Abstract
Lumbar hernias are uncommon and about 300 cases have been reported till date. They commonly occur due to trauma, surgery and infection. They are increasingly being reported after motor vehicle collision injuries. However, spontaneous lumbar hernias are rare and are reported infrequently. It is treated with different surgical approaches and methods. We report a case of primary spontaneous lumbar hernia which was repaired by transperitonial laparoscopic approach using Vypro (polypropylene/polyglactin) mesh and covered with a peritoneal flap.
1. Introduction
Lumbar hernias are rare among all other hernias. Hafner et al.1 stated that general surgeons will get only one opportunity to repair a lumbar hernia during their life time due. However, due to the increased incidence of traumatic etiology and the advances in diagnostic methods available, lumbar hernias are encountered more frequently in current practice.
Lumbar hernia was first suggested by P. Barbette in 1672 and R.J.C. Garangeot published a case for the first time in 1731. Since then, only about 300 cases have been reported.2
The lumbar region is bordered superiorly by the 12th rib, inferiorly by the iliac crest, medially by the erector spinae muscles and laterally by the external oblique muscle. Lumbar hernias occur through two potential weak spaces, which are superior and inferior lumbar spaces. Inferior lumbar space was described by which is bordered by the iliac crest inferiorly, external oblique muscle laterally, latismus dorsi muscle medially. Superior lumbar space which is the larger one was identified. It is an inverted triangle and the base is formed by 12th rib and the lower edge of the serrratus posterior inferior muscle, anterior boundary is formed by the internal oblique muscle and the roof is formed by external oblique and latissimus dorsi.2 Initially, it was believed that inferior lumbar hernias are more common but later studies have shown that superior triangle hernias are much more common.
There are different classifications of the lumbar hernias apart from the site of their occurrence. They can be congenital or acquired. Acquired hernias can be primary/spontaneous and secondary. Secondary lumbar hernias can occur due to trauma, infections or following surgical interventions. Primary spontaneous hernias are the rarest among all the presentations.
2. Case report
A 33-year-old male presented with progressively enlarging swelling in the right loin. There was no history of trauma, fever, weight loss and any associated bowel or urinary complaint. There was no significant past medical or surgical history.
On examination there was a 5 cm× 5 cm partially reducible non tender mass located in the superior lumbar triangle which was prominent during valsalva maneuver. Computer tomography (CT) scan was done which confirmed the diagnosis of superior lumbar hernia, Fig. 1.
Fig. 1.
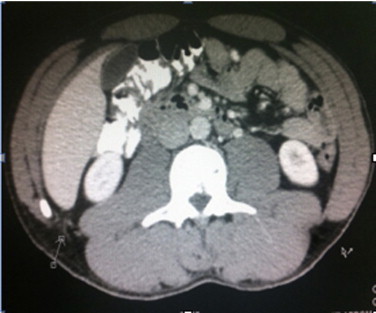
Axial view, CT abdomen showing the lumbar hernia.
The patient required surgical treatment and posted for laparoscopic lumbar hernia repair.
He was placed in left lateral position. Pneumoperitoneum created by open technique and three ports were used. 10 mm umbilical port and two other 5 mm ports were inserted in right hypochondrium and right iliac fossa. The posterior abdominal wall was approached and a peritoneal flap was elevated. The posterior abdominal wall defect was identified and the content was reduced, Fig. 2.
Fig. 2.
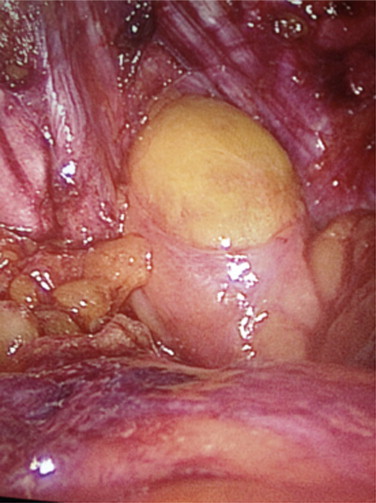
Retroperitoneal opend and the L hernia contents being reduced.
The retroperitoneal fat which was herniating through this defect was reduced and a single 3/0 Vicryl stitch was placed to approximate the defect. The size of defect was measured and 15 cm × 9 cm Vypro mesh was positioned over the defect keeping margins of at least 4 cm all around. The mesh was anchored with tacks to the posterior abdominal wall, Fig. 3, and then covered entirely with the previously elevated peritoneal flap, Fig. 4. The flap was anchored with additional tacks.
Fig. 3.
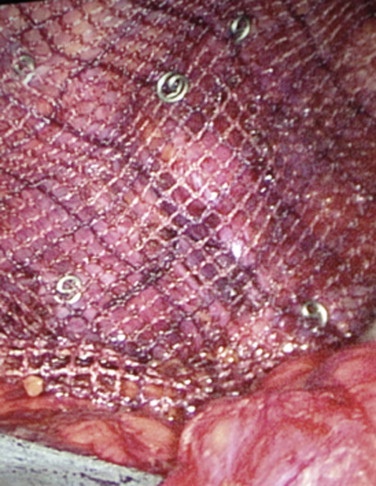
Mesh placed over the defect and anchored with tacks.
Fig. 4.
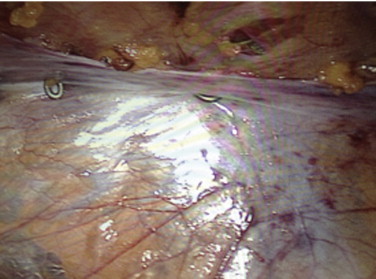
Peritonial flaps were used to cover the entire mesh.
The patient recovered very well without any post operative complications and was discharged home on the third post-op day on analgesics.
3. Discussion
Primary lumbar hernias present most commonly as a palpable mass which increases in size on coughing. They are usually reducible and may disappear in supine position. Patients may present with nonspecific abdominal pain or back pain which may represent sciatica. There are occasions when lumbar hernias may lead to bowel obstruction and sometimes urinary obstruction resulting in hydronephrosis. The most common differential diagnoses are lipomas, fibromas, hematomas, abcesses, intraabdominal/retroperitoneal tumors and panniculitis.
X-rays may not be helpful in diagnosis and CT scan remains the routine method of investigation. In selected patients MRI also has a role in diagnosing and planning the surgical treatment.
91% of the patients present as non emergency cases and only 9% present as surgical emergencies to the hospitals.9 Surgical treatment is the only option and it should be considered early to avoid complications. Earlier, most of the lumbar hernias were repaired primarily using muscle flaps from gluteus major and medius muscle, latissimus dorsi muscle and fascia lata.3 But the recurrence rate was very high due to poor fascial strength and high tension of the repair. Later, artificial mesh with polypropylene, Marlex, or prolene was used to bridge the defect. The Dowd-Ponka technique of repairing lumbar hernias involves making an incision over the hernia site and reducing the contents to the abdomen, followed by covering the defect with prosthetic mesh which is sutured to the external oblique, latissimus dorsi and the lumbar periostium. This is followed by constructing a gluteal fascial flap to cover the defect approximating the external oblique and latissimus dorsi muscles.4 In 1996 the first transabdominal laparoscopic approach was introduced by Burick and Parascandola.5 The balloon dissector was used in 1999 for total extraperitonial approach which was described by Woodward et al.6 A paper published in 2005 shows a prospective study of lumbar hernia repairs – classical versus laparoscopic approaches. It has shown statistically significant lower morbidity rates, shorter length of hospital stay, reduced analgesics requirement and earlier return of normal activity in the laparoscopic group.7 Synthetic mesh for hernia repair has the complications of infection, bowel obstruction and fistula formation. More recently use of biosynthetic mesh made of human acellular dermis has been used with good results especially in contaminated wounds.8 Even though there are multiple operative ways described, there is no recommendation for any one of these approaches.
4. Conclusion
Lumbar hernias are rare. A good history and general physical examination can rule out most of the differential diagnoses. CT scan should be done as a routine prior to planning surgical approach unless the patient presents with life threatening complications. Even though the data available to us regarding the management of lumber hernias are limited, current literature suggests laparoscopic approach is the best method of treatment. Open surgery should be reserved for patients who have very large defects or after failed laparoscopic approach. The operative technique should be planned based on the size of the hernia, location, contents, etiology, chances of recurrence and the availability of facilities and expertise in the hospital.
Written informed consent was obtained from the patient for publication of this case report and case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Conflict of interest
No conflict of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Dr. Yaqoob Alsawafi, operating, writing and reviewing the paper and literature. Dr. Ramesh B.S. operating, writing the article. Dr. Thilan operating, writing the article.
Key learning points
-
•
Lumbar hernias are rare and good history and general physical examination can rule out most of the differential diagnosis.
-
•
CT scan should be done as routine prior to planning surgical approach unless patient is in life threatening emergency situation.
-
•
Even though the data available for us regarding the management of lumber hernias are limited current literature suggests laparoscopic approach is the best method of treatment.
-
•
Open surgery should be reserved for patients who have very large defects or failed laparoscopic approach.
-
•
The operative technique should be decided on the size of the hernia, location, contents, etiology, recurrence and availability of facilities and expertise of the hospital.
References
- 1.Hafner C., Wylie J., Jr., Brush B.E. Petit's lumbar hernia: repair with Marlex mesh. Arch Surg. 1963;86:180–186. doi: 10.1001/archsurg.1963.01310080004002. [DOI] [PubMed] [Google Scholar]
- 2.Moreno-Egea A., Baena E.G., Calle M.C., Martínez J.A., Albasini J.L. Controversies in the current management of lumbar hernias. Arch Surg. 2007;1:82–88. doi: 10.1001/archsurg.142.1.82. [DOI] [PubMed] [Google Scholar]
- 3.Swartz D.W.T. Lumbar hernia. In: Nyhus L.M., Condon R.E., editors. Hernia. 2nd ed. Lippincott; Philadelphia: 1978. pp. 409–426. [Google Scholar]
- 4.Skandalakis L.J., Skandalakis J.E., Skandalakis P.N. 3rd ed. Springer; 2008. Surgical anatomy and technique. [Google Scholar]
- 5.Burick A.J., Parascandola S. Laparoscopic repair of a traumatic lumbar hernia: a case report. J Laparoendosc Surg. 1996;6:259–262. doi: 10.1089/lps.1996.6.259. [DOI] [PubMed] [Google Scholar]
- 6.Woodward A.M., Flint L., Ferrara J. Laparoscopic retroperitoneal repair of recurrent postoperative lumbar hernia. J Laparoendosc Adv Surg Tech A. 1999;9:181–186. doi: 10.1089/lap.1999.9.181. [DOI] [PubMed] [Google Scholar]
- 7.Moreno-Egea A., Torralba J.A., Morales G. Open vs laparoscopic repair of secondary lumbar hernias: a prospective nonrandomized study. Surg Endosc. 2005;19:184–187. doi: 10.1007/s00464-004-9067-7. [DOI] [PubMed] [Google Scholar]
- 8.Beth-Ann S., Victoriya Sara C., Kelly J., Joshua N.H., Tomer D. Repair of a traumatic lumbar hernia with biosynthetic mesh: a novel approach and review of the literature. J Curr Surg. 2012;2(3):105–109. [Google Scholar]
- 9.Alfredo M.-E., Enrique G.B., Miquel C.C., José Antonio T.M., José L.A. Controversies in the current management of lumbar hernias. Arch Surg. 2007;142:82–88. doi: 10.1001/archsurg.142.1.82. [DOI] [PubMed] [Google Scholar]


