Highlights
-
•
Musculoskeletal hydatid cyst is usually associated with involvement of other solid organs.
-
•
Echinococcus can mimic a tumor as mass in the muscle.
-
•
The muscle is considered an unfavorable site for hydatidosis.
-
•
Hydatid cyst should be kept in mind when observing soft tissue mass of the extremities in patients from areas endemic of Echinococcus granulosus.
Keywords: Cyst hydatid, Hydatid disease, Echinococcus granulosus, Vastus lateralis
Summary
Introduction
Musculoskeletal hydatid disease is a rare pathology and its diagnosis is often delayed because of slowly growing mass without inflammation. It is critical to suspicious clinical diagnosis in rural endemic areas and for preoperative diagnosis of this disease.
Presentation of case
We present a 9-year-old boy referred with mass located on the anterolateral part of distal thigh. Diagnosis was verified with MRI histopathologically for the presence of hydatid cyst located in vastus lateralis muscle. Magnetic resonance imaging (MRI) was performed for further imaging. MRI showed an oval cystic mass approximately 77 × 20 × 18 mm in the left vastus lateralis muscle, containing round-shaped daughter cysts. Patients were treated with surgical excision and medical therapy. Clinical, radiological and serologic tests showed no recurrence after treatment.
Discussion
The muscle is considered an unfavorable site for hydatidosis because of its high lactic acid level that creates an unfavorable milieu for growth. The detachment of the germinative membrane from pericyst (water–lily sign) is considered to be pathognomonic and is reported in locations other than the liver and lung in magnetic resonance imaging. Surgery is the most effective way to treat hydatid cysts. Complete surgical resection and medical therapy are the preferred treatment for isolated echinococcosis.
Conclusion
Hydatid cyst in vastus lateralis is a very rare disease. Hydatid cyst should be kept in mind when observing soft tissue mass of the extremities in patients from areas endemic of Echinococcus granulosus.
1. Introduction
Hydatid disease is a zoonosis; humans are infected by consuming food and water that are contaminated with the eggs of the Echinococcus granulosus. The disease is prevalent in most parts of the world, especially in sheep farming and cattle farming areas of Asia, North and East Africa, South America, Australia and the Middle East.1,2 The most common infected sites are the liver, spleen and lungs.3,4 Any tissue can be infected by the disease except hair and nail.4 Musculoskeletal involvement is rare, with an incidence of <2.5% of all cases. Although thoracal spine is the most infected site, muscles are rarely infected and account for approximately <1%.5 These cysts appear as slow-growing masses of soft tissue, sometimes with inflammatory signs and fistulization.6
In this report, we present a very rare case of muscular hydatid disease in a child. It is critical to suspicious clinical diagnosis in rural endemic areas and for preoperative diagnosis of this disease.
2. Case
A 9-year-old boy was referred our hospital with slowly growing mass that localized in his left thigh above the knee. Patient have moderate pain without any daily distraction. His history was not relevant with trauma or septic disease. He did not have pain that localized on the abdomen and chest. The patient lives in a rural area and he is in close contact with animals due to his family's farmery.
Physical examination revealed a 6 × 5 × 4 cm fixed, firm and tender mass in anterolateral and distal parts of the left thigh. There was no ecchymosis, erythema, increased warmth or lymphadenopathy (Fig. 1).
Fig. 1.

The clinical view shows a part of the mass localized on anterolateral part of distal thigh without inflammation.
Laboratory tests were normal and showed a total leukocyte count (WBC) of 5700/mm3, erythrocyte sedimentation rate (ESR) of 25 mm/h (Westergen) and C-reactive protein (CRP) of 0.
Firstly, ultrasound examination was performed and it showed multiple cystic lesion in the muscle localized on vastus lateralis. Magnetic resonance imaging (MRI) was performed for further imaging. MRI showed oval cystic mass approximately 77 × 20 × 18 mm in the left vastus lateralis muscle, containing round-shaped daughter cysts (Fig. 2). The cysts seen hypointense in T1 A weighted images and hyperintense in T2 A weighted images (Fig. 3).
Fig. 2.
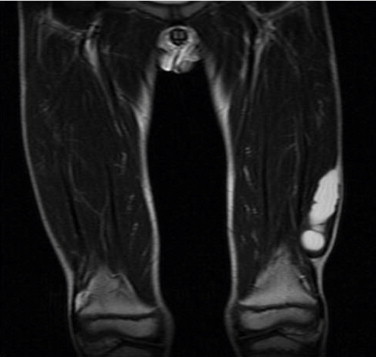
Frontal view of MRI with T2 weighted images showing cystic mass in the left vastus lateralis muscle. The enlargement of the mass is approximately 77 × 20 × 18 mm.
Fig. 3.

Axial view of MRI with T1 weighted images, cysts are seen hypointense with well shaped.
Since the MR images were suggestive of hydatid cyst, further laboratory and imaging studies were employed to support the diagnosis and to detect the other sites of possible involvement. There was no other involvement by hydatid cyst. There was a positive response to indirect hemagglutination test for hydatid disease.
The mass was operated under general anesthesia. Cyst localized in vastus lateralis muscle was removed with muscle for preventing cyst wall intact (Figs. 4 and 5). Cyst area was irrigated with hypertonic 3% saline after removal of mass to reduce risk of recurrence. Incision was closed primarily after inserting suction drain and patient was discharged after removal of drain on day two. Histological examination of the specimen revealed daughter cysts and fragments of lamellar membrane of the hydatid cyst. No bacterial pathogen was cultivated in cyst fluid.
Fig. 4.

The clinical view that was taken intraoperatively shows hydatid cyst wall and its relationship with muscle of vastus lateralis.
Fig. 5.

Cyst's view after removal shows cysts inner wall and internal area.
Albendazole therapy, 200 mg twice daily, was given for six weeks after operation. Clinical, radiological and serologic tests showed no recurrence after treatment.
3. Discussion
Soft tissue hydatid disease is unusual even in endemic areas, and skeletal muscle involvement is extremely rare, with a reported prevalence of 0.5–4.7%.4,5 Musculoskeletal hydatid cyst is usually associated with involvement of other solid organs.5–7 The muscle is considered an unfavorable site for hydatidosis because of its high lactic acid level that creates an unfavorable milieu for growth.6–8 Although there are many reports of intramuscular hydatid cyst there are only a few reports in children.9–12
Preoperative diagnosis of musculoskeletal hydatid cyst is difficult clinically and radiologically. It resembles soft tissue tumor. Ultrasonography(US), computed tomography(CT), and MR imaging have a valuable role in the radiologic diagnosis and follow-up of hydatid disease.4,9,13 MRI is capable of adequately demonstrating most features of hydatid disease.8,9,13 Double-layer wall, daughter cysts and water–lilly sign are the specific findings.8–13 The detachment of the germinative membrane from pericyst (water–lily sign) is considered to be pathognomonic and is reported in locations other than the liver and lung9 in our case; hydatid cyst was determined with MRI. Radiological view was useful for differentiating hydatid disease and other diseases such as muscle malignancy.
In musculoskeletal involvement of hydatid disease, blood culture cannot be useful for diagnosis. And our case's blood test was normal except for indirect hemagglutination test. This case report is the first hydatid cyst reported in vastus lateralis at childhood. Diagnosis of echinococcosis should be considered when slowly growing soft tissue mass is present in a patient from rural area especially endemic countries.2,5,6,9 Biopsy can be done for histopathological diagnosis but it must be known that this infection can be spread after direct inoculation. We do not recommend routine biopsy.
Surgery is the most effective way to treat hydatid cysts. Complete surgical resection and medical therapy is the preferred treatment for isolated echinococcosis.6–14 Rupture or spoilage of cysts should be avoided to prevent local or distant dissemination and immediate anaphylaxis.15,16 Irrigation should be made in operation with hypertonic saline in an attempt to kill scoleces.5–7,17 We performed wide resection with muscle combined with hypertonic saline irrigation.
Medical therapy is used to reduce the rate of local recurrence after radical resection.18 Mebendazol and albendazol are used for hydatid disease, but albendazol has better intestinal absorption and a higher concentration within cystic material, making it a more effective treatment.18 In our case, albendazol was used for medical therapy.
4. Conclusion
In conclusion hydatid cyst in vastus lateralis is a very rare disease. Hydatid cyst should be kept in mind when observing soft tissue mass of the extremities in patients from areas endemic of Echinococcus granulosus.
Conflict of interest
None declared.
Funding
None.
Ethical approval
Not required.
Author contributions
Ozgur Çiçekli was involved in data collection and Turgut Akgul was involved in writing the paper.
Contributor Information
Özgür Çiçekli, Email: drozgurc@gmail.com.
Turgut Akgül, Email: trgtakgul@gmail.com.
References
- 1.Giri S., Parija S.C. A review on diagnostic and preventive aspects of cystic echinococcosis and human cysticercosis. Trop Parasitol. 2012;2:99–108. doi: 10.4103/2229-5070.105174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Budke C.M., Carabin H., Ndimubanzi P.C., Nguyen H., Rainwater E., Dickey M. A systematic review of the literature on cystic echinococcosis frequency worldwide and its associated clinical manifestations. Am J Trop Med Hyg. 2013;88:1011–1027. doi: 10.4269/ajtmh.12-0692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beggs I. The radiology of hydatid disease. AJR Am J Roentgenol. 1985;145:639–648. doi: 10.2214/ajr.145.3.639. [DOI] [PubMed] [Google Scholar]
- 4.Dahniya M.H., Hanna R.M., Ashebu S., Muhtaseb S.A., el-Beltagi A., Badr S. The imaging appearances of hydatid disease at some unusual sites. Br J Radiol. 2001;74:283–289. doi: 10.1259/bjr.74.879.740283. [DOI] [PubMed] [Google Scholar]
- 5.Merkle E.M., Schulte M., Vogel J., Tomczak R., Rieber A., Kern P. Musculoskeletal involvement in cystic echinococcosis: report of eight cases and review of the literature. AJR Am J Roentgenol. 1997;168:1531–1534. doi: 10.2214/ajr.168.6.9168719. [DOI] [PubMed] [Google Scholar]
- 6.Sreeramulu P.N., Krishnaprasad, Girish Gowda S.L. Gluteal region musculoskeletal hydatid cyst: case report and review of literature. Indian J Surg. 2010;72:302–305. doi: 10.1007/s12262-010-0096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arazi M., Erikoglu M., Odev K., Memik R., Ozdemir M. Primary echinococcus infestation of the bone and muscles. Clin Orthop Relat Res. 2005;(432):234–241. doi: 10.1097/01.blo.0000149816.86222.2d. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Diez A.I., Ros Mendoza L.H., Villacampa V.M., Cozar M., Fuertes M.I. MR1 evaluation of soft tissue hydatid disease. Eur Radiol. 2000;(10):462–466. doi: 10.1007/s003300050077. [DOI] [PubMed] [Google Scholar]
- 9.Kerimoglu U., Kapicioglu S., Emlik D., Arazi M., Ural O. Hydatid disease with water lily sign manifesting as a soft-tissue mass in the calf of a child. Radiology. 2010;256:1007–1010. doi: 10.1148/radiol.10081066. [DOI] [PubMed] [Google Scholar]
- 10.Erol B., Tetik C., Altun E., Soysal A., Bakir M. Hydatid cyst presenting as a soft-tissue calf mass in a child. Eur J Pediatr Surg. 2007;17:55–58. doi: 10.1055/s-2007-964949. [DOI] [PubMed] [Google Scholar]
- 11.Marwah S., Subramanian P., Marwah N., Rattan K.N., Karwasra R.K. Infected primary intramuscular echinococcosis of thigh. Indian J Pediatr. 2005;72:799–800. doi: 10.1007/BF02734157. [DOI] [PubMed] [Google Scholar]
- 12.Dudkiewicz I., Salai M., Apter S. Hydatid cyst presenting as a soft-tissue thigh mass in a child. Arch Orthop Trauma Surg. 1999;119:474–475. doi: 10.1007/s004020050025. [DOI] [PubMed] [Google Scholar]
- 13.Guthrie J.A., Lawton J.O., Chalmers A.G. Case report: the MR appearances of primary intramuscular hydatid disease. Clin Radiol. 1996;51:377–379. doi: 10.1016/s0009-9260(96)80122-x. [DOI] [PubMed] [Google Scholar]
- 14.Ozdemir G., Zehir S., Ozdemir B.A., Sipahioğlu S., Severge U. Hydatid cyst involvement of shoulder and deltoid muscle: a case report. Eklem Hastalik Cerrahisi. 2012;23:173–176. [PubMed] [Google Scholar]
- 15.Ozkoc G., Akpinar S., Hersekli M.A., Ozalay M., Tandogan R. Primary hydatid disease of the quadriceps muscle: a rare localization. Arch Orthop Trauma Surg. 2003;123:314–316. doi: 10.1007/s00402-003-0512-1. [DOI] [PubMed] [Google Scholar]
- 16.Combalia A., Sastre-Solsona S. Hydatid cyst of gluteus muscle. Two cases. Review of the literature. Joint Bone Spine. 2005;72:430–432. doi: 10.1016/j.jbspin.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Adas G., Arikan S., Kemik O., Oner A., Sahip N., Karatepe O. Use of albendazole sulfoxide, albendazole sulfone, and combined solutions as scolicidal agents on hydatid cysts. World J Gastroenterol. 2009;15:112–116. doi: 10.3748/wjg.15.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arif S.H., Shams-Ul-Bari, Wani N.A., Zargar S.A., Wani M.A., Tabassum R. Albendazole as an adjuvant to the standard surgical management of hydatid cyst liver. Int J Surg. 2008;6:448–451. doi: 10.1016/j.ijsu.2008.08.003. [DOI] [PubMed] [Google Scholar]


