Abstract
Objective
To examine whether all-cause hospitalization rates for patients with rheumatoid arthritis (RA) differ from patients without RA.
Patients and Methods
This is a retrospective, population-based cohort study focused on Olmsted County, Minnesota. The RA cohort consisted of patients aged ≥18 years who first fulfilled 1987 ACR criteria for RA in 1980-2007, and was compared to a cohort of similar age, sex, and calendar year without RA. Data on all hospitalizations were retrieved electronically for 1987-2012. Analyses utilized person-year methods and rate ratios (RR) comparing patients with and without RA.
Results
The 799 patients with RA experienced 2968 hospitalizations and the 797 patients without RA experienced 2069 hospitalizations. Patients with RA were hospitalized at a greater rate than patients without RA (RR 1.51, 95% confidence interval [CI] 1.42, 1.59). This increased rate of hospitalization was found in both sexes, all age groups, all calendar years studied and throughout disease duration. Male patients with RA were hospitalized for depression at a greater rate than male subjects without RA (RR 7.16, CI 2.78, 30.67). Patients with RA were hospitalized at a greater rate for diabetes mellitus than subjects without RA (RR 2.45, CI 1.34, 4.89). Among the RA, the indicators of disease severity (e.g., seropositivity, erosions, nodules) in the first year following RA incidence were associated with higher rates of hospitalization.
Conclusion
Patients with RA were hospitalized for all causes at a greater rate than patients without RA. Increased rates of hospitalization were true for several disease categories and patient sub-groups.
Keywords: rheumatoid arthritis, hospitalization, health utilization
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune disorder that is associated with systemic inflammation, but primarily targets synovial joints and the surrounding tissue. While advances in treatment have improved patient outcomes in recent decades [1-4], RA still proves quite debilitating and over one third of patients undergo work disability during their lifetime [5]. Furthermore, numerous extraarticular disease manifestations, such as vasculitis, pericarditis, and rheumatoid lung, complicate treatment and exacerbate patient outcomes, particularly in regard to increased mortality [6-8]. Additional comorbidities, such as infection, depression, gastrointestinal events, and myocardial infarction, also occur with greater frequency in patients with RA [9-11]. While new therapies have improved control of disease manifestations, TNF inhibitors, the most commonly prescribed biologic, are associated with increased risk of opportunistic infection.
Although RA involves such complex and chronic management issues, hospitalization for select RA manifestations [2] and arthritis-related orthopedic surgeries [12] has recently decreased. It is unknown, however, whether all-cause hospitalization rates and utilization for patients with RA differ from the general population.
Research into this subject is nearly nonexistent. A recent study from Sweden concluded that healthcare utilization for patients with RA has decreased relative to the general population in the recent decade; however, the study only examined rheumatological and orthopedic hospitalizations and the usage of outpatient rheumatological and orthopedic clinics, nurses, and physiotherapists [13].
The purpose of this study is to examine whether all-cause hospitalization rates and utilization for patients with RA differ from patients without RA. We examined whether patients with RA are hospitalized at a greater rate than patients without RA, and whether patients with RA experience greater lengths of stay and readmission rates than those without RA.
PATIENTS AND METHODS
This was a retrospective, population-based cohort study including residents of Olmsted County, Minnesota. This study was possible because of the resources of the Rochester Epidemiology Project, a medical records linkage system that contains the complete medical records of all patients in Olmsted County [14, 15]. The previously identified RA cohort consisted of patients who were aged 18 years or older and who first fulfilled the 1987 American College of Rheumatology classification criteria for RA between January 1, 1980 and December 31, 2007 [16]. The earliest date of fulfillment of 4 of the 7 criteria was considered as the RA incidence date. A reference cohort of patients without RA with similar age, sex, and calendar year was randomly selected from the same population, as previously described [7]. Each non-RA subject was assigned an index date corresponding to the RA incidence date of the designated patient with RA.
Data on hospitalizations (admission dates, discharge dates and admission and discharge diagnoses) were retrieved electronically from billing data from Olmsted County medical providers including Mayo Clinic and Olmsted Medical Center and their affiliated hospitals and were available beginning in 1987. Hence, follow-up began with the latter of index date or January 1, 1987, and ended at death, migration from Olmsted County, or December 31, 2012. Of the original 813 patients with RA and 813 subjects without RA, those who died or migrated from Olmsted County prior to 1987 were excluded (10 RA and 10 non-RA) as were those who declined to authorize the use of their medical records for research purposes per Minnesota statute sometime following their initial inclusion in the cohorts (4 RA and 6 non-RA). Discharge diagnoses were grouped together using the Clinical Classifications Software (CCS) for ICD-9-CM from Healthcare Cost and Utilization Project [17]. The CCS groups diagnoses into 18 chapters: infections and parasitic diseases; neoplasms; endocrine, nutritional, and metabolic diseases and immunity disorders (referred to as “endocrine/metabolic” hereafter); diseases of the blood and blood-forming organs; mental illness; diseases of the nervous system and sense organs; diseases of the circulatory system; diseases of respiratory system; diseases of the digestive system; diseases of the genitourinary system; complications of pregnancy, childbirth and puerperium; diseases of the skin and subcutaneous tissue; diseases of the musculoskeletal system and connective tissue; congenital anomalies; certain conditions originating in the perinatal period; injury and poisonings (which includes fractures); symptoms, signs and ill-defined conditions; and residual codes, unclassified. Readmissions were defined as hospital admissions occurring within 30 days of a previous hospital discharge.
For patients with RA, information on RA disease severity was also collected previously via medical record review. These included rheumatoid factor (RF) positivity, anti-citrullinated protein antibody (ACPA) positivity, repeatedly high erythrocyte sedimentation rates (ESR) (i.e., ≥ 3 ESR measures ≥ 50 mm/1hr with a minimum interval of 30 days between 2 measurements), presence of joint erosions/destructive changes and rheumatoid nodules during the first year following diagnosis of RA.
Statistical Methods
Descriptive statistics (means percentages, etc.) were used to summarize the data. Data were analyzed using person-year methods and rate ratios comparing RA to non-RA. Within the RA cohort, patients with and without certain disease severity characteristics were also compared. Comparisons of person-year rates were performed using Poisson methods. Poisson regression models with smoothing splines were used to examine trends over time to allow for non-linear effects. Comparisons of length of stay for RA vs. non-RA were performed using generalized linear models adjusted for age, sex and calendar year with random intercepts to account for multiple hospitalizations in the same patient. Readmission rates were calculated as the number of readmissions divided by the number of subsequent hospitalizations (not counting the first hospitalization for each patient, as it could not be a readmission by definition). Analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA) and R 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
The RA cohort consisted of 799 patients and the non-RA cohort of 797 patients. The mean age in both cohorts was 56 years (68% female) and the mean follow-up was 12 and 13 years, respectively. The patients with RA had 2968 hospitalizations during 9748 person-years [py] of follow-up and the subjects without RA had 2069 hospitalizations during 10232 py. Length of stay was similar among the RA and non-RA hospitalizations (median 3 days, 25th percentile 2 days, 75th percentile 6 days in both cohorts; P=.57).
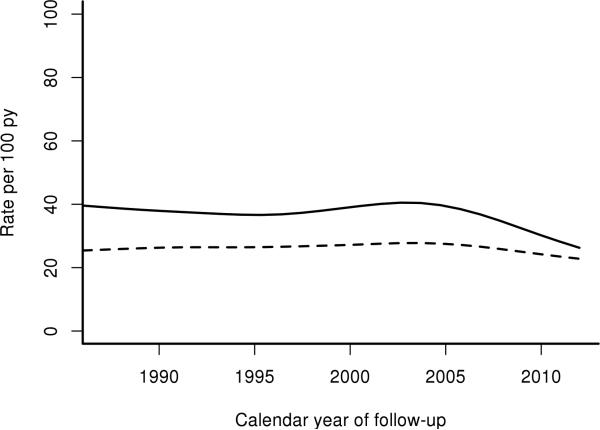
Patients with RA demonstrated hospitalization rates about 1.5 times higher than subjects without RA (Table 1). An increased rate of all-cause hospitalizations for patients with RA also held true for both sexes, all age groups, all calendar years, and throughout disease duration. Patients, both with and without RA, were hospitalized at increasing rates after age 64. However, the RR of hospitalization for patients with RA to patients without RA decreased. As well, the RR of hospitalizations for patients with RA increased after 14 years past diagnosis. The rate of all-cause hospitalizations remained relatively stable across calendar years for patients with and without RA (Figure 1).
Table 1.
a Rate of Hospitalization for Patients with Rheumatoid Arthritis (RA) and Patients without RA
| RA Rateb | Non-RA Rateb | Rate Ratio (95% | ||
|---|---|---|---|---|
| Overall | 30.4 | 20.2 | 1.51 (1.42, 1.59) | |
| Sex | Female | 29.0 | 19.2 | 1.51 (1.41, 1.62) |
| Male | 33.6 | 22.4 | 1.50 (1.36, 1.65) | |
| Ages | 18-44 | 12.4 | 8.6 | 1.44 (1.14, 1.84) |
| 45-64 | 22.4 | 10.8 | 2.07 (1.86, 2.32) | |
| 65-84 | 41.1 | 28.1 | 1.46 (1.36, 1.58) | |
| 85+ | 70.3 | 55.6 | 1.26 (1.09, 1.46) | |
| Calendar Years | 1987-1991 | 30.5 | 19.8 | 1.54 (1.27, 1.88) |
| 1992-1996 | 28.4 | 17.6 | 1.61 (1.37, 1.90) | |
| 1997-2001 | 31.0 | 19.2 | 1.61 (1.41, 1.84) | |
| 2002-2006 | 34.5 | 22.1 | 1.56 (1.41, 1.73) | |
| 2007-2012 | 27.8 | 20.4 | 1.36 (1.23, 1.50) | |
| Years After RA Diagnosis | 0-4 | 26.7 | 17.7 | 1.51 (1.36, 1.68) |
| 5-9 | 28.8 | 20.8 | 1.38 (1.24, 1.53) | |
| 10-14 | 30.3 | 23.0 | 1.32 (1.16, 1.50) | |
| 15-19 | 40.0 | 19.9 | 2.01 (1.71, 2.37) | |
| 20+ | 42.0 | 22.6 | 1.86 (1.55, 2.24) |
Statistically significant results are presented in bold font.
Rate of hospitalizations per 100 person-years.
Figure 1.
Rate of all-cause hospitalization in patients with RA (solid line) and subjects without RA (dashed line) according to calendar year.
Of particular note, only about 20% of patients with RA received biologic therapy in the time period of the study. We did not find any meaningful change in hospitalization rates for patients with RA after the introduction of biologics in 1998 (Table 1). The rate of hospitalizations per 100 py initially increased for patients with RA in the years 2002-2006. However, this increase was also noted in the patients without RA and the resulting RR did not differ from previous years. In the years 2007-2012, we found a decrease in hospitalization rates for patients with and without RA, and the corresponding RR.
In ten of the eighteen CCS chapters, patients with RA were hospitalized at a greater rate than patients without RA (Table 2). These ten disease chapters were: infections/parasitic diseases; endocrine/metabolic diseases; diseases of the blood/blood-forming organs; diseases of the circulatory system; diseases of respiratory system; diseases of the digestive system; diseases of the genitourinary system; diseases of the skin/subcutaneous tissue; diseases of the musculoskeletal/connective tissue; and injury/poisonings. Patients with RA age 45-64 years (493 patients with 945 hospitalizations during 4221 py) were hospitalized at a significantly greater rate for all ten of these chapters when compared to those without RA (488 subjects with 453 hospitalizations during 4198 py; Table 3). Patients with RA age 65-84 (448 patients with 1496 hospitalization during 3639 py) were also hospitalized at a greater rate in comparison to those without RA (455 subjects with 1148 hospitalization during 4087 py) for all ten chapters except genitourinary diseases and endocrine/metabolic diseases. Patients with RA age 85+ years (119 patients with 356 hospitalizations during 507 py) experienced more hospitalizations for infections/parasitic and skin/subcutaneous causes than those without RA (145 subjects with 356 hospitalizations during 640 py). Patients with RA age 18-44 (211 patients with 171 hospitalizations during 1382 py) experiences more hospitalizations for endocrine/metabolic, circulatory, genitourinary and musculoskeletal/connective tissue causes compared to those without RA (206 subject with 112 hospitalizations during 1307 py).
Table 2.
a Rate of Hospitalization for Specific Disease Categories of Patients with Rheumatoid Arthritis (RA) and Patients without RA
| Disease Categoriesb | RA Ratec | Non-RA Ratec | Rate Ratio (95% CI) |
|---|---|---|---|
| Infections, Parasitic | 0.7 | 0.3 | 2.59 (1.68, 4.18) |
| Neoplasms | 1.5 | 1.4 | 1.09 (0.86, 1.37) |
| Endocrine, Metabolic | 1.1 | 0.5 | 2.07 (1.50, 2.91) |
| Blood, Blood-Forming Organs | 0.5 | 0.2 | 2.87 (1.73, 5.08) |
| Mental | 1.1 | 0.9 | 1.17 (0.89, 1.54) |
| Nervous, Sense Organs | 0.8 | 0.6 | 1.35 (0.97, 1.88) |
| Circulatory | 6.3 | 5.0 | 1.26 (1.12, 1.42) |
| Respiratory | 3.3 | 2.0 | 1.64 (1.38, 1.96) |
| Digestive | 3.0 | 2.1 | 1.44 (1.20, 1.72) |
| Genitourinary | 1.8 | 1.4 | 1.34 (1.07, 1.67) |
| Complications of Pregnancy (females only) | 0.6 | 0.5 | 1.13 (0.72, 1.76) |
| Skin, Subcutaneous | 0.8 | 0.2 | 3.32 (2.16, 5.40) |
| Musculoskeletal, Connective Tissue | 4.5 | 1.8 | 2.56 (2.16, 3.05) |
| Injury, Poisoning | 3.0 | 1.9 | 1.59 (1.33, 1.91) |
| Symptoms and Ill-defined conditions | 1.4 | 1.4 | 1.00 (0.79, 1.26) |
Statistically significant results are presented in bold font.
Results for the following CCS categories were not shown due to fewer than 10 total hospitalizations in the RA cases: congenital anomolies; conditions originating in the perinatal period; residual/unclassified codes.
Rate of hospitalizations per 100 person-years
Table 3.
a Rate Ratio (95% Confidence Interval) of Hospitalization for Specific Disease Categories of Patients with Rheumatoid Arthritis compared to Patients without Rheumatoid Arthritis by Select Patient Subgroups
| Disease Categoriesb | Age 18-44 | Age 45-64 | Age 65-84 | Age 85+ | Female | Male |
|---|---|---|---|---|---|---|
| Infections, Parasitic | -- | 7.36 (2.51, 45.54) | 1.80 (1.06, 3.16) | 4.88 (1.74, 21.38) | 3.29 (1.82, 6.65) | 1.95 (1.05, 3.85) |
| Endocrine, Metabolic | 16.08 (2.66, 15895.8) | 3.70 (2.08, 7.41) | 1.36 (0.86, 2.19) | 1.66 (0.72, 4.06) | 1.83 (1.25, 2.75) | 2.68 (1.51, 5.19) |
| Blood, Blood-Forming Organs | -- | 4.25 (1.86, 12.90) | 2.49 (1.28, 5.31) | 1.26 (0.18, 9.03) | 3.71 (2.07, 7.44) | 1.07 (0.34, 3.32) |
| Circulatory | 3.97 (1.22, 25.08) | 1.79 (1.35, 2.38) | 1.29 (1.11, 1.51) | 1.13 (0.87, 1.46) | 1.25 (1.07, 1.47) | 1.28 (1.07, 1.52) |
| Respiratory | 1.09 (0.37, 3.33) | 2.37 (1.51, 3.91) | 1.91 (1.54, 2.40) | 1.12 (0.75, 1.66) | 1.72 (1.36, 2.17) | 1.56 (1.20, 2.05) |
| Digestive | 1.52 (0.74, 3.33) | 2.10 (1.51, 2.99) | 1.35 (1.06, 1.73) | 1.01 (0.61, 1.66) | 1.50 (1.21, 1.86) | 1.31 (0.96, 1.80) |
| Genitourinary | 2.50 (1.20, 6.06) | 1.82 (1.23, 2.74) | 1.08 (0.77, 1.50) | 1.06 (0.58, 1.90) | 1.29 (0.99, 1.68) | 1.45 (0.96, 2.22) |
| Skin, Subcutaneous | 2.84 (0.16, 2451.73) | 5.64 (2.37, 19.55) | 2.93 (1.69, 5.53) | 2.64 (1.01, 8.42) | 4.21 (2.43, 8.15) | 2.18 (1.11, 4.68) |
| Musculoskeletal, Connective Tissue | 8.51 (3.41, 36.17) | 3.82 (2.83, 5.33) | 2.02 (1.60, 2.56) | 1.63 (0.92, 2.96) | 2.66 (2.18, 3.27) | 2.28 (1.66, 3.21) |
| Injury, Poisoning | 0.32 (0.07, 0.94) | 2.22 (1.55, 3.25) | 1.71 (1.34, 2.20) | 1.35 (0.89, 2.06) | 1.65 (1.33, 2.06) | 1.47 (1.07, 2.02) |
Statistically significant results are presented in bold font.
Results shown only for the 10 CCS categories with significantly higher hospitalization rates among RA compare to non-RA as reported in Table 1.
In addition, female patients with RA (546 patients with 1958 hospitalization during 6740 py) were hospitalized at a greater rate in comparison to those without RA (543 subjects with 1351 hospitalization during 7025 py) for all ten chapters except genitourinary diseases, although it did not reach statistical significance. Male patients with RA (253 patients with 1010 hospitalizations during 3008 py) in comparison to those without RA (254 subjects with 718 hospitalizations during 3207 py) were also hospitalized at a greater rate for all ten chapters except diseases of the blood/blood-forming organs, diseases of the digestive system, and genitourinary diseases. However, the increased rates of hospitalizations for digestive and genitourinary disease among males with RA compared to non-RA did not reach statistical significance, as statistical power was limited due to the lower frequency of males with RA.
In examining the specific categories within each of the 10 CCS chapters with higher hospitalizations rates among the RA, we noted two specific categories of particular interest: depression and diabetes mellitus. Hospitalization for depression was at a greater rate for male patients with RA (23 hospitalizations) than for those without RA (3 hospitalizations) (RR 7.16, CI 2.78, 30.67). Second, patients with RA were hospitalized at a greater rate for diabetes mellitus (31 hospitalizations) than subjects without RA (13 hospitalizations) (RR 2.45, CI 1.34, 4.89).
Within the RA cohort, measures of the severity of the disease in the first year after RA incidence were also examined for association with hospitalization rates. Characteristics of severe disease included RF and/or ACPA positivity, joint erosions (213 present versus 586 absent), rheumatoid nodules (137 present versus 662 absent), and repeatedly high ESR (72 present versus 727 absent) (Table 4). Hospitalization rates for diseases of the respiratory system, the musculoskeletal/connective tissue system and the blood/blood-forming organs were significantly increased among 542 patients with RF/ACPA positivity compared to 257 patients who were RF/ACPA negative. However, RF/ACPA positive patients were less likely to be hospitalized for disease of the mental, circulatory, and genitourinary systems or for complications of pregnancy causes than those who were RF/ACPA negative. Patients with joint erosions in the first year after RA incidence had higher rates of hospitalization overall and for endocrine/metabolic, circulatory, skin/subcutaneous and musculoskeletal/connective tissue compared to those without erosions. Rheumatoid nodules in the first year were associated with higher rates of hospitalization for pulmonary causes, and lower rates of hospitalization for neoplasms, endocrine/metabolic and digestive causes compared to those without nodules. Repeatedly high ESR in the first year was associated with elevated hospitalization rates overall and for many of the specific disease chapters.
Table 4.
a Rate Ratio (95% Confidence Interval) of Hospitalization for Specific Disease Categories of Patients with Rheumatoid Arthritis by Select Metrics of Disease Severityb
| Disease Categories | Total number of hospitalizations | RF/ACPA + | Erosions | Nodules | Repeatedly high ESR |
|---|---|---|---|---|---|
| Overall | 2968 | 1.04 (0.97, 1.13) | 1.24 (1.14, 1.34) | 1.01 (0.91, 1.11) | 2.76 (2.51, 3.02) |
| Infectious, Parasitic | 65 | 1.03 (0.62, 1.79) | 0.95 (0.50, 1.64) | 1.19 (0.58, 2.12) | 2.33 (1.10, 4.23) |
| Neoplasms | 149 | 1.13 (0.81, 1.64) | 1.43 (0.99, 2.00) | 0.60 (0.33, 0.98) | 2.52 (1.59, 3.76) |
| Endocrine, Metabolic | 105 | 0.85 (0.57, 1.28) | 2.01 (1.34, 2.95) | 0.37 (0.14, 0.72) | 4.75 (3.03, 7.14) |
| Blood, Blood-Forming Organs | 50 | 2.69 (1.35, 6.67) | 1.48 (0.78, 2.61) | 0.68 (0.23, 1.45) | 0.91 (0.22, 2.20) |
| Mental | 108 | 0.58 (0.40, 0.85) | 0.98 (0.60, 1.50) | 1.15 (0.66, 1.83) | 5.95 (3.92, 8.78) |
| Nervous, Sense Organs | 81 | 1.48 (0.92, 2.57) | 1.13 (0.66, 1.81) | 0.82 (0.39, 1.47) | 5.25 (3.18, 8.27) |
| Circulatory | 610 | 0.80 (0.68, 0.94) | 1.21 (1.01, 1.45) | 1.08 (0.86, 1.33) | 3.15 (2.57, 3.82) |
| Respiratory | 320 | 1.38 (1.08, 1.80) | 0.82 (0.61, 1.07) | 1.58 (1.20, 2.04) | 4.33 (3.35, 5.52) |
| Digestive | 289 | 0.97 (0.76, 1.25) | 0.85 (0.63, 1.12) | 0.66 (0.44, 0.94) | 2.29 (1.64, 3.10) |
| Genitourinary | 177 | 0.67 (0.50, 0.91) | 1.13 (0.79, 1.56) | 0.65 (0.38, 1.01) | 1.78 (1.10, 2.68) |
| Complications of Pregnancy (females only) | 40 | 0.38 (0.20, 0.80) | 0.72 (0.29, 1.48) | 1.37 (0.55, 2.80) | 1.90 (0.64, 4.14) |
| Skin, Subcutaneous | 77 | 1.39 (0.86, 2.41) | 1.74 (1.06, 2.74) | 1.18 (0.61, 2.01) | 1.12 (0.42, 2.24) |
| Musculoskeletal, Connective Tissue | 439 | 1.58 (1.28, 2.00) | 1.96 (1.61, 2.37) | 1.11 (0.85, 1.41) | 1.85 (1.38, 2.41) |
| Injury, Poisoning | 297 | 1.11 (0.87, 1.44) | 1.29 (1.00, 1.66) | 1.17 (0.86, 1.56) | 2.28 (1.64, 3.07) |
| Symptoms Ill-Defined | 141 | 1.20 (0.84, 1.76) | 1.13 (0.75, 1.62) | 1.23 (0.77, 1.84) | 2.83 (1.79, 4.21) |
Statistically significant results are presented in bold font.
Results for the following CCS categories were not shown due to fewer than 10 total hospitalizations in the RA cases: congenital anomalies; conditions originating in the perinatal period; residual/unclassified codes.
Readmission rates were similar among the RA with 616 readmissions (26% of 2398 subsequent hospitalizations) compared to the non-RA with 382 readmissions (25% of 1549 subsequent hospitalizations; P=.47).
DISCUSSION
This first ever study of all-cause hospitalizations for patients with RA demonstrated that patients with RA undergo hospitalization at a higher rate than the general population. This increased rate of hospitalization was found in both sexes, all age groups, all calendar years studied, and throughout disease duration. Patients with RA as a whole also experienced increased rates of hospitalization for almost all of the CCS chapters except neoplasms, mental illness, diseases of the nervous system, complications of pregnancy, and symptoms/signs/ill-defined conditions. Many of the CCS chapters which were found to have high rates of hospitalization, such as infections and diseases of the circulatory system, were expected as these morbidities are associated with RA [7, 9-11].
Diabetes mellitus was a cause of increased hospitalization for patients with RA and depression was a cause for a seven fold increased hospitalization rate for male patients with RA. Why the RR is of this magnitude and for males only is clear, but may relate to the CCS coding methodology and small numbers of patients.
Overall, hospitalization rates were similar for patients who were RF/ACPA positive and those who were seronegative. Patients with RF/ACPA positivity experienced more hospitalizations in the areas of blood/ blood-forming organs, respiratory diseases and musculoskeletal/connective tissue diseases. However, they also experienced lower rates of hospitalization for mental illness, circulatory diseases, genitourinary diseases and pregnancy complications. In general, seropositivity is associated with more severe disease; it is possible that the general structure of CCS categories may have affected these results in ways difficult to interrogate in a study of this type. Repeatedly elevated ESR, a marker of disease activity and severity, in the first year was related to higher hospitalization rates through the disease course overall and for almost all disease chapters. Several categories demonstrated high rate ratios for hospitalization and suggest that early, aggressive treat-to-target strategies in patients with markers of active disease, such as repeatedly elevated ESR in early disease, may greatly reduce the risk of hospitalization for various causes over time.
Interestingly, we did not find marked change in all-cause hospitalization rates after the introduction of biologics in 1998. The RR of hospitalizations in years 2002-2006 did not differ greatly from the RR in the years 1987-1991, 1992-1996, and 1997-2001. We did observe a moderate decrease in RR in the years 2007-2012. It is unknown, however, whether this reduction in RR will be sustained or whether this decrease will indeed be attributable to use of biologic therapy. Only 20% of the patients with RA in this cohort have used biologics, so their effect on hospitalization rates may not be reflected in the overall trends. Length of hospital stay was found to be similar between the patients with RA and the patients without RA. Likewise, readmission rates were nearly identical for patients with and without RA.
There are few studies of hospitalizations for patients with RA. Hospitalizations for select RA manifestations [2] and arthritis-related orthopedic related surgeries [12] have decreased in recent years. A recent study from Sweden concluded that healthcare utilization for patients with RA has decreased relative to the general population in the 21st century. In contrast, we did not find any change in rates of all-cause hospitalization over the range of calendar years included in our study (1987-2012). However, the Swedish study only examined rheumatological and orthopedic hospitalizations and the usage of outpatient rheumatological and orthopedic clinics, nurses, and physiotherapists [13]. No other large scale studies of this topic have been performed. Strengths of our study include that it utilizes a well-characterized, population-based cohort of patients with RA, and it includes a comparison cohort of subjects without RA. Also, the comprehensive resources of the Rochester Epidemiology Project allow complete ascertainment of hospitalizations from all providers in Olmsted County. Usage of CCS is advantageous as it conforms to national data and allows for easy, comparative studies in the future. CCS data is disadvantageous, however, in that it lacks granularity of diagnosis and some categories may overlap. It is possible that some hospitalizations outside Olmsted County may have been missed; however, this is unlikely to be different for patients with and without RA. As well, this information is captured at subsequent visits to Olmsted County providers. An additional limitation of this study may be the population of Olmsted County, Minnesota, which is predominantly white. Thus while our findings should be reflective of the majority of patients with RA seen in Western countries, the generalizability of our findings to more ethnically diverse populations may be limited [18].
CONCLUSION
Patients with RA experience higher rates of hospitalization than the general population. This is true for both sexes, all ages, all calendar years, and throughout disease duration. The higher hospitalization rates associated with repeatedly high ESR in the first year may support aggressive, treat-to-target strategies as a way of potentially reducing the need for hospitalization, but further study would be needed to demonstrate this. Understanding these risks for hospitalization should lead to further studies in order to both identify specific risk factors and to address and prevent hospitalization.
Acknowledgments
Financial support and disclosure:
This work was funded by a grant from the National Institutes of Health, NIAMS (R01 AR46849). Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- ACPA
anti-citrullinated protein antibody
- CCS
Clinical Classifications Software
- CI
95% Confidence Interval
- py
person-years
- RA
Rheumatoid Arthritis
- RR
Rate Ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors do not have any financial conflicts of interest for the work reported herein.
References
- 1.Silman AJ. Trends in the incidence and severity of rheumatoid arthritis. J Rheumatol Suppl. 1992;32(1):71–73. [PubMed] [Google Scholar]
- 2.Ward MM. Decreases in rates of hospitalizations for manifestations of severe rheumatoid arthritis, 1983- 2001. Arthritis Rheum. 2004;50(4):1122–1131. doi: 10.1002/art.20158. [DOI] [PubMed] [Google Scholar]
- 3.Finckh A, Choi HK, Wolfe F. Progression of radiographic joint damage in different eras: Trends towards milder disease in rheumatoid arthritis are attributable to improved treatment. Ann Rheum Dis. 2006;65(9):1192–1197. doi: 10.1136/ard.2005.049338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pincus T, Sokka T, Chung C, Cawkwell G. Declines of tender and swollen joint counts between 1985 and 2001 in patients with rheumatoid arthritis seen in standard care: possible considerations for revision of inclusion criteria for clinical trials. Ann Rheum Dis 2006. 65(7):878–883. doi: 10.1136/ard.2005.044131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allaire S, Wolfe F, Niu J, Lavalley MP. Contemporary prevalence and incidence of work disability associated with rheumatoid arthritis in the US. Arthritis Rheum. 2008;59(4):474–480. doi: 10.1002/art.23538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turesson C, O'Fallon WM, Crowson C, Gabriel SE, Matteson EL. Occurrence of extraarticular disease manifestations is associated with excess mortality in a community-based cohort of patients with rheumatoid arthritis. J Rheumatol. 2002;29(1):62–67. [PubMed] [Google Scholar]
- 7.Gabriel SE, Crowson CS, Kremers HM, et al. Survival in rheumatoid arthritis: a population-based analysis of trends over 40 years. Arthritis Rheum. 2003;48(1):54–58. doi: 10.1002/art.10705. [DOI] [PubMed] [Google Scholar]
- 8.Turesson C, Matterson EL. Management of extra-articular disease manifestations in rheumatoid arthritis. Curr Opin Rheumatol. 2004;16(3):206–211. doi: 10.1097/00002281-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Doran MF, Crowson CS, Pond GR, O'Fallon WM, Gabriel SE. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum. 2002;46(9):2287–2293. doi: 10.1002/art.10524. [DOI] [PubMed] [Google Scholar]
- 10.Myasoedova E, Matteson EL, Talley NJ, Crowson CS. Increased incidence and impact of upper and lower gastrointestinal events in patients with rheumatoid arthritis in Olmsted County, Minnesota: a longitudinal population-based study. J Rheumatol. 2012;39(7):1355–1362. doi: 10.3899/jrheum.111311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21(5):885–906. doi: 10.1016/j.berh.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Shourt CA, Crowson CS, Gabriel SE, Matteson EL. Orthopedic surgery among patients with rheumatoid arthritis 1980-2007: a population-based study focused on surgery rates, sex, and mortality. J Rheumatol. 2012;39(3):481–485. doi: 10.3899/jrheum.111056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagel S, Petersson IF, Bremander A, Lindqvist E, Bergknut C, Englund M. Trends in the first decade of 21st century healthcare utilisation in a rheumatoid arthritis cohort compared with the general population. Ann Rheum Dis. 2013;72(7):1212–1216. doi: 10.1136/annrheumdis-2012-202571. [DOI] [PubMed] [Google Scholar]
- 14.St. Sauver JL, Grossardt BR, Yawn BP, Melton LJ, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocca WA, Yawn BP, St. Sauver JL, Grossardt BR, Melton LJ. History of the Rochester epidemiology project: half a century of medical records linkage in US population. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988. 31(3):315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 17.Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS) 2014. US Agency for Healthcare Research and Quality; [August 14, 2014]. www.hcupus.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 18.St. Stauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LF, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]