Abstract
Purpose
To test the efficacy of meaning-centered group psychotherapy (MCGP) to reduce psychological distress and improve spiritual well-being in patients with advanced or terminal cancer.
Patients and Methods
Patients with advanced cancer (N = 253) were randomly assigned to manualized eight-session interventions of either MCGP or supportive group psychotherapy (SGP). Patients were assessed before and after completing the treatment and 2 months after treatment. The primary outcome measures were spiritual well-being and overall quality of life, with secondary outcome measures assessing depression, hopelessness, desire for hastened death, anxiety, and physical symptom distress.
Results
Hierarchical linear models that included a priori covariates and only participants who attended ≥ three sessions indicated a significant group × time interaction for most outcome variables. Specifically, patients receiving MCGP showed significantly greater improvement in spiritual well-being and quality of life and significantly greater reductions in depression, hopelessness, desire for hastened death, and physical symptom distress compared with those receiving SGP. No group differences were observed for changes in anxiety. Analyses that included all patients, regardless of whether they attended any treatment sessions (ie, intent-to-treat analyses), and no covariates still showed significant treatment effects (ie, greater benefit for patients receiving MCGP v SGP) for quality of life, depression, and hopelessness but not for other outcome variables.
Conclusion
This large randomized controlled study provides strong support for the efficacy of MCGP as a treatment for psychological and existential or spiritual distress in patients with advanced cancer.
INTRODUCTION
Coping with advanced cancer can cause serious psychological distress in even the most resilient individuals. Distress can manifest in many ways, ranging from depression and hopelessness to a loss of spiritual well-being, existential distress, and even desire for hastened death. The assessment and treatment of psychological disorders (eg, depression, anxiety) are widely recognized as critical components of care in oncology and palliative care settings; however, few interventions specifically target the loss of spiritual well-being and existential distress that that often accompany advanced cancer. Several psychotherapeutic interventions have focused on patients with advanced or terminal illness, but these studies have often generated modest results (eg, small treatment effects, inconsistent findings across outcome variables) and have typically relied on small samples (eg, < 100 participants).1–9 A number of interventions focused primarily on existential issues have not targeted patients with advanced or terminal cancer.10–12
We developed meaning-centered psychotherapy (MCP) specifically to address the loss of spiritual well-being or sense of meaning in life and the existential distress that often arise in patients with advanced cancer.13,14 Our pilot studies of group and individualized formats of MCP provided preliminary support for this intervention.15,16 Although these randomized controlled trials (RCTs) demonstrated significant improvement in spiritual well-being, results for other outcome variables (eg, quality of life, hopelessness, desire for hastened death, depression) were weaker and/or inconsistent across the two studies. The current study was designed to provide a rigorous test of group MCP (MCGP) in a large sample of patients with advanced cancer using an RCT design. The primary hypothesis was that MCGP would result in significantly greater improvement in spiritual well-being and quality of life compared with supportive group psychotherapy (SGP). Secondary outcome variables included depression, hopelessness, desire for hastened death, anxiety, and physical symptom distress.
PATIENTS AND METHODS
Participants
Patients with advanced cancer were recruited from outpatient clinics at Memorial Sloan-Kettering Cancer Center between August 2007 and May 2012. Prospective participants (N = 3,291) were identified through flyers posted in waiting areas (eg, breast, prostate, thoracic, pancreatic ambulatory care clinics), a review of medical records in these clinics, and direct referral from physicians. Power analysis based on effect sizes observed in our pilot study (d = .38 to .64 for primary outcome variables within MCGP) indicated that 126 participants were needed in each treatment arm to generate 0.80 power (P < .01) for the primary analyses. Eligibility requirements were stage IV cancer (or stage III cancer if diagnosed with poor-prognosis disease [eg, pancreatic cancer]), English speaking, age > 18 years, and ambulatory. Exclusion criteria were significant cognitive impairment or psychotic symptoms (based on clinician assessment) or physical limitations that impeded completion of an outpatient group-based intervention. Potential participants were informed of the study risks and benefits and provided written consent. The study was approved by the institutional review boards of Memorial Sloan-Kettering Cancer Center and Fordham University.
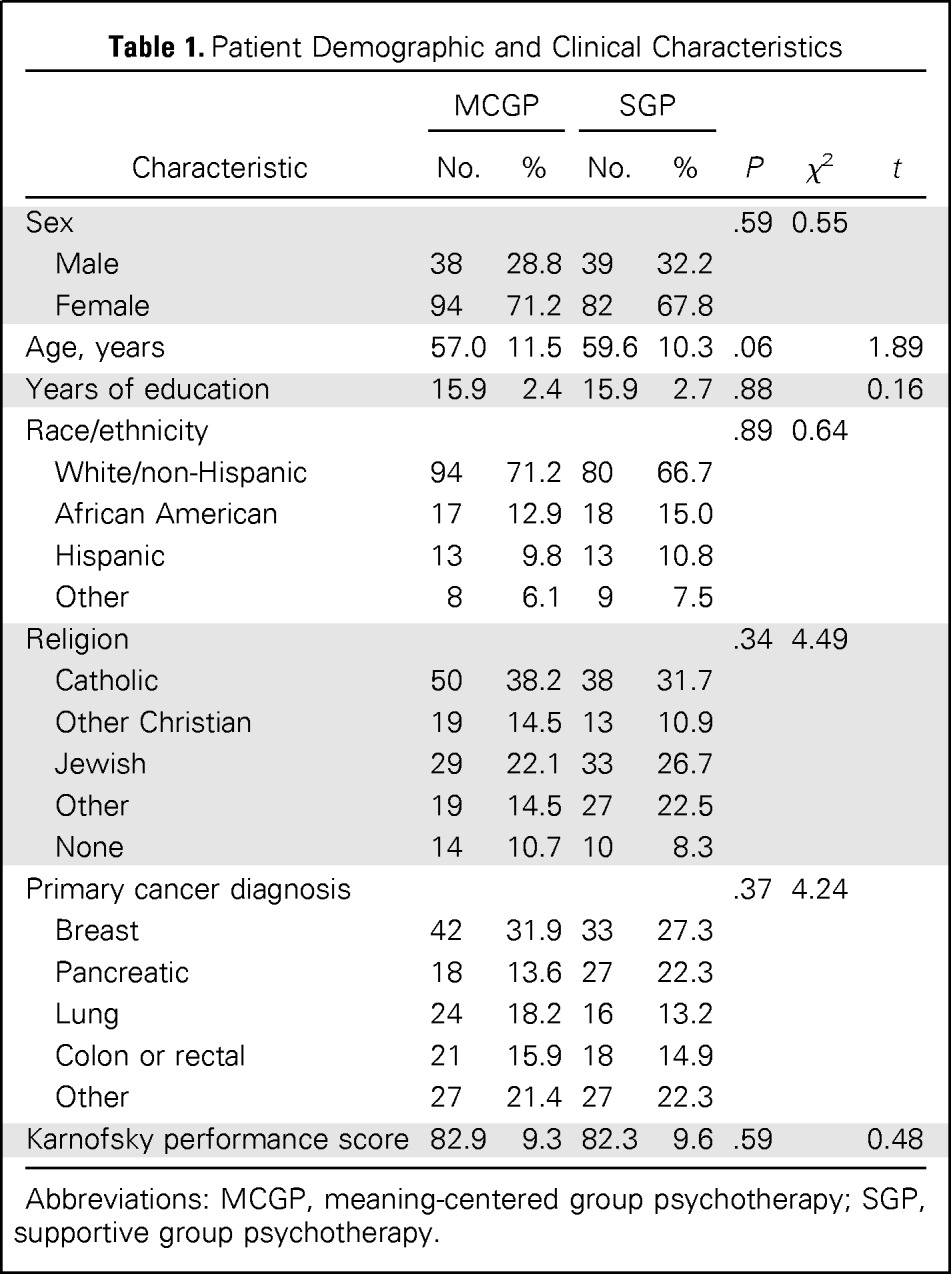
A total of 253 patients (77 men, 176 women) consented to participate and completed the baseline assessment (Table 1). The sample ranged in age from 27 to 91 years, with a mean age of 58.2 years (± standard deviation [SD], 11.0) and an average of 15.9 years of education (SD, 2.5; range, 9 to 23 years). The sample was predominantly white (n = 191 [75.5%]), and the most common religious affiliations were Catholic (n = 88 [34.8%]) and Jewish (n = 61 [24.1%]). Common cancer diagnoses included breast (n = 75 [29.6%]), pancreatic (n = 45 [17.8%]), lung (n = 40 [15.8%]), and colon or rectal (n = 39 [15.4%]); 216 participants (85.4%) had stage IV disease, and 35 (12.8%) had stage III disease (typically pancreatic cancer). There were no differences on any demographic or medical variables between the two treatment arms (Table 1).
Table 1.
Patient Demographic and Clinical Characteristics
| Characteristic | MCGP |
SGP |
P | χ2 | t | ||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Sex | .59 | 0.55 | |||||
| Male | 38 | 28.8 | 39 | 32.2 | |||
| Female | 94 | 71.2 | 82 | 67.8 | |||
| Age, years | 57.0 | 11.5 | 59.6 | 10.3 | .06 | 1.89 | |
| Years of education | 15.9 | 2.4 | 15.9 | 2.7 | .88 | 0.16 | |
| Race/ethnicity | .89 | 0.64 | |||||
| White/non-Hispanic | 94 | 71.2 | 80 | 66.7 | |||
| African American | 17 | 12.9 | 18 | 15.0 | |||
| Hispanic | 13 | 9.8 | 13 | 10.8 | |||
| Other | 8 | 6.1 | 9 | 7.5 | |||
| Religion | .34 | 4.49 | |||||
| Catholic | 50 | 38.2 | 38 | 31.7 | |||
| Other Christian | 19 | 14.5 | 13 | 10.9 | |||
| Jewish | 29 | 22.1 | 33 | 26.7 | |||
| Other | 19 | 14.5 | 27 | 22.5 | |||
| None | 14 | 10.7 | 10 | 8.3 | |||
| Primary cancer diagnosis | .37 | 4.24 | |||||
| Breast | 42 | 31.9 | 33 | 27.3 | |||
| Pancreatic | 18 | 13.6 | 27 | 22.3 | |||
| Lung | 24 | 18.2 | 16 | 13.2 | |||
| Colon or rectal | 21 | 15.9 | 18 | 14.9 | |||
| Other | 27 | 21.4 | 27 | 22.3 | |||
| Karnofsky performance score | 82.9 | 9.3 | 82.3 | 9.6 | .59 | 0.48 | |
Abbreviations: MCGP, meaning-centered group psychotherapy; SGP, supportive group psychotherapy.
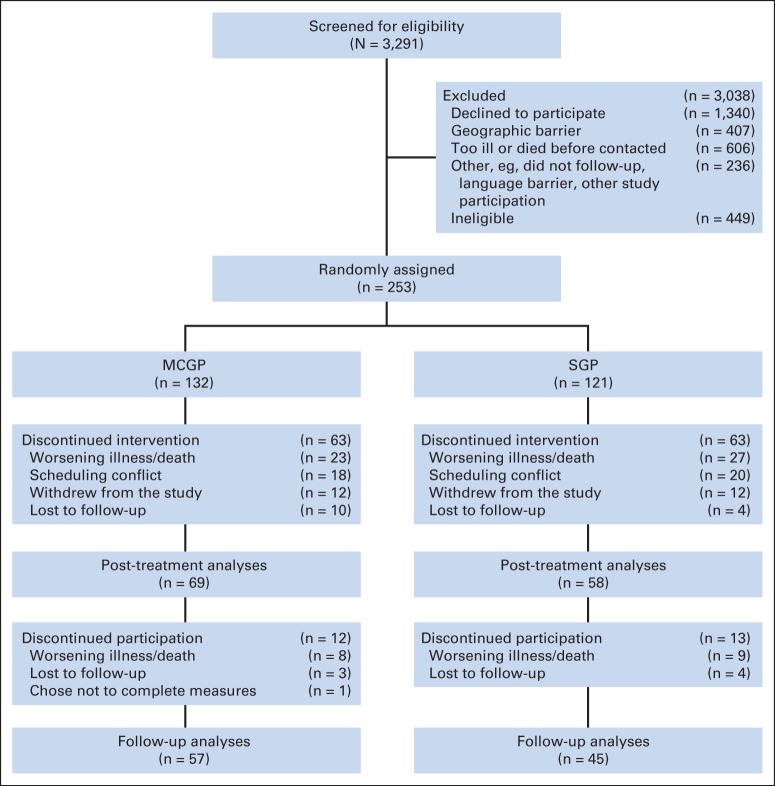
Of 253 individuals who consented to participate in the study, 132 (52.2%) were randomly assigned to MCGP and 121 (47.8%) to SGP.17,18 However, 81 participants (32.0%) never attended any group sessions, typically because of scheduling conflicts (n = 35) or deteriorating health (n = 33); seven participants withdrew because of a lack of interest; reasons for withdrawal were unavailable for six individuals (Fig 1). Of 172 participants who began treatment, 127 (73.8%) completed the 8-week study and post-treatment assessment (50.1% of 253 participants); 102 (40.3%) completed the follow-up assessment 2 months after treatment ended.
Fig 1.
CONSORT diagram. MCGP, meaning-centered group psychotherapy; SGP, supportive group psychotherapy.
Procedures
Clustered randomization was used to assign patients to treatment arm; groups of eight to 10 participants were formed and then randomly assigned to either MCGP or SGP, with each set of eight groups containing four MCGP and four SGP groups. Before the first group session (but after being informed of group assignment), all participants completed self-report questionnaires to measure pretreatment spiritual, psychological, and physical well-being. The same questionnaires were completed after the last group session and 2 months after completion of treatment. The questionnaires included the Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale,19 a measure specifically developed for use in patients with cancer, and the McGill Quality of Life Questionnaire,20 a measure of overall quality of life. Measures of psychological distress included the Beck Depression Inventory21 and the anxiety subscale of the Hospital Anxiety and Depression Scale.22 In addition, the Hopelessness Assessment in Illness Questionnaire,23 a measure of hopelessness developed for use in patients with advanced cancer, and the Schedule of Attitudes Toward Hastened Death,24 a widely used measure of desire for hastened death, were administered to assess more-severe forms of despair. The Memorial Symptom Assessment Scale (MSAS)25 and the Karnofsky Performance Rating Scale26 were used to gauge physical health. Additional measures included the Mini–Mental State Examination (MMSE),27 the Functional Social Support Questionnaire (FSSQ),28 and the Intrinsic/Extrinsic Religiosity Questionnaire (IE-12).29 Participants also completed a post-treatment questionnaire regarding the perceived nature of the intervention.
MCGP is an eight-session manualized psychotherapy intervention grounded in the work of Viktor Frankl.30,31 It focuses on helping patients with advanced cancer develop or increase a sense of meaning in their lives. MCGP sessions were led by a psychiatrist, clinical psychologist, or social worker with experience treating patients with advanced cancer and co-led by a either a second clinician or clinical psychology doctoral student. Group facilitators (n = 9) were trained using both didactic and observational methods and received weekly supervision.
The control condition (SGP) also used a manualized approach developed for patients with advanced cancer.17,18 Weekly SGP sessions focused on coping with advanced cancer by encouraging patients to share concerns related to their diagnosis and treatment, describe experiences and emotions related to cancer, identify challenges they faced, and offer support and advice to one another. Group facilitators (n = 8) included a clinical psychologist or social worker, with a second psychologist or clinical psychology doctoral student co-therapist; therapists were trained in SGP before the study and received weekly supervision. To prevent bleed across conditions, facilitators were trained and conducted sessions in only one intervention.
Adherence to Treatment Format
Group sessions were audio taped, and a random sample (30% of all sessions) were reviewed independently by two raters to monitor treatment adherence. Adherence ratings were made by clinical psychology doctoral students who listened (blinded to treatment arm) to two sessions drawn at random from each group. These ratings indicated close adherence to the manualized treatment (ie, critical elements of each treatment arm were significantly associated with corresponding treatment; P < .001) and significant differences between the two treatments in both content and process (ie, meaning themes were more common among MCGP sessions, and support themes were more common in SGP sessions; P < .001). No differences were found in nonspecific elements of treatment (eg, promoting sense of hope, fostering group cohesion; P > .05).
After completing treatment, patients were asked three questions about their perception of the content of the groups they attended: “How much did this group focus on providing support from other cancer patients?” “How much did this group focus on talking about your feelings about cancer?” and “How much did this group focus on finding a sense of meaning and purpose in life despite having cancer?” These questions were rated on a 0-to-4 scale, ranging from “not at all” to “very much.” There we no significant differences (P > .05) between treatment arms for the first two questions (focus on support: MCGP, 3.6; SGP, 3.2; talking about feelings: MCGP, 3.8; SGP, 3.5), but MCGP participants reported significantly greater emphasis on finding meaning (MCGP, 3.8; SGP, 2.5; F [1,98] = 60.53; P < .001).
Statistical Analysis
Descriptive analyses were used to analyze sample characteristics (eg, attrition rates across treatment arm, adherence to treatment manual). Attrition and patient perceptions of treatment were analyzed with a series of mixed models accounting for the clustered (within treatment group) nature of the data. The analyses of treatment effects used a series of hierarchical linear models (HLMs), with study measures as dependent variables (repeated across time), treatment arm and assessment time point as fixed effects, and group (to account for clustered data) and participant as random effects. The primary dependent variables were spiritual well-being (Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale) and overall quality of life (McGill Quality of Life Questionnaire). Secondary dependent variables included depression (Beck Depression Inventory), anxiety (anxiety subscale of Hospital Anxiety and Depression Scale), hopelessness (Hopelessness Assessment in Illness Questionnaire), desire for hastened death (Schedule of Attitudes Toward Hastened Death), and physical symptom distress (MSAS). In addition, four covariates (also identified a priori) were included to control for potential confounding influences: sex, social support (FSSQ), cognitive functioning (MMSE), and level of religiosity (IE-12). Because treatment effects were not expected to emerge for participants who do not receive an adequate “dose” of treatment, data were analyzed three ways: once for those participants who attended ≥ three sessions, a second time including all participants who were randomly assigned to treatment (ie, intent to treat), and a third time including all participants and no covariates (highly conservative extension of intent-to-treat analysis). The threshold of ≥ three sessions was selected to provide some opportunity for treatment-related differences to emerge while still retaining a conservative approach to these analyses. Because multiple outcome variables were analyzed, critical α values (based on two-tailed tests) were adjusted in accordance with the false-discovery method.32
RESULTS
Group Differences in Attendance and Attrition
Preliminary analyses focused on whether treatment adherence and attrition differed across the two treatment arms, including attrition before treatment began, during the intervention, and after treatment concluded. There were no group differences. Of 132 MCGP participants, 93 (70.5%) attended at least one session versus 79 (65.3%) of 121 SGP participants (χ2 = 0.77; df = 1; P = .23). Of those who began treatment, 69 (74.2%) of 93 MCGP participants completed the post-treatment assessment versus 58 (73.4%) of 79 SGP participants (F [1,110] = 0.36; P = .55). There was also no group difference in number of sessions completed (MCGP: M, 5.55; SD, 2.3; SGP: M, 5.28; SD, 2.3; F [1,111] = 0.63; P = .43). To assess the potential for biased attrition unrelated to group assignment, a series of univariable analyses were used to identify demographic, clinical, and psychosocial variables associated with attrition. Only religion was significant associated with attrition; Christian and Jewish participants had less attrition than those with other or no religious affiliation.
Efficacy of MCGP
A series of HLMs incorporating all three time points were used to evaluate treatment effects. These models analyzed the extent to which treatment group assignment affected the slope of improvement (ie, group × time interaction effect) for each outcome variable. The first set of analyses included four covariates measured at baseline: sex, social support (FSSQ), cognitive functioning (MMSE), and level of religiosity (IE-12). In addition to theoretic relevance, two of these covariates (FSSQ, IE-12) were significantly positively associated with most study outcome variables; sex was included because of its well-established relationship to psychological distress, and MMSE was included based on the expectation that cognitive impairment might limit the ability to benefit from intervention.
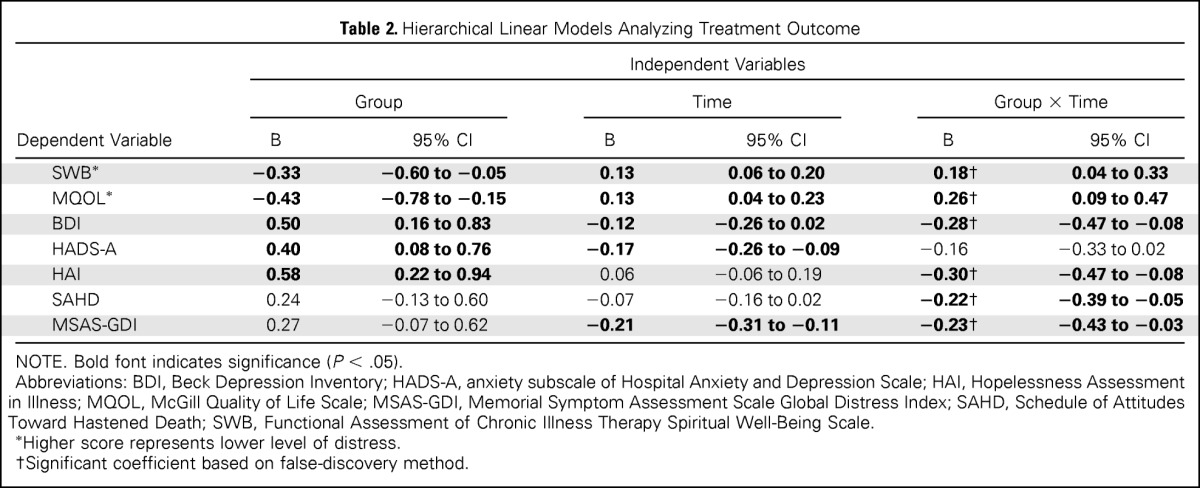
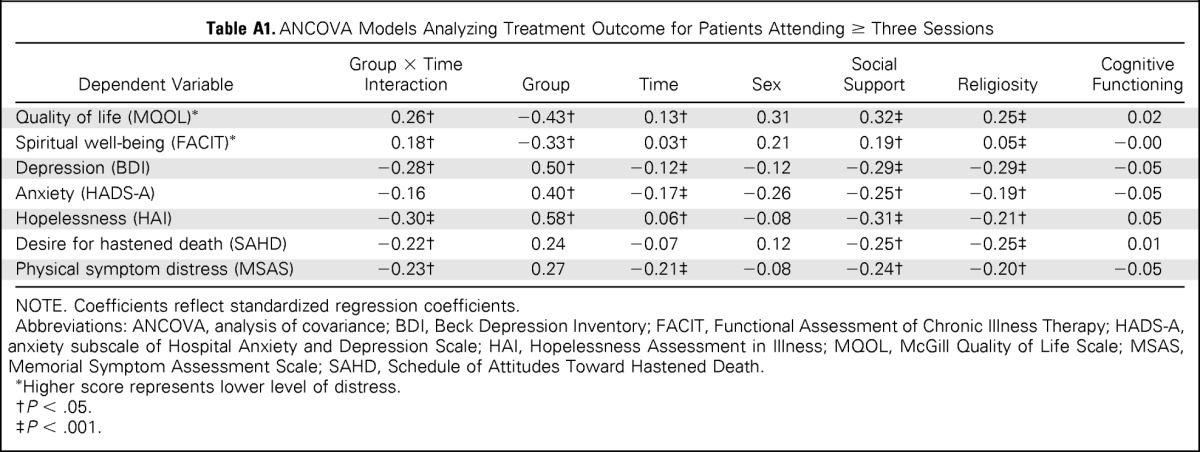
Analyses that included only those individuals who attended ≥ three intervention sessions revealed a significant group × time interaction effect for all but one of the dependent variables (Table 2). Significantly stronger treatment effects were observed for MCGP compared with SGP for quality of life, spiritual well-being, depression, hopelessness, desire for hastened death, and physical symptom distress. There was no significant treatment effect observed for anxiety symptom severity. Of note, each of these treatment effects remained significant when applying the false-discovery method to correct for possible type I error. A significant main effect for time was also observed for most study variables (spiritual well-being, overall quality of life, depression, anxiety, hopelessness, and physical symptom distress), indicating improvement over time for the sample as a whole; no time effect was observed for desire for hastened death. Several models also included a significant main effect for treatment group, indicating a baseline difference in scores on the dependent measure (ie, at baseline, MCGP group had lower levels of spiritual well-being and quality of life and higher levels of anxiety, depression, and hopelessness v SGP group). In addition, two of the covariates provided a significant contribution to each of the models: quality of social support and religiosity (Appendix Table A1, online only). Neither sex nor cognitive functioning was associated with changes in any of the study outcome variables in these multivariable models.
Table 2.
Hierarchical Linear Models Analyzing Treatment Outcome
| Dependent Variable | Independent Variables |
|||||
|---|---|---|---|---|---|---|
| Group |
Time |
Group × Time |
||||
| B | 95% CI | B | 95% CI | B | 95% CI | |
| SWB* | −0.33 | −0.60 to −0.05 | 0.13 | 0.06 to 0.20 | 0.18† | 0.04 to 0.33 |
| MQOL* | −0.43 | −0.78 to −0.15 | 0.13 | 0.04 to 0.23 | 0.26† | 0.09 to 0.47 |
| BDI | 0.50 | 0.16 to 0.83 | −0.12 | −0.26 to 0.02 | −0.28† | −0.47 to −0.08 |
| HADS-A | 0.40 | 0.08 to 0.76 | −0.17 | −0.26 to −0.09 | −0.16 | −0.33 to 0.02 |
| HAI | 0.58 | 0.22 to 0.94 | 0.06 | −0.06 to 0.19 | −0.30† | −0.47 to −0.08 |
| SAHD | 0.24 | −0.13 to 0.60 | −0.07 | −0.16 to 0.02 | −0.22† | −0.39 to −0.05 |
| MSAS-GDI | 0.27 | −0.07 to 0.62 | −0.21 | −0.31 to −0.11 | −0.23† | −0.43 to −0.03 |
NOTE. Bold font indicates significance (P < .05).
Abbreviations: BDI, Beck Depression Inventory; HADS-A, anxiety subscale of Hospital Anxiety and Depression Scale; HAI, Hopelessness Assessment in Illness; MQOL, McGill Quality of Life Scale; MSAS-GDI, Memorial Symptom Assessment Scale Global Distress Index; SAHD, Schedule of Attitudes Toward Hastened Death; SWB, Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale.
Higher score represents lower level of distress.
Significant coefficient based on false-discovery method.
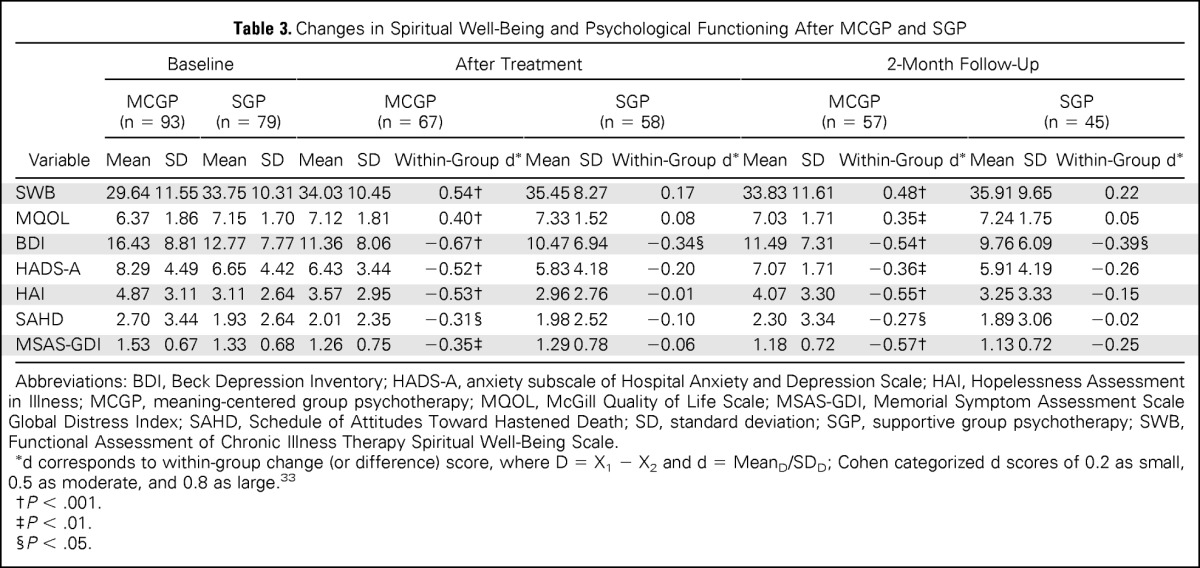
A second set of analyses was conducted that included all of the study participants regardless of how many sessions were attended. As with the previous set of analyses, these analyses included the same four covariates: sex, social support, religiosity, and cognitive functioning. These intent-to-treat analyses revealed a significant group × time interaction for spiritual well-being, quality of life, depression, hopelessness, and desire for hastened death, although not surprisingly, the treatment effects were somewhat more modest. A final set of analyses included all study participants and no covariates, providing the most conservative estimate of treatment effects. These analyses again demonstrated a significant group × time interaction for quality of life, depression, and hopelessness, but the interaction effect for spiritual well-being was no longer significant (P = .07). Examination of the simple change scores (reported solely for descriptive purposes) revealed moderate to strong and significant treatment effects for each of the study variables within the MCGP sample but little benefit (other than for depression) for the SGP group (Table 3). Finally, to assess whether nonrandom attrition affected study results, these models were estimated after including a propensity score based on all available variables measured at baseline.34 Findings were essentially unchanged; only one treatment effect (for MSAS Global Distress Index) was no longer significant after inclusion of the propensity score.
Table 3.
Changes in Spiritual Well-Being and Psychological Functioning After MCGP and SGP
| Variable | Baseline |
After Treatment |
2-Month Follow-Up |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MCGP (n = 93) |
SGP (n = 79) |
MCGP (n = 67) |
SGP (n = 58) |
MCGP (n = 57) |
SGP (n = 45) |
|||||||||||
| Mean | SD | Mean | SD | Mean | SD | Within-Group d* | Mean | SD | Within-Group d* | Mean | SD | Within-Group d* | Mean | SD | Within-Group d* | |
| SWB | 29.64 | 11.55 | 33.75 | 10.31 | 34.03 | 10.45 | 0.54† | 35.45 | 8.27 | 0.17 | 33.83 | 11.61 | 0.48† | 35.91 | 9.65 | 0.22 |
| MQOL | 6.37 | 1.86 | 7.15 | 1.70 | 7.12 | 1.81 | 0.40† | 7.33 | 1.52 | 0.08 | 7.03 | 1.71 | 0.35‡ | 7.24 | 1.75 | 0.05 |
| BDI | 16.43 | 8.81 | 12.77 | 7.77 | 11.36 | 8.06 | −0.67† | 10.47 | 6.94 | −0.34§ | 11.49 | 7.31 | −0.54† | 9.76 | 6.09 | −0.39§ |
| HADS-A | 8.29 | 4.49 | 6.65 | 4.42 | 6.43 | 3.44 | −0.52† | 5.83 | 4.18 | −0.20 | 7.07 | 1.71 | −0.36‡ | 5.91 | 4.19 | −0.26 |
| HAI | 4.87 | 3.11 | 3.11 | 2.64 | 3.57 | 2.95 | −0.53† | 2.96 | 2.76 | −0.01 | 4.07 | 3.30 | −0.55† | 3.25 | 3.33 | −0.15 |
| SAHD | 2.70 | 3.44 | 1.93 | 2.64 | 2.01 | 2.35 | −0.31§ | 1.98 | 2.52 | −0.10 | 2.30 | 3.34 | −0.27§ | 1.89 | 3.06 | −0.02 |
| MSAS-GDI | 1.53 | 0.67 | 1.33 | 0.68 | 1.26 | 0.75 | −0.35‡ | 1.29 | 0.78 | −0.06 | 1.18 | 0.72 | −0.57† | 1.13 | 0.72 | −0.25 |
Abbreviations: BDI, Beck Depression Inventory; HADS-A, anxiety subscale of Hospital Anxiety and Depression Scale; HAI, Hopelessness Assessment in Illness; MCGP, meaning-centered group psychotherapy; MQOL, McGill Quality of Life Scale; MSAS-GDI, Memorial Symptom Assessment Scale Global Distress Index; SAHD, Schedule of Attitudes Toward Hastened Death; SD, standard deviation; SGP, supportive group psychotherapy; SWB, Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale.
d corresponds to within-group change (or difference) score, where D = X1 − X2 and d = MeanD/SDD; Cohen categorized d scores of 0.2 as small, 0.5 as moderate, and 0.8 as large.33
P < .001.
P < .01.
P < .05.
DISCUSSION
This randomized controlled study provides strong support for the efficacy of MCGP as a treatment for psychological, spiritual, and existential distress among patients with advanced cancer. Although our pilot studies generated preliminary support for the utility of this approach, small sample sizes resulted in limited power and some inconsistent findings.15,16 The current study addresses this limitation and demonstrates that although participants in both treatment groups showed some benefit from treatment (based on main effect for time in HLM analyses), improvement was significantly stronger for patients receiving MCGP compared with those receiving SGP (as evidenced by significant time × treatment arm interaction effects for virtually all study variables). More importantly, desire for hastened death, and to a lesser extent, hopelessness, were only affected by MCGP, suggesting that more-severe forms of despair may respond better to an existentially oriented treatment approach than to traditional interventions. These findings are particularly important given the many challenges faced by patients with advanced cancer, including painful symptoms, deteriorating physical functioning, and increasing awareness of mortality, which often lead to worsening distress over time.
Although study results were stronger when we analyzed only those patients who attended ≥ three sessions, intent-to-treat analysis still demonstrated significantly stronger treatment effects for MCGP on most study variables (eg, quality of life, hopelessness). These intent-to-treat analyses are even more important given the modest recruitment rate in our study. Low recruitment rates are not surprising in psychotherapy treatment studies, particularly in the context of aggressive outreach efforts. Thus, although our efforts to identify patients who might not have been aware of or spontaneously sought treatment no doubt decreased our recruitment rate, it likely enhances the generalizability of our study findings to a broader patient population than would be the case if only patients who sought mental health treatment without outreach efforts were included.
There were a number of strengths to this study design, but there were some limitations as well. The most important strengths included the randomized study design comparing a structured, manualized intervention with an active treatment control arm. In addition, adequate treatment adherence and integrity, the large and heterogeneous sample, and well-validated dependent variables and covariates all represented key strengths. Limitations included the lack of a threshold for distress as an entry criterion, which likely resulted in the inclusion of some participants with relatively little distress and hence less opportunity for improvement. This study also did not include midtreatment assessments, which would have facilitated an evaluation of treatment response mediators. Furthermore, despite random assignment of a large sample, group differences in some study variables were observed at baseline. Although the use of HLM analyses limits the impact of baseline group differences on study results, it is still possible that treatment effects were affected by the greater level of distress in patients randomly assigned to MCGP. Finally, like other interventions for patients with advanced cancer, our study had considerable attrition. The group format of this intervention presents challenges for severely ill patients, because group sessions cannot be rescheduled for patients who have illness-related complications or other logistic barriers that affect their ability to attend. Despite this impediment, the significant findings for the intent-to-treat analyses demonstrate that the benefits of MCGP are not simply the result of sample biases or nonrandom attrition. Nevertheless, given that much of the attrition occurred before the first group session, increased attention to screening of prospective participants may help identify those most likely to participate in (and complete) the intervention.
Study limitations notwithstanding, these results provide strong evidence that MCGP is an efficacious intervention for improving quality of life and spiritual well-being and reducing depression, hopelessness, and desire for hastened death. This intervention seems to uniquely target critical elements of existential, spiritual, and psychological distress in patients with advanced cancer. Given that patients confronting a terminal illness often experience these strong feelings of distress, a manualized empirically supported intervention such as MCGP represents an important tool for clinicians who struggle to help their patients with these complex challenges.
Supplementary Material
Acknowledgment
We thank the following colleagues who assisted in this undertaking: Lia Amakawa, PhD, Jordana Jacobs, MA, Elissa Kolva, MA, Yeulin Li, PhD, Allison Marziliano, MA, Megan Olden, PhD, Shannon Popitto, PhD, and Emily Sachs, PhD.
Appendix
Table A1.
ANCOVA Models Analyzing Treatment Outcome for Patients Attending ≥ Three Sessions
| Dependent Variable | Group × Time Interaction | Group | Time | Sex | Social Support | Religiosity | Cognitive Functioning |
|---|---|---|---|---|---|---|---|
| Quality of life (MQOL)* | 0.26† | −0.43† | 0.13† | 0.31 | 0.32‡ | 0.25‡ | 0.02 |
| Spiritual well-being (FACIT)* | 0.18† | −0.33† | 0.03† | 0.21 | 0.19† | 0.05‡ | −0.00 |
| Depression (BDI) | −0.28† | 0.50† | −0.12‡ | −0.12 | −0.29‡ | −0.29‡ | −0.05 |
| Anxiety (HADS-A) | −0.16 | 0.40† | −0.17‡ | −0.26 | −0.25† | −0.19† | −0.05 |
| Hopelessness (HAI) | −0.30‡ | 0.58† | 0.06† | −0.08 | −0.31‡ | −0.21† | 0.05 |
| Desire for hastened death (SAHD) | −0.22† | 0.24 | −0.07 | 0.12 | −0.25† | −0.25‡ | 0.01 |
| Physical symptom distress (MSAS) | −0.23† | 0.27 | −0.21‡ | −0.08 | −0.24† | −0.20† | −0.05 |
NOTE. Coefficients reflect standardized regression coefficients.
Abbreviations: ANCOVA, analysis of covariance; BDI, Beck Depression Inventory; FACIT, Functional Assessment of Chronic Illness Therapy; HADS-A, anxiety subscale of Hospital Anxiety and Depression Scale; HAI, Hopelessness Assessment in Illness; MQOL, McGill Quality of Life Scale; MSAS, Memorial Symptom Assessment Scale; SAHD, Schedule of Attitudes Toward Hastened Death.
Higher score represents lower level of distress.
P < .05.
P < .001.
Footnotes
Supported by National Cancer Institute Grant No. CA128187 (principal investigator, W.B.).
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
Clinical trial information: NCT00494910.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at www.jco.org.
AUTHOR CONTRIBUTIONS
Conception and design: William Breitbart, Barry Rosenfeld, Hayley Pessin
Collection and assembly of data: All authors
Data analysis and interpretation: William Breitbart, Barry Rosenfeld, Hayley Pessin
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Meaning-Centered Group Psychotherapy: An Effective Intervention for Improving Psychological Well-Being in Patients With Advanced Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
William Breitbart
No relationship to disclose
Barry Rosenfeld
No relationship to disclose
Hayley Pessin
No relationship to disclose
Allison Applebaum
No relationship to disclose
Julia Kulikowski
No relationship to disclose
Wendy G. Lichtenthal
No relationship to disclose
REFERENCES
- 1.Classen C, Butler LD, Koopman C, et al. Supportive-expressive group therapy and distress in patients with metastatic breast cancer: A randomized clinical intervention trial. Arch Gen Psychiatry. 2001;58:494–501. doi: 10.1001/archpsyc.58.5.494. [DOI] [PubMed] [Google Scholar]
- 2.Edelman S, Bell DR, Kidman AD. A group cognitive therapy programme with metastatic breast cancer patients. Psychooncology. 1999;8:295–305. doi: 10.1002/(SICI)1099-1611(199907/08)8:4<295::AID-PON386>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 3.Edmonds CVI, Lockwood GA, Cunningham AJ. Psychological response to long-term group therapy: A randomized trial with metastatic breast cancer patients. Psychooncology. 1999;8:74–91. doi: 10.1002/(SICI)1099-1611(199901/02)8:1<74::AID-PON339>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 4.Kissane DW, Grabsch B, Clarke DM, et al. Supportive-expressive group therapy for women with metastatic breast cancer: Survival and psychosocial outcome from a randomized controlled trial. Psychooncology. 2007;16:277–86. doi: 10.1002/pon.1185. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel D, Bloom JR, Yalom I. Group support for patients with metastatic cancer: A randomized outcome study. Arch Gen Psychiatry. 1981;38:527–533. doi: 10.1001/archpsyc.1980.01780300039004. [DOI] [PubMed] [Google Scholar]
- 6.Yalom ID, Greaves C. Group therapy with the terminally ill. Am J Psychiatry. 1977;134:396–400. doi: 10.1176/ajp.134.4.396. [DOI] [PubMed] [Google Scholar]
- 7.Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: A randomized controlled trial. Lancet Oncol. 2011;12:753–762. doi: 10.1016/S1470-2045(11)70153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Vries MJ, Schilder JN, Mulder CL, et al. Phase II study of psychotherapeutic intervention in advanced cancer. Psychooncology. 1997;6:129–137. doi: 10.1002/(SICI)1099-1611(199706)6:2<129::AID-PON264>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 9.Steinhauser KE, Alexander SC, Byock IR, et al. Do preparation and life completion discussions improve functioning and quality of life in seriously ill patients? Pilot randomized control trial. J Palliat Med. 2008;11:1234–1240. doi: 10.1089/jpm.2008.0078. [DOI] [PubMed] [Google Scholar]
- 10.Coward DD. Facilitation of self-transcendence in a breast cancer support group: II. Onc Nurs Forum. 2003;30:291–300. doi: 10.1188/03.ONF.291-300. [DOI] [PubMed] [Google Scholar]
- 11.Kissane DW, Bloch S, Smith GC, et al. Cognitive-existential group psychotherapy for women with primary breast cancer: A randomised controlled trial. Psychooncology. 2003;12:532–546. doi: 10.1002/pon.683. [DOI] [PubMed] [Google Scholar]
- 12.Lee V, Robin Cohen S, Edgar L, et al. Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Soc Sci Med. 2006;62:3133–3145. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 13.Breitbart W. Spirituality and meaning in supportive care: Spirituality and meaning-centered group psychotherapy intervention in advanced cancer. Support Care Cancer. 2002;10:272–278. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 14.Greenstein M, Breitbart W. Cancer and the experience of meaning: A group psychotherapy program for people with cancer. Am J Psychother. 2000;54:486–500. doi: 10.1176/appi.psychotherapy.2000.54.4.486. [DOI] [PubMed] [Google Scholar]
- 15.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psychooncology. 2010;19:21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012;30:1304–1319. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cain EN, Kohorn EI, Quinlan DM, et al. Psychosocial benefits of a cancer support group. Cancer. 1986;57:183–189. doi: 10.1002/1097-0142(19860101)57:1<183::aid-cncr2820570135>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 18.Payne DK, Lundberg JC, Brennan MF, et al. A psychosocial intervention for patients with soft tissue sarcoma. Psychooncology. 1997;6:65–71. doi: 10.1002/(SICI)1099-1611(199703)6:1<65::AID-PON236>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 19.Brady MJ, Peterman AH, Fitchett G, et al. A case of including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8:417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SR, Mount BM, Strobel MG, et al. The McGill Quality of Life Questionnaire: A measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9:207–219. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosenfeld B, Pessin H, Lewis C, et al. Assessing hopelessness in terminally ill cancer patients: Development of the Hopelessness Assessment in Illness Questionnaire. Psych Assess. 2011;23:325–336. doi: 10.1037/a0021767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenfeld B, Breitbart W, Stein K, et al. Measuring desire for death among patients with HIV/AIDS: The Schedule of Attitudes Toward Hastened Death. Am J Psychiatry. 1999;156:94–100. doi: 10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- 25.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: An instrument for evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30A:1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 26.Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, editor. Evaluation of Chemotherapeutic Agents. New York, NY: Columbia University Press; 1949. pp. 191–205. [Google Scholar]
- 27.Folstein M, Folstein S, McHugh P. “Mini-Mental State”: A practical method of grading the cognitive state of patients for the clinician. J Psychiat Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Broadhead WE, Gehlbach SH, DeGruy FV, et al. The Duke-UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients. Med Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Maltby J. The internal structure of a derived, revised, and amended measure of the Religious Orientation Scale: The “Age-Universal” I-E Scale-12. Soc Behav Person. 1999;27:407–412. [Google Scholar]
- 30.Frankl VF. Man's Search for Meaning (ed 4) Boston, MA: Beacon Press; 1959/1992. [Google Scholar]
- 31.Frankl VF. The Will to Meaning: Foundations and Applications of Logotherapy—Expanded Edition. New York, NY: Penguin Books; 1969/1988. [Google Scholar]
- 32.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289–300. [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. London, United Kingdom: Routledge; 1977. [Google Scholar]
- 34.West SG, Cham H, Thoemmes F, et al. Propensity scores as a basis for equating groups: Basic principles and application in clinical treatment outcome research. J Consult Clin Psych. 2014;82:906–919. doi: 10.1037/a0036387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.