Highlights
-
•
Bleeding may be due for foreign bodies ingestion.
-
•
Both foreign body ingestion and jejunal diverticula are rare causes of bleeding.
-
•
Surgeons should be aware that patients may fail to recognize and report the possible cause of bleeding.
Keywords: Gastrointestinal bleeding, Foreign bodies ingestion, Hypovolemic shock, Jejunal diverticula, Damage control surgery
Abstract
Introduction
Acute upper gastrointestinal bleeding is a common emergency. The ingestion of foreign bodies represents a less frequent cause of bleeding, but it is equally life-threatening, especially if the patient does not report the incident.
Presentation of case
We are reporting the case of a 77-year-old patient with a bleeding caused by ingestion of glass fragments with co-existing jejunal diverticula.
Discussion
The ingestion of foreign bodies is a rare, mostly accidental event. Another possible source of upper G.I. bleeding is jejunal diverticula; in this case, the examination of the specimens showed evidence of glass ingestion fragments as the likely cause of bleeding.
Conclusion
Surgeons should be aware that patients may fail to report correctly on the possible causes of bleeding, misleading the diagnosis, and delaying the diagnostic routes.
1. Introduction
Acute upper gastrointestinal bleeding is a common emergency that has a 10% hospital mortality rate; despite changes in management, mortality has not significantly improved over the past 50 years.1 Elderly patients and people with chronic medical diseases withstand acute upper gastrointestinal bleeding less well than younger, and have a higher risk of death. The ingestion of foreign bodies represents a less frequent cause of bleeding, but it is equally life-threatening, especially if the patient, unaware of the connection ingestion of foreign body/bleeding, does not report the incident.
2. Presentation of a case
We present a case of a 77 years-old man who, in a summer afternoon of 2008, was admitted to the emergency department of a local hospital for recurrent rectal bleeding. The patient’s medical history reported a mild anemia which had been not yet completely investigated, temporarily treated with oral iron therapy and no further morbidities. After entering the emergency department (ED) of the previous admitting hospital, the patient underwent a complete physical examination that proved to be consistent with age without any sign of distress related to bleeding. A colonoscopy was performed, but no bleeding source was identified. An esophagogastroduodenoscopy was also performed up to the third duodenal portion, without identifying bleeding lesions. As the patient was experiencing recurrent episodes of rectal bleeding and clots emission, he needed several blood transfusions and underwent a spiral computed tomography angiogram (angioCT-scan) that identified a possible bleeding source in the first arterial branch of the superior mesenteric artery. The patient was then transferred to the emergency department (ED) of our institution to undergo a diagnostic selective angiography and eventual angioembolysation of the bleeding source, as, at night, ours is the only admitting hospital for angiography. Although apparently the patient was hemodynamically stable and cooperative, the bleeding had been going on for several hours before being admitted to our institution, hence the presence of an anesthesiologist was required.
Considered that hypovolemia, acidosis, and coagulopathy were already present, the operating room (OR) was set up in a standby mode for a likely emergency surgery. During angiography, the patient experienced a further massive rectal bleeding with red blood and clots, clinical sign of impending shock, and a haemoglobin (Hb) blood gas test of 4.5 g/dl. The procedure was immediately stopped, and the patient was sent to the operating room (OR) for an emergency laparotomy. Multiple diverticula of the upper jejunum were found during surgery, and a 70 cm resection of the small bowel was performed by sectioning the bowel with a GIA35. At that moment, fresh blood started to spontaneously flow through the nasogastric tube, whereas no fluid was present in the stomach since tube insertion. Consequently, we decided to directly check the duodenal stump for other bleeding sources. As the duodenum was opened, a gush of fresh arterial blood and clots burst out, so we decided to extend the intestinal resection to the fourth duodenal portion. (GIA 35) The abdomen was then temporarily closed without any attempt to immediate reconstruction to reduce surgery time as much as possible, minimize hypothermia and treat hypovolemia, acidosis, and coagulopathy. The macroscopic examination of the specimens did not show any sign of bleeding from the diverticula, but the fourth duodenal portion showed several profound linear cuts with fresh bleeding signs and clots. (Fig. 1) These peculiarities were confirmed by histopathological examination.
Fig. 1.
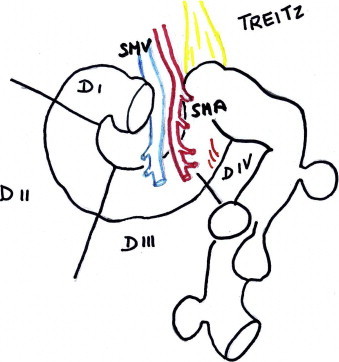
Original anatomy. I – First duodenal portion. II – Second duodenal portion. III – Third duodenal portion. IV – Fourth duodenal portion. SMV – Superior mesenteric vein. SMA – Superior mesenteric artery. TREITZ – Ligament of Treitz.
The figure represented the diverticula of the first 70 cm of the jeunum and some linear cuts of the fourth duodenal portion which were the bleeding source.
The patient was admitted to the intensive care unit (ICU) for an aggressive resuscitation. Twenty-four hours after surgery, the patient was hemodynamically stable, with no sign of further bleeding, conscious and cooperative. Two days later a side-to-side duodeno–jejunal anastomosis was performed, and a double lumen naso–jejunal tube was inserted through the anastomosis for decompression and feeding (Fig. 2). When expressly asked about the possible ingestion of anything that might be the cause of the bleeding, this time the patient recalled to have swallowed some glass fragments of the phyal for his oral iron therapy, but he was so unconcerned by this event that he had completely forgotten it. Even after reporting this event, he still did not see the relation between a “rectal” bleeding and the oral ingestion of small glass fragments.
Fig. 2.
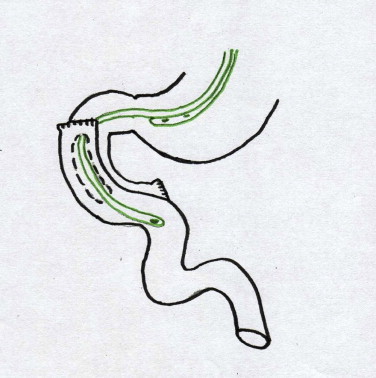
Schematic drawing of the nasojejunal tube for dreinage and feeding and of side-to-side jejunum–duodenal reconstruction.
This was the only possible cause of accidental ingestion of damaging substances we could find in the recent medical history of the patient that matched with the surgical specimen findings.
The gastro–jejunal tube was removed on post-op day thirteen. Patient was discharged after two weeks. Presently, after five years, he is still healthy.(Fig. 3)
Fig. 3.
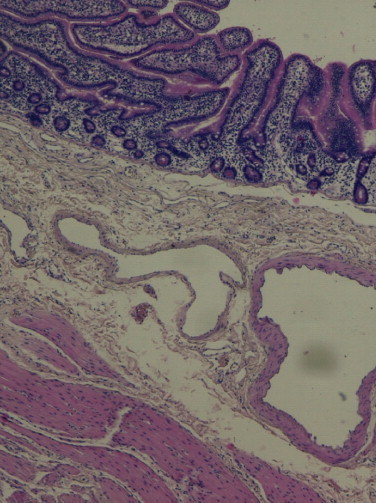
Histologic section of the bleeding duodenum including mucosa and vessels.
3. Discussion
The ingestion of foreign bodies most frequently occurs in children (1–3 years old).2 In adulthood this is seen in psychotic patients,2 but it is a rare, mostly accidental event, in normal population, mainly occurring due to food bones’ ingestion. Perforation of the duodenum, and small bowel have been reported for trichobezoar obstruction or sponge obstruction. A case of bleeding was published for the accidental ingestion of a fish hook.5 To our knowledge, only one case of glass ingestion is present in literature, a toddler who swallowed fragments of an ornamental Christmas bulb3 with severe complication, that produced multiple intestinal lacerations requiring several surgical operations up to total colectomy and permanent ileostomy.
As the colonoscopy and the esophagus gastroduodenoscopy did not show the bleeding source, a CT angio scan was performed. This was the first diagnostic exam which identified a possible bleeding source through the first arterial branch of the superior mesenteric artery, shifting the diagnosis from lower intestinal bleeding to upper G.I. bleeding.
At that point, the patient was sent to our emergency department, the only admitting hospital for emergent angiography at night-time in the area. By then, the patient, although hemodynamically stable, had been bleeding all the time requiring several transfusions so an impeding hypovolemic shock was present with a low HB.
A damage control surgery proved to be the right choice for this patient. The intestinal resection was performed without any attempt to immediate reconstruction to allow the resuscitation procedures in the intensive care unit. Reconstruction was performed on post-surgery day 2 after normalization of the parameters.
About the possible source of the bleeding, jejunal diverticula4 were present in the first portion of the jejunum, consistent with the possible source of bleeding through the first branch of the superior mesenteric artery, but the macroscopic examination of the specimens did not show any sign of bleeding from the diverticula, while the specimen of the fourth duodenal portion showed several profound linear cuts with fresh bleeding signs and clots. These peculiarities were confirmed by histopathological examination and consequently the latter was the only possible cause of bleeding in the patient’s recent medical history that matched with the surgical specimen findings.
4. Conclusion
Our case could serve an educational purpose: usually, the initial rectal bleeding is a self-limiting condition that rarely requires surgery. Besides, the patient, unaware of the danger, failed to tell his physician that he accidentally swallowed glass fragments of the phyal for his oral iron therapy, misleading the initial diagnosis and delaying the diagnostic plane.
Conflict of interest
None.
Funding
None.
Ethical approval
Not appllicable.
Author contributions
Riccardo Gattai: data analisys, data interpretation, and writing. Maria Luisa Migliaccio: data collection. Manuela Bonizzoli: data collection. Adriano Peris: data interpretation. Paolo Bechi: data interpretation. Desiree Pantalone: writing, literature search, and data interpretation.
Consent
Not applicable.
Guarantor
Desiree Pantalone, Department of Surgery and Translational Medicine, University of Florence, Italy Largo Brambilla 50134 Florence, Italy. Email: desire.pantalone@unifi.it, desireepantalone@gmail.com.
Acknowledgment
The Authors thank Dr. Patrizia Agresti (registered Translator at Court House of Florence) for her kind assistance in editing the case report.
Footnotes
Presented at: Communication session 115° Congresso Società Italiana di Chirurgia, Turin October 13–16, 2013
Contributor Information
Riccardo Gattai, Email: rgattai@unifi.it.
Desire’ Pantalone, Email: desire.pantalone@unifi.it, desireepantalone@gmail.com.
Maria Luisa Migliaccio, Email: migliaccioml@aou-careggi.toscana.it.
Manuela Bonizzoli, Email: bonizzolim@aou-careggi.toscana.it.
Adriano Peris, Email: perisa@aou-careggi.toscana.it.
Paolo Bechi, Email: paolo.bechi@unifi.it.
References
- 1.NHS. National Institute of health and clinical excellence- Acute upper gastrointestinal bleeding: management. NICE clinical guideline 141, 2012, guidance.nice.org.uk/cg141.
- 2.Saliakellis E., Borrelli O., Thapar N., Pediatric G.I. Emergencies. Best Pract Res Clin Gastroenterol. 2013;27(5):799–817. doi: 10.1016/j.bpg.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Norberg HP, Reyes HM. Complications of ornamental Christmas bulb ingestion. Case report and review of the literature. [DOI] [PubMed]
- 4.Hamada N., Ishizaki N., Shirahama K., Nakamura N., Murata R., Kadono J. Multiple duodeno–jejunal diverticula causing massive intestinal bleeding. J Gastroenterol. 2000;35:159–162. doi: 10.1007/s005350050030. [DOI] [PubMed] [Google Scholar]
- 5.Mellinghoff CJ The sequelae of a fish dinner. Bleeding in Bangkok. Foreign body-fishing hook. MMW Fortschr Med., 7:155, (19), 2013, 5. [DOI] [PubMed]


