Abstract
Objectives. To describe and explore current exercise and physical activity behaviour in older adults with knee pain in the UK.
Methods. A survey was mailed to 2234 adults ≥50 years of age registered with one general practice within the UK to determine the presence and severity of knee pain and levels of physical activity. Semi-structured interviews were conducted with 22 questionnaire responders with knee pain.
Results. The questionnaire response rate was 59% (n = 1276) and 611 respondents reported knee pain. Only ∼40% of individuals with knee pain were sufficiently active to meet physical activity recommendations. Interviews revealed individual differences in the type and setting of physical activity completed and some self-monitored their symptoms in response to physical activity in order to guide future behaviour.
Conclusion. Innovative interventions that can be adapted to suit individual needs and preferences are required to help older adults with knee pain become more physically active.
Keywords: exercise, physical activity, older adults, knee pain, quantitative, qualitative, mixed methods
Introduction
Exercise, including local strengthening and general aerobic exercise, is recommended as a core treatment for older adults with knee pain, likely to be attributable to OA [1]. Although current guidelines for knee OA do not provide advice about the optimal dose of exercise and physical activity required, the American College of Sports Medicine (ACSM) recommends that adults, including those aged ≥65 years and those with chronic conditions such as OA [2, 3], should complete a minimum of 30 min/day (which can be accumulated in 10 min sessions) of moderate-intensity aerobic exercise on at least five 5 days/week for a total of ≥150 min/week, or 20 min of vigorous aerobic exercise on at least 3 days/week for a total of ≥75 min/week [3]. However, many individuals do not meet these recommendations [4], and for older adults with knee pain, activity levels can be even lower than in the general population [5], although this is relatively unexplored within the UK [5].
Older adults with knee pain face many barriers to physical activity and exercise, which can be broadly grouped into person-related factors such as their attitude towards physical activity (e.g. lack of enjoyment), the knee problem itself, including symptoms felt during and after activity, and social and environmental factors (e.g. the presence or not of an exercise buddy) [6]. Interventions to increase physical activity in older adults with knee pain not only need to address these barriers, but also need to be acceptable to this patient group so that physical activity behaviour is initiated and then maintained over time [7]. There is currently limited understanding about the physical activity behaviour of older adults with knee pain, particularly in the UK, including the type and intensity of physical activity undertaken and why these behaviours exist. This information would be valuable in helping to design acceptable physical activity interventions for older adults with knee pain. The objectives of this study were therefore to describe the levels of physical activity among a sample of older adults in the UK, to compare these between individuals with and without knee pain and between those with differing severities of knee problems and to qualitatively explore the exercise and physical activity experiences of older adults with knee pain.
Methods
Participants
We undertook a postal survey and semi-structured interviews with adults aged ≥50 years registered with one general practice in the UK. Following ethics approval from the Cheshire East Local Research Ethics Committee (REC reference 06/Q1503/12), data were gathered sequentially: questionnaire surveys were completed and their analyses then guided the content and focus of the semi-structured interviews. All participants provided informed consent according to the Declaration of Helsinki. For clarity, the survey and interview methods and results are presented separately and then discussed together to facilitate a comprehensive exploration of the findings [8].
The survey
A cross-sectional questionnaire was mailed to a computer-generated simple random sample of 2150 older adults registered with one large general practice in central Cheshire (in total, 8158 patients aged ≥50 years were registered with the practice). In order to optimize response, a reminder postcard was sent at 2 weeks and a second questionnaire was mailed to all non-responders at 4 weeks. A screening question within the questionnaire identified individuals with knee pain (defined as any ache, pain, discomfort or stiffness experienced in or around the knee joint within the last 12 months) [9]. Within those who reported knee pain, two further groups were identified, based on the Chronic Pain Grade (CPG) [10]: those with low knee pain intensity and low disability (defined as CPG group I) and those with high pain intensity but low disability or high disability that is moderately or severely limiting (CPG groups II–IV combined). Individuals within CPG II–IV can be defined as having clinically significant pain and are more likely to have consulted a health care professional about their knee problem [11–13]. This cut-off was used to explore differences in physical activity behaviour of individuals with differing severities of knee problem.
Based on the results of previous research [9, 14, 15] and a pilot study (n = 180), it was anticipated that the survey would achieve ∼480 responses from older adults reporting knee pain, of whom ∼260 would be in CPG I and 220 would be in CPG II–IV [14, 15]. This would allow survey estimates (proportions) to be calculated with a margin of error of <5% and with 95% confidence. Only very minor changes to the questionnaire were made following the pilot study, hence responders to the pilot study were combined with the main study responders for analyses.
Survey instrument
A questionnaire was developed that included questions on respondents’ personal characteristics and their general health [including the 12-item Short Form Health Survey (SF-12)] [16] as well as questions to describe individuals’ knee problems. These included the Knee Pain Screening Tool, a validated, short questionnaire designed to act as an initial screen to identify those who have knee pain in the general population [9], the WOMAC [17] and the CPG [10], both used to determine the severity of participants’ knee problems. Physical activity was measured by the Short Telephone Activity Recall Questionnaire [18], adapted for use in a postal questionnaire. This measure of physical activity was chosen from the plethora available, as its measurement properties have been tested and found adequate for use in older adult populations [19], and it is relatively brief, making it suitable for inclusion alongside other questions within a large questionnaire.
Survey data analysis
Data analyses were carried out using the Statistical Package for Social Science (SPSS, version 14; IBM, Armonk, NY, USA). Descriptive analyses were completed to describe the sample, the severity of knee problem, the proportion meeting the 2007 ACSM physical activity recommendations (the physical activity recommendations at the time of the survey, which recommended a minimum of 30 min of moderate-intensity aerobic exercise ≥5 days/week or 20 min of vigorous aerobic exercise at least 3 days/ [2]) and the proportion who were inactive (i.e. completed moderate to vigorous activity of <10 min duration <1 day/week [18]. Pearson’s chi-squared and Yates’ correction for continuity were used to investigate whether there were any statistically significant differences in physical activity behaviour between individuals with and without knee pain and between those with differing severities of knee pain (between individuals grouped as CPG I and CPG II–IV).
The interview study
Face-to-face semi-structured interviews were completed with a sample of older adults with knee pain who had completed and returned the questionnaire and provided consent for further contact. To ensure variation in the interview sample, interviewees were purposefully selected based on their questionnaire responses and included both males and females of different ages with varying severity of knee problem and levels of physical activity. We aimed to conduct between 20 and 30 interviews guided by saturation of key themes.
The interview guide
Participants were probed about their exercise and physical activity experiences. Qualitative data analyses of early interviews guided further data collection, allowing the interview guide to be modified with ongoing analysis and facilitating a thorough exploration of emerging themes. One researcher completed all interviews (M.H.), which were audiotaped, transcribed verbatim and anonymized for analysis. Data collection ceased when no new key themes were emerging.
Interview data analyses
Interview data were thematically analysed, aided by the computer software package NVivo version 2.0 (QSR International, Doncaster, VIC, Australia). Analysis was based on the constant comparison method [20, 21]. The lead author reviewed interview transcripts and, by constantly searching for commonalities and contrasts within the data, identified and developed themes that were clustered into categories that shared meanings, and links between categories were explored [21, 22]. Emerging ideas were discussed and checked for credibility by other members of the study team, who independently coded four transcripts. In the final stages of analysis, a qualitative researcher independent of the study team analysed two interview transcripts and her interpretation of the interviews was compared with that of the research team. In Table 1, themes are grouped with categories and verbatim anonymized quotations are used to exemplify each theme.
Table 1.
Categories, themes and verbatim examples from the interviews
| Category and theme | Verbatim example |
|---|---|
| Type of exercise or physical activity | |
| Therapeutic exercise | Well one, I lie, you have to lie flat on the bed and I have to lift me knee up and hold it up as long as I can, then let it down and then you lift one leg over the other one that’s straight and then you try to lift. You can feel that it’s stretching, it sounds silly, but it does do your knees good. They click a bit, but, it does do them good. #534 |
| Lifestyle activity | I suppose I combine the exercises with the way I live and the way I bend down for things, like this afternoon, I was putting some shopping away in the cupboards, the lower cupboards, so, I squat rather than kneel down, I’ll squat to try and make my quads stronger. #537 |
| Preference about type of exercise | What doesn’t help is I used to do a lot of walking and walking seemed to compound the situation more than it should have done, so I gave up walking and took to cycling. Cycling’s been the winning factor … . #304 |
| I don’t like bike riding, I hate bikes, I just don’t want any bikes, I’ve had enough bikes when I was small. I have an aversion totally … . #1178 | |
| Dose | |
| Amount | If there are days when it’s particularly bad, sometimes it’ll go into two or three days or so, and then I just do what I can. I still move about, but more slowly and I use the stair lift more. When I don’t have to use the stair lift, I’ll walk upstairs, because that’s helping to keep the knee muscles built up. #983 |
| The last couple of years, I was going through a divorce so obviously, motivation to race, just time allocation, everything was topsy-turvy for a while but that’s all sorted now. #442 | |
| Moderate-intensity exercise | If you’ve ever felt a, sort of, jar in your knee when you’ve landed on it, it makes you wary of the high impact stuff and the exercise people don’t recommend it at our age. They do these over 50’s classes now, which are lower impact. I’m sure keeping it gently going is the best bet, it seems to work for me anyway. #930 |
| Listen to your body | Sitting with it up is not comfortable, it’s better to have it down and then, as you said, gradually just keep, if you like, swinging it and then you’re moving the joints, as long as it doesn’t hurt. It just tells you to listen to your body really, that’s what it’s saying. #1115 |
| Previous exercise experiences guide behaviour | It’s, you know, I know if it’s like a push-off movement with a twist in it, I’d fall over. There’s no doubt about that because I’ve done it. So, you learn by, you know, if someone keeps prodding you with a pin, in the end you just say don’t, it hurts me (laughs). #537 |
| Setting of exercise | |
| Home | I’m restricted because of the wife and not being able to leave her for any length of time, all this medication that doesn’t help because a couple of hours after you’ve had it, it has adverse affects, but it seems to wear off, then, so exercising in a group, I don’t think I’d be able to accommodate it now, much as I’d like to. That’s the way it is, at the moment. #993 |
| With others | I think doing exercises on your own, unless you’re a very introverted person, is very boring. You go to a class and you all have a bit of a joke and join in, you know, and you all say I can do it with this leg and I can’t do it with that leg, or arm, or whatever. I think it’s good psychologically to be gathered in a crowd and also, to know that there are people who are worse off than you are. It doesn’t half boost the morale, it doesn’t do any harm to see people who are struggling more than you are. I think, also, that give you the impetus to work at it, myself. #930 |
Results
Survey findings
Response
Of the 2330 participants included in the initial sample [main study (n = 2150) and pilot study (n = 180) combined], 180 were excluded [e.g. due to death, moving, changing their general practitioner (GP), judged not appropriate to be invited to participate in the study by their GP] and there were 1276 responses (adjusted response rate 59%). The characteristics of the sample are shown in Table 2. The mean age of responders was 66 years, 54% were women, 48% (n = 611) reported knee pain in the last 12 months and ∼60% reported having one or more health problems, most commonly high blood pressure, heart disease, asthma and diabetes, irrespective of the presence of knee pain. Individuals with knee pain were more likely to be overweight or obese (60% vs 48%) and have other joint pain (90% vs 69%) than individuals with no knee pain. With regard to their knee pain, 386/611 individuals (67%) were classified in CPG I (i.e. low disability–low intensity) and 194/611 individuals (33%) were classified in CPG II–IV (i.e. low disability–high intensity to high disability–severely limiting). Those in CPG II–IV had higher WOMAC pain, function and stiffness scores (8.2 vs 2.8, 28.7 vs 9.0 and 3.9 vs 1.6, respectively), indicating more severe knee problems. They also reported having had their knee pain longer (pain present for ≥3 months, 70% vs 26%) and were more likely to have consulted their GP or used other health care services for their knee pain in the last 12 months than those in CPG I (51% vs 13% and 63% vs 22%, respectively).
Table 2.
Characteristics of survey responders
| Characteristic | Sample without knee pain (n = 665) | Total sample with knee pain (n = 611) | Within those with knee pain |
|
|---|---|---|---|---|
| CPG group I (n = 386) | CPG group II–IV (n = 194) | |||
| Age, n (%), years | ||||
| 50–59 | 193 (32) | 213 (35) | 163 (42) | 46 (24) |
| 60–69 | 194 (32) | 190 (31) | 113 (29) | 70 (36) |
| 70–79 | 162 (27) | 147 (24) | 86 (22) | 50 (26) |
| ≥80 | 60 (10) | 61 (10) | 24 (6) | 28 (14) |
| Gender, n (%) | ||||
| Female | 313 (51) | 349 (57) | 217 (56) | 107 (55) |
| Education status, n (%) | ||||
| Higher educationa | 185 (32) | 167 (29) | 130 (35) | 32 (18) |
| Employment status, n (%) | ||||
| Currently employed | 170 (29) | 185 (32) | 141 (38) | 39 (21) |
| BMI, n (%), kg/m2 | ||||
| Underweight (<18.4) | 8 (1) | 10 (2) | 5 (1) | 4 (2) |
| Normal (18.5–24.9) | 295 (51) | 213 (38) | 148 (41) | 49 (28) |
| Overweight (25–29.9) | 209 (36) | 228 (40) | 146 (40) | 77 (43) |
| Obese (30+) | 70 (12) | 115 (20) | 62 (17) | 48 (27) |
| SF-12, mean (s.d.) | ||||
| Physical component | 49.2 (10) | 43.0 (12.07) | 47.3 (10.06) | 34.40 (10.94) |
| Mental component | 53.3 (8) | 50.8 (10.79) | 52.0 (9.93) | 48.66 (12.18) |
| Other health problems, n (%) | ||||
| Yes | 350 (58) | 366 (60) | 210 (54) | 133 (69) |
| High blood pressure | 266 (44) | 283 (46) | 158 (41) | 104 (54) |
| Heart disease | 63 (10) | 79 (13) | 41 (11) | 31 (16) |
| Asthma | 54 (9) | 64 (11) | 37 (10) | 26 (14) |
| Diabetes | 53 (9) | 54 (9) | 33 (9) | 18 (9) |
| Otherb | 83 (14) | 96 (916) | 58 (16) | 30 (16) |
| Other body site pain, n (%) | ||||
| Yes | 418 (69) | 548 (90) | 340 (88) | 183 (94) |
| One other joint | 206 (34) | 143 (23) | 106 (28) | 30 (16) |
| Two other joints | 113 (19) | 145 (24) | 93 (24) | 42 (22) |
| Three or more other joints | 99 (16) | 259 (43) | 141 (37) | 110 (57) |
| WOMAC, mean (s.d.) | N/A | |||
| Pain (0–20) | 4.6 (4.16) | 2.8 (2.75) | 8.2 (4.17) | |
| Function (0–68) | 15.6 (15.10) | 9.0 (9.80) | 28.7 (15.36) | |
| Stiffness (0–8) | 2.3 (1.98) | 1.6 (1.45) | 3.9 (1.99) | |
| Chronicity of knee pain, n (%) | N/A | |||
| <3 months | 339 (58) | 275 (74) | 58 (30) | |
| ≥3 months | 241 (42) | 97 (26) | 136 (70) | |
| GP consultation in last year for knee problem, n (%) | N/A | |||
| Yes | 152 (26) | 50 (13) | 98 (51) | |
| Other health care for knee, n (%) | N/A | |||
| Yes | 211 (35) | 83 (22) | 121 (63) | |
| Prescription medication | 135 (22) | 44 (11) | 85 (44) | |
| Physiotherapist | 75 (12) | 33 (9) | 41 (21) | |
| Hospital specialist | 50 (8) | 16 (4) | 34 (18) | |
| Otherc | 95 (16) | 35 (7) | 57 (31) | |
Individual items may not add to totals due to missing data. aDefined as completing full-time education after leaving school. bIncludes stroke, cancer, Parkinson’s disease and chronic bronchitis/emphysema. cIncludes occupational therapist, acupuncturist, osteopath/chiropractor, knee operation and knee injection. SF-12: 12-item Short Form Health Survey [16]; GP: general practitioner; CPG: Chronic Pain Grade.
Exercise and physical activity behaviour
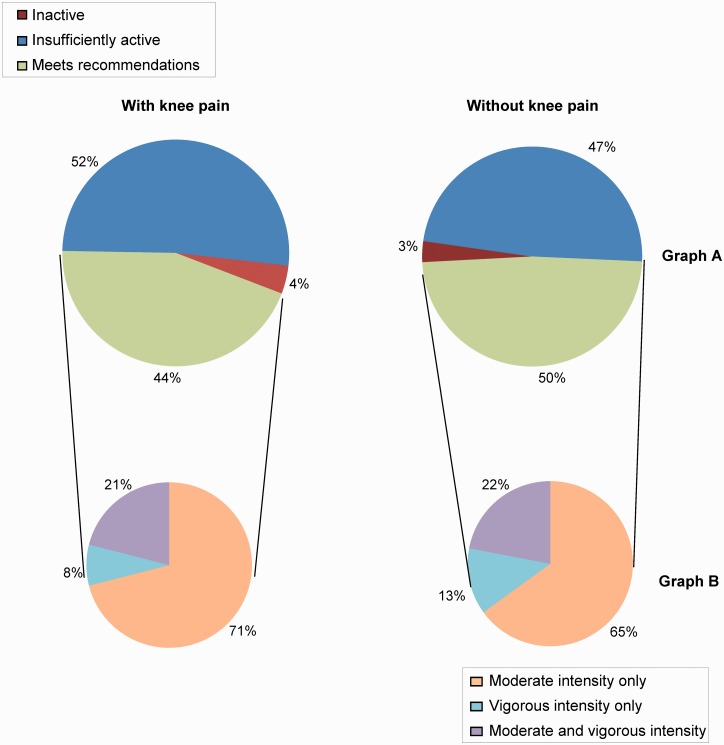
Overall, levels of physical activity were low. As summarized in Fig. 1, only 44% of individuals with knee pain met the physical activity recommendations [2], 52% were insufficiently active to meet these recommendations and 4% were classed as inactive. Of those who were sufficiently active to meet the recommendations, the majority did so through completing moderate-intensity activity (71%). Only 29% achieved the recommended levels of vigorous activity. In fact, out of the whole sample with knee pain, 64% reported that they never or only occasionally (1–3 times/mo) completed vigorous activity for at least 20 min duration.
Fig. 1.
Physical activity patterns in older adults with and without knee pain
(A) Percentage of responders who were inactive or sufficiently active or not to meet the 2007 American College of Sports Medicine physical activity recommendations [2]. (B) Of those who were sufficiently active, percentage of responders who met the 2007 ACSM physical activity recommendations by completing moderate activities, vigorous activities or both [2].
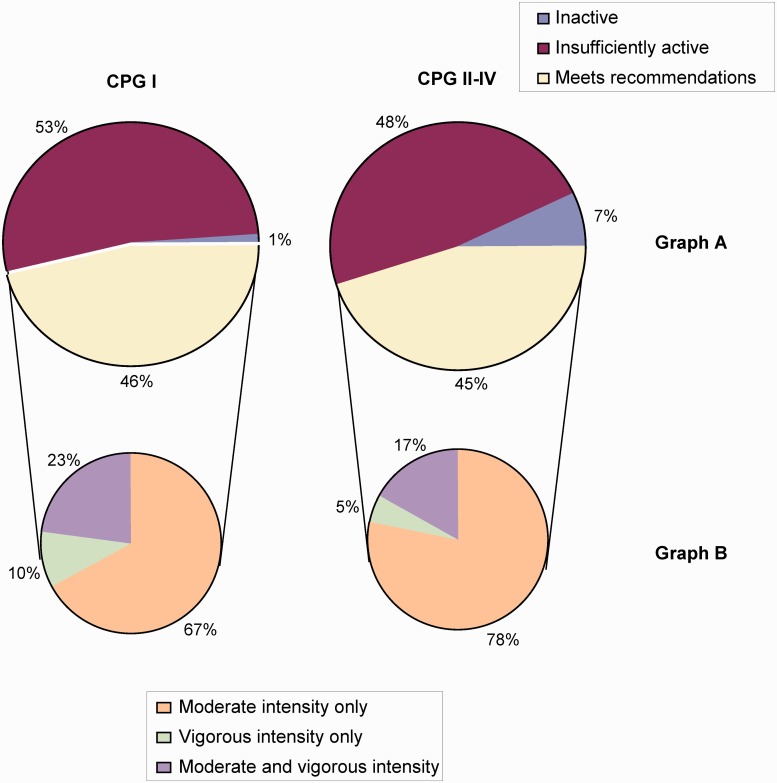
As shown in Fig. 1, a higher proportion of individuals without knee pain met the physical activity recommendations than those with knee pain, but this difference was not statistically significant (44% vs 50%, P = 0.06). There was also no significant difference in the proportion of individuals meeting the physical activity recommendations between those with differing severities of knee pain (CPG I vs CPG II–IV, 46% vs 45%, P = 1.0; see Fig. 2). Although more individuals without knee pain than those with knee pain and more individuals in CPG I than in CPG II–IV met the recommendations for vigorous activity, these differences were not statistically significant (35% vs 29%, P = 0.21 and 33% vs 22%, P = 0.15, respectively).
Fig. 2.
Physical activity patterns of individuals within CPG I and CPG II–IV
(A) Percentage of responders who were inactive or sufficiently active or not to meet the 2007 ACSM physical activity recommendations [2]. (B) Of those who were sufficiently active, the percentage of responders who met the 2007 ACSM physical activity recommendations by completing moderate activities, vigorous activities or both [2]. ACSM: American College of Sports Medicine; CPG: Chronic Pain Grade.
Interview findings
Response
From individuals reporting knee pain, 67 people were invited to participate in the semi-structured interviews and 22 individuals agreed to take part and were interviewed. One interview was excluded from the analysis because the participant became upset during the interview and it was stopped. In line with the purposive sampling strategy, interviewees had a range of different personal characteristics, including age, gender and level of physical activity, summarized in Tables 3 and 4.
Table 3.
Characteristics of the interview sample
| Subject no. | Age, years | Gender | CPG (I–IV) | Meets current physical activity recommendation |
|---|---|---|---|---|
| 208 | 76 | F | I | Y |
| 304 | 76 | M | I | Y |
| 402 | 66 | F | IV | N |
| 413 | 66 | M | Missing | N |
| 442 | 51 | M | I | Y |
| 459 | 76 | M | IV | Y |
| 511 | 54 | F | I | Y |
| 534 | 57 | F | I | N |
| 537 | 53 | M | II | Y |
| 736 | 77 | F | I | N |
| 779 | 65 | M | IV | N |
| 866 | 61 | F | I | Y |
| 911 | 56 | M | II | N |
| 930 | 69 | F | I | Y |
| 956 | 59 | M | III | Missing |
| 983 | 64 | F | IV | Y |
| 993 | 80 | M | II | Missing |
| 998 | 69 | F | I | Y |
| 1115 | 73 | F | II | Missing |
| 1178 | 79 | M | I | N |
| 1179 | 50 | F | I | Y |
Grade I: low disability–low intensity; grade II: low disability–high intensity; grade III: high disability–moderately limiting; grade IV: high disability–severely limiting [10]. The physical activity recommendations at the time of the survey recommended a minimum of 30 min of moderate-intensity aerobic exercise on ≥5 days/week or 20 min of vigorous aerobic exercise at least 3 days/week [2]. CPG: Chronic Pain Grade; F: female; M: male; Y: yes; N: no.
Table 4.
Characteristics of the survey and interview samples
| Characteristic | Survey sample (n = 611) | Interview participants (n = 21) |
|---|---|---|
| Age (years), n (%) | ||
| 50–59 | 213 (35) | 7 (33) |
| 60–69 | 190 (31) | 7 (33) |
| 70–79 | 147 (24) | 6 (29) |
| ≥80 | 61 (10) | 1 (5) |
| Gender, n (%) | ||
| Female | 349 (57) | 11 (52) |
| Education status, n (%) | ||
| Higher educationa | 167 (29) | 4 (21) |
| Employment status, n (%) | ||
| Currently employed | 184 (31) | 5 (24) |
| BMI, n (%) | ||
| Underweight (<18.4) | 10 (2) | 0 |
| Normal (18.5–24.9) | 213 (38) | 8 (47) |
| Overweight (25–29.9) | 228 (40) | 5 (29) |
| Obese (≥30) | 115 (20) | 4 (24) |
| SF-12, mean (s.d.) | ||
| Physical component | 43.0 (12.07) | 47.2 (10.65) |
| Mental component | 50.8 (10.79) | 49.5 (14.53) |
| Physical activity levelb, n (%) | ||
| Meets recommendations | 256 (44) | 11 (61) |
| Insufficiently active | 298 (52) | 7 (39) |
| Physically inactive | 24 (4) | 0 |
| CPG, n (%) | ||
| Grade I (low disability–low intensity) | 386 (67) | 11 (55) |
| Grade II (low-disability–high intensity) | 107 (18) | 4 (20) |
| Grade III (high disability–moderately limiting) | 43 (7) | 1 (5) |
| Grade IV (high disability–severely limiting) | 44 (8) | 4 (20) |
| WOMAC, mean (s.d.) | ||
| Pain (0–20) | 4.6 (4.16) | 6.2 (5.03) |
| Function (0–68) | 15.6 (15.10) | 19.5 (16.76) |
| Stiffness (0–8) | 2.3 (1.98) | 3.1 (1.12) |
Individual items may not add to totals due to missing data. aDefined as completing full-time education after leaving school. bThe physical activity recommendations at the time of the survey recommended a minimum of 30 min of moderate-intensity aerobic exercise on ≥5 days/week or 20 min of vigorous aerobic exercise at least 3 days/week [2]. SF-12: 12-item Short Form Health Survey [16]; CPG: chronic pain grade [10].
Exercise and physical activity behaviour
The interviews provided greater insight into the exercise and physical activity experience of older adults with knee pain. The type of exercise or physical activity that individuals completed was wide ranging and was broadly grouped as therapeutic exercise (structured exercise completed specifically for the knee joint that focused primarily on local knee exercises) and lifestyle activity [making conscious choices about physical activity and exercise as part of day-to-day living (e.g. using the stairs rather than a lift) and completing structured exercise including leisure pursuits such as golf and swimming]. Many participants described walking as a simple and feasible way of exercising, including completing organized walks, walking with family or friends and walking for transportation. Individuals had clear preferences about the type of exercise that they completed and there were different reasons for these preferences. For example, participant 1178 disliked cycling due to previous negative experiences using a bike as a boy, whereas participant 304 favoured cycling over walking because he felt that walking jarred his knee, making his problem worse.
There was much variation in the amount of therapeutic and lifestyle activity completed, both between different individuals and for each individual over time. This ranged from swinging it [the knee] when sitting (participant 1115), breaking up periods of sitting with a short walk, completing organized activities such as aerobic classes and participating in competitive cycling (participant 442). On the whole, interviewees expressed a preference for completing moderate-intensity exercise and talked about completing gentle activities and pacing themselves. Individuals placed importance on listening to their own body and monitoring their symptoms to guide the amount and type of exercise that they completed. Any increase in symptoms, including pain or swelling, was interpreted as having overdone it, thus participants on the whole completed exercise within the limits of their pain. Perhaps unsurprisingly, individuals’ previous exercise experiences guided their behaviour. If a previous activity was painful and resulted in a significant increase in symptoms, that activity may then be avoided altogether. However, in some cases individuals appeared to modify their activity patterns in order to remain as active as possible. This could include changing the type of exercise completed, e.g. changing from walking to cycling, reducing the intensity of exercise or breaking up periods of activity with rest.
As with the type of exercise completed, individuals expressed clear preferences with regard to the exercise setting. Some preferred to exercise at home, while others preferred exercising with others, either within a structured exercise group or less formally, e.g. with family or friends. Individuals who engaged in exercise with others highlighted many benefits: it was an enjoyable social experience, it was a motivator to continue to exercise and to work harder during the exercise session and it helped individuals to cope better with their knee problem.
Discussion
This study provides a description of the current patterns of exercise and physical activity behaviour among a sample of older adults with knee pain in the UK and provides insight into the experience of exercising in the presence of such pain. Overall the response rate to the survey was considered acceptable [23]. Individuals with knee pain were more likely to report pain in other body regions and be overweight or obese than those without knee pain. In addition, 60% had other co-morbidities, most commonly high blood pressure, heart disease, asthma and diabetes. This overall picture of older adults with multisite joint pain and multiple health problems highlights the importance of prescribing not only a local knee strengthening programme for patients with knee pain, but also a physical activity programme in line with current guideline recommendations [2, 3], which could also benefit these multiple health problems.
Exercise and physical activity
Amount
There were relatively low levels of physical activity among older adults, including those with knee pain, with only 4 in 10 being sufficiently active to meet the physical activity recommendations [2]. While only 4% of the sample with knee pain were categorized as inactive, suggesting that this group participates in some exercise and physical activity, they were not sufficiently active to achieve optimal benefits in terms of both their knee problem [24] and their wider general health [2]. The overall low levels of physical activity in those with and without knee pain and in individuals with differing severity of knee pain reinforces the importance of prescribing exercise and physical activity for adults who have consulted about their knee pain. However, broader population-based approaches to increasing physical activity among older adults in general are also likely to be important [25].
Despite individuals with knee pain having more pain in other body regions than individuals without knee pain, there was no statistically significant difference in the proportion of those with and without knee pain who were meeting current physical activity recommendations or between individuals with differing severities of knee problem. This could simply be a reflection of the low levels of physical activity in older adults in general, and larger samples may be needed to detect differences in physical activity between groups. Alternatively, the findings may suggest that individuals with joint problems find ways to remain as active as their peers despite their pain. The interviews highlighted that individuals self-monitored their symptoms in response to exercise and physical activity. Although this led to activity avoidance for some, for others levels of physical activity were not necessarily reduced in response to pain, rather activity was modified in some way, for example, by reducing its intensity, completing shorter bouts of physical activity or altering the type of activity completed. Overall, individuals with and without knee pain and those with more or less severe knee problems may have similar levels of physical activity (which are on average low), but there may be subtle differences in how that exercise and physical activity is completed. The survey supports this hypothesis to some extent, given the trend that more individuals with knee pain compared with those with no knee pain and more individuals in CPG II–IV than in CPG I met the physical activity recommendations by completing moderate activity only.
Intensity of exercise and physical activity
The survey and interviews highlighted that moderate-intensity or gentle activity was favoured over more vigorous exercise due in part to individuals listening to their own body and preferring to exercise in pain-free ways. As there is some evidence to suggest that there is no difference in pain reduction as a result of moderate and vigorous exercise in older adults with knee pain [26], it may be more appropriate to focus exercise prescription on moderate-intensity activities, as it appears that this kind of activity is more acceptable and thus more likely to be continued over the long term.
Exercise type and setting
The interviews revealed that individuals had clear preferences about the type and setting of exercise and physical activity that they completed. As the type of exercise does not appear to directly influence exercise adherence [27], and given the known benefits of both group and individualized exercise [28], it would seem sensible to try and tap into individual preferences when recommending an exercise programme for older adults with knee pain.
Comparison with other research
In line with the findings of this investigation, other quantitative studies also highlight that overall levels of physical activity completed by older adults with knee problems can be low [5], although estimates vary greatly [5, 29, 30]. Although this study showed that more people without knee pain were meeting physical activity recommendations than those with knee pain, this was not a significantly significant difference, which contrasts with the findings of other studies [31–33]. This could be due to differences in study methodology, including the specific groups sampled and the measures of physical activity used.
The qualitative findings within this study, that older adults with knee pain complete a wide range of activities, prefer moderate intensity exercise and make deliberate choices about exercise dependent on their knee symptom response, are supported by Der Ananian et al. [34]. They found that adults with arthritis completed a wide range of gentle activities, a choice informed by what they believed was safe or appropriate for arthritis.
Strengths and limitations
The key strength of this study is the mixed methods approach adopted: using the interviews to expand upon the survey findings has added richness and depth of understanding that would not have been achieved by survey data alone [8]. However, although the survey sample was randomly selected from a large general practice in Cheshire and the characteristics of the sample have been clearly described, this population as a whole may be different from other areas within the UK (e.g. this population has a lower ethnic mix than across England as a whole [35]), thus reducing the generalizability of findings. In addition, although the questionnaire response rate was considered acceptable, non-response bias may have been present. Finally, this study used a measure of physical activity that has not been developed or tested for use within a postal survey or within populations of older adults with knee pain specifically. It is therefore possible that the tool was not accurately capturing levels of exercise and physical activity within our study.
Clinical and research implications
This study has shown that levels of physical activity among older adults with knee pain are low, reinforcing the key message within current guideline recommendations for knee OA [1] that exercise and physical activity should be a core treatment for this group. However, it has also shown that due to individual differences in exercise and physical activity behaviour, these core treatment recommendations might be challenging to implement in a way that promotes long-term exercise behaviour change. Innovative interventions that can be adapted to suit different individual’s needs and preferences are required. In addition, exercise programmes and physical activity opportunities that target those with less severe knee problems, who are not consulting in primary care settings, and older adults in general are also needed.
Rheumatology key messages.
Physical activity among older adults is low, irrespective of the presence or severity of knee pain.
High levels of co-morbidity and obesity highlight the importance of prescribing general physical activity for older adults with knee pain.
Innovative physical activity interventions for older adults with knee pain are required that are adaptable to individual needs and preferences.
Acknowledgements
The authors would like to thank the administrative and health informatics staff at Arthritis Research UK Primary Care Centre and the doctors and staff at the participating practice for their help in planning and conducting the survey. For ongoing support throughout the study we would like to thank Dr Elaine Thomas, Professor Mike Doherty and Dr Edward Roddy. For independently analysing three interview transcripts and sharing her interpretation of these we would like to thank Dr Janet Grime. We would like to thank all the individuals that participated in the study. We would also like to thank two funding bodies for funding two members of the research team. Melanie Holden was funded by an Allied Health Professional Training Fellowship from Arthritis Research UK (grant reference 18004). Nadine Foster is supported by a Research Professorship from the National Institute of Health Research (NIHR; NIHR-RP-011-015). The views expressed in this manuscript are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health.
Funding: This work was supported by Arthritis Research UK, the Physiotherapy Research Foundation, the Chartered Society of Physiotherapy Charitable Trust and the NHS North Staffordshire Primary Care Research Consortium.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.National Collaborating Centre for Chronic Conditions. Osteoarthritis: National Clinical Guideline for Care and Management in Adults. London: Royal College of Physicians; 2014. [PubMed] [Google Scholar]
- 2.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendations from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 3.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 4.Scholes S, Mindell J. Physical Activity in Adults. Vol. 1, Chapter 2. Leeds, UK: Health and Social Care Information Centre; 2013. Health Survey for England 2012. [Google Scholar]
- 5.Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis Cartilage. 2013;21:1648–59. doi: 10.1016/j.joca.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Holden MA, Nicholls EE, Young J, Hay EM, Foster NE. The role of exercise for knee pain: what do older adults in the community think? Arthritis Care Res. 2012;64:1554–64. doi: 10.1002/acr.21700. [DOI] [PubMed] [Google Scholar]
- 7.Dekker J. Osteoarthritis: promoting exercise for OA in ambivalent older adults. Nat Rev Rheumatol. 2012;8:442–4. doi: 10.1038/nrrheum.2012.107. [DOI] [PubMed] [Google Scholar]
- 8.Creswell JW. Research Design: Qualitative, Quantitative and Mixed Methods Approaches. London: SAGE Publications; 2003. [Google Scholar]
- 9.Jinks C, Jordan KM, Ong BN, Croft P. A brief screening tool for knee pain in primary care (KNEST): results from a survey in the general population aged 50 and over. Rheumatology. 2004;43:55–61. doi: 10.1093/rheumatology/keg438. [DOI] [PubMed] [Google Scholar]
- 10.Von Korff M, Ormel J, Keele FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 11.Dunn KM, Croft PR, Main CJ, Von Korff M. A prognostic approach to defining chronic pain: replication in a UK primary care low back pain population. Pain. 2008;135:48–54. doi: 10.1016/j.pain.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Thomas E, Dunn KM, Mallen C, Peat G. A prognostic approach to defining chronic pain: application to knee pain in older adults. Pain. 2008;138:389–97. doi: 10.1016/j.pain.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 13.Von Korff M, Miglioretti DL. A prognostic approach to defining chronic pain. Pain. 2005;117:304–13. doi: 10.1016/j.pain.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Duncan R, Peat G, Thomas E, et al. Symptoms and radiographic osteoarthritis: not as discordant as they are made out to be? Ann Rheum Dis. 2007;66:86–91. doi: 10.1136/ard.2006.052548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peat G, Thomas E, Croft P. Staging joint pain and disability: a brief method using persistence and global severity. Arthritis Rheum. 2006;55:411–9. doi: 10.1002/art.21986. [DOI] [PubMed] [Google Scholar]
- 16.Ware JE, Kosinski, Keller SD. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–9. [PubMed] [Google Scholar]
- 18.Matthews CE, Ainsworth BE, Hanby C, et al. Development and testing of a short physical activity recall questionnaire. Med Sci Sports Exerc. 2005;37:986–94. [PubMed] [Google Scholar]
- 19.Smith RD, Healey EL, McHugh GA, Holden MA, Dziedzic KS. Measurement properties of self-reported physical activity instruments suitable for osteoarthritis (OA) or joint pain populations: a systematic review. Ann Rheum Dis. 2013;72(Suppl 3):700. [Google Scholar]
- 20.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York, USA: Aldine de Gruyter; 1967. [Google Scholar]
- 21.Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. London: SAGE Publications; 1998. [Google Scholar]
- 22.Sim J, Wright C. Research in Health Care: Concepts, Designs and Methods. Cheltenham: Stanley Thornes; 2000. [Google Scholar]
- 23.Mangione TW. Mail surveys. In: Bickman L, Rog DL, editors. Handbook of Applied Social Research Methods. Thousand Oaks, CA, USA: SAGE Publications; 1998. [Google Scholar]
- 24.Minor M, Stenstrom CH, Klepper SE, et al. Work group recommendations: 2002 Exercise and Physical Activity Conference, St. Louis, Missouri. Session V: evidence of benefit of exercise and physical activity in arthritis. Arthritis Care Res. 2003;49:453–4. doi: 10.1002/art.11125. [DOI] [PubMed] [Google Scholar]
- 25.Brady TJ, Sniezek JE. Implementing the national arthritis action plan: new population-based approaches to increasing physical activity among people with arthritis. Arthritis Care Res. 2003;49:471–6. doi: 10.1002/art.11052. [DOI] [PubMed] [Google Scholar]
- 26.Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66:622–36. doi: 10.1002/art.38290. [DOI] [PubMed] [Google Scholar]
- 27.Jordan JL, Holden MA, Mason EEJ, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010;1:CD005956. doi: 10.1002/14651858.CD005956.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hurley MV, Walsh NE, Mitchell HL, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: a cluster randomized trial. Arthritis Care Res. 2007;57:1211–9. doi: 10.1002/art.22995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Care Res. 2003;49:129–35. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 30.Manning VL, Hurley MV, Scott DL, Bearne LM. Are patients meeting the updated physical activity guidelines? Physical activity participation, recommendation, and preferences among inner-city adults with rheumatic diseases. J Clin Rheumatol. 2012;18:399–404. doi: 10.1097/RHU.0b013e3182779cb6. [DOI] [PubMed] [Google Scholar]
- 31.Farr JN, Going SB, Lohman TG, et al. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Care Res. 2008;59:1229–36. doi: 10.1002/art.24007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosemann T, Kuehlein T, Laux G, Szecsenyi J. Factors associated with physical activity of patients with osteoarthritis of the lower limb. J Eval Clin Pract. 2008;14:288–93. doi: 10.1111/j.1365-2753.2007.00852.x. [DOI] [PubMed] [Google Scholar]
- 33.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006;30:385–93. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Der Ananian CA, Wilcox S, Abbott J, et al. The exercise experience in adults with arthritis: a qualitative approach. Am J Health Behav. 2006;30:731–44. doi: 10.5555/ajhb.2006.30.6.731. [DOI] [PubMed] [Google Scholar]
- 35. Office for National Statistics. 2011 Census. http://www.neighbourhood.statistics.gov.uk/dissemination/ (18 July 2014, date last accessed)