Abstract
Introduction
Spontaneous cervical-mediastinal hematoma caused by extracapsular rupture of parathyroid gland occurs extremely rarely. There are no standard treatment approaches because of the peculiarities of each case.
Presentation of case
We report herewith about a rare case of spontaneous cervical-mediastenal hematoma occured by hemorrhage in parathyroid adenoma, which was detected in an previously absolutely healthy female patient in the age of 29. This woman was hospitalized in 2 days after the manifestation, complaining about a neck ache. Indirect laryngoscopy: right-side larynx paresis. Blood test: parathyroid hormone 843 pg/ml (norm 15–65), ionized calcium 1.8 mmol/l (norm 0.9–1.1). Positive dynamics was observed throughout 8 days of anti-inflammatory therapy. Symptoms of neck organs compression increased acutely at the 9th day. The patient was operated – hematoma lancing with resection of walls. Histological examination discovered the fragments of parathyroid adenoma in the hematoma's wall. Level of ionized blood calcium got normal approximately in 24 h after the surgery. The patient was examined 6 months after the surgery. The patient had no disphagy, voice quality was intact, breathing was not restricted. Level of parathyroid hormone in blood got normal.
Discussion
A rareness of this pathology and treatment variability does not allow to choose a unified medical and diagnostic tactics.
Conclusion
Our case demonstrates that radical correction of primary hyperparathyroidism by excision of hematoma and its fibrous capsule with preservation of thyroid gland is possible in conditions of tense cervical-mediastinal hematoma with inflammation process in the hemorrhage area.
Keywords: Hyperparathyroid gland disease, Acute neck diseases, Extracapsular parathyroid hemorrhage, Hypercalcemia, Tumors of parathyroid glands, Larynx paresis
1. Introduction
Spontaneous cervical-mediastinal hematoma caused by extracapsular rupture of parathyroid gland occurs extremely rarely. The first occasion of an spontaneous cervical-mediastinal hematoma caused by hemorrhage into parathyroid adenoma was determined during autopsy.1 It indicates the extreme hazard of this condition. There were 28 reports of individual clinical observations in the PubMed databases until 2009. And 3 more reports during 2010–2013. Clinical presentation of hematoma depends on its localization, dimensions, hemorrhage severity, timing of manifestation and hormonal activity of the parathyroid gland. Differential diagnosis includes acute thyroiditis, hemorrhage into thyroid cysts, descending destructive mediastinitis, aortic dissection. A two-staged clinical presentation is described in one of the reports.1 In the treatment of spontaneous cervical-mediastinal hematoma caused by extracapsular rupture of parathyroid gland is used conservative therapy, emptying and drainage of the hematoma, adenomectomy, excision of adenoma in combination with hematoma evacuation, excision of the respective lobe of thyroid gland together with the hematoma.
2. Case report
Female patient, age 29, admitted to the hospital in 2 days after the manifestation, complaining about neck pain irradiating into nose, mouth, mostly on the right side, difficulty in swallowing, swollen neck, mostly on the right side. There was no determined prior history of trauma, invasive manipulations or pathology of parathyroid glands. During child years, the patient was observed by endocrinologist due to endemic goiter. During the examination, it was discovered that the thyroid gland was enlarged, the consistency was soft and elastic, moderate pain was felt during palpation. The patient had a low-grade fever.
Echography of the thyroid gland indicated that the right lobe was enlarged due to an isoechoic area in the lower posterior part, with dimensions of 28 mm × 26 mm × 30 mm. The patient was hospitalized with suspected acute thyroiditis. A nonhomogenous structure with contained liquid and abnormally high blood circulation, which was spreading over the posterior surface of the thyroid gland into mediastinal septum was determined one day later, during echography of the thyroid gland (Fig. 1). Indirect laryngoscopy: right-side larynx paresis. Blood test: parathyroid hormone 843 pg/ml (norm 15–65), chlorine – 110.7 mmol/l (norm 97–110), calcium – 2.96 mmol/l (norm 2.10–2.60), ionized calcium 1.8 mmol/l (norm 0.9–1.1), TSh 0.9 mкME/ml (norm 0.4–4.0), fT4 11.9 pmol/l (norm 9.0–22.2) hemoglobin 129 g/l (norm 120–150), hematocrit 37.4% (norm 36–42). Within three days of hospitalization the patient was diagnosed with spontaneous hematoma of the neck on the right side. We did not know the reason for the hematoma, but figured out an increase of blood calcium levels. This was the basis for determining of the level of parathyroid hormone. The result of this analysis was obtained the 3rd day after. Positive dynamics was observed throughout 8 days of fluid treatment (0.9% aqueous solution of sodium chloride) and anti-inflammatory therapy (prednisolone, amoxicillin + clavulanic acid) – reduction of pain syndrome, dysphagy, reduction of swelling and pain in the neck area. Ecchymosis appeared in the skin of neck area and chest. The patient continued to run a low-grade fever. The patient's condition improved within 8 days, and there was a hope for recovery without any operation. We have not seen any activity of the parathyroid glands by 99mTc-Pertechnetate Scintigraphy. However, a simple combination of hematoma and hyperparathyroidism seemed unlikely.
Fig. 1.
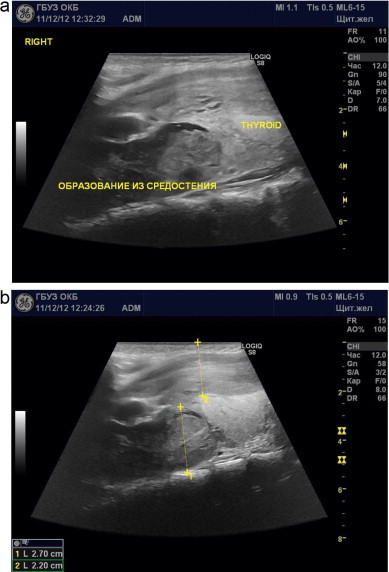
Transcutaneous echography. Sagittal section. (a) A nonhomogenous structure in cervical-mediastenal area, to the right of the thyroid gland. (b) An isoechoic nonhomogenous structure sized up to 3 cm is adjacent to the posterior surface of thyroid gland, with an apparent capsule (1) (parathyroid gland adenoma with hemorrhage). A hypoechoic to echonegative area spreads from the structure into mediastenal septum and into the anterior neck surface (2) (a cervical-mediastenal hematoma).
Symptoms of neck organs compression increased at the 9th day. There were signs of breathing difficulties and the operation got inevitable. An ultrasonography of the neck vessels was performed to identify the source of bleeding before surgery – the source was not found. A tense hematoma (Fig. 2) and hemorrhage into the hematoma cavity from the branch of inferior thyroid artery were visualized on a multi-slice CT scan with angiography. Discussion dealt with several possible operations: a simple hematoma emptying from a small incision; a full audit of the neck and removal of the modified parathyroid gland simultaneously with the removal of the hematoma. The difficulty consisted in that we did not know what parathyroid gland caused the hyperparathyroidism. We did not know how many parathyroid glands have increased its function. There was the risk of hypercalcemic crisis while leaving the source of hyperparathyroidism. There was a risk of rebleeding by simply hematoma draining. In addition, we bewared of the presence of inflammation in the hematoma area that bores the risk of wound infection in case of a full neck audit. Therefore it was decided to search for the parathyroid glands only on the right side after hematoma emptying and ligation of the bleeding source. The patient was operated – hematoma lancing with resection of walls. The standard cross cervical access used for thyroidectomy was applied. The operation detected the deformation of the right lobe of thyroid gland. The capsule was involved in an inflammatory process. A significant scarring process was observed in the area of hematoma capsule. The hematoma cavity was opened by a small incision. 100 ml of old blood was removed. The hematoma cavity contained fragments of tissues, which were not related to the capsule. These tissues were removed for histological examination. There was a defect along the lower lateral wall of hematoma cavity. The blood clots were removed from a mediastinum through this defect. There was no hemorrhage during the surgery.
Fig. 2.
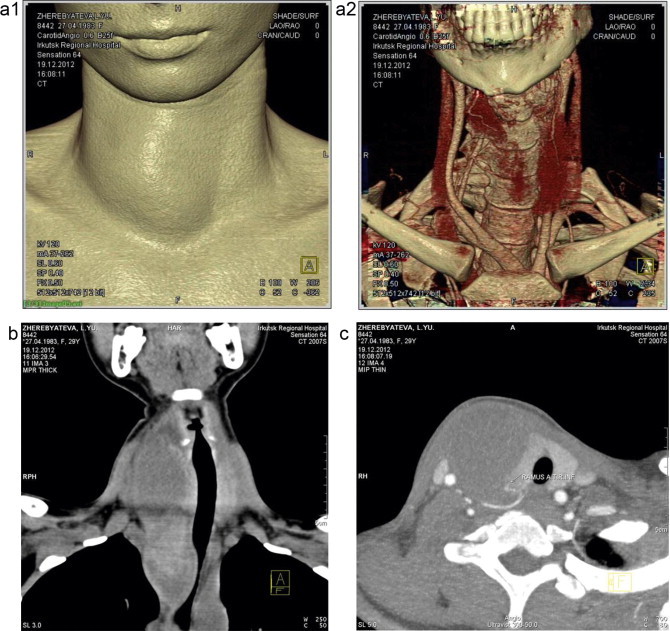
Multi-slice CT scan with angiography: (a) 3D reconstruction. Deformation of the anterior neck surface with shift of thyroid gland by a non-vascular lesion (hematoma) and (c) axial scan. A mass lesion compressing the tracheal lumen is located to the right of the thyroid gland. Extravasation of contrast media into hematoma volume is observed in the bifurcation zone of inferior thyroid artery. (b) Multi-slice CT scan: Frontal scan. A mass lesion is located to the right of the thyroid gland, propagating into mediastenal septum and compressing the tracheal lumen.
The right recurrent laryngeal nerve was exposed through the rear wall of the hematoma and separated from scars along the distance up mediastinum to larynx. Hematoma wall joined to thyroid gland were removed for histological examination. Hematoma wall joined to shroud of common carotid artery and internal jugular vein were removed for histological examination. A branch of the inferior thyroid artery was exposed during mobilization of the lateral hematoma wall. The branch ended in the hematoma wall. The proximal part of that branch was ligated, while the distal part was excised together with hematoma wall.
Histological examination discovered the fragments of parathyroid adenoma in the hematoma wall (Fig. 3). Level of ionized blood calcium got normal (1.06) approximately 24 h after the surgery. There were no complications during the post-operative period. Level of parathyroid hormone in blood at the 10th day after the surgery amounted to 26 pmol/l (norm 1.45–10.41). The patient was examined 6 months after the surgery. The patient had no complaints. She observed that her voice quality restored 2 months after the surgery, though the laryngoscopy indicated a still conserved right-side paresis of the larynx. The patient did not feel disphagy, voice quality was intact, breathing was not restricted. Level of parathyroid hormone in blood amounted to 8 pmol/l (norm 1.45–10.41), serum ionized calcium concentration 1.14 pmol/l (norm 1.03–1.23), inorganic phosphorus 1.37 mmol/l (norm 0.87–1.45).
Fig. 3.
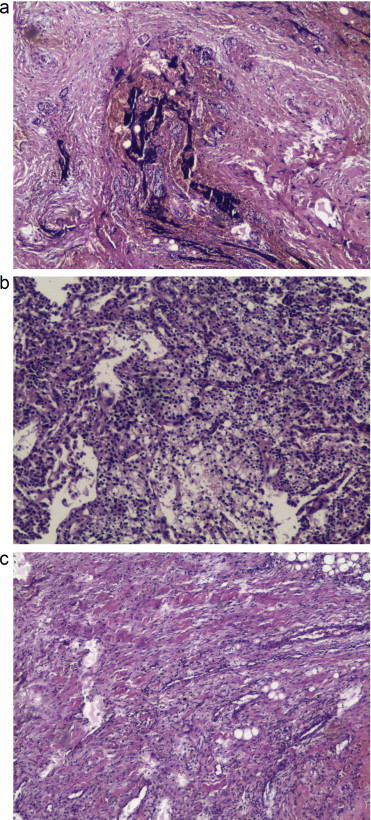
Microphotography of operative material. Tinted with hematoxylin and eosine. Magnification ×400. (a) Hematoma wall is composed of fibrous connective tissue, sediment of hemosiderin, fragment of fat tissue, lymphoplasmocitary infiltration. (b) Hematoma wall is composed of fibrous connective tissue, vessels, small fragments of parathyroid gland tissue in fibrous tissue. (c) Tissue of parathyroidgland adenoma with focal hemorrhage.
3. Discussion
For the first time, our observation demonstrates the cyclic dynamics in the clinical presentation of parathyroid adenoma rupture. First indicators of hemorrhage are determined as acute pain, neck deformation and dysphagy. In our case, this clinical presentation maintained during 3 days. The symptoms of neck organs compression were reduced during a week. It was period of assumptive recovery. Moderately increased level of blood calcium and absence of breathing restriction served as reason for conservative therapy, which is compliant with opinions of a number of authors: an uncomplicated hematoma does not require urgent surgery2; adenomectomy may be performed 3 months after drainage or dispersion of the hematoma; spontaneous remission of primary hyperparathyroid gland disease is possible in case of hemorrage into parathyroid glands.3 Neck compression syndrome, which developed by the end of the second week since the manifestation of the condition, became the immediate cause for surgery. Disturbed anatomic relations and presence of an inflammatory process in the surgery area require minimal surgical invasion – emptying and drainage of the hematoma.4 At the same time, this tactic can lead to the hemorrhage recurrence and risk of a hypercalcemic crisis. An alternative viewpoint suggests that excision of adenoma in combination with hematoma evacuation at early stages causes serum calcium normalization.4 During later stages of the condition, the respective lobe of thyroid gland is excised together with the hematoma.1 In our case, operation time was unfavorable because of inflammatory and scarring processes in the hemorrhage zone. Despite of this, the excision of the hematoma wall enabled to identify and eliminate the hemorrhage source and remove fragments of parathyroid adenoma, while preserving the thyroid gland lobe. Recuperation of the patient confirms the correctness of chosen therapy tactics. At the same time, this observation demonstrates that conservative therapy in case of parathyroid adenoma rupture does not eliminate the risks of repeated hemorrhage or compressive damage to recurrent laryngeal nerve. The duration of vocal cords recuperation in this condition is not systematized. Based on our data, mobility of vocal cords in the condition of post-operative larynx paresis is restored over the period from 1 to 15 months.5 Prolonged nerve compression may determine longer recuperation period.
4. Conclusion
The present clinical observation is targeted to draw the attention of a wide range of medical doctors (general practitioners, ENT specialists, dentists, surgeons) to this rare complication. If a patient develops sudden swelling of the neck area, the possibility of spontaneous rupture of pathologically deformed parathyroid gland must be suspected. Positive dynamics associated with conservative therapy may be of temporary nature, followed by deterioration of life-threatening neck organs compression symptoms. Excision of hematoma and its fibrous capsule with preservation of thyroid gland is followed by elimination of neck organs compression syndrome, elimination of repeated hemorrhage risk, and later normalization of hormonal status. Identification of larynx paresis by cervical-mediastinal hematoma may be viewed as an additional argument in favor of early surgery.
Conflict of interest
The author states that no conflict of interests is involved with the present publication.
Ethical approval
A written informed consent was granted by the patient to publish the present case and all associated images. A copy of the patient's written consent is available for review of the journal's Editor-in-Chief.
Author contributions
The author of the present publication has performed the surgical stage of therapy, publications analysis, described the case and compiled the manuscript.
Acknowledgments
I am grateful to the following persons for their role during this study: Ekaterina Danilova, Chief of Endocrinology Department, State Budgetary Institution of Public Health “Irkutsk Regional Clinical Hospital”, Irkutsk (physician-in-chief P.E. Dudin) for examination of the patient's endocrinological status; Valery Makhutov, Chief of Surgical Department, State Budgetary Institution of Public Health “Irkutsk Regional Clinical Hospital”, Irkutsk (physician-in-chief P.E. Dudin) for the support during all stages of therapy and assistance in manuscript drafting; Natalia Krasnikov and Tatyana Boyko, radiologists, State Budgetary Institution of Public Health “Irkutsk Regional Clinical Hospital”, Irkutsk (physician-in-chief P.E. Dudin) in the preparation for publishing (Fig. 1) and (Fig. 2), respectively; Elena Rozhanskaya, anatomic pathologist, Oleg Kanya, Chief of Anatomic Pathology Department, State Budgetary Institution of Public Health “Irkutsk Regional Bureau of Anatomic Pathology” (Director L.P. Grishina) in the preparation for publishing (Fig. 3).
References
- 1.Merante-Boschin I., Fassan M., Pelizzo M.R., Ide E.C. Neck emergency due to parathyroid adenoma bleeding: a case report. J Med Case Rep. 2009;3:7404. doi: 10.1186/1752-1947-3-7404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nito T., Miyajima C., Kimura M., Sugasawa M. Parathyroid adenoma causing spontaneous cervical hematoma: a case report. Acta Otolaryngol Suppl. 2007:160–163. doi: 10.1080/03655230701600491. Dec;(559) [DOI] [PubMed] [Google Scholar]
- 3.Chaffanjon P.C., Chavanis N., Chabre O., Brichon P.Y. Extracapsular hematoma of the parathyroid glands. World J Surg. 2003;27(1):14–17. doi: 10.1007/s00268-002-6429-y. [abstract] [DOI] [PubMed] [Google Scholar]
- 4.Rehman H.U., Markovski M., Khalifa A. Spontaneous cervical hematoma associated with parathyroid adenoma. CMAJ. 2010;182:E632. doi: 10.1503/cmaj.091167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Il’icheva E.A., Shpakova E.A., Roi T.A., Makhutov V.N., Tarnueva I.F., Moshkova E.S. Specific features of laryngeal paresis following surgical treatment of diffuse toxic goiter (a prospective longitudinal passive study) Vestn Otorinolaringol. 2011;3:51–54. [abstract] [PubMed] [Google Scholar]


