Abstract
Background
Retention in care is important for all HIV-infected persons and is strongly associated with initiation of antiretroviral therapy and viral suppression. However, it is unclear how retention in care and age interact to effect viral suppression. We evaluated whether the association between retention and viral suppression differed by age at entry into care.
Methods
Cross-sectional analysis (2006-2010) involving 17,044 HIV-infected adults in 14 clinical cohorts across the U.S. and Canada. Patients contributed one year of data during their first full calendar year of clinical observation. Poisson regression examined associations between retention measures [U.S. National HIV/AIDS Strategy (NHAS), U.S. Department of Health and Human Services (DHHS), 6-month gap, and 3-month visit constancy] and viral suppression (HIV RNA ≤200 copies/mL) by age group: 18-29, 30-39, 40–49, 50–59, and ≥60 years old.
Results
Overall, 89% of patients were retained in care using the NHAS measure, 74% with the DHHS indicator, 85% did not have a 6-month gap, and 62% had visits in 3-4 quarters of the year; 54% achieved viral suppression. For each retention measure, the association with viral suppression was significant for only the younger age groups (18-29 and 30-39 years): 18-29 [adjusted prevalence ratio (APR)=1.33, 95% confidence interval (CI)=1.03-1.70]; 30-39 (APR=1.23, CI=1.01-1.49); 40-49 (APR=1.06, CI=0.90-1.22); 50-59 (APR=0.92, CI=0.75-1.13); ≥60 years (APR=0.99, CI=0.63-1.56) using the NHAS measure as a representative example.
Conclusions
These results have important implications for improving viral control among younger adults, emphasizing the crucial role retention in care plays in supporting viral suppression in this population.
Keywords: Retention in Care, Viral Suppression, Age, Engagement, HIV
Introduction
HIV-infected persons must complete several steps along a care continuum – HIV testing and diagnosis, linkage to and retention in primary HIV care, and receipt and adherence to antiretroviral therapy (ART) – to optimize individual and public health outcomes.1,2 Retention in care is a key step in this process, associated with initiation of ART, decreased mortality, and reduced HIV transmission to others.3-12
Multiple surveillance and cohort studies indicate that both patients’ age and retention in care status may impact HIV viral suppression.13-22 Among 35,433 HIV-infected adults followed at 18 primary and specialty care clinics in the United States (U.S.) between 2006 and 2011, older individuals and those retained in care were more likely to achieve viral suppression than younger persons and those poorly engaged in care, respectively.15 Similarly, of 338,959 persons living with HIV in 19 U.S. jurisdictions in 2010, older age and retention in care were both significantly associated with viral suppression.19
However, it is unclear how retention in care and age interact to effect viral suppression. Retention in care may enhance medication adherence in younger adults, who are reported to have lower rates of ART compliance compared to older populations.23-26 Alternatively, consistent engagement in care may support ART adherence in older individuals by minimizing drug-drug interactions and treating comorbid conditions.27,28 Gaining a better understanding of the relationships between retention in care, age, and viral suppression may assist in designing interventions to improve HIV care and outcomes. We used data from a multisite cohort collaboration to evaluate whether the association between retention in care and viral suppression varied by age at entry into care.
Methods
Study Design and Population
We conducted a cross-sectional analysis from 2006-2010 using data from the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), a multisite collaboration of cohort studies of HIV-infected adults (age ≥18 years) receiving care in the U.S. and Canada. NA-ACCORD is one of the multinational cohort studies sponsored by the International Epidemiological Databases to Evaluate AIDS consortium of the National Institutes of Health. Details on the NA-ACCORD collaboration have been published previously.29 Briefly, contributing cohorts have standardized cohort-specific methods of data collection. At scheduled intervals, investigators at these cohorts submit data regarding participants’ demographic characteristics, ART prescription information, dates and results of laboratory tests including HIV-1 RNA and CD4 count, clinical diagnoses, and vital status. These data are transferred securely to the NA-ACCORD central Data Management Core, where they undergo quality control for completeness and accuracy before they are combined into harmonized data files. The activities of the NA-ACCORD have been reviewed and approved by the local institutional review boards for each site and at Johns Hopkins School of Medicine.
Data from 14 NA-ACCORD clinical cohorts, with participants residing in all 50 U.S. states, the District of Columbia, Puerto Rico, and 10 Canadian provinces and territories, were included in analyses. HIV-infected adults (age ≥18 years) newly enrolled in care at these NA-ACCORD sites (i.e. first visit to these sites) between January 1, 2006 and December 31, 2010 were eligible for inclusion.30 To assure exclusion of those who may have received care previously (e.g. transferring care from a clinic outside the NA-ACCORD to an NA-ACCORD site), we excluded patients with first recorded HIV-1 RNA ≤ 200 copies/mL and individuals with ART use prior to NA-ACCORD enrollment. Interval cohort studies that participate in NA-ACCORD were excluded from this analysis because of our focus on the nature of HIV care in the U.S. and Canada.31
Retention Measures
Since multiple measures of retention in care are currently in use, with no clear gold standard,13,32 we applied four commonly used measures of retention for each patient in their first full calendar year of observation (subsequent to their year of entry at an NA-ACCORD site) to describe their pattern of attendance at primary HIV care visits. For some patients this also represented their first full calendar year after initial HIV diagnosis. The use of the first full calendar year reflects the common practice of measuring retention in care on a calendar year basis.32
First, the U.S. National HIV/AIDS Strategy (NHAS) retention in care measure dichotomously defines retention as having 2 or more HIV visits separated by ≥ 90 days during a calendar year.33 Second, the U.S. Department of Health and Human Services (DHHS) retention in HIV care indicator defines retention as having ≥ 1 HIV visits in each half of the calendar year (Jan-Jun and Jul-Dec), at least 60 days apart.34 Third, the 6- month gap in care measure reflects whether a patient had ≥ 6 months between sequential outpatient visits, with no gap signifying retention in care. Fourth, 3-month visit constancy, an ordinal measure, is the number of 3-month intervals in a calendar year in which a patient completes at least 1 HIV visit (range, 1-4). For all four measures evaluated in this study, HIV visits refer only to completed primary HIV care appointments at NA-ACCORD clinics and do not include nursing, pharmacy, laboratory, social services, or other types of visits.
Each retention measure has its particular advantages and limitations.13,32,35 Constancy measures, such as the NHAS measure, DHHS indicator, 3-month visit constancy measure, and the 6-month gap in care measure, do not require scheduled and missed visit data to be calculated; data elements which are not always readily available. The NHAS measure and DHHS indicator are unique in that several federal programs utilize them to monitor HIV outcomes. However, they may overestimate retention for patients needing more frequent visits. Conversely, the 3-month visit constancy measure is at risk of underestimating retention for patients needing less frequent monitoring. The 6-month gap in care measure is able to capture long breaks between visits, but may be difficult to calculate when there is no recently attended visit. Multiple studies have compared different measures of retention in care, demonstrating moderate to strong correlation between measures and modest discrimination for viral suppression.13,15,32,36
Outcome Variable
HIV viral suppression was the outcome of interest, defined by the U.S. Health Resources and Services Administration (HRSA) HIV/AIDS Bureau HIV viral load suppression performance measure.37 Persons were categorized as suppressed (HIV-1 RNA ≤ 200 copies/mL) and not suppressed (HIV-1 RNA > 200 copies/mL) using the last HIV-1 RNA value reported in the calendar year. Those with missing HIV-1 RNA values (10% of the sample) were excluded from regression analyses; sensitivity analyses were conducted classifying these individuals as “not suppressed.”38
Sociodemographic and Clinical Variables
Patients’ age as of January 1 of the calendar year was divided into five groups: 18-29, 30-39, 40–49, 50–59, and ≥ 60 years old. Race/ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and other/unknown. HIV transmission risk factor was grouped into men who had sex with men (MSM), heterosexual transmission (HET), injection drug use (IDU), and other/unknown. Patients who had IDU in combination with another risk factor (e.g. MSM, HET) were classified as IDU. Patients were considered to be on ART if they concomitantly were prescribed ≥ 3 antiretroviral drugs from at least 2 classes or triple nucleoside/nucleotide reverse transcriptase inhibitor regimen containing abacavir or tenofovir for at least 6 months during the calendar year. First CD4 count recorded in the calendar year was grouped as < 350, 350-499, or ≥ 500 cells/mm3.
Statistical Analyses
Standard descriptive analyses of demographic and clinical characteristics of the sample were conducted. Chi-squared tests for differences in proportion were used to detect unadjusted differences in viral suppression status by age group, within retention strata. Multivariable Poisson regression models with robust variance were used to estimate adjusted prevalence ratios (APR) and 95% confidence intervals of the association between each measure of retention and viral suppression, adjusting for age group, gender, race/ethnicity, HIV transmission risk factor, use of ART, first CD4 count, calendar year, and cohort. Covariates were selected a priori based on a literature review of factors influencing retention in care and viral suppression.13-18 Insurance status was not uniformly collected by NA-ACCORD cohorts and thus was not included in analyses. Separate models were estimated for each retention measure. To evaluate whether the association between retention in care and viral suppression differs by age group, we included an interaction term between age group and each measure of retention; an adjusted Wald test was used to determine if there was statistical evidence of interaction. Statistical analyses were performed using Stata 12.1 (Stata Corporation, College Station, TX).
Results
A total of 17,044 adults who met study criteria initiated care at NA-ACCORD clinical sites between 2006 and 2010. (Table 1) The majority of the patients were <50 years old (15% of patients were 18-29 years, 25% were 30-39 years, 34% were 40-49 years), male (81%), and of minority race/ethnicity (56%). The predominant HIV risk factor was MSM (40%) followed by HET (27%) and IDU (11%). Overall, 89% of patients were retained in care according to the NHAS measure, 74% according to the DHHS indicator, 85% did not have a 6-month gap, and 62% had visits in 3-4 quarters of the year. Fifty-five percent of the sample was prescribed ART in their first full calendar year of observation. Among those with available viral load data (n=15,378 or 90% of the 17,044 who initiated care), 54% achieved viral suppression.
Table 1.
Demographic and Clinical Characteristics of the Sample
| Characteristic | Overall N=17,044 (%) |
|---|---|
| Age (years) | |
| 18-29 | 2,560 (15%) |
| 30-39 | 4,261 (25%) |
| 40-49 | 5,826 (34%) |
| 50-59 | 3,259 (19%) |
| ≥ 60 | 1,138 (7%) |
| Sex | |
| Male | 13,764 (81%) |
| Female | 3,289 (19%) |
| Race/Ethnicity | |
| White | 6,244 (37%) |
| Black | 7,101(42%) |
| Hispanic | 2,143 (13%) |
| Unknown | 1,364 (8%) |
| HIV Risk Factor | |
| MSM | 6,789 (40%) |
| Heterosexual | 4,591 (27%) |
| IDU | 1,850 (11%) |
| Unknown | 3,409 (22%) |
| First CD4 Count in Year | |
| < 350 cell/mm3 | 7,511 (44%) |
| 350-499 cell/mm3 | 3,669 (22%) |
| ≥500 cell/mm3 | 4,321 (25%) |
| Missing | 1,534 (9%) |
| Use of ART in Year | |
| No | 7,590 (45%) |
| Yes | 9,454 (55%) |
| Calendar Year | |
| 2006 | 3,719 (22%) |
| 2007 | 3,510 (21%) |
| 2008 | 3,611 (21%) |
| 2009 | 3,346 (20%) |
| 2010 | 2,858 (16%) |
| NHAS Retention Measure | |
| Not Retained | 1,846 (11%) |
| Retained | 15,198 (89%) |
| DHHS Retention Indicator | |
| Not Retained | 4,473 (26%) |
| Retained | 12,571 (74%) |
| 6-Month Gap | |
| Yes (Not Retained) | 2,563 (15%) |
| No (Retained) | 14,481 (85%) |
| 3-Month Visit Constancy | |
| 1 | 2,901 (17%) |
| 2 | 3,586 (21%) |
| 3 | 4,806 (28%) |
| 4 | 5,751 (34%) |
| Viral Suppression | |
| No | 7,119 (42%) |
| Yes | 8,259 (48%) |
| Missing | 1,666 (10%) |
Abbreviations: ART, antiretroviral therapy; DHHS, Department of Health and Human Services; HET, heterosexual transmission; HIV, human immunodeficiency virus; IDU, injection drug use; MSM, men who have sex with men; NHAS, National HIV/AIDS Strategy.
Figure 1 shows the unadjusted proportions of patients with viral suppression, by age group and retention measure. For each measure, three significant (p <0.05) results from chi-squared tests are clear: (1) the older the individual, the greater the probability of viral suppression in both the retained and not retained in care groups; (2) patients who were retained in care had a greater probability of viral suppression than those not retained in care, but this difference decreased as age groups increased; and (3) the association between retention in care and viral suppression was greatest for younger versus older age groups.
Figure1.
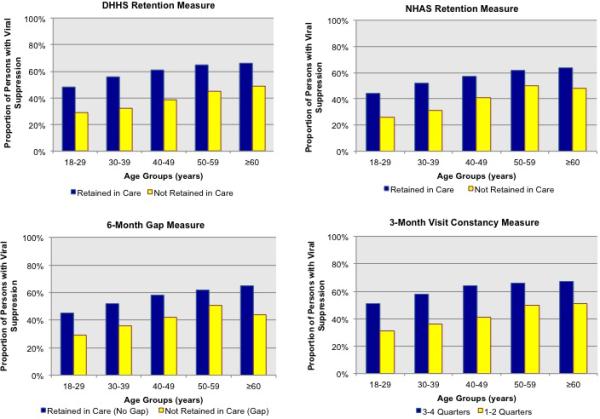
Unadjusted Proportion of HIV-Infected Persons with Viral Suppression by Retention Measure and Age Group
Table 2 shows APRs for the joint effect of retention in care on viral suppression at different age groups. For each retention measure, the association with viral suppression was significant (p <0.05) for only the younger age groups (18-29 years and 30-39 years): NHAS measure (APR=1.33 [1.03, 1.70] for 18-29; APR=1.23 [1.01, 1.49] for 30-39), DHHS indicator (APR=1.19 [1.02, 1.39] for 18-29; APR=1.23 [1.09, 1.39] for 30-39), 6-month gap in care measure (APR=1.28 [1.04,1.57] for 18-29; APR=1.16 [1.01, 1.35] for 30-39), and 3-month visit constancy (APR=1.36 [1.09, 1.69] for 3 quarters and APR=1.47 [1.18, 1.82] for 4 quarters for 18-29; APR=1.27 [1.07, 1.50] for 3 quarters and APR=1.41 [1.19, 1.66] for 4 quarters for 30-39). Pairwise comparisons of APR between the two youngest age groups were significant (p <0.05). We did not observe any significant differences in the probability of viral suppression for older individuals who were retained versus not retained in care. Sensitivity analyses categorizing those with missing viral load data as “not suppressed” yielded similar results. (Appendix Table 1)
Table 2.
Association between Retention in Care Measures and Viral Suppression by Age Group
| Retention Measure | Age Group |
||||
|---|---|---|---|---|---|
| 18-29 years APR (95% CI) | 30-39 years APR (95% CI) | 40-49 years APR (95% CI) | 50-59 years APR (95% CI) | ≥ 60 years APR (95% CI) | |
| NHAS Measure | |||||
| Not Retained | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] |
| Retained | 1.33 (1.03-1.70) | 1.23 (1.01-1.49) | 1.06 (0.90-1.22) | 0.92 (0.75-1.13) | 0.99 (0.63-1.56) |
| DHHS Indicator | |||||
| Not Retained | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] |
| Retained | 1.19 (1.02-1.39) | 1.23 (1.09-1.39) | 1.08 (0.97-1.19) | 0.99 (0.87-1.14) | 0.97 (0.75-1.25) |
| 6-Month Gap in Care | |||||
| Yes (Not Retained) | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] |
| No (Retained) | 1.28 (1.04-1.57) | 1.16 (1.01-1.35) | 1.12 (0.99-1.27) | 0.96 (0.81-1.14) | 1.09 (0.74-1.60) |
| 3-Month Visit Constancy | |||||
| 1 | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] | 1.00 [Ref] |
| 2 | 1.22 (0.97-1.55) | 1.16 (0.97-1.40) | 0.98 (0.85-1.14) | 1.02 (0.83-1.25) | 1.01 (0.67-1.52) |
| 3 | 1.36 (1.09-1.69) | 1.27 (1.07-1.50) | 1.12 (0.98-1.29) | 1.00 (0.83-1.20) | 0.95 (0.65-1.37) |
| 4 | 1.47 (1.18-1.82) | 1.41 (1.19-1.66) | 1.13 (0.99-1.29) | 1.03 (0.86-1.23) | 1.01 (0.71-1.45) |
Abbreviations: APR, adjusted prevalence ratio; CI, confidence interval; DHHS, Department of Health and Human Services; NHAS, National HIV/AIDS Strategy.
Models included an interaction between retention measure and age group, and adjusted for sex, race/ethnicity, HIV risk factor, first CD4 cell count in the year, use of ART for >6 months during the year, calendar year, and cohort as time-fixed covariates.
Bold signifies adjusted prevalence ratios with p-vale <0.05.
Appendix Tables 2 and 3 present associations between patient factors and viral suppression. In models adjusting for gender, race/ethnicity, HIV transmission risk factor, use of ART, first CD4 count, calendar year, cohort, and including a interaction term between age group and retention in care, persons with black race/ethnicity (vs. white) and HET risk or IDU risk (vs. MSM) were significantly (p <0.05) less likely to achieve viral suppression, regardless of the retention measure assessed. Persons on ART and those who entered care in more recent years were significantly (p <0.05) more likely to be virally suppressed.
Discussion
This study evaluate the relationship between age, retention in care, and viral suppression, and suggests that viral suppression is significantly more prevalent in younger HIV-infected adults (18-39 years old) retained in care than in similarly aged persons not retained in care. The U.S. Centers for Diseases Control and Prevention estimate that approximately 14,200 individuals aged 20-29 and 11,200 individuals aged 30-39 were newly infected with HIV in 2010, representing the highest burden of new HIV infections among all age groups.39 Retaining younger HIV-infected persons in care may be particularly important to improving clinical outcomes and reducing transmission of HIV in this population.40
While older patients were more likely to achieve viral suppression, we demonstrate that the effect of retention in care on viral suppression was greatest for patients aged 18-39 compared to those 40 years and older. This pattern persisted independent of the measure of retention utilized. Prior research indicates that younger adults have lower rates of ART adherence than older adults.23,24,26 Of 5,090 HIV-infected patients enrolled in a large integrated health care system, patients 50 years or older sustained higher therapy adherence (88.9%) than 18-39 (83.7%) and 40-49 years old (85.7%), respectively.26 Among 148 HIV-infected adults on ART and receiving care in Los Angeles, CA, adherence to HIV therapy was significantly higher in older (≥50 years old) versus younger (<50 years old) patients (87.5% versus 78.3%, respectively).24 Similarly, a recent systematic review and meta-analysis noted that older age reduced the risk of ART non-adherence by 27% (relative risk 0.72, [0.64, 0.82]).25 These studies suggest that differences in ART adherence between older and younger adults exist and may mediate the relationships with viral suppression. Unfortunately, ART adherence data was unavailable and thus was not included in our analyses. Regular clinic attendance may help younger adults comply with HIV treatment and achieve viral suppression by providing one-on-one ART education and counseling, tools to improve medication adherence (e.g. pillboxes, reminder devices), and access to case management and ancillary services to address competing food insecurity, housing, and transportation needs.41 These resources may be equally important to maintaining ART adherence in older adults.
HIV-related stigma, fear of disclosure, and stress significantly impact the experiences and health of people living with HIV.42-44 Some data suggest that younger individuals may confront these challenges at higher rates than older adults, while other report no difference between age groups.45-48 Among 147 HIV-infected adolescents and young adults aged 16-29 years living in New York, Los Angeles, and San Francisco, almost all (89%) reported perceived stigma (a stigmatized person's fear or anticipation of discrimination and rejection, and internal sense of shame) and 64% reported enacted stigma (actual experiences of stigma and discrimination) during their lifetime.49 In an analysis exploring the relationship between age and patterns of disclosure, younger adults were significantly more likely to fear losing their job because of their HIV status than older adults.45 Likewise, among 102 adults living with HIV in a large city, individuals ≤50 years old had more social isolation than those >50 years old.47 Maintaining a continuous relationship with a provider may offer younger adults access to resources to better manage HIV-related stigma and barriers to care, which may contribute to improved ART adherence and achievement of viral suppression. However, the availability and quality of these resources may differ by provider and clinic.
Our finding that the association between retention in care and viral suppression was strongest for younger patients does not preclude the possibility that there may be subgroups of older individuals for whom retention may be equally or more important to achieving viral control and other health outcomes. For example, continuous engagement in care may be key to managing comorbid conditions (e.g. diabetes, heart failure) in older people with HIV infection.50 Further studies examining these nuances may help in the development of more personalized measures of retention in care.
Our analysis has several limitations. First, our data do not reflect visits to multiple providers by the same patient. It is possible that patients may switch facilities or providers in the same locality, emigrate from the area, or become incarcerated, institutionalized, or hospitalized but still be receiving care. Younger adults may be more mobile than older adults, impacting engagement in care.51 Second, we measured use of ART and viral suppression, but did not specifically assess adherence to HIV treatment. Future studies are warranted to investigate the relationship between ART adherence, age, retention in care, and viral suppression. Third, we focused on the first full calendar year in primary HIV care to allow sufficient time to observe retention measures. Thus, patients who were linked to outpatient care with less than one year of follow-up were excluded; additional research to better understand persons who are unable to establish consistent care is warranted.2,52. Fourth, HIV-infected individuals are living longer,53 which requires new evaluations of longer-term retention in care and viral suppression. Similarly, as HIV therapy, national treatment guidelines, and telehealth continue to advance new standards and methods for assessing retention in care will be needed. Fifth, our cross-sectional study design precludes inference of causality. Sixth, we are limited by the current retention measures in use, which only include primary HIV care appointments and do not account for nursing, pharmacy, laboratory, or other types of visits. Exclusion of these points of contact with the healthcare system may underestimate retention in care. Lastly, while NA-ACCORD constitutes a patient population that is a large proportion of and demographically similar to persons living with HIV/AIDS in the U.S.,54 care sites vary in operations and support services provided, which may impact generalizability of our findings.
In summary, we reported that retention in care is more strongly associated with viral suppression in younger adults. These results have important implications for the test and treat approach to HIV prevention, emphasizing the crucial role retention in care plays in supporting viral suppression in younger adults.
Supplementary Material
Acknowledgement
We are grateful to all patients, physicians, investigators, and staff involved in the NA-ACCORD. This work was supported by grants U01-AI069918, U01-AA013566, U24-AA020794, U01-AA020790, U01-AI31834, U01-AI34989, U01-AI34993, U01-AI34994, U01-AI35004, U01-AI35039, U01-AI35040, U01-AI35041, U01-AI35042, U01-AI35043, U01-AI37613, U01-AI37984, U01-AI38855, U01-AI38858, U01-AI42590, U01-AI68634, U01-AI68636, U01-AI69432, U01-AI69434, U01-HD32632, U10-EY08057, U10-EY08052, U10- EY08067, UL1-RR024131, UL1-TR000083, U54- MD007587, F31-DA035713, G12- MD007583, K01-AI071754, K01-AI093197, K23-MH097647, K23 EY013707, K24-DA00432, MO1-RR-00052, N02-CP55504, P30-AI027763, P30-AI094189, P30-AI27757, P30-AI27767, P30-AI50410, P30-AI54999, P30-AI036219, P30-MH62246, R01-CA165937, R01-AA16893, R01-DA11602, R01-DA04334, R01-DA12568, R24-AI067039, R56-AI102622, Z01-CP010214, and Z01-CP010176 from the National Institutes of Health, USA; contract CDC200-2006-18797 from the Center's for Disease Control and Prevention, USA; contract 90047713 from the Agency for Healthcare Research and Quality, USA; contract 90051652 from the Health Resources and Services Administration, USA; grants TGF-96118, HCP-97105, CBR-86906, CBR-94036 from the Canadian Institutes of Health Research, Canada; Ontario Ministry of Health and Long Term Care; and the Government of Alberta, Canada.
Footnotes
Conflicts: None
NA-ACCORD Collaborating Cohorts and Representatives
* Indicates cohort data included in this analysis.
AIDS Link to the IntraVenous Experience: Gregory D. Kirk.
Adult AIDS Clinical Trials Group Longitudinal Linked Randomized Trials: Constance A. Benson, Ronald J. Bosch, and Ann C. Collier.
*Fenway Health HIV Cohort: Stephen Boswell, Chris Grasso, and Kenneth H. Mayer.
HAART Observational Medical Evaluation and Research: Robert S. Hogg, P. Richard Harrigan, Julio SG Montaner, Angela Cescon, and Hasina Samji.
*HIV Outpatient Study: John T. Brooks and Kate Buchacz.
*HIV Research Network: Kelly A. Gebo and Richard D. Moore.
*Johns Hopkins HIV Clinical Cohort: Richard D. Moore.
*John T. Carey Special Immunology Unit Patient Care and Research Database, Case Western Reserve University: Benigno Rodriguez.
Kaiser Permanente Mid-Atlantic States: Michael A. Horberg.
*Kaiser Permanente Northern California: Michael J. Silverberg.
Longitudinal Study of Ocular Complications of AIDS: Jennifer E. Thorne.
Multicenter Hemophilia Cohort Study–II: James J. Goedert.
Multicenter AIDS Cohort Study: Lisa P. Jacobson.
*Montreal Chest Institute Immunodeficiency Service Cohort: Marina B. Klein.
Ontario HIV Treatment Network Cohort Study: Sean B. Rourke, Ann N. Burchell, and Anita R. Rachlis.
Retrovirus Research Center, Bayamon Puerto Rico: Robert F. Hunter-Mellado and Angel M. Mayor.
*Southern Alberta Clinic Cohort: M. John Gill.
Studies of the Consequences of the Protease Inhibitor Era: Steven G. Deeks and Jeffrey N. Martin.
*University of Alabama at Birmingham 1917 Clinic Cohort: Michael S. Saag, Michael J. Mugavero, and James Willig.
*University of North Carolina at Chapel Hill HIV Clinic Cohort: Joseph J. Eron and Sonia Napravnik.
*University of Washington HIV Cohort: Mari M. Kitahata and Heidi M. Crane.
*Veterans Aging Cohort Study: Amy C. Justice, Robert Dubrow, and David Fiellin.
*Vanderbilt-Meharry Centers for AIDS Research Cohort: Timothy R. Sterling, David Haas, Sally Bebawy, and Megan Turner.
Women's Interagency HIV Study: Stephen J. Gange and Kathryn Anastos.
References
- 1.Vital signs: HIV prevention through care and treatment--United States. MMWR. Morb Mortal Wkly Rep. 2011 Dec 2;60(47):1618–1623. [PubMed] [Google Scholar]
- 2.Fleishman JA, Yehia BR, Moore RD, Korthuis PT, Gebo KA. Establishment, retention, and loss to follow-up in outpatient HIV care. J Acquir Immune Defic Syndr. 2012 Jul 1;60(3):249–259. doi: 10.1097/QAI.0b013e318258c696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mugavero MJ. Improving engagement in HIV care: what can we do? Top HIV Med. 2008 Dec;16(5):156–161. [PubMed] [Google Scholar]
- 4.Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV-infected patients in care: Where are we? Where do we go from here? Clin Infect Dis. 2010 Mar 1;50(5):752–761. doi: 10.1086/649933. [DOI] [PubMed] [Google Scholar]
- 5.Ulett KB, Willig JH, Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009 Jan;23(1):41–49. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berg MB, Safren SA, Mimiaga MJ, Grasso C, Boswell S, Mayer KH. Nonadherence to medical appointments is associated with increased plasma HIV RNA and decreased CD4 cell counts in a community-based HIV primary care clinic. AIDS Patient Care STDS. 2005 Oct;17(7):902–907. doi: 10.1080/09540120500101658. [DOI] [PubMed] [Google Scholar]
- 7.Giordano TP, White AC, Jr., Sajja P, et al. Factors associated with the use of highly active antiretroviral therapy in patients newly entering care in an urban clinic. J Acquir Immune Defic Syndr. 2003 Apr 1;32(4):399–405. doi: 10.1097/00126334-200304010-00009. [DOI] [PubMed] [Google Scholar]
- 8.Lucas GM, Chaisson RE, Moore RD. Highly active antiretroviral therapy in a large urban clinic: risk factors for virologic failure and adverse drug reactions. Ann Intern Med. 1999 Jul 20;131(2):81–87. doi: 10.7326/0003-4819-131-2-199907200-00002. [DOI] [PubMed] [Google Scholar]
- 9.Mugavero MJ, Lin HY, Willig JH, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009 Jan 15;48(2):248–256. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metsch LR, Pereyra M, Messinger S, et al. HIV transmission risk behaviors among HIV-infected persons who are successfully linked to care. Clin Infect Dis. 2008 Aug 15;47(4):577–584. doi: 10.1086/590153. [DOI] [PubMed] [Google Scholar]
- 11.Yehia BR, Kangovi S, Frank I. Patients in transition: avoiding detours on the road to HIV treatment success. AIDS. 2013 Feb 21; doi: 10.1097/QAD.0b013e328360104e. [DOI] [PubMed] [Google Scholar]
- 12.Yehia BR, Fleishman JA, Moore RD, Gebo KA. Retention in Care and Health Outcomes of Transgender Persons Living With HIV. Clin Infect Dis. 2013 May 30; doi: 10.1093/cid/cit363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mugavero MJ, Westfall AO, Zinski A, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012 Dec 15;61(5):574–580. doi: 10.1097/QAI.0b013e318273762f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tripathi A, Youmans E, Gibson JJ, Duffus WA. The impact of retention in early HIV medical care on viro-immunological parameters and survival: a statewide study. AIDS Res Hum Retroviruses. 2011 Jul;27(7):751–758. doi: 10.1089/AID.2010.0268. [DOI] [PubMed] [Google Scholar]
- 15.Yehia BR, French B, Fleishman JA, et al. Retention in Care is More Strongly Associated with Viral Suppression in HIV-Infected Patients with Lower versus Higher CD4 Counts. J Acquir Immune Defic Syndr. 2013 Oct 14; doi: 10.1097/QAI.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dombrowski JC, Kitahata MM, Van Rompaey SE, et al. High levels of antiretroviral use and viral suppression among persons in HIV care in the United States, 2010. J Acquir Immune Defic Syndr. 2013 Jul 1;63(3):299–306. doi: 10.1097/QAI.0b013e3182945bc7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanna DB, Buchacz K, Gebo KA, et al. Trends and disparities in antiretroviral therapy initiation and virologic suppression among newly treatment-eligible HIV-infected individuals in North America, 2001-2009. Clin Infect Dis. 2013 Apr;56(8):1174–1182. doi: 10.1093/cid/cit003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yehia BR, Fleishman JA, Metlay JP, Moore RD, Gebo KA. Sustained viral suppression in HIV-infected patients receiving antiretroviral therapy. JAMA. 2012 Jul 25;308(4):339–342. doi: 10.1001/jama.2012.5927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 U.S. jurisdictions. J Acquir Immune Defic Syndr. 2014 Sep 18; doi: 10.1097/QAI.0000000000000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robertson M, Laraque F, Mavronicolas H, Braunstein S, Torian L. Linkage and retention in care and the time to HIV viral suppression and viral rebound - New York City. AIDS. 2014 Sep 22;:1–8. doi: 10.1080/09540121.2014.959463. [DOI] [PubMed] [Google Scholar]
- 21.Hall HI, Tang T, Westfall AO, Mugavero MJ. HIV care visits and time to viral suppression, 19 U.S. jurisdictions, and implications for treatment, prevention and the national HIV/AIDS strategy. PloS One. 2013;8(12):e84318. doi: 10.1371/journal.pone.0084318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Torian LV, Xia Q, Wiewel EW. Retention in care and viral suppression among persons living with HIV/AIDS in New York City, 2006-2010. Am J Public Health. 2014 Sep;104(9):e24–29. doi: 10.2105/AJPH.2014.302080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barclay TR, Hinkin CH, Castellon SA, et al. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007 Jan;26(1):40–49. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hinkin CH, Hardy DJ, Mason KI, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS. 2004 Jan 1;18(Suppl 1):S19–25. doi: 10.1097/00002030-200418001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghidei L, Simone MJ, Salow MJ, et al. Aging, antiretrovirals, and adherence: a meta analysis of adherence among older HIV-infected individuals. Drugs and Aging. 2013 Oct;30(10):809–819. doi: 10.1007/s40266-013-0107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silverberg MJ, Leyden W, Horberg MA, DeLorenze GN, Klein D, Quesenberry CP., Jr Older age and the response to and tolerability of antiretroviral therapy. Arch Intern Med. 2007 Apr 9;167(7):684–691. doi: 10.1001/archinte.167.7.684. [DOI] [PubMed] [Google Scholar]
- 27.Holtzman C, Armon C, Tedaldi E, et al. Polypharmacy and risk of antiretroviral drug interactions among the aging HIV-infected population. J Gen Intern Med. 2013 Oct;28(10):1302–1310. doi: 10.1007/s11606-013-2449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greene M, Justice AC, Lampiris HW, Valcour V. Management of human immunodeficiency virus infection in advanced age. JAMA. 2013 Apr 3;309(13):1397–1405. doi: 10.1001/jama.2013.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gange SJ, Kitahata MM, Saag MS, et al. Cohort profile: the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD). Int J Epidemiol. 2007 Apr;36(2):294–301. doi: 10.1093/ije/dyl286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rebeiro P, Althoff KN, Buchacz K, et al. Retention among North American HIV-infected persons in clinical care, 2000-2008. J Acquir Immune Defic Syndr. 2013 Mar 1;62(3):356–362. doi: 10.1097/QAI.0b013e31827f578a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lau B, Gange SJ, Moore RD. Interval and clinical cohort studies: epidemiological issues. AIDS Res Hum Retroviruses. 2007 Jun;23(6):769–776. doi: 10.1089/aid.2006.0171. [DOI] [PubMed] [Google Scholar]
- 32.Yehia BR, Fleishman JA, Metlay JP, et al. Comparing different measures of retention in outpatient HIV care. AIDS. 2012 Jun 1;26(9):1131–1139. doi: 10.1097/QAD.0b013e3283528afa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White House Office of National HIV/AIDS Policy The National HIV/AIDS Strategy of the United States. 2010 [Google Scholar]
- 34.Forsyth AYV. Office of HIV/AIDS and Infectious Disease Policy. US Department of Health and Human Services; 2012. [January 5, 2014]. Secretary Sebelius approves indicators for monitoring HHS-funded HIV services. http://blog.aids.gov/2012/08/secretary-sebelius-approves-indicators-for-monitoring-hhs-funded-hiv-services.html. [Google Scholar]
- 35.Giordano TP. [September 29, 2014];How Should We Measure Retention in HIV Care? 2012 http://www.medscape.com/viewarticle/768913.
- 36.Crawford TN, Sanderson WT, Thornton A. A comparison study of methods for measuring retention in HIV medical care. AIDS Behav. 2013 Nov;17(9):3145–3151. doi: 10.1007/s10461-013-0559-0. [DOI] [PubMed] [Google Scholar]
- 37.Health Resources and Services Administration HIV/AIDS Bureau Performance Measures. 2013 http://hab.hrsa.gov/deliverhivaidscare/coremeasures.pdf.
- 38.Mugavero MJ, Westfall AO, Zinski A, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012 Dec 15;61(5):574–580. doi: 10.1097/QAI.0b013e318273762f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012;17:4. [Google Scholar]
- 40.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care. 2014 Mar;28(3):128–135. doi: 10.1089/apc.2013.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Medicine. 2012 Jun 5;156(11):817–833. W-284, W-285, W-286, W-287, W-288, W-289, W-290, W-291, W-292, W-293, W-294. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003 Feb;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 43.Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006 Sep;10(5):473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Emlet CA. A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care STDS. 2006 May;20(5):350–358. doi: 10.1089/apc.2006.20.350. [DOI] [PubMed] [Google Scholar]
- 46.Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS. 2009 May;23(5):371–376. doi: 10.1089/apc.2008.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Webel AR, Longenecker CT, Gripshover B, Hanson JE, Schmotzer BJ, Salata RA. Age, stress, and isolation in older adults living with HIV. AIDS. 2013 Oct 14; doi: 10.1080/09540121.2013.845288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grov C, Golub SA, Parsons JT, Brennan M, Karpiak SE. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS. 2010 May;22(5):630–639. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Swendeman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV-related stigma among young people living with HIV. Health Psychol. 2006 Jul;25(4):501–509. doi: 10.1037/0278-6133.25.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crawford TN, Sanderson WT, Breheny P, Fleming ST, Thornton A. Impact of non-HIV related comorbidities on retention in HIV medical care: does retention improve over time? AIDS Behav. 2014 Mar;18(3):617–624. doi: 10.1007/s10461-013-0524-y. [DOI] [PubMed] [Google Scholar]
- 51.Yehia BR, Schranz AJ, Momplaisir F, et al. Outcomes of HIV-Infected Patients Receiving Care at Multiple Clinics. AIDS Behav. 2013 Sep 28; doi: 10.1007/s10461-013-0625-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giordano TP, Visnegarwala F, White AC, Jr., et al. Patients referred to an urban HIV clinic frequently fail to establish care: factors predicting failure. AIDS. 2005 Aug;17(6):773–783. doi: 10.1080/09540120412331336652. [DOI] [PubMed] [Google Scholar]
- 53.Samji H, Cescon A, Hogg RS, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PloS one. 2013;8(12):e81355. doi: 10.1371/journal.pone.0081355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ford MA, Spicer CM. Monitoring HIV care in the United States : indicators and data systems. National Academies Press; Washington, D.C.: 2012. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


