Highlights
-
•
Primary malignant melanoma of the esophagus is a rare and aggressive disease.
-
•
Only a handful of long term survivors have been reported.
-
•
We report the case of a 7 year survivor treated with surgical resection who remains disease free.
-
•
We review the literature for the treatment of primary malignant melanoma of the esophagus, which remains controversial.
Abbreviations: PMME, primary malignant melanoma of the esophagus; CT, computed tomography; PET, positron emission tomography
Keywords: Primary malignant melanoma of the esophagus, Esophageal neoplasms, Video assisted thoracoscopic surgery
Abstract
Introduction
Primary malignant melanoma of the esophagus is a rare diagnosis with only a few hundred cases reported in the literature. Due to the aggressive nature of this disease, long-term survivors are exceedingly rare with only a handful of case reports.
Presentation of case
We report the case of a 38 year old man who presented with chest and back pain. Workup revealed a mediastinal mass and the patient was diagnosed with primary malignant melanoma of the esophagus and treated with radical resection. Despite the poor prognosis associated with primary malignant melanoma of the esophagus, he remains disease free for over 7 years.
Discussion
Initially primary malignant melanoma of the esophagus was a controversial diagnosis until the demonstration of normal melanocytes in healthy patients. It is an aggressive disease that is nearly uniformly fatal. Review of the literature shows that treatment with radical surgical resection extends prognosis by months while treatment with adjuvant chemotherapy is controversial.
Conclusion
Primary malignant melanoma of the esophagus is a rare and aggressive disease that should be treated with surgical resection when feasible. We report the rare case of a long term survivor over 7 years since diagnosis.
1. Case presentation
An athletic 38 year old African American gentleman presented to the emergency room after a bout of “food poisoning” with chest pain and back discomfort. The workup included a chest X-ray (Fig. 1) revealing a mediastinal mass. Upon further questioning the patient denied any history of hematemesis, melena, dysphagia, or weight loss. His family history was notable for colon cancer in his mother. Physical exam was unremarkable for a palpable abdominal mass or any suspicious skin lesions.
Fig. 1.

Conventional chest X-ray showing a mediastinal mass superimposed on the left heart.
He underwent a computed tomography (CT) scan which showed a large posterior mediastinal mass measuring 9.4 cm × 7.8 cm × 8.4 cm extending laterally from the esophagus and compressing the left lower lobe of the lung at the level of T8–T11 (Fig. 2). There were no other lesions or masses identified, no lymphadenopathy, and no free fluid. An esophageal contrast study showed extrinsic compression of the posterior esophagus with no mucosal lesion (Fig. 3). Endoscopic ultrasound was consistent with a submucosal lesion without mucosal involvement. An adjacent lymph node at 47 cm was observed, when biopsied was consistent with malignant melanoma. Further workup with fluoro-deoxyglucose–positron emission tomography (FDG–PET), magnetic resonance imaging of the brain, and fundoscopic exams showed no evidence of distant disease. Resection was recommended.
Fig. 2.
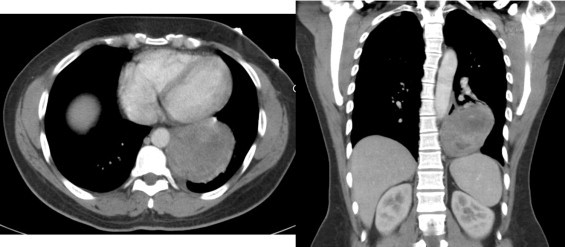
Computed tomography showing transverse (left) and coronal (right) sections through the tumor.
Fig. 3.

Barium swallow study showing extrinsic compression of the esophagus. The mediastinal mass is again demonstrated.
At the time of operation a video-assisted thoracoscopy was performed to rule out gross dissemination, which would make resection futile. The tumor was observed to extend directly from the esophagus to the left lower lobe at the fissure but appeared resectable (Fig. 4). A thoracoabdominal approach was performed from the sixth interspace. The esophagus and stomach were mobilized and the Kocher maneuver was carried out with dissection across the hiatus into the lower chest freeing up the tumor with the attached portion of the lower lobe. A left lower lobectomy was then performed to be included en bloc with the esophagus. The proximal esophagus was divided and the stomach tubularized. A pyloroplasty was performed and the gastric conduit anastamosed to the proximal esophagus using an end to end anastomosis stapler.
Fig. 4.
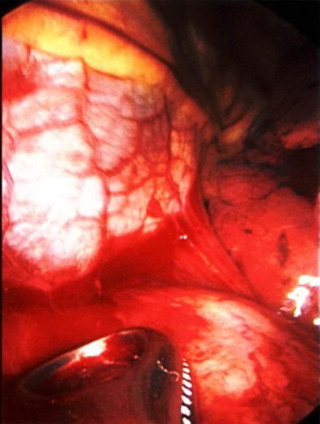
VATS image of clamp displacing mass revealing inflammatory adhesions to the pericardium.
Pathology of the specimen revealed a malignant melanoma, circumscribed, bordering the esophageal adventitia and the pleura of the left lower lobe (Fig. 5). Incidentally found was a CD 117 positive gastrointestinal tumor of the stomach.
Fig. 5.
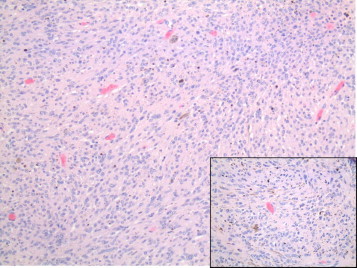
Photomicrograph showing diffuse sheets of atypical cells with dark brown pigments in the background. (Hematoxylin and eosin × 200). Inset shows pleomophic cells with abundant eosinophilic cytoplasm (Hematoxylin and eosin × 400).
The patient had an uneventful hospital course and was discharged home. He has subsequently undergone regular CT and PET–CT scans and remains disease free for over 7 years.
2. Discussion
Primary malignant melanoma of the esophagus (PMME) is a rare diagnosis. The first described case was by Baur [1] in 1906, and since then approximately 340 have been reported in the literature [2]. In a recently published series of 910 esophageal biopsies in Japan, only 2 were found to be melanoma (0.2%) [3]. This is consistent with previously published data in which PMME accounted for 0.1–0.2% of malignant esophageal lesions [4]. The average age of onset is 60.5 years with a male to female ratio of 2:1 [2].
In 1964 Das Gupta and Brasfield [5] demonstrated that malignant melanoma metastasized to the esophagus in 4% of autopsies of patients who had died of melanoma arising from cutaneous sites. It was not until 1963 that typical melanocytes were demonstrated in the esophagus in 4% of cadavers who did not die of malignant melanoma [6]. Until then, typical melanocytes had not been described in the esophagus, so a diagnosis of PMME was controversial. Melanocytosis of the esophagus, sometimes a consequence of chronic esophagitis, may be a precursor of PMME. There is at least one documented case of PMME arising from localized benign melanocytosis [7].
Regardless of the pathophysiology, the prognosis of PMME is very poor and with few exceptions is uniformly fatal. Sabanathan et al. reported an overall survival of 9.8 months, 14.2 months for radical resections and 9 months after limited local resection [4]. Of the patients undergoing palliative or therapeutic resection, they reported a 5-year survival rate of 4% for patients undergoing surgery in a series of 139 patients. More recently, Volpin et al. calculated an improved 5-year survival rate of 37% in a review 25 patients undergoing surgical resection based on the literature between 1989 and 2000. Death occurred in the first postoperative year in 77% of those patients [8].
Reports of long-term survivors are still rare, however. Radical excision extends mean survival to just over a year, and the role for chemotherapy and interferon therapy is unclear. There are five reports of patients surviving more than 7 years, several of whom had chemotherapy in addition to surgical resection. In 2004, Uetsuka et al. [9] reported a disease-free 8-year survivor who underwent sub-total esophagectomy and proximal gastrectomy after two weeks of preoperative chemotherapy with dacarbazine, nimustine, cisplatin, and tamoxifen, which resulted in shrinkage of the tumor by approximately 30%. The patient also underwent post-operative chemotherapy with 12 courses of the same regimen and continued on daily tamoxifen and monthly interferon-beta injections [9]. In 2007, Kawada et al. [10] reported another 7-year survivor who underwent a similar treatment with 1 course of pre-operative and 9 courses of post-operative therapy with dacarbazine, nimustine, and vincristine. In addition to postoperative injections, interferon beta was injected preoperatively directly into the tumor. Tamoxifen was not used in this case. In a third case, a patient treated with resection alone was found to have metastasis to a supraclavicular lymph node 30 months after surgery and treated with radiation and 5-fluoro uracil [11]. This patient went on to be disease-free for at least 9 years after the original operation. Itami et al. [12] report a woman who was alive and disease free 11 years after resection of PMME. She received neoadjuvant and adjuvant cisplatin. Interestingly, the longest reported survivor had positive lymph nodes and did not receive chemotherapy as Hamdy et al. [13] reported a woman who had a large 12 cm esophageal melanoma with positive lymph nodes found at the time of surgery. She was treated with surgical resection alone and despite positive nodes she was disease-free for at least 12 years.
The patient we report here did not receive chemotherapy but is a long-term survivor who has been disease-free for 7 years. While the role of chemotherapy and interferon therapy is unclear, radical surgical resection of PMME offers the opportunity for long-term survival despite a poor overall prognosis.
Conflicts of interest
The authors have no conflicts of interest to report.
Funding
There were no sources of funding for this work.
Consent
The patient provided written, informed consent to access his medical record and publish his case report.
Author contributions
Dr. Joseph Sabat authored the manuscript.
Dr. Rifat Mannan interpreted and provided the pathological images and description of the histopathology.
Dr. Alan Legasto interpreted and provided the radiological images.
Dr. Cliff Connery is the attending surgeon who follows the patient and performed the surgery.
References
- 1.Baur E. Ein Fall von primärem Melanom des Oesophagus. Arb. Geb. Pathol. Anat. Inst. Tuebingen. 1906;5:343–354. [Google Scholar]
- 2.Iwanuma Y., Tomita N., Amano T. Current status of primary malignant melanoma of the esophagus: clinical features, pathology, management and prognosis. J. Gastroenterol. 2012;47(1):21–28. doi: 10.1007/s00535-011-0490-y. [DOI] [PubMed] [Google Scholar]
- 3.Terada T. A clinicopathologic study of esophageal 860 benign and malignant lesions in 910 cases of consecutive esophageal biopsies. Int. J. Clin. Exp. Pathol. 2013;6(2):191–198. [PMC free article] [PubMed] [Google Scholar]
- 4.Sabanathan S., Eng J., Pradhan G.N. Primary malignant melanoma of the esophagus. Am. J. Gastroenterol. 1989;84(12):1475–1481. [PubMed] [Google Scholar]
- 5.Dasgupta T., Brasfield R. Metastatic melanoma. A clinicopathological study. Cancer. 1964;17:1323–1339. doi: 10.1002/1097-0142(196410)17:10<1323::aid-cncr2820171015>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 6.De La Pava S., Nigogosyan G., Pickren J.W., Cabrera A. Melanosis of the esophagus. Cancer. 1963;16:48–50. doi: 10.1002/1097-0142(196301)16:1<48::aid-cncr2820160107>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 7.Maroy B., Baylac F. Primary malignant esophageal melanoma arising from localized benign melanocytosis. Clin. Res. Hepatol. Gastroenterol. 2013;37(2):e65–67. doi: 10.1016/j.clinre.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Volpin E., Sauvanet A., Couvelard A., Belghiti J. Primary malignant melanoma of the esophagus: a case report S. D. E. review of the literature. Dis. Esophagus: Off. J. Int. Soc. Dis. Esophagus. 2002;15(3):244–249. doi: 10.1046/j.1442-2050.2002.00237.x. [DOI] [PubMed] [Google Scholar]
- 9.Uetsuka H., Naomoto Y., Fujiwara T. Primary malignant melanoma of the esophagus: long-term survival following pre- and postoperative adjuvant hormone/chemotherapy. Digest. Dis. Sci. 2004;49(10):1646–1651. doi: 10.1023/b:ddas.0000043379.60295.cb. [DOI] [PubMed] [Google Scholar]
- 10.Kawada K., Kawano T., Nagai K. Local injection of interferon beta in malignant melanoma of the esophagus as adjuvant of systemic pre- and postoperative DAV chemotherapy: case report with 7 years of long-term survival. Gastrointest. Endosc. 2007;66(2):408–410. doi: 10.1016/j.gie.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 11.Khoury-Helou A., Lozac’h C., Vandenbrouke F., Lozac’h P. [Primary malignant melanoma of the esophagus] Ann. Chir. 2001;126(6):557–560. doi: 10.1016/s0003-3944(01)00553-3. [DOI] [PubMed] [Google Scholar]
- 12.Itami A., Tomokazu M., Yutaka S., Masayuki I. A case of primary malignant melanoma of the esophagus with long-term survival. Esophagus. 2004;1(3):135–137. [Google Scholar]
- 13.Hamdy F.C., Smith J.H., Kennedy A., Thorpe J.A. Long survival after excision of a primary malignant melanoma of the oesophagus. Thorax. 1991;46(5):397–398. doi: 10.1136/thx.46.5.397. [DOI] [PMC free article] [PubMed] [Google Scholar]


