Abstract
Streptococcus mitis has emerged as one of the leading causes of bacterial endocarditis and is related to Streptococcus pneumoniae. Antibiotic resistance has also increased among strains of S. mitis and S. pneumoniae. Phages are being reinvestigated as alternatives to antibiotics for managing infections. In this study, the two virulent phages Cp-1 (Podoviridae) and Dp-1 (Siphoviridae), previously isolated from S. pneumoniae, were found to also infect S. mitis. Microbiological assays showed that both pneumophages could not only replicate in S. mitis but also produced more visible plaques on this host. However, the burst size and phage adsorption data were lower in S. mitis as compared to S. pneumoniae. A comparison of the genomes of each phage grown on both hosts produced identical nucleotide sequences, confirming that the same phages infect both bacterial species. We also discovered that the genomic sequence of podophage Cp-1 of the Félix d’Hérelle collection is different than the previously reported sequence and thus renamed SOCP.
Introduction
The Mitis group of streptococci is a member of the viridans group of streptococci [VGS], which includes several species that reside in the human oral cavity and the upper respiratory tract. In the Mitis group, Streptococcus pneumoniae and Streptococcus mitis are closely related species, making discrimination between them very difficult [1]. Although both bacteria are oral commensals they can cause a wide variety of human invasive diseases [2]. S. pneumoniae (pneumococcus) is the most common cause of community-acquired pneumonia worldwide and is also associated with a range of other diseases, including otitis media, meningitis, and septicemia [3]. S. mitis has traditionally been regarded as an innocuous commensal of the oropharynx, skin, and both the gastrointestinal and genitourinary tracts [4]. Some S. mitis strains have been shown to cause endocarditis and blood stream infections [5]. The transition from commensalism to pathogenesis is likely related to the acquisition of virulence genes.
S. pneumoniae and S. mitis have emerged as significant pathogens but differ in their expression of virulence factors. For example, phase variation is an important step in virulence and also an adaptive process that leads to the distribution of bacteria to other sites, causing disease [6]. The switching of phenotypes was noted in S. pneumoniae where phase variation changes the colony morphology from opaque to transparent without any change in the serotype. To our knowledge, this type of phase variation has not been observed for S. mitis [7], however, strains of S. mitis were recently shown to have a capsule, a well known virulence factor in S. pneumoniae [8]. In fact, genomic analysis of S. mitis revealed the presence of several virulence factors similar to those found in S. pneumoniae. However, it has not been confirmed whether these virulence factors are just implicated in adhesion and attachment of S. mitis or whether they are related to pathogenicity as in S. pneumoniae [5,9].
Strains nonsusceptible to the common antimicrobial drugs were detected among S. pneumoniae and S. mitis, especially to beta-lactams which have been widely used to treat such bacterial infections [10]. It was also reported for S. pneumoniae and other bacterial species that low concentrations of some antibiotics induces natural transformation and mutagenesis [11,12,13]. The ubiquitous nature of antibiotic resistance genes may also be due to horizontal gene transfer among strains of the naturally transformable Mitis group. Therefore, there is pressure to develop novel antibacterial alternatives.
Virulent phages may represent such an alternative strategy to combat antibiotic-resistant bacteria. Phages are recognized as the most abundant biological entities in the biosphere [14]. The study of phages of hemolytic streptococci began decades ago [15], and the vast majority of phages currently isolated from S. mitis and S. pneumoniae are temperate phages. In fact, both bacterial species contain many prophages in their genomes [16,17]. Prophage carriage was identified in clinical isolates of S. pneumoniae by hybridation and also via induction by mitomycin C [16,17]. At least seven phage-related gene clusters were detected in the genome of S. mitis B6 and two complete prophages (SM1 and phiB6) were isolated and sequenced [18,19]. Because temperate phages have the ability to transfer host DNA, which may encode virulence genes or toxins, into other bacterial strains [18,20], virulent phages are thought to be better suited for biocontrol purposes.
Very few lytic phages have been isolated for either of these two bacterial species. Despite the isolation of pneumophages, also called Omega phages [21], only two virulent pneumococcus phages are readily available today. Phage Dp-1 was the first virulent pneumophage isolated in 1975 [21,22] and belongs to the Siphoviridae family. Phage Cp-1 was isolated in 1981 [23] and is a member of the Picovirinae subfamily of the Podoviridae family, with a linear double-stranded DNA genome [24]. One virulent phage of S. mitis, vB_SmM_GEC-SmitisM_2, was isolated in 2012 from sewage water and belongs to the Myoviridae family [25].
Of interest, enzymes from virulent pneumococcal phages have also shown promise as antimicrobials [26,27,28,29,30,31,32]. At the end of their lytic cycle, virulent phages produce an enzyme (endolysin or lysine) that degrades the bacterial peptidoglycan to release new virions. A number of studies have demonstrated the potential of the lysin [Cpl-1] from phage Cp-1 to eradicate nasopharyngeal colonization and bacteremia [28], and to prevent otitis media [30]. The administration of Cpl-1 by inhalation [27] or by repetitive intraperitoneal injections even rescued mice from severe pneumococcal pneumonia [32].
In this study, we show that the virulent pneumophages Dp-1 and Cp-1 can infect S. mitis. Microbiological assays and genomic analyses were performed to compare phage behavior in both bacterial species.
Materials and Methods
Bacterial strains and culture conditions
The unencapsulated strain S. pneumoniae R6 (host of phage Cp-1), a derivative of S. pneumoniae strain R36A [host strain of phage Dp-1], was grown on TSA (Trypticase Soy Agar) containing 5% sheep’s blood at 37°C in the presence of 5% CO2. Single colonies were suspended in filtered BHI (Brain heart infusion) broth containing 0.5% yeast extract and incubated at 37°C in the presence of 5% CO2. S. mitis CCRI-15019 was grown at 30°C in BHI supplemented with 0.2 mM magnesium sulfate and 0.25 mM calcium chloride to prevent cell aggregation. The bacterial strains are stored at the Félix d’Hérelle Reference Center for Bacterial Viruses (www.phage.ulaval.ca).
Bacterial species identification
The bacterial housekeeping genes recA, recP, HexB, and xpt were amplified by PCR using the primers listed in S1 Table [22]. The PCR products were sequenced by the Plateforme de Séquençage et de Génotypage des Génomes service at the CHUL/CHUQ Research Center using the ABI data 3730XL DNA analyzer. Both DNA strands of the amplicons were sequenced using the same primer pairs used for PCR amplification. Sequences were aligned and analysed using the bioinformatics tools (Clustal W2 and BioEdit).
Phages
Pneumophages Cp-1 [23] and Dp-1 [22] were obtained from the Félix d’Hérelle Reference Center for Bacterial Viruses. For phage amplification, and to facilitate enumeration, we used liquid BHI+ medium, which consisted of BHI supplemented with 8 μM MnCl2, 0.25 mM CaCl2, 0.2 mM MgSO4, 50 Mm Tris-HCl pH 7.5, 50 ng/μl choline chloride, 0.4% glycine, and 100 μl/ml catalase. Amplifications of phage Cp-1 on S. pneumoniae and on S. mitis were performed with agitation, as follows: a single colony, isolated from overnight culture on BHI blood agar, was used for cultivation in BHI. After overnight growth of the host strains an aliquot of the culture was transferred into fresh BHI and incubated until it reached an optical density at 600 nm (OD600nm) of 0.06–0.08. The culture was diluted with an equal volume of BHI+, phages were added and incubated overnight at 30°C. Phage titers were obtained using a standard, double-layer agar assay method. To maximize plaque visualization, the bottom layer of BHI+ contained 1.5% agarose while the top agar contained 0.4% agarose.
Microbiological assays
Phage lytic development was assessed using a one-step growth curve assay, in triplicate, as described elsewhere [33]. After overnight growth of the host strain in BHI, an aliquot of the culture was transferred into fresh BHI and incubated until it reached an OD600nm of 0.06–0.08. The bacterial culture was diluted 1:3 in BHI+ and then infected at a multiplicity of infection of 0.05 at 30°C. Phages were allowed to adsorb to the host cells for 10 min. Unadsorbed phages were removed by centrifugation, the bacterial pellet was washed twice with BHI media and then we proceeded as described elsewhere [33]. The plates were incubated at 30°C overnight with 5% CO2, and the plaque forming units (PFU) were counted. The burst size was determined by calculating the ratio of the average phage titer after the exponential phase to the average titer before the infected cells began to release virions [33]. Phage adsorption tests were also carried out on S. pneumoniae R6 and S. mitis CCRI-15019, in triplicate, essentially as previously reported [34]. Modifications: BHI+ broth was used, CaCl2 was not added again at phage infection and the incubation was carried out at 30°C for 10 min.
Electron microscopy
Phage preparations produced on S. pneumoniae and S. mitis were purified using a CsCl gradient, as previously described [35]. Phages were then centrifuged and 100 μl of the pellet were kept and washed with 1.5 ml of ammonium acetate (0.1 M, pH 7.5). This process was repeated twice and 100 μl from the final wash was retained for observation by transmission electron microscopy. Grid preparation and observation were performed as previously described [36]. Phages were observed at 80 kV using a JEOL 1230 transmission electron microscope.
Phage DNA preparation and sequencing
Genomic DNAs of phages Cp-1 and Dp-1 amplified on S. mitis CCRI-15019 were isolated using a Lambda Maxi Kit (Qiagen). Phage Cp-1 DNA was also isolated after propagation on S. pneumoniae R6. Genome sequencing was performed on a 454 FLX instrument at the Plateforme d’Analyses Génomiques of the Université Laval (IBIS). The genomic sequences were completed by primer walking (primer sequences are listed in S2 Table) and by sequencing of PCR products. All mutations were also confirmed by primer walking.
Phage genome analyses
Genomic sequences were analyzed using BioEdit 7.2.0 (http://www.mbio.ncsu.edu/bioedit/bioedit.html) and the Staden package [37,38] (http://staden.sourceforge.net/). Sequence alignments were performed using BioEdit and Clustal W2 software (http://www.ebi.ac.uk/Tools/msa/clustalw2/). Open reading frames [ORFs] were identified using GenMark (http://exon.gatech.edu/) and ORFinder (http://www.ncbi.nlm.nih.gov/projects/gorf/). Sequences were considered to be ORFs if they showed a putative ribosome binding site (RBS) at a reasonable distance from the starting codon (AUG, UUG, or GUG) and they consisted of at least 29 amino acids (aa). Function was attributed to an ORF by comparing the translated product to proteins available at the National Center for Biotechnology Information (BLASTp, http://blast.ncbi.nlm.nih.gov/Blast.cgi). The annotations were reinforced by searching for protein functional domains using the NCBI Conserved Domain Database (http://www.ncbi.nlm.nih.gov/Structure/cdd/wrpsb.cgi) and EMBL InterProScan (http://www.ebi.ac.uk/Tools/InterProScan/). The theoretical molecular masses [MM] and isoelectric points [pI] of each deduced phage protein were determined using the ProtParam software tool available on the bioinformatics resource portal ExPASy Web site (http://ca.expasy.org/tools/protparam.html). The genomes of phages Cp-1 and Dp-1 were searched for tRNAs using tRNAscan-SE [39] and BLASTn from NCBI. Bacterial codon usage for the host strains was obtained from the Kazusa DNA Research Institute database (http://www.kazusa.or.jp/codon/) while codon usage for the phages was determined using the DNA 2.0 web server (Menlo Park, CA); the frequency per thousand codons was then calculated.
The complete genome sequence of phage SOCP has been deposited in GenBank under accession number KJ617393.
Results
Speciation of bacterial hosts
The species identification of S. mitis from the closely related S. pneumoniae represents a challenge. For example, significant sequence conservation of the 16S rRNA gene sequence within the Mitis group limits the use of these sequences for species differentiation [40]. To confirm the bacterial strains used in this study, degenerate primers were used and the PCR products of four housekeeping genes, recA, recP, hex B and xpt (S1 Table) [40] were amplified and sequenced. Our results confirmed that the isolate CCRI-15019 is highly related to S. mitis B6 [18]. Our S. pneumoniae R6 and R36A strains were similarly confirmed.
Morphological analysis of phages Dp-1 and SOCP
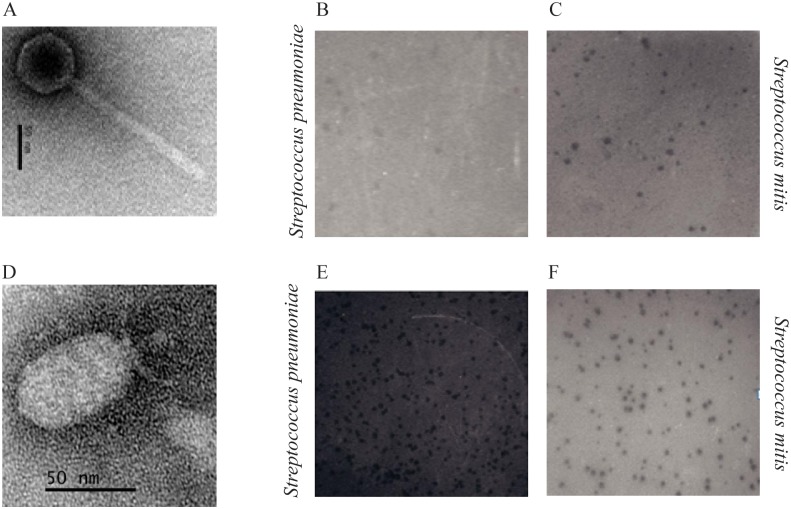
As documented previously [40], phage Dp-1 belongs to the Siphoviridae family. It has an icosahedral capsid with an estimated diameter of 69.8 ± 1.2 nm (Fig. 1A) and a long non-contractile tail of 169.9 ± 3.6 nm in length and 19.6 ± 2 nm in width. Phage Cp-1, used in this study and stored at the d’Hérelle Center, was re-named SOCP due to genome variations (see below). Phage SOCP belongs to the Podoviridae family and has a hexagonal capsid of 65.8 ± 1.1 nm (top to bottom) and 42.1 ± 1.7 nm in width (Fig. 1D). This phage has a short non-contractile tail, 19.3 ± 1 nm in length and 7.5 ± 1.2 nm in width. Observations of phages Dp-1 and SOCP, amplified on both bacterial species, confirmed that the general morphology of these virions was not affected by growth in either hosts.
Fig 1. Electron microscopy of virulent phage Dp-1 (A) and phage SOCP (D).
Scale bars correspond to 50 nm. Photographic images (B, C, E, F) show plaques of phages Dp-1 and SOCP propagation in media containing agarose. Plaques produced by phage Dp-1 on strains S pneumoniae R6 (B) and S. mitis CCRI-15019 (C). Plaques produced by phage SOPC on strains S pneumoniae R6 (E) and S. mitis CCRI-15019 (F).
Microbiological assays
One of the great difficulties of working with virulent pneumophages is the ability to visualize plaques consistently. We were able to observe plaques for both phages using BHI+ media (Figs. 1B & E). We also noticed that liquid cultures of S. pneumoniae grew better in BHI+ when started from colonies grown on blood agar. Finally, replacing agar by agarose in both top and bottom media led to an improvement in the plaque size and visibility.
The availability of an improved plaque assay allowed us to investigate the host range of phages Dp-1 and SOCP. Interestingly, we observed that they could both replicate on a S. mitis strain (CCRI-15019). Moreover, even larger phage plaques were obtained on S. mitis, compared to S. pneumoniae host cells grown under the same conditions (Figs. 1BC & EF). To further investigate the behavior of the two phages on both bacterial species, one-step growth curve assays were performed using S. pneumoniae R6 and S. mitis CCRI-15019. The latent period of phage Dp-1 was calculated to be 71 ± 4 min when amplified on S. pneumoniae and 59 ± 4 min on S. mitis. The burst sizes were 73 ± 6 plaque-forming units (PFU) per infected cell and 63 ± 6 PFU for S. pneumoniae and S. mitis, respectively. Similarly, the latent period of phage SOCP was estimated to be 78 ± 2 min on S. pneumoniae and 66 ± 5 min on S. mitis, while the burst size was 94 ± 4 PFU on its pneumococcal host and 53 ± 4 PFU on S. mitis. These data indicated a lower burst size for both phages on S. mitis cells but a shorter latent period.
Adsorption to the cell surface was also evaluated for the two phages on both strains. Under the conditions tested, the percentage of adsorption of phage Dp-1 on S. pneumoniae R6 was 95% ± 1.8% and was 79% ±1% on S. mitis. The adsorption of phage SOCP was 94% ± 0.6% on S. pneumoniae R6 and 86 ± 1.3% on S. mitis B6. Thus, both pneumophages could also readily adsorb to the S. mitis cell surface.
The efficacy of plaquing (EOP) of both phages on the two propagating hosts was determined. When phages Dp-1 and SOCP were amplified on their S. pneumoniae hosts they had EOPs of 10–1 and 10–4 on S. mitis, respectively. Similarly, when Dp-1 and SOPC were amplified on S. mitis, their EOPs on S. pneumoniae were 10–1 and 10–3, respectively. These data suggest the presence of host factors that modify the phage behavior.
Genome analysis
To determine if replicating these phages on various hosts had an impact at the nucleotide level, we determined the complete genome sequence of both phages after amplification on S. pneumoniae or S. mitis. The double-stranded DNA (dsDNA) genome of phage Dp-1 is made of 56,506 bp. The analysis of the sequence found no nucleotide variation compared to the genomic sequence recently reported for Dp-1 [41]. Moreover, the sequence was identical when Dp-1 was amplified on both S. pneumoniae and S. mitis hosts, indicating that propagating this siphophage on two distinct streptococcal species did not lead to genomic changes.
Similarly, the genome of the podophage was also identical when propagated on either S. pneumoniae or S. mitis. However, analysis of the genomic sequence of the phage Cp-1 used in this study showed variations compared to the GenBank sequence no. NC_001825.1. As indicated above, we thus renamed our Cp-1-like phage SOCP due to these differences. The dsDNA genome of SOCP is 19,347 bp long, while the reported genome of phage Cp-1 is 19,343 bp. Comparative analyses revealed 31 variations in the genome of SOCP as compared to Cp-1 (S3 Table). These differences were confirmed through primer walking directly on the phage genome.
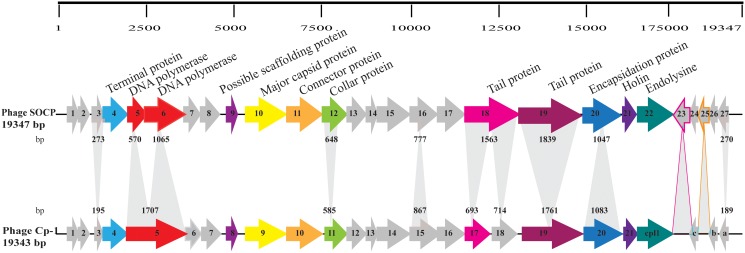
The genome of phage SOCP has a GC content of 38.8%. It has 27 open reading frames, each preceded by a putative ribosome-binding site (RBS) (Table 1). Putative functions could be attributed to only 12 ORFs (44%). Interestingly, we found two additional ORFs in SOCP as compared to Cp-1, namely ORF23 and ORF25 (Fig. 2). Of interest were also the products of genes orf5 and orf6, which likely code for DNA polymerase subunits [42,43], whereas only one (orf5) was found in Cp-1. Conversely in the case of orf18, one gene was found in SOCP whereas it was split into two genes (orf17 and orf18) in Cp-1. The major capsid protein ORF10 was also affected by mutations, although its size remained the same (S3 Table). Other notable ORFs containing mutations included the tail protein ORF19, the collar protein ORF12, as well as ORF4, ORF9, ORF12, ORF16, ORF23, ORF25, and ORF27.
Table 1. Putative Open Reading Frames deduced from SOCP genome sequences and their predicted functions.
| ORF | Start | End | Strand | Length [aa] a | IP b | Mw [kDa] c | Putative RBS d and start codon | Putative function | Best hit with Blast ‘Locus tag’ | ORF in Cp-1 | # of identical aa/ size of the alignment [% aa identity] | Length [aa] | E-value | Accession number [GenBank] e |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 376 | 642 | + | 88 | 4.4 | 10.4 | AAAGGAGAAAGAAAACATG | Hypothetical protein | Cp-1, p01 | 1 | 88/88[100%] | 88 | 3E-57 | NP_044813.1 |
| 2 | 657 | 947 | + | 96 | 6.6 | 11.7 | AAAGGAGATAATAAAAATG | Hypothetical protein | Cp-1, p02 | 2 | 96/96[100%] | 96 | 5E-61 | NP_044814.1 |
| 3 | 1074 | 1346 | + | 90 | 4.7 | 10.5 | AAAGGAGTAAAAGCACTTG | Hypothetical protein | Cp-1, p03 | 3 | 63/64[98%] | 64 | 3E-36 | NP_044815.1 |
| 4 | 1351 | 2043 | + | 230 | 10.1 | 26.7 | AAGGGGTGTAATTAAATG | Terminal protein | Cp-1, p04 | 4 | 229/230[99%] | 230 | 7E-165 | NP_044816.1 |
| 5 | 2040 | 2609 | + | 189 | 4.6 | 22.1 | AAAGAAGCGAGGGAAGAAGTG | DNA polymerase | Cp-1, p05 | 5 | 178/179[99%] | 568 | 3E-123 | NP_044817.1 |
| 6 | 2681 | 3745 | + | 354 | 6.8 | 40.8 | AATCTTAGATGAAAAGGTG | DNA polymerase | Cp-1, p05 | 5 | 341/354[96%] | 568 | 0 | NP_044817.1 |
| 7 | 3702 | 4148 | + | 148 | 9.2 | 17.6 | AAAGGGGGTACGCTGATTTATG | Hypothetical protein | Cp-1, p06 | 6 | 148/148[100%] | 148 | 1E-100 | NP_044818.1| |
| 8 | 4141 | 4653 | + | 170 | 4.8 | 18.9 | AAACGGAGATAAACAAAATG | Hypothetical protein | Cp-1, p07 | 7 | 170/170[100%] | 170 | 5E-118 | NP_044819.1 |
| 9 | 4875 | 5165 | + | 96 | 4.2 | 10.5 | AAAGGAGAGGGCTATG | Scaffolding protein | Cp-1, p08 | 8 | 95/96[99%] | 96 | 4E-59 | NP_044820.1 |
| 10 | 5409 | 6506 | + | 365 | 5.4 | 41.7 | AAGAGGGAGAAGAATAGAATG | Major head protein | Cp-1, p09 | 9 | 352/365[96%] | 365 | 0 | NP_044821.1 |
| 11 | 6563 | 7576 | + | 337 | 5.3 | 39.5 | AAAGGGGACTAAATG | Connector protein | Cp-1, p11 | 10 | 337/337[100%] | 337 | 0 | NP_044823.1 |
| 12 | 7563 | 8210 | + | 215 | 5.1 | 24.7 | AAAAGGAGGGGACAATCATTG | Collar protein | Cp-1, p12 | 11 | 192/194[99%] | 194 | 2E-137 | NP_044824.1 |
| 13 | 8223 | 8807 | + | 194 | 8.6 | 22.8 | AAAGGTGTATAGATG | Hypothetical protein | Cp-1, p13 | 12 | 194/194[100%] | 194 | 5E-140 | NP_044825.1 |
| 14 | 8804 | 9118 | + | 104 | 5.8 | 11.9 | AAAGAGGACATGAAAACCTATG | Hypothetical protein | Cp-1, p14 | 13 | 104/104[100%] | 104 | 7E-67 | NP_044826.1 |
| 15 | 9102 | 9989 | + | 295 | 4.9 | 32.9 | AAAAAGAGGTAGAAACAAATG | Hypothetical protein | Cp-1, p15 | 14 | 295/295[100%] | 295 | 0 | NP_044827.1 |
| 16 | 10011 | 10787 | + | 258 | 5.0 | 29.4 | AAAGGATTTTAAAACATG | Hypothetical protein | Cp-1, p16 | 15 | 192/207[93%] | 288 | 4E-132 | NP_044828.1 |
| 17 | 10787 | 11548 | + | 253 | 6.0 | 28.4 | AGGAGGTATCTAATG | Hypothetical protein | Cp-1, p18 | 16 | 253/253[100%] | 253 | 0 | NP_044830.1 |
| 18 | 11515 | 13077 | + | 520 | 5.7 | 59.0 | AAAGTCGGGTCAATG | Tail protein | Cp-1, p19 / Cp-1, p20 | 17 18 | 210/224[94%]/ 236/237[99%] | 230 /237 | 6e-149/ 2E-164 | NP_044831.1 / NP_044832.1 |
| 19 | 13081 | 14919 | + | 612 | 4.8 | 67.5 | AAAGGGTAAACAATG | Tail protein | Cp-1, p21 | 19 | 582/583[99%] | 586 | 0 | NP_044833.1 |
| 20 | 14993 | 16039 | + | 348 | 7.6 | 40.8 | AAATGGTACAATCCGCAGAAAATG | Encapsidation protein | Cp-1, p23 | 20 | 348/348[100%] | 360 | 0 | NP_044835.1 |
| 21 | 16029 | 16433 | + | 134 | 7.9 | 15.5 | AGGTTATCAATCATG | Holin protein | Cp-1, p24 | 21 | 134/134[100%] | 134 | 1E-89 | NP_044836.1 |
| 22 | 16433 | 17452 | + | 339 | 4.6 | 39.2 | AAAGGAGAAAAGAAATAATG | Lysozyme | Cp-1, p25 | 22 | 339/339[100%] | 339 | 0 | NP_044837.1 |
| 23 | 17480 | 17896 | - | 139 | 5.62 | 15.8 | AAAACGTAGGGGGTTAATACTATG | Hypothetical protein | SP058_00395 | 24/65[37%] | 234 | 6E+00 | YP_008239483.1 | |
| 24 | 17901 | 18143 | - | 80 | 9.9 | 9.4 | AAATTGAGGTATTAAGAAAATG | Hypothetical protein | Cp-1, p26 [orfc] | c | 80/80[100%] | 80 | 5E-50 | NP_044838.1 |
| 25 | 18148 | 18423 | - | 91 | 5.1 | 10.9 | AAGGGACGGTTACTAGATG | Hypothetical protein | AGR66263 | 14/44[32%] | 410 | 8E-01 | gb|AGR66263.1 | |
| 26 | 18424 | 18693 | - | 89 | 7.7 | 10.8 | ACAAATAGGAGGGTAAACATG | Hypothetical protein | Cp-1, p27[orfb] | b | 89/89[100%] | 89 | 5E-58 | NP_044839.1 |
| 27 | 18704 | 18973 | - | 89 | 5.0 | 10.2 | AAAGAGGTATAACAAAATG | Hypothetical protein | Cp-1, p28 [orfa] | a | 60/61[98%] | 62 | 7E-35 | NP_044840.1 |
a Number of amino acids (aa),
b IP, isoelectric point and
c MM, molecular mass.
d RBS, ribosomal binding site. Bases in bold correspond to nucleotides identical to the RBS consensus; lowercase indicates.
Fig 2. Genome alignment of phages SOCP and Cp-1.
The scale above the phage genome SOCP is in base pairs. Each arrow represents a gene, and the numbering for SOCP refers to Table 1. Some putative functions of the deduced proteins are indicated above the arrows (see Table 1 for details). Grey arrows indicate that no putative function was attributed to the deduced protein. Arrows with the same color indicate the same general function and have at least 90% identity at the amino acid level. Heterologous regions are shaded gray, and the shaded numbers indicate the number of base pairs between the corresponding gene sequences. Shadows light with colored contour highlight ORFs not found in the genome of phage Cp-1.
Three open reading frames were identified on the negative strand of the SOCP genome, specifically within three other ORFs (major capsid protein, tail protein and one hypothetical protein). These ORFs were not included in the annotation of the phage genome since no BLAST data support these proteins as valid protein products.
Codon usage
No tRNAs were found in either of the two pneumophages. Still, the codon usage frequency was investigated for the phage genomes and compared with the codon usage of S. pneumoniae and S. mitis (S4 Table). The codon usage of pneumophages mostly corresponds to the codons most frequently used by these two bacteria, although the codon usage of the phages was closer to S. pneumoniae, suggesting that both phages are mode adapted to this bacterial species. In a few cases, some codons were over-represented in the phages as compared to the two bacterial hosts, likely to favor phage multiplication (S4 Table).
Comparative genomics
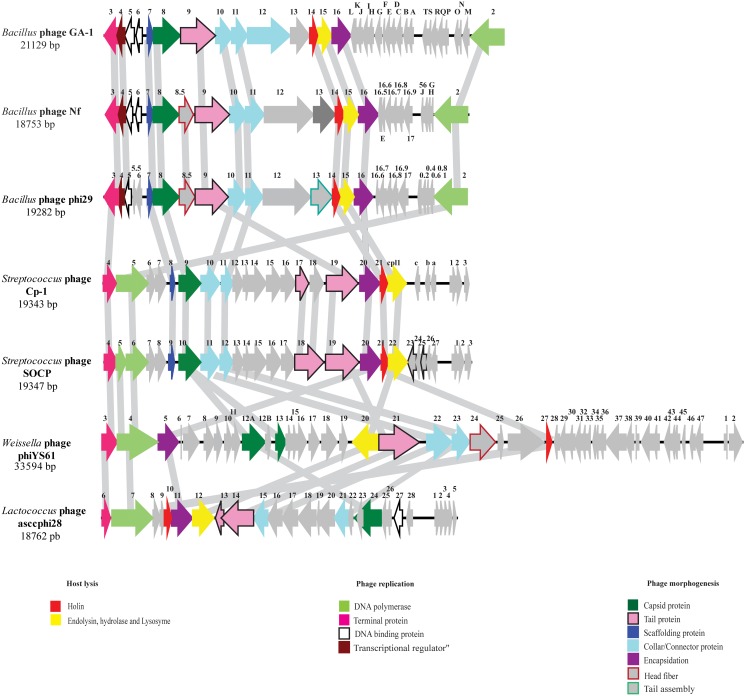
Protein-primed DNA replication was reported for phage Cp-1 [44]. Few other phages of the Podoviridae family replicate using this mechanism of DNA replication [44,45,46] and, in general, initiation of replication arises at the 3’ nucleotide of the DNA [44]. The genomes of phages SOCP and Cp-1 were aligned with the genomes of five phages infecting other Gram-positive bacteria, namely Bacillus subtilis phage phi29, Lactococcus lactis phage asccphi28, Weissella cibaria phage phiYS6 as well as Bacillus sp. phages GA-1 and Nf (Fig. 3). The genome organization of the two pneumophages is somewhat different from the other phages due to alternate orientations of some genes, although a few annotated proteins are related (Fig. 3). The genes coding for the DNA polymerase and terminal proteins are on the positive strand in one group (phage Cp-1, SOCP, phiYS61 and asccphi28) and on the opposite strand for another group (phage GA-1, Nf and phi29). Moreover, the genes for structural proteins in the lactococcal phage asccphi28 are in the opposite direction, compared to the other podophages shown in Fig. 3. Overall, a low level of identity was found between phages Cp-1/SOCP and these podophages, which is likely due to their distinct ecological niches and host strains.
Fig 3. Comparison of the proteome of pneumophage SOCP/ Cp-1 with other related phages replicating through a protein priming DNA replication system.
Phage genome sequences were downloaded from GenBank, aligned in BioEdit and each deduced protein was compared using BioEdit and protein BLAST. Arrows of the same color correspond to ORFs with the same general function.
Discussion
S. mitis is a species closely related to S. pneumoniae that colonizes the human oral cavity. Both species have emerged as multidrug-resistant pathogens due to their ability to acquire foreign DNA by natural competence. The genome of S. mitis has significant similarity to the genome of S. pneumoniae and shares a core of 900 genes [18]. Since the publication of the S. mitis B6 genome, studies have been carried out to understand this relationship and a number of studies support the hypothesis of evolution of S. pneumoniae from S. mitis by acquisition of virulence factors and numerous sugar-related transport systems [18,47]. Other studies have proposed that another possible concept is the evolution from a pathogenic bacterium, S. pneumoniae, to a commensal, S. mitis, through loss of virulence genes [18,40]. Virulence genes could also have been acquired through horizontal gene transfer between other related species [48]. Many virulence factors are cell surface proteins that play a role in the interaction with host cells [49]. Other pneumococcal cell surface components such as choline-containing teichoic acid, are components of the Dp-1 phage receptors [50].
Here, we report that two pneumophages can efficiently replicate on a S. mitis strain. These two virulent phages were initially isolated from throat swabs of patients with upper respiratory infections—the natural habitat of S. mitis. The ability of phage Dp-1 to infect S. mitis may be related to the choline-binding proteins found in S. mitis [50]. Homologues of pneumococcal surface choline-binding proteins are present in S. mitis but their role in this bacterium remains unknown [5]. The host autolysin system, involved in pneumophage virion release [51], is also found in both S. pneumoniae and S. mitis [52]. The adsorption of phages Dp-1 and SOCP was slightly higher on the S. pneumoniae host compared to S. mitis and this may be due to the availability of phage receptors on the cell surface or differences in receptor sequences. It was previously reported that phage Cp-1 adsorbed very poorly to the host cell surface [52]. Phage SOPC adsorbed very well to its host as well as the S. mitis strain. This could be due to the mutations observed in the genome of SOCP or the experimental conditions used in our study.
The burst size and latent period reported here are rather different from previous studies for both pneumophages [23,53]. Again, this could be due to the difference in experimental conditions and media used. For phage Dp-1, the host bacterial strain used by Lopez et al. [53] was S. pneumoniae R36A and in our study we used the S. pneumoniae R6, a derivative of R36A. Likewise for phage SOCP, its burst size was much higher than reported for Cp-1 [41]. It is not known if this difference is due to the experimental conditions or the genomic variations. Of note, it was previously reported that phage Cp-1 can infect some Streptococcus oralis strains [54]. SOCP can also infect a few S. oralis strains (data not shown).
In addition to the observations that pneumophages can replicate on S. mitis, the other most striking finding was the difference (0.16%) in the genome sequences between SOCP and Cp-1. The nature of such discrepancies remains unclear. Phage SOCP was retrieved from the Félix d’Hérelle Reference Center for Bacterial Viruses and was initially believed to be Cp-1. Either sequencing errors occurred in the original deposited sequence (GenBank no. Z47794) or a very efficient pneumophage was recovered. The latter could be due to phage host-adaptation, giving SOCP the ability to efficiently infect its hosts [55]. It has been reported that viral adaptation occurs through numerous mutations in the genome at low frequency that increases fitness of the phage [55,56]. It will thus be interesting to assess whether some of the nucleotide variations detected in SOCP are enabling such increased fitness.
This study on virulent phages provides another example of the relatedness of S. pneumonia and S. mitis. Both species also carry numerous temperate phages in their genomes that are probably involved in their evolution. Further study is needed to identify most of the hypothetical genes in phage SOCP as well as to increase our understanding of phage-host interactions [57], with a goal of eventually using virulent streptococcal phages in medical applications.
Supporting Information
F, forward; R, reverse.
(DOCX)
F, forward; R, reverse.
(DOCX)
a relative to the genome of phage Cp-1.—absence of the nucleotide.
(DOCX)
The values represent the frequency of codon usage per thousand. The phage preferentially used codons for each amino acid are displayed in bold.
(DOCX)
Acknowledgments
We are grateful to M. Boissinot for the Streptococcus mitis strain CCRI-15019 and to D. Tremblay for electron microscopy.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by an Emerging Team Grant from the Canadian Institutes of Health Research (CIHR). S.O. is the recipient of a scholarship from the Programme Canadien de Bourse de la Francophonie (PCBF) and (CIHR). S.M. holds a Tier 1 Canada Research Chair in Bacteriophages. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Arbique JC, Poyart C, Trieu-Cuot P, Quesne G, Carvalho Mda G, et al. (2004) Accuracy of phenotypic and genotypic testing for identification of Streptococcus pneumoniae and description of Streptococcus pseudopneumoniae sp. nov. J Clin Microbiol 42: 4686–4696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doern CD, Burnham CA (2010) It’s not easy being green: the viridans group streptococci, with a focus on pediatric clinical manifestations. J Clin Microbiol 48: 3829–3835. 10.1128/JCM.01563-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Joyce EA, Popper SJ, Falkow S (2009) Streptococcus pneumoniae nasopharyngeal colonization induces type I interferons and interferon-induced gene expression. BMC Genomics 10: 404 10.1186/1471-2164-10-404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carrascosa M, Perez-Castrillon JL, Sampedro I, Valle R, Cillero L, et al. (1994) Lung abscess due to Streptococcus mitis: case report and review. Clin Infect Dis 19: 781–783. [DOI] [PubMed] [Google Scholar]
- 5. Mitchell J (2011) Streptococcus mitis: walking the line between commensalism and pathogenesis. Mol Oral Microbiol 26: 89–98. 10.1111/j.2041-1014.2010.00601.x [DOI] [PubMed] [Google Scholar]
- 6. Donkor ES (2013) Understanding the pneumococcus: transmission and evolution. Front Cell Infect Microbiol 3: 7 10.3389/fcimb.2013.00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arai J, Hotomi M, Hollingshead SK, Ueno Y, Briles DE, et al. (2011) Streptococcus pneumoniae isolates from middle ear fluid and nasopharynx of children with acute otitis media exhibit phase variation. J Clin Microbiol 49: 1646–1649. 10.1128/JCM.01990-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rukke HV, Hegna IK, Petersen FC (2012) Identification of a functional capsule locus in Streptococcus mitis . Mol Oral Microbiol 27: 95–108. 10.1111/j.2041-1014.2011.00635.x [DOI] [PubMed] [Google Scholar]
- 9. Madhour A, Maurer P, Hakenbeck R (2011) Cell surface proteins in S. pneumoniae, S. mitis and S. oralis . Iran J Microbiol 3: 58–67. [PMC free article] [PubMed] [Google Scholar]
- 10. Sunderkotter C, Becker K (2014) Systemic therapy with antibiotics: Overview of important antibiotics in dermatology. Hautarzt 65: 113–124. 10.1007/s00105-013-2743-6 [DOI] [PubMed] [Google Scholar]
- 11. Gutierrez A, Laureti L, Crussard S, Abida H, Rodriguez-Rojas A, et al. (2013) beta-Lactam antibiotics promote bacterial mutagenesis via an RpoS-mediated reduction in replication fidelity. Nat Commun 4: 1610 10.1038/ncomms2607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Henderson-Begg SK, Livermore DM, Hall LM (2006) Effect of subinhibitory concentrations of antibiotics on mutation frequency in Streptococcus pneumoniae . J Antimicrob Chemother 57: 849–854. [DOI] [PubMed] [Google Scholar]
- 13. Prudhomme M, Attaiech L, Sanchez G, Martin B, Claverys JP (2006) Antibiotic stress induces genetic transformability in the human pathogen Streptococcus pneumoniae . Science 313: 89–92. [DOI] [PubMed] [Google Scholar]
- 14. Serwer P, Hayes SJ, Thomas JA, Hardies SC (2007) Propagating the missing bacteriophages: a large bacteriophage in a new class. Virol J 4: 21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krause RM (1957) Studies on bacteriophages of hemolytic streptococci. I. Factors influencing the interaction of phage and susceptible host cell. J Exp Med 106: 365–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ramirez M, Severina E, Tomasz A (1999) A high incidence of prophage carriage among natural isolates of Streptococcus pneumoniae . J Bacteriol 181: 3618–3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Romero P, Croucher NJ, Hiller NL, Hu FZ, Ehrlich GD, et al. (2009) Comparative genomic analysis of ten Streptococcus pneumoniae temperate bacteriophages. J Bacteriol 191: 4854–4862. 10.1128/JB.01272-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Denapaite D, Bruckner R, Nuhn M, Reichmann P, Henrich B, et al. (2010) The genome of Streptococcus mitis B6—what is a commensal? PLoS One 5: e9426 10.1371/journal.pone.0009426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Siboo IR, Bensing BA, Sullam PM (2003) Genomic organization and molecular characterization of SM1, a temperate bacteriophage of Streptococcus mitis . J Bacteriol 185: 6968–6975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gindreau E, Lopez R, Garcia P (2000) MM1, a temperate bacteriophage of the type 23F Spanish/USA multiresistant epidemic clone of Streptococcus pneumoniae: structural analysis of the site-specific integration system. J Virol 74: 7803–7813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tiraby JG, Tiraby E, Fox MS (1975) Pneumococcal bacteriophages. Virology 68: 566–569. [DOI] [PubMed] [Google Scholar]
- 22. McDonnell M, Lain R, Tomasz A (1975) "Diplophage": a bacteriophage of Diplococcus pneumoniae . Virology 63: 577–582. [DOI] [PubMed] [Google Scholar]
- 23. Ronda C, Lopez R, Garcia E (1981) Isolation and characterization of a new bacteriophage, Cp-1, infecting Streptococcus pneumoniae . J Virol 40: 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martin AC, Lopez R, Garcia P (1998) Pneumococcal bacteriophage Cp-1 encodes its own protease essential for phage maturation. J Virol 72: 3491–3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rigvava S, Tchgkonia I, Jgenti D, Dvalidze T, Carpino J, et al. (2013) Comparative analysis of the biological and physical properties of Enterococcus faecalis bacteriophage vB_EfaS_GEC-EfS_3 and Streptococcus mitis bacteriophage vB_SmM_GEC-SmitisM_2. Can J Microbiol 59: 18–21. 10.1139/cjm-2012-0385 [DOI] [PubMed] [Google Scholar]
- 26. Djurkovic S, Loeffler JM, Fischetti VA (2005) Synergistic killing of Streptococcus pneumoniae with the bacteriophage lytic enzyme Cpl-1 and penicillin or gentamicin depends on the level of penicillin resistance. Antimicrob Agents Chemother 49: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Doehn JM, Fischer K, Reppe K, Gutbier B, Tschernig T, et al. (2013) Delivery of the endolysin Cpl-1 by inhalation rescues mice with fatal pneumococcal pneumonia. J Antimicrob Chemother 68: 2111–2117. 10.1093/jac/dkt131 [DOI] [PubMed] [Google Scholar]
- 28. Loeffler JM, Djurkovic S, Fischetti VA (2003) Phage lytic enzyme Cpl-1 as a novel antimicrobial for pneumococcal bacteremia. Infect Immun 71: 6199–6204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Loeffler JM, Fischetti VA (2003) Synergistic lethal effect of a combination of phage lytic enzymes with different activities on penicillin-sensitive and-resistant Streptococcus pneumoniae strains. Antimicrob Agents Chemother 47: 375–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCullers JA, Karlstrom A, Iverson AR, Loeffler JM, Fischetti VA (2007) Novel strategy to prevent otitis media caused by colonizing Streptococcus pneumoniae . PLoS Pathog 3: e28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nelson D, Loomis L, Fischetti VA (2001) Prevention and elimination of upper respiratory colonization of mice by group A streptococci by using a bacteriophage lytic enzyme. Proc Natl Acad Sci U S A 98: 4107–4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Witzenrath M, Schmeck B, Doehn JM, Tschernig T, Zahlten J, et al. (2009) Systemic use of the endolysin Cpl-1 rescues mice with fatal pneumococcal pneumonia. Crit Care Med 37: 642–649. 10.1097/CCM.0b013e31819586a6 [DOI] [PubMed] [Google Scholar]
- 33. Moineau S, Durmaz E, Pandian S, Klaenhammer TR (1993) Differentiation of Two Abortive Mechanisms by Using Monoclonal Antibodies Directed toward Lactococcal Bacteriophage Capsid Proteins. Appl Environ Microbiol 59: 208–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Duplessis M, Moineau S (2001) Identification of a genetic determinant responsible for host specificity in Streptococcus thermophilus bacteriophages. Mol Microbiol 41: 325–336. [DOI] [PubMed] [Google Scholar]
- 35. Sambrook J, Fritsch EF, Maniatis T (1989) Molecular cloning: a laboratory manual. Cold Spring Harbor, N.Y: CSH Protoc; 3v p. [Google Scholar]
- 36. Rousseau GM, Moineau S (2009) Evolution of Lactococcus lactis Phages within a Cheese Factory. Appl Environ Microbiol 75: 5336–5344. 10.1128/AEM.00761-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Staden R, Beal KF, Bonfield JK (2000) The Staden package, 1998. Methods Mol Biol 132: 115–130. [DOI] [PubMed] [Google Scholar]
- 38. Kraemer L, Beszteri B, Gabler-Schwarz S, Held C, Leese F, et al. (2009) STAMP: Extensions to the STADEN sequence analysis package for high throughput interactive microsatellite marker design. BMC Bioinformatics 10: 41 10.1186/1471-2105-10-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lowe TM, Eddy SR (1997) tRNAscan-SE: a program for improved detection of transfer RNA genes in genomic sequence. Nucleic Acids Res 25: 955–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kilian M, Poulsen K, Blomqvist T, Havarstein LS, Bek-Thomsen M, et al. (2008) Evolution of Streptococcus pneumoniae and its close commensal relatives. PLoS One 3: e2683 10.1371/journal.pone.0002683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sabri M, Haüser R, Ouellette M, Liu J, Dehbi M, et al. (2011) Genome annotation and intraviral interactome for the Streptococcus pneumoniae virulent phage Dp-1. J Bacteriol 193: 551–562. 10.1128/JB.01117-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Samson JE, Moineau S (2010) Characterization of Lactococcus lactis phage 949 and comparison with other lactococcal phages. Appl Environ Microbiol 76: 6843–6852. 10.1128/AEM.00796-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mark DF, Richardson CC (1976) Escherichia coli thioredoxin: a subunit of bacteriophage T7 DNA polymerase. Proc Natl Acad Sci U S A 73: 780–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Martin AC, Blanco L, Garcia P, Salas M, Mendez J (1996) In vitro protein-primed initiation of pneumococcal phage Cp-1 DNA replication occurs at the third 3′ nucleotide of the linear template: a stepwise sliding-back mechanism. J Mol Biol 260: 369–377. [DOI] [PubMed] [Google Scholar]
- 45. Longas E, Villar L, Lazaro JM, de Vega M, Salas M (2008) Phage phi29 and Nf terminal protein-priming domain specifies the internal template nucleotide to initiate DNA replication. Proc Natl Acad Sci U S A 105: 18290–18295. 10.1073/pnas.0809882105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kotsonis SE, Powell IB, Pillidge CJ, Limsowtin GK, Hillier AJ, et al. (2008) Characterization and genomic analysis of phage asccphi28, a phage of the family Podoviridae infecting Lactococcus lactis . Appl Environ Microbiol 74: 3453–3460. 10.1128/AEM.02379-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Raskin DM, Seshadri R, Pukatzki SU, Mekalanos JJ (2006) Bacterial genomics and pathogen evolution. Cell 124: 703–714. [DOI] [PubMed] [Google Scholar]
- 48. Zahner D, Gandhi AR, Yi H, Stephens DS (2011) Mitis group streptococci express variable pilus islet 2 pili. PLoS One 6: e25124 10.1371/journal.pone.0025124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ikryannikova LN, Filimonova AV, Malakhova MV, Savinova T, Filimonova O, et al. (2013) Discrimination between Streptococcus pneumoniae and Streptococcus mitis based on sorting of their MALDI mass spectra. Clin Microbiol Infect 19: 1066–1071. 10.1111/1469-0691.12113 [DOI] [PubMed] [Google Scholar]
- 50. Lopez R, Garcia E, Garcia P, Ronda C, Tomasz A (1982) Choline-containing bacteriophage receptors in Streptococcus pneumoniae . J Bacteriol 151: 1581–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ronda-Lain C, Lopez R, Tapia A, Tomasz A (1977) Role of the pneumococcal autolysin (murein hydrolase) in the release of progeny bacteriophage and in the bacteriophage-induced lysis of the host cells. J Virol 21: 366–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sheppard CL, Harrison TG, Morris R, Hogan A, George RC (2004) Autolysin-targeted LightCycler assay including internal process control for detection of Streptococcus pneumoniae DNA in clinical samples. J Med Microbiol 53: 189–195. [DOI] [PubMed] [Google Scholar]
- 53. Lopez R, Ronda C, Tomasz A, Portoles A (1977) Properties of “diplophage”: a lipid-containing bacteriophage. J Virol 24: 201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ronda C, Garcia JL, Lopez R (1989) Infection of Streptococcus oralis NCTC 11427 by pneumococcal phages. FEMS Microbiol Lett 53: 187–192. [DOI] [PubMed] [Google Scholar]
- 55. Benmayor R, Hodgson DJ, Perron GG, Buckling A (2009) Host mixing and disease emergence. Curr Biol 19: 764–767. 10.1016/j.cub.2009.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hall JP, Harrison E, Brockhurst MA (2013) Viral host-adaptation: insights from evolution experiments with phages. Curr Opin Virol 3: 572–577. 10.1016/j.coviro.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 57. Häuser R, Sabri M, Moineau S, Uetz P (2011) The proteome and interactome of Streptococcus pneumoniae phage Cp-1. J Bacteriol 193: 3135–3138. 10.1128/JB.01481-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
F, forward; R, reverse.
(DOCX)
F, forward; R, reverse.
(DOCX)
a relative to the genome of phage Cp-1.—absence of the nucleotide.
(DOCX)
The values represent the frequency of codon usage per thousand. The phage preferentially used codons for each amino acid are displayed in bold.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.