Abstract
Objective
The purpose of this secondary data analysis was to examine the relationship of individual sociodemographic variables, life events, chronic stressors including asthma control and management and environmental stressors to maternal depression.
Design
Cross sectional descriptive design study consisting of baseline data from participants enrolled in a randomized clinical trial of an asthma communication educational intervention.
Sample
Two hundred and one mothers of children with asthma (ages 6-12) recruited from community pediatric practices and pediatric emergency departments of two urban university hospitals. Measurement: Subjects responded to a questionnaire that included sociodemographic characteristics, life events, and chronic stressors. Depressive symptoms were assessed with the CESD.
Results
Close to 25% of the mothers had a score of 16 or greater on the CESD. Significant bivariate relationships between low education, unemployment, feeling unsafe, and the use of quick relief asthma drugs with high depressive symptoms were found. In the multiple logistic regression models, education or unemployment (in separate models) and the use of quick relief medications for asthma were positively associated with depressive symptoms.
Conclusions
Implications for practice include the need to assess for the presence of maternal depression particularly in mothers of children with a chronic illness such as asthma.
Keywords: asthma, depressive symptoms, mothers, chronic illness
Introduction
Depression is one of the most prevalent psychiatric illnesses and is particularly common in women of childbearing age (Burke, 2003). The National Co-Morbidity Replication Survey conducted between 2001–2003 estimated that the prevalence of lifetime major depression to be 16. 9 % overall with a higher prevalence in females (20.2%) compared to males (13.2%) (Kessler, Berglund, Demler, Merikangas, & Walters, 2005). A recent review of data collected from the National Survey of Families and Household for several years (1987–1994) found that the correlates of persistent depressive symptoms include age (less than 30), ethnicity (African American), marital status, education, and being indigent (Pascoe, Stolfi, & Ormond, 2006). Depressive symptoms are particularly prevalent among low-income African American mothers of young children (Coiro, 2001; Lazear, Pires, Isaacs, Chaulk, & Huang, 2008)
In addition to traditional sociodemographic risk factors for depression, the relationship of adverse life events to psychological functioning has been clearly identified for several decades for adults (Cohen, 1988; Everly & Lating, 2002). Recently there has also been a growing interest in urban environmental factors and their role in predicting mental health outcomes (Mulvaney & Kendrick, 2005; Aneshensel et al, 2007; Siefert et al, 2007; Kawachi & Berkman, 2003; Cutrona et al, 2005). In particular, there is a growing interest in the role and impact of violence on the mental health of individuals as well as childhood lung function and asthma morbidity outcomes (Suglia, Ryan, Laden, Dockery, & Wright, 2008; Wright, 2006). Exposure to violence has been conceptualized as a chronic psychosocial stressor. There is also a growing awareness that if caregivers experience chronic stressors, in this case exposure to community violence, their children may also experience the same stressors (Shalowitz et. al, 2001).
Finally, depressive symptoms have also been described among mothers of children with chronic illness (Shalowitz, Berry, Quinn & Wolf, 2001). Mental health symptoms are common in caregivers of children with asthma (Brown et al, 2006). Almost half (47%) of mothers of inner city children with asthma had significant levels of depressive symptoms based on using the Center for Epidemiologic Studies-Depression (CES-D) scale (Bartlett, Krishnan, Reikert, Butz, Malveaux, & Rand, 2004). Wade and colleagues(1997) found that 50% of 1528 caregivers of inner city children with asthma had significant symptom severity based on a Brief Symptom Inventory (BSI). The relationship of caregiving stress to depression has long been recognized in the literature and may be related to the physical strains, financial constraints, emotional effects and social isolation of caring for a child with complex medical needs (Kuster & Merkle, 2008). In a recent study, parenting stress in caregivers of children with asthma was related to limitation of activities and the parents own health conditions (Chio & Hsieh, 2008).
Understanding the correlates of depressive symptoms of mothers of children with a chronic disease is important for several reasons. Depressive symptoms in caretakers for example has been associated with poor asthma outcomes in children including greater use of acute care services, including emergency departments (ED) (Bartlett, Kolodner, Butz, Eggleston, Malveaux, & Rand, 2001). Brown et al (2006) found that a depressive disorder (not just symptoms) was associated with an increase in unscheduled pediatric clinic visits although there was not an increase in hospitalizations or (ED) visits. Depressive symptoms have also been associated with illness management. Mothers with higher depressive symptoms reported more problems with their child using inhalers properly and forgetting doses of medication (Bartlett et al, 2004).
The purpose of this study was to examine the relationships among maternal demographic variables, experiences with life events, chronic stressors focused on their child’s asthma management and environmental stressors related to community violence and symptoms of depression. Our study hypothesis was that in addition to sociodemographic variables, and life stressors or/events, chronic stressors would be related to maternal depressive symptoms. In particular, we hypothesized that asthma management and exposures to community violence would be related to maternal depressive symptoms.
Conceptual Framework
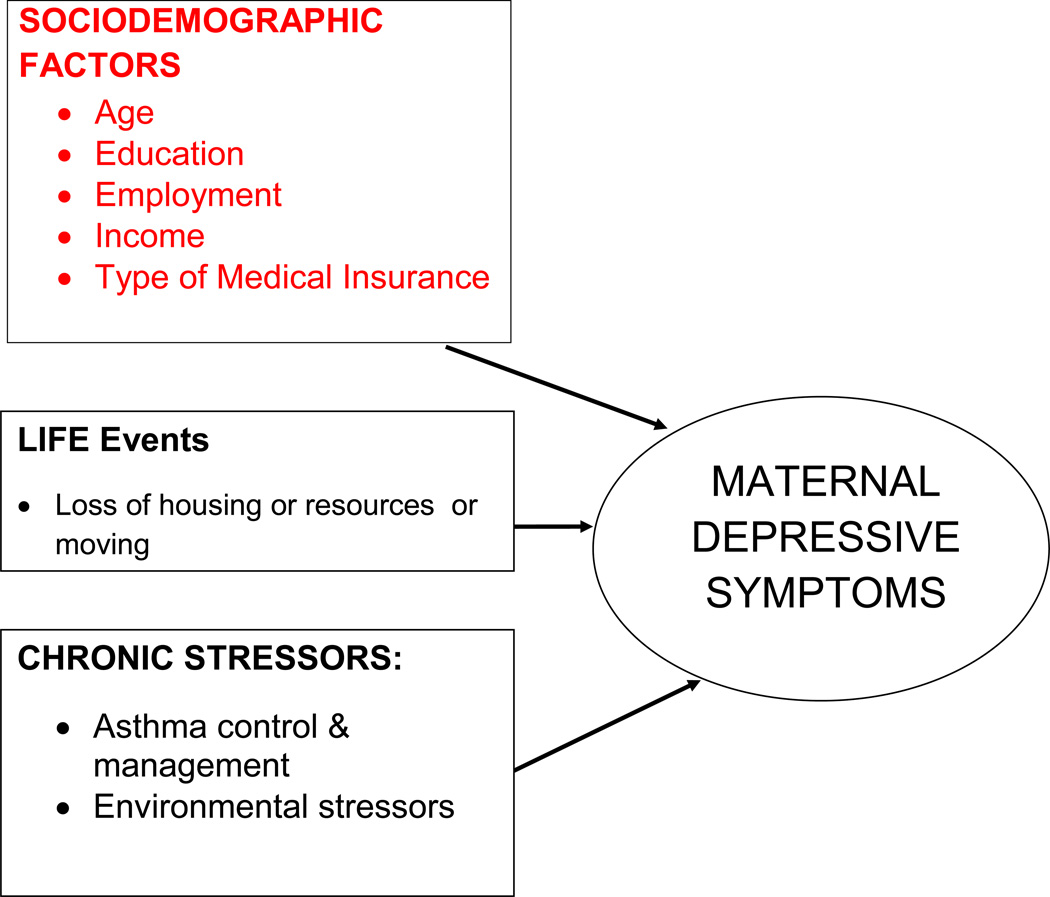
The term stress, which was introduced into the health sciences in 1926 by Hans Selye, refers to a physiological reaction, or response ( Everly & Lating, 2002). The term stressor refers to the stimulus that engenders the response. The stress process serves as an ideal conceptual model to examine the impact of numerous determinants of health status (Wenzel, Glanz, & Lerman, 2002; Pearlin, 1983; Cohen, 1988; Everly & Lating, 2002). This model posits that environmental and psychosocial stressors are associated with physiological, psychological, and behavioral responses (Israel, Farquhar, Schulz, James, & Parker, 2002). Stress has often been conceptualized as major life events, which are discrete events that disrupt normal activities and often require adaptive responses. It also includes chronic stressors which are defined as “the problems, challenges, and difficulties that people experience during extended periods of time in their daily lives” (Israel et al, 2002, p. 343). In this study, the conceptual framework guiding the study is based on numerous determinants and their relationship to maternal depressive symptoms (Figure 1). The present study examines the relationships between demographic variables (age, income, education, health insurance, and employment), life events, chronic stressors (asthma management and control and exposures to violence in the community) and maternal depressive symptoms.
Figure 1.
Methods
Research Design
The study was a secondary data analysis of baseline data collected from participants enrolled in a randomized clinical trial examining the effectiveness of an asthma communication educational intervention. The intervention was aimed at increasing the caregiver and/or child communication skills for use with the child’s primary care provider. Baseline socio-demographic and health data were collected via face to face. Baseline survey data collected from the mothers only are presented in this manuscript. The institutional review boards of the Johns Hopkins University Medical Institutions and the University of Maryland School of medicine approved the study protocols. Informed consent from all the participating parents or caregivers were obtained and assent from children were also obtained.
Sample
The caregivers (231) and child participants were recruited from community pediatric practices and pediatric emergency departments of two urban university hospitals from December 2004 through December, 2006. The participants did not differ between the various recruitment sites. Both emergency departments care for low income inner city patients. Caregiver inclusion criteria included having a child age 6–12 years of age with persistent asthma, current use of asthma medications, or having one or more ED visits or hospitalizations during the past 12 months. Of the 666 children with asthma screened, 243 were eligible and 231 or 95% were enrolled into the study. Of the 231 parents or caregivers completing the baseline questionnaire, 201 mothers were included in the final analysis excluding stepmothers, fathers, and grandmothers. This study focused on mothers only in order to study maternal depression specifically.
Measures
Demographic Variables
Demographic data were collected via self-report on questions about the mothers and their families and included maternal race/ethnicity, level of education (less than high school, high school, and college or above), age, and type of medical health insurance for the child including Medicaid, private insurance or self pay.
Mothers were asked about the combined family income for their household. The choices were less than $10,000, $10,000–$19,999, $20,000–$29,999, $30,000–$39,999 and over $40,000. Participants had the option to refuse to answer this question. Based on these responses and the number of people living in the household, a poverty index variable using 2007 HHS Poverty guidelines was also created (Department of Health and Human Services, 2007). Based on household size and income each caregiver was categorized as below the poverty level, probable poverty or above the poverty level. The women were also asked if they were employed with the possible responses being yes or no.
Life events
Discrete life events were measured using questions that captured stressful experiences of their child moving in the last six months, losing their housing, or having their telephone, electricity or gas turned off in the last 6 months. Responses to these questions were the number of times moved and yes/no to the other two questions.
Chronic Stressors
Child asthma morbidity was measured on the baseline questionnaire using items to measure symptom frequency and was based on (1) the International Asthma and Allergies in Childhood (ISSAC) study (Asher et al, 1995), NHANES Respiratory Health and Disease (2003–2004) Questionnaire (National Health and Nutrition Examination Survey (1999) and (3) child respiratory health studies (Nafstad et al, 2004; Jaakkola et al, 2006; Hugg et al, 2007). Items include measures of asthma symptoms, impact on activity limitation, asthma control, school absences, restricted activity, day and nighttime symptoms, asthma medications, and family asthma home management. All of the children recruited into the study were categorized with mild persistent to severe asthma using national guidelines (NAEPP 2007) (U.S. Department of Health and Human Service. NIH, NHLBI. Expert Panel Report, 2007).
Asthma management requirements were ascertained by asking the mothers “how often their child’s asthma has been out of control in the past four weeks and how often their child had to use his or her “quick relief” inhaler medications. The responses to these items were none of the time, a little, some, a lot, and all of the time. Responses were dichotomized into none, a little, or some, a lot, or all of the time. Finally, the mothers were asked how many times in the last 6 months their child was treated in the emergency room but not hospitalized.
Chronic environmental stressors were conceptualized as those experiences primarily focused on exposures to violence. The mothers were asked if they had seen violence such as street fighting gang fights, shootings, stabbings, or other violence in the last six months, or if their child had seen violence in the last six months. The response to each was yes or no. In addition, to address perceptions of safety, they were asked if anything happened in their neighborhood that made them feel unsafe in the last 6 months. The response was yes or no.
Depressive Symptoms
Maternal depression was measured using The Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977). This scale is a widely used scale to measure depressive symptomatology in general populations in the community as well as psychiatric populations. It contains 20 items and the respondents indicate the frequency of symptoms using a scale of 0 -’Less than a day’, 1-”1–2 days’, 2- ‘3–4 days’ and 3- ‘5–7 days against a time frame of the past week. The scale has been used to measure levels of depressive symptomatology as well as to identify probable clinical depression. This scale correlates with the scores indictive of depression on the Zung scale (r= .90) and the Beck Depression scale (r= .81) establishing its validity (Myers & Weissmann, 1980). The dependent variable of depressive symptoms for this study was coded as a dichotomous variable based on CESD scores (0 for <16 and 1 ≥ 16). A threshold of 16 is commonly used as the likely presence of clinically significant depression (Radloff, 1977). The Cronbach’s alpha for the CES-D in our sample was 0.91.
Analytic Strategy
Descriptive statistics including frequencies and percents were calculated for the study variables and bivariate relationships were examined using the chi square or Fisher’s exact tests where appropriate for categorical variables and t-tests for continuous variables. Collinearity checks were conducted among variables measuring similar constructs or suspected to be associated, i.e. measures of socioeconomic status including education, employment and income. Significant variables (p value of < 0.05) were entered into a multiple logistic regression to determine the likelihood of depressive symptoms. Significant variables identified in bivariate analyses to be collinear were also entered into separate models. Backwards step regression was used to identify a final model. All data analyses were performed using SAS V.8.0 software.
Results
Demographics
The mothers mean age was 32.8 with a range from 21- 49. Ninety six percent of the mothers identified themselves as African Americans. Approximately one- third of the mothers had not graduated from high school (31.8%), 36.8% had completed high school or an equivalent, while the remaining mothers reported some years in college. Mean child age was 8.02 years (SD 1.9) and most children (88.3%) had Medicaid health insurance. Of those mothers who reported income (n= 151), 58.3% made less than $20,000 and 42.5% of the sample was unemployed. When families were classified into the categories using the poverty index, 52% met the criteria for poverty.
Life Events
The prevalence of life events are presented in Table 1. Approximately 16% or 32 of the women had experienced their gas, phone or electricity being turned off. Approximately 7 percent or 13 of the mothers reported losing their housing and 31 families (16%) had moved in the last 6 months.
Table 1.
Life Events by Depressive Symptoms.
| Variable | N | Depressive Symptoms | P value | |
|---|---|---|---|---|
| Low | High | |||
| 145(75.5%) | 47(24.5%) | |||
| Electricity cut off | ||||
| Yes | 32 | 75% | 25.0% | .95 |
| No | 169 | 74.6% | 25.4% | |
| Lost Housing | ||||
| Yes | 13 | 61.5% | 38.5% | .25 |
| No | 186 | 75.8% | 24.2% | |
| Times child moved | ||||
| None | 158 | 74.7% | 25.3% | .20 |
| 1 or more | 31 | 64.5% | 35.5% | |
Chronic Stressors (asthma management requirements, environmental stressors)
Eighty five percent of the children were seen in the emergency department in the past six months. From mothers’ reports of the severity of their child’s asthma, nineteen of the children (10%), reported their child were “a lot” or “ always” out of control while 38 percent of the mothers reported their child used quick relief drugs “a lot” or “always.
Mothers reported that both for themselves and children, seeing violence was not unusual. Close to 20 % or 39 of the mothers had seen violence in the last 6 months while they reported that 25 or 13% of their children had seen violence. A slightly larger percentage (23%) of the mothers (N= 47) also reported that they had seen something in their neighborhood that made them feel unsafe.
Bivariate relationships with Maternal Depression
In this sample, there were 24.5 % of the mothers with a score of 16 or greater on the CESD, indicating probable depression. There was no significant difference in mean parent age between those mothers reporting high depressive symptoms (Mean age −31) and those reporting low symptoms (Mean age- 29). Comparisons of mothers reporting low versus high depressive symptoms for demographic variables are presented in Table 2. Mothers with an education level less than college were significantly more likely to report high depressive symptoms (p=.02). Unemployment was related to maternal depressive symptoms (p=.026). Of unemployed moms, 32.9% reported CES-D scores greater than 16, while only 18.2% of those employed reported CES-D scores within this range. No life event variable was related to depressive symptoms (Table 1). Of the chronic stressors, there was no relationship between maternal report of asthma being out of control or the number of ED visits and depressive symptoms. The mean number of emergency room visits was 1.91 for mothers with low depressive symptoms and 1.96 for mothers scoring 16 or greater on the CESD. There was a significant association, however, between increased quick relief medication use and depressive symptoms. Close to 36% of those mothers reporting that their child had high quick relief medication use also reported high depressive symptoms compared to 18 percent of those mothers reporting less use of quick relief meds (p=.006) (Table 3) .
Table 2.
Sociodemographic Characteristics of Mothers of Children with Asthma Low and High in Depressive Symptoms. ( N=192)
| Variable | N | Depressive Symptoms | P value | |
|---|---|---|---|---|
| Low | High | |||
| 145(75.5%) | 47(24.5%) | |||
| Age | N | (%) | (%) | |
| 21–24 | 21 | 11.4% | 11.9% | |
| 25–34 | 100 | 51.8% | 64.3% | .21 |
| 35–50 | 62 | 36.9% | 23.8% | |
| Education | ||||
| High school or less | 133 | 70.7% | 29.3% | .02 |
| College | 59 | 86.4% | 13.6% | |
| Insurance Type | ||||
| Medical Assistance | 158 | 81.2% | 81.3% | .21 |
| Private or self pay | 32 | 18.8% | 10.9% | |
| Employment | ||||
| Yes | 110 | 62.1% | 42.5% | .02 |
| No | 82 | 37.9% | 57.5% | |
| Annual Income | ||||
| <$10,000 | 48 | 31.2% | 68.8% | |
| $10,000–19,999 | 35 | 11.4% | 88.8% | |
| $ 20,000- $29,999 | 23 | 21.7% | 78.3% | .32 |
| $30,000- $39,999 | 22 | 22.7% | 77.3% | |
| >$40,000 | 16 | 18.8% | 81.25% | |
| Poverty Index | ||||
| Possible/No | 71 | 81.7% | 18.3% | .24 |
| Yes | 80 | 73.8% | 26.2% | |
Table 3.
Chronic Stressors by Depressive Symptoms.
| Variable | N | Depressive Symptoms | P value | |
|---|---|---|---|---|
| Low | High | |||
| 145(75.5%) | 47(24.5%) | |||
| Asthma Out of Control | ||||
| None/A little | 173 | 23.1% | 76.8% | .19 |
| A lot/always | 19 | 36.8% | 63.2% | |
| Quick Relief Meds | ||||
| None/A little | 122 | 82.0% | 18.0% | .006 |
| A lot/always | 70 | 64.3% | 35.7% | |
| Maternal Perceptions of being unsafe | ||||
| Yes | 47 | 63.8% | 36.2% | .05 |
| No | 154 | 77.9% | 22.1% | |
| Mother saw violence | ||||
| Yes | 39 | 69.2% | 30.8% | .40 |
| No | 161 | 75.8% | 24.2% | |
| Child saw violence | ||||
| Yes | 25 | 64.0% | 36.0% | .17 |
| No | 175 | 76.6% | 23.4% | |
Of the environmental stressors, the perception of feeling unsafe in the neighborhood was the only variable related to maternal depression (p value <.05). Almost one-third (32%) of mothers who reported feeling unsafe also reported depressive symptoms compared to 22% of those mothers reporting depressive symptoms but not feeling unsafe. Seeing violence for either the mothers or children was not related to maternal depressive symptoms.
Multivariate Models
Variables included in the full multivariate model were chosen based on significant bivariate relationships or variables with theoretical importance such as age (Table 4). Variables included were the use of quick relief medications, feeling unsafe, parental age as a continuous variable, education of the mothers and employment status. The full model results clearly show that only two of the variables (unemployment and high use of quick relief meds) were significant. Because of multicollinearity however between education and employment (chi square 5.17- p=.02) employment without education was entered in one regression model (Final Model 1) and education without employment (Final Model 2) along with the other variables. Insignificant variables were eliminated one step at a time for each of these models. Results based on backwards step logistic regression are shown in the second column and third columns. Employment and the use of quick relief medicines were retained in Final Model 1. Unemployment was a risk factor with those mothers who were unemployed 2.4 times more likely to report depressive symptoms. Mothers reporting the use of quick relief medications at a lot or always were over two and half times (2.8) more likely to report depressive symptoms than those mothers reporting less use of quick relief medications. The final model that includes education without employment status shown in Table 4, Model 2, reveals that mothers with an education of high school or less were 2.7 times more likely to report high depressive symptoms and mothers reporting higher use of quick relief meds were 2.4 times more likely to report high symptoms.
Table 4.
Adjusted Odds Ratios (AORs) of Associations Between Depressive Symptoms and Demographic characteristics and Stressors (n=183)
| Full Model 1 | Final Model 1 | Final Model 2 | ||||
|---|---|---|---|---|---|---|
| Demographic Characteristics | AOR (95% CI) | p value | AOR(95% CI) | p value |
AOR(95% CI) | p |
| Parent Age | .99(.94, 1.05) | .80 | ||||
| Educational Level (No High School/High School or college | 2.12 (.83, 5.40) | .11 | 2.62 (1.07, 6.39)- | .03* | ||
| Employment Status (No, Yes) | 2.18(1.04, 4.60) | 0.04* | 2.38 (1.16, 4.90) | .02* | x | |
| Stressors | ||||||
| Perceptions of Feeling Unsafe (Yes, No) | 1.86(.83, 5.40) | 0.13 | ||||
| Use of Quick Relief Meds (A lot, none/some) | 2.45(1.18, 5.13) | .02* | 2.74(1.33, 5.66) | .006** | 2.40 (1.18, 4.91)- | .02* |
p value < 0.05
p value < 0.01
Discussion
Maternal depressive symptomatology was assessed in mothers of children attending an urban pediatric primary care practice in Baltimore close to twenty years ago using the CES-D scale (Orr, James, Burns, & Thompson, 1989). The percentage of mothers with scores in the depressed range (16 or greater) on the CES-D in this study (25%) was less than reported in the study reported by Orr and colleagues (38.3%). More recently, in a study of 177 mothers of young minority children with asthma residing in Baltimore and Washington DC, almost half (47%) of the mothers reported clinically significant levels of depressive symptoms using a shortened version of the CES-D (Bartlett et. al, 2004). One explanation for the lower CES-D scores in our data may be due to the difference between the shortened CES-D scale used in the Bartlett study and the complete CES-D used in our data, although the brief version of the CES-D has been shown to have good predictive accuracy when compared with the full length version (Irwin, Artin, & Oxman, 1999; Andresen, Malmgren, Carter, & Patrick, 1994).
However our findings of the correlates with depression are congruent with other studies. Lower maternal education level (high school or less), unemployment, and having a child who needed quick relief medications were all associated with high depressive symptoms. These socioeconomic related variables (education and employment) are often correlated and are also related to income. What our results seem to suggest is that some measure or proxy for socioeconomic status is important when predicting maternal depressive symptomatology.
More acute life events were not related to depressive symptoms for these women. We did find a significant relationship with one environmental chronic stressor (that of feeling unsafe) in the bivariate relationship but this was no longer significant in the multivariate model. Many of the neighborhoods that these women come from are known for their level of violence and crime. It is also noteworthy that the children, like their parents, were exposed to similar violence exposure events in this study, supporting the claim that when caregivers experience life stressors, their children may also experience the same life stressors (Shalowitz, Berry, Quinn & Wolf, 2001).
Although feelings of being unsafe was not significant in the multivariate model, the nature of these neighborhoods, and the relationship of neighborhoods to depressive symptomatology deserves further study. There is certainly evidence in the literature of the role of neighborhood disorder and its impact on health (Hill, Ross, & Angel, 2005; Steptoe & Feldman, 2001; Gary, Stark, & LaVeist, 2006). A previous study in Detroit found that stressors such as neighborhood disorder and discrimination independent of household income influenced depressive symptoms. Household income in another study did not protect African American women residing in a high poverty community (Schulz et al. 2005).
In this study, having a child with asthma requiring quick relief treatment was strongly related to depressive symptoms. It is a well known fact that the use of daily anti-inflammatory agents remain underused in inner-city children (Warman, Silver & Stein, 2001; Lieu et al, 2002; Finkelstein, Lozano, Farber, Miroshnik, & Lieu, 2002) and may result in overuse of quick relief medication to control asthma symptoms. The explanation for the relationship between high quick relief medications and maternal depressive symptoms may be associated with factors related to access to health care factors. Alternative explanations may be that the use of quick relief medications is an indicator of poorly managed asthma by the family or poorly managed asthma by the healthcare system. Parental caregiver perspectives on barriers to asthma care in the Medicaid system were explored in focus groups for parents with persistent asthma (Valerio, Cabana, White, Heidmann, Brown & Bratton, 2006). In this study, barriers specific to Medicaid-insured patients included difficulty maintaining continuity of care due to physician participation. In a prior study, children whose families reported using daily antiinflammatory agents had more primary care visits in a 6 month period than children not receiving antiinflammatory agents (Warman et al, 2001). From the perspective of family management, Warren and colleagues did not find any relationship of caretaker sociodemogrpahic factors or self efficacy to the use of antiinflammatory agents while another study of 1648 children found that parental education beyond high school was protective against underuse of controller therapy. None of these studies examined the relationship of maternal depressive symptoms and the use of quick relief medications. Other measures of asthma status, perceptions of asthma control and the use of the emergency department were not related to depressive symptoms. Shalowitz and colleagues (2006), in contrast to our study, did not find any independent effects of either asthma status on maternal symptoms of depression after accounting for life stressors and social support.
There are several limitations of this study. Because the study is a cross sectional design, the ability to examine causality is impossible. Consequently, we have no way of knowing whether chronic symptoms in children influence maternal depression or if maternal depression influences childhood symptoms. In addition, the high refusal rate among the mothers to report income eliminates the ability to adequately examine income as a correlate of depressive symptoms. Finally, the sample was recruited from two inner-city emergency rooms resulting in a large proportion of the families where asthma may be more poorly managed. Therefore it may be more difficult to generalize beyond high-at risk populations.
Conclusions
The findings of this study support the relationship of the use of quick relief drugs for a child with asthma and maternal depression. Because this study was a cross sectional study, we are not able to determine the sequencing of events; whether high maternal depressive symptoms result from caring for a child with asthma or whether maternal depressive symptoms influence the ability of the mothers to care for their children resulting in increased asthma morbidity. Other research findings have documented the association of maternal depressive symptoms and asthma outcomes of children. Bartlett et al (2001) for example found a correlation between maternal depressive symptoms and problems noted with children using inhalers properly and forgetting doses of meds. The mechanisms to explain these relationships are not always so clear. Bartlett and colleagues suggested that the correlation between maternal depressive symptoms and children forgetting medication may have resulted in increased asthma symptoms requiring the mother to seek medical attention for the child, increasing her anxiety about the child’s health. Previous studies have also suggested that the mechanisms involved in explaining the relationship between maternal mental health and caring for a special needs child are complex (Shalowitz et al, 2006; Shalowitz et.al., 2001).
Nursing Implications
From a practice perspective, it is critical that public health nurses recognize and assess for the presence of maternal depression particularly in mothers of children with a chronic illness. It is generally well known that post partum depression is of concern for new mothers (Mayberry, Horowitz, & Declercq, 2007). This study contributes to the field by further providing evidence of the relationship of having a child with asthma and maternal depressive symptoms. In particular this study should alert public health nurses to the need for further mental health assessment of mothers using standardized depression instruments with certain demographic characteristics and certain health behaviors such as the use of quick relief asthma medications for their children. Depressive symptoms in mothers are important from a clinical perspective. There is certainly strong evidence that depression in mothers not only impacts the mother’s health but can also impair maternal-child relationships (Horowitz et al, 2001). There is also evidence that maternal depression is linked to child psychological dysfunction and indirectly to physical dysfunction of children with asthma (Lim, Wood, and Miller, 2008). For the public health nurse, it is important to assess maternal demographic factors and chronic stressors associated with maternal depression, with the awareness that depressive symptoms have implications for maternal and child health.
Selected bibliography
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Archives Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Aneshensel CS, Wight, Miller-Martinez D, Botticello AL, Karlamangia AS, Seeman TE. Urban neighborhoods and depressive symptoms among older adults. Journal of Geronotol B Psycholo Soc Sci. 2007;62(1):S52–S59. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, Strachan D, Weiland SK, Williams HC. International Study of asthma and allergies in childhood (ISSAC): Rationale and methods. Eur Respir. 1995;J8:483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Arch Pediatrics Adolescent Medicine. 2001;155:347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. The American Journal of Psychiatry. 1994;151(7):979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Brown ES, Gan V, Jeffress J, Mullen-Gingrich K, Khan DA, Wood BL, Miller BD, Gruchalla R, Rush AJ. Psychiatric symptomatology and disorders in caregivers of children with asthma. Pediatrics. 2006;118(6):ei1715–ei1720. doi: 10.1542/peds.2006-1119. [DOI] [PubMed] [Google Scholar]
- Burke L. The impact of maternal depression on familial relationships. International Review of Psychiatry. 2003;15:243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Chiou HH, Hsieh LP. Parenting stress in parents of children with epilepsy and asthma. Journal of Child Neurology. 2008;23(3):301–306. doi: 10.1177/0883073807308712. [DOI] [PubMed] [Google Scholar]
- Cohen LH. Life Events and Psychological Functioning. Newbury Park, California: Sage Publications; 1988. [Google Scholar]
- Coiro MJ. Depressive symptoms among women receiving welfare. Women’s Health. 2001;32(1–2):1–23. doi: 10.1300/J013v32n01_01. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology. 2005;114(1):3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services. The 2007 HHS Poverty Guidelines. 2007 Retrieved on 8/27/07 @ http://aspe.hhs.gov/poverty/07poverty.shtml.
- Everly GS, Lating JM. A clinical guide to the treatment of the human stress response. New York: Kluwer Academic; 2002. [Google Scholar]
- Finkelstein JA, Lozano P, Farber HJ, Miroshnik KI, Lieu TA. Underuse of controller medications among Medicaid-insured children with asthma. Archives Pediatric Adolescent Medicine. 2002;156(6):562–567. doi: 10.1001/archpedi.156.6.562. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Annual Epidemiology. 2007;17(3):171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health & Place. 2006;13:569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Hill TD, Ross CE, Angel RJ. Neighborhood disorder, psychophysiological distress, and health. Journal of Health and Social Behavior. 2005;46:170–186. doi: 10.1177/002214650504600204. [DOI] [PubMed] [Google Scholar]
- Horowitz JA, Bell M, Trybulski J, Munro BH, Moser D, Hartz SA, McCordic L, Sokol ES. Promoting responsiveness between mothers with depressive symptoms and their infants. Journal of Nursing Scholarship. 2001;33:323–329. doi: 10.1111/j.1547-5069.2001.00323.x. [DOI] [PubMed] [Google Scholar]
- Hugg TT, Kaakkola MS, Ruotsalainen RO, Pushkarev VJ, Jaakkola JJK. Parental smoking behavior and effects of tobacco smoke on children’s health in Finland and Russia. European Journal of Public Health. 2007;1:1–8. doi: 10.1093/eurpub/ckm053. [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10 item Center for Epidemiological Studies Depression Scale (CES-D) Archives for Internal Medicine. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Israel BA, Farquhar SA, Schulz AJ, James SA, Parker EA. The relationship between social support, stress, and health among women on Detroit’s East Side. Health Education & Behavior. 2002;29(3):342–360. doi: 10.1177/109019810202900306. [DOI] [PubMed] [Google Scholar]
- Jaakkola JJK, Kosheleva AA, Katsnelson BA, Kuzmin SV, Privalova LI, Spengler JD. Prenatal and postnatal tobacco smoke exposure and respiratory health in Russian children. Respiratory Research. 2006;7:48–57. doi: 10.1186/1465-9921-7-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanaugh M, McMillen RC, Pascoe JM, Hill Southward L, Winickoff JP, Weitzman M. The co-occurrence of maternal depressive symptoms and smoking in a national survey of mothers. Ambulatory Pediatrics. 2005;5(6):341–348. doi: 10.1367/A04-207R.1. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Neighborhoods and Health. United States: Oxford Press; 2003. [Google Scholar]
- Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, Blazer D. Sex and depression in the National Comorbidity Survey. II: cohort effects. Journal of Affective Disorders. 1994;30(1):15–26. doi: 10.1016/0165-0327(94)90147-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangus KH, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kuster PA, Merkle CJ. Caregiving stress. Immune function, and health: implications for research with parents of medically fragile children. Issues of Comprehensive Pediatric Nursing. 2004;27(4):257–276. doi: 10.1080/01460860490884165. [DOI] [PubMed] [Google Scholar]
- Lazear KJ, Pires SA, Isaacs MR, Chaulk P, Huang L. Depression among low-income women of color: Qualitative findings from cross-cultural focus groups. Journal of Minority Health. 2008;10:127–133. doi: 10.1007/s10903-007-9062-x. [DOI] [PubMed] [Google Scholar]
- Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, Quesenberry CP, Selby JV, Farber HJ. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- Lim J, Wood BL, Miller BD. Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology. 2008;22(2):264–273. doi: 10.1037/0893-3200.22.2.264. [DOI] [PubMed] [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression symptoms prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. JOGNN. 2007;36:542–549. doi: 10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- Mulvaney C, Kendrick D. Depressive symptoms in mothers of pre-school children-effect of deprivation, social support, stress, and neighborhood social capital. Social Psychiatry Psychiatric Epidemiology. 2005;40(3):202–208. doi: 10.1007/s00127-005-0859-4. [DOI] [PubMed] [Google Scholar]
- Myers JK, Weissmann MM. Use of a self-report symptom scale to detect depression in a community sample. American Journal of Psychiatry. 1980;137(9):1081–1084. doi: 10.1176/ajp.137.9.1081. [DOI] [PubMed] [Google Scholar]
- Nafstad P, Jaakkola JJK, Skrondal A, Magnus P. Day care center characteristics and children’s respiratory health. Indoor Air. 2004;15:69–75. doi: 10.1111/j.1600-0668.2004.00310.x. [DOI] [PubMed] [Google Scholar]
- National Health and Nutrition Examination Survey (NHANES) NCHS 1999–2006 Survey. Respiratory Health and Disease. Retrieved on 8/27/07 @ www.cdc.gov/nchs/data/nhanes_03_04.
- Nguyen HT, Kitner-Triolo M, Evans MK, Zonderman AB. Factoral invariance of the CES-D in low-socioeconomic status of African American compared with a nationally representative sample. Psychiatry Research. 2004;126:177–187. doi: 10.1016/j.psychres.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Orr ST, James SA, Burns BJ, Thompson B. Chronic Stressors and maternal depression: implications for prevention. American Journal of Public Health. 1989;79(9):1295–1296. doi: 10.2105/ajph.79.9.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe JM, Stolfi A, Ormond MB. Correlate of mothers’ persistent depressive symptoms: a national study. Journal of Pediatric Health Care. 2006;20(4):261–269. doi: 10.1016/j.pedhc.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Pearlin LL. Role strains and personal stress. In: Kaplan HB, editor. Psychosocial stress: Trends in theory and research. Orlando, FL: Academic Press; 1983. pp. 3–32. [Google Scholar]
- Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Applied Psychological Measures. 1977;1:385–401. [Google Scholar]
- Shalowitz MU, Berry CA, Quinn KA, Wolf RL. The relationship of life stressors and maternal depression to pediatric asthma morbidity in a subspecialty practice. Ambulatory Pediatrics. 2001;1(4):185–193. doi: 10.1367/1539-4409(2001)001<0185:trolsa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Shalowitz MU, Mijanovich T, Berry CA, Clark-Kauffman E, Quinn KA, Perez EL. Context matters: a community-based study of maternal mental health, life stressors, social support, and children’s asthma. Pediatrics. 2006;117(5):e940–e948. doi: 10.1542/peds.2005-2446. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Israel BA, Zenk SN, Parker EA, Lichtenstein R, Shellman-Weir S, Klem L. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit’s eastside. Social Science & Medicine. 2005;62:510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- Siefert K, Finlayson Williams Delva Ismail AI. Modifiable risk and protective factors for depressive symptoms in low income African American mothers. American Journal of Orthopsychiatry. 2007;77(1):113–123. doi: 10.1037/0002-9432.77.1.113. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annual Behavioral Medicine. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Suglia SF, Ryan L, Laden F, Dockery DW, Wright RJ. Violence exposure, a chronic psychosocial stressor, and childhood lung function. Psychosomatic Medicine. 2008;70(2):160–169. doi: 10.1097/PSY.0b013e318160687c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The NSFH Project. National Survey of Families and Households. 2006 Retrieved on 8/27/07 @ http://www.ssc.wisc.edu/nsfh/
- U.S. Department of Health and Human Service. NIH, NHLBI. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Full Report 2007. National Asthma Education and Prevention Program (NAEPP), 2007. 2007 Aug; NIH Publication No 07-4051. [Google Scholar]
- Valerio M, Cabana MD, White DF, Heidmann DM, Brown RW, Bratton ST. Understanding asthma management: Medicaid parents’ perspectives. Chest. 2006;129(3):594–601. doi: 10.1378/chest.129.3.594. [DOI] [PubMed] [Google Scholar]
- Wade S, Weil C, Holden G, et al. Psychological characteristics of inner-city children with asthma. Pediatric Pulmonology. 1997;24:263–276. doi: 10.1002/(sici)1099-0496(199710)24:4<263::aid-ppul5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Warman KL, Silver EJ, Stein RE. Asthma symptoms, morbidity, and anti-inflammatory use in inner-city children. Pediatrics. 2001;108(2):277–282. doi: 10.1542/peds.108.2.277. [DOI] [PubMed] [Google Scholar]
- Wenzel L, Glanz K, Lerman C. Stress, coping, and health behavior. In: Glanz K, Rimer B, Lewis F, editors. Health behavior and health education. San Francisco, CA: Jossey-Bass; 2002. pp. 210–239. [Google Scholar]
- Wright RJ. Health effects of socially toxic neighborhoods: The violence and urban asthma paradigm. Clin Chest Med. 2006;27:413–421. doi: 10.1016/j.ccm.2006.04.003. [DOI] [PubMed] [Google Scholar]