Jaarsveld CH, Fidler JA, Steptoe A, Boniface D, Wardle J. Perceived stress and weight gain in adolescence: a longitudinal analysis. Obesity (Silver Spring) 2009;17(12):2155–61. doi: 10.1038/oby.2009.183. [DOI] [PubMed] [Google Scholar]
- 33.Tsiotra PC, Tsigos C. Stress, the endoplasmic reticulum, and insulin resistance. Ann N Y Acad Sci. 2006;1083:63–76. doi: 10.1196/annals.1367.007. [DOI] [PubMed] [Google Scholar]
- 34.Yudkin JS. Confounders in chronic stress at work and metabolic syndrome. BMJ. 2006;332(7550):1153–4. doi: 10.1136/bmj.332.7550.1153-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blum WF, Englaro P, Hanitsch S, et al. Plasma leptin levels in healthy children and adolescents: dependence on body mass index, body fat mass, gender, pubertal stage, and testosterone. J Clin Endocrinol Metab. 1997;82(9):2904–10. doi: 10.1210/jcem.82.9.4251. [DOI] [PubMed] [Google Scholar]
- 36.Cai G, Cole SA, Butte N, et al. A quantitative trait locus on chromosome 18q for physical activity and dietary intake in Hispanic children. Obesity (Silver Spring) 2006;14(9):1596–604. doi: 10.1038/oby.2006.184. [DOI] [PubMed] [Google Scholar]
- 37.Elshorbagy AK, Valdivia-Garcia M, Refsum H, Butte N. The association of cysteine with obesity, inflammatory cytokines and insulin resistance in Hispanic children and adolescents. PLoS One. 2012;7(9):e44166. doi: 10.1371/journal.pone.0044166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29(3):470–7. [PubMed] [Google Scholar]
- 39.Thoits PA. Stress and health: major findings and policy implications. J Health Soc Behav. 2010;51(Suppl):S41–53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- 40.Riggs NR, Sakuma KK, Pentz MA. Preventing risk for obesity by promoting self-regulation and decision-making skills: pilot results from the PATHWAYS to health program (PATHWAYS). Eval Rev. 2007;31:287–310. doi: 10.1177/0193841X06297243. [DOI] [PubMed] [Google Scholar]
- 41.Department of Health and Mental Hygiene . New York City Healthy Bodegas Initiative 2010 Report. Department of Health and Mental Hygiene; New York: 2010. [Google Scholar]
- 42.Garasky S, Stewart SD, Gundersen C, Lohman BJ, Eisenmann JC. Family stressors and child obesity. Soc Sci Res. 2009;38(4):755–66. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent overweight and obesity: links to food insecurity and individual, maternal, and family stressors. J Adolesc Health. 2009;45(3):230–7. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.