Abstract
Background
Toxoplasmosis is an important, widespread, parasitic infection caused by Toxoplasma gondii. The chronic infection in immunocompetent patients, usually considered as asymptomatic, is now suspected to be a risk factor for various neurological disorders, including epilepsy. We aimed to conduct a systematic review and meta-analysis of the available literature to estimate the risk of epilepsy due to toxoplasmosis.
Methods
A systematic literature search was conducted of several databases and journals to identify studies published in English or French, without date restriction, which looked at toxoplasmosis (as exposure) and epilepsy (as disease) and met certain other inclusion criteria. The search was based on keywords and suitable combinations in English and French. Fixed and random effects models were used to determine odds ratios, and statistical significance was set at 5.0%.
Principal findings
Six studies were identified, with an estimated total of 2888 subjects, of whom 1280 had epilepsy (477 positive for toxoplasmosis) and 1608 did not (503 positive for toxoplasmosis). The common odds ratio (calculated) by random effects model was 2.25 (95% CI 1.27–3.9), p = 0.005.
Conclusions
Despite the limited number of studies, and a lack of high-quality data, toxoplasmosis should continue to be regarded as an epilepsy risk factor. More and better studies are needed to determine the real impact of this parasite on the occurrence of epilepsy.
Author Summary
Toxoplasmosis is a common parasitic infection and affects one-third of the global population. The burden this figure represents clearly signifies the public health relevance of toxoplasmosis. Epilepsy, another chronic condition, is often caused by a variety of infections that affect numerous low- and middle-income tropical countries—including toxoplasmosis. Earlier meta-analysis found only three studies and reported a 4.8-fold greater risk of epilepsy. This had many limitations, as discussed in this paper, our estimate is rather more robust, based on a higher number of studies, and corrects deficiencies that were present previously.
Introduction
Epilepsy is a major chronic neurological disorder that affects about 70 million people worldwide [1]. However, its importance goes beyond mere numbers [2]. Most of its burden is felt in low- and middle-income tropical countries, where a number of infections that are important risk factors for epilepsy, are predominantly reported [3–5]. Parasitic infections are important causes of epileptic seizures or epilepsy, among other neurological and mental health conditions [6,7]. Infection with Toxoplasma gondii (T. gondii) in particular is reported to affect one-third of the world’s population, mainly in the low- and middle-income countries [8,9]. Certain currently available data strongly suggest the possibility of a relationship between toxoplasmosis and epilepsy [6] [10], although results to the contrary have also appeared [11]. Therefore, we conducted a systematic review and meta-analysis of published data to estimate the risk of epilepsy due to toxoplasmosis.
Methods
Literature search
To identify published studies on the association between toxoplasmosis and epilepsy, we conducted a systematic search of the literature published in English or French. The search was conducted on MEDLINE, INGENTACONNECT, REFDOC, SCIENCEDIRECT, GOOGLE, Médecine/Sciences, PLOS ONE and the database of the Institut d’Epidémiologie neurologique et Neurologie Tropicale (IENT): http://www.unilim.fr/IENT/recherche_bvna.phpbase. This database contains medical dissertations, theses, and articles on tropical neurology and parasitology. The keywords for epidemiological aspects were: “epilepsy, Toxoplasma, toxoplasmosis”. Similar keywords were used in French. While searching, OR and/or AND were used for combination terms. We also searched the bibliographies of the articles retained after our database search.
Selection of studies
Articles were selected based on their titles and then their abstracts. Those retained were read in full, but only those articles that met the inclusion-exclusion criteria were finally included. Inclusion criteria were: epilepsy as a disease and toxoplasmosis as an exposure, presence of a control group, sample sizes suitably estimated, details of techniques used to diagnose epilepsy and toxoplasmosis, and details on selection of participants, including socio-economic level. Data were then entered in a database covering: title, principal author, year of publication, type of study, objectives, methods, results, and any additional comments.
Meta analysis
The meta-analysis was conducted using EasyMA version 2001 and Medcalc (Belgium) version 12.6.0. The measure of association between toxoplasmosis and epilepsy was a common odds-ratio (OR), recommended for the meta-analysis of observational studies. Respective ORs of each included study were individually verified. Random effects models were used to determine common odd ratios. Homogeneity of the studies was examined using Cochrane Q, 95% confidence intervals (CI) were also derived, and the statistical significance was set at 5%. A scatter plot was drawn from the combined data obtained.
Results
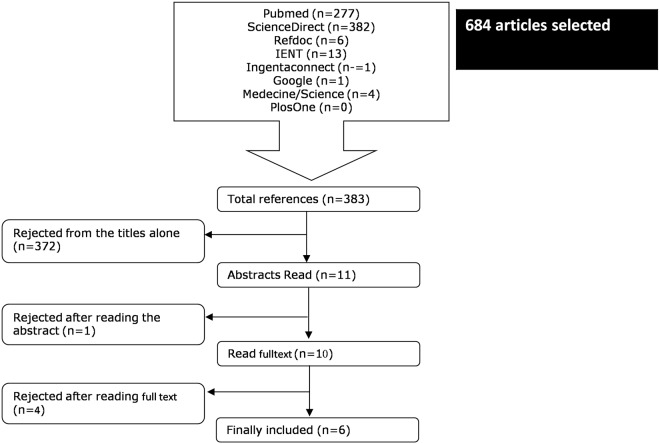
The results of the search are presented in Fig. 1. Five databases (Pubmed, ScienceDirect, Refdoc, IENT and Ingentaconnect), two journals (Médecine/Sciences, PlosOne) and Google search gave a total of 684 articles. Of these, 301 were cited more than once. Of the remaining 383 articles on toxoplasmosis and epilepsy, 372 articles were eliminated on the basis of title as either non-epidemiological or in a language other than English or French. The remaining 11 articles were read as abstracts, and one was excluded because its full text was not accessible. Furthermore, two were literature reviews [12] [13], one was a meta-analysis [10] and one was an epidemiological study that did not meet our inclusion criteria i.e. no control group [14]. The references of the review articles and meta-analysis did not add any new articles. Lastly, six studies were retained [2] [11] [3,15] [16] [17] [18], from Israel, USA, Turkey, Iran and various countries of sub-Saharan Africa. Interestingly, no studies were from Latin America, Europe, or most of Asia, table 1.
Fig 1. Flowchart of search of studies for epidemiological correlation between toxoplasmosis and epilepsy.
Table 1. Description of studies included in the meta-analysis of association between toxoplasmosis and epilepsy.
| Reference | Study | Source 1 | Definition | Source 2 | Matching* | Measure of exposure |
|---|---|---|---|---|---|---|
| Potasman (Israel) | CC | Hospital | Other | Hospital | Unspecified | ELISA IgG (Tox-G EAI diagnostic kit, Abbott lab) |
| Stommel (USA) | CC | GP | ILAE | Community | Unspecified | ELISA IgG |
| Yazar (Turkey) | CC | Hospital | ILAE | Volunteers | Yes | ELISA IgG (ELISA Kit EUROIMMUN) |
| Akyol (Turkey) | CC | Hospital | ILAE | Volunteers | Yes | in house ELISA IgG kit |
| Zibaei (Iran) | CC | GP | ILAE | Community | Yes | Diaplus Inc, Toxo IgG, USA |
| Ngugi (SSA) | CC | GP | WHO | Community | Yes | IgG-ELISA, Genesis Diagnostics |
CC: Case-control; GP: General population; ELISA: enzyme-linked immunosorbent assay; IgG: Immunoglobulin G; ILAE: International league against epilepsy; SSA: Sub-saharan Africa, WHO: World health organization,
*matching is by age and gender alone
Study: Study type; source 1: source of epilepsy cases; source 2: source of non-epilepsy controls; definition: definition of epilepsy; Other: clinical history by pediatric neurologist, repeated electroencephalography and computed tomography of the brain
As summarized in table 1, three studies recruited cases from hospital(s), but only one recruited controls from hospital(s). The remaining studies (n = 5) recruited controls from the community or used volunteers. Four studies matched controls for age and gender. Toxoplasma infection status was determined with the use of IgG ELISA, table 1. As summarized in table 2, only one study recruited subjects of all ages, as is often recommended. All but one study [11] reported a “risk relationship” between toxoplasmosis and the development of epilepsy, table 2. Only one of the included studies provided any urban-rural information [16].
Table 2. Description of data extracted from the included studies in the meta-analysis searching for an association between toxoplasmosis and epilepsy.
| Reference | N | Age | EP+ (n) | EA- (n) | EP & T+(n, %) | EA & T+ (n, %) | OR (95% CI) | P-value |
|---|---|---|---|---|---|---|---|---|
| Potasman (1987–91, Israel) | 161 | 1–15 | 52 | 109 | 10 (19.2%) | 10 (9.0%) | 2.36 (0.91–6.08) | 0.11 |
| Stommel (1997–99, USA) | 45 | adults | 22 | 23 | 17 (75.0%) | 13 (56.5%) | 2.62 (0.72–9.54) | 0.075 |
| Yazar (1999–2002, Turkey) | 100 | adults | 50 | 50 | 27 (54.0%) | 9 (25.0%) | 5.35 (2.15–13.30) | <0.001 |
| Akyol (2003, Turkey) | 150 | 11–64 | 100 | 50 | 31 (31.0%) | 10 (20.0%) | 1.80 (0.80–4.05) | 0.2 |
| Zibaei (2010, Iran) | 170 | 7–62 | 85 | 85 | 12 (14.1%) | 4 (4.7%) | 3.33 (1.03–10.78) | 0.036 |
| Ngugi (2007–11, SSA) | 2262 | All | 971 | 1291 | 380 (39.1%) | 457 (35.4%) | 1.17 (0.99–1.39) | 0.06 |
Age is in years; CI: Confidence interval; EP+: People with epilepsy; EA-: People without epilepsy; EP & T+: People with epilepsy and Toxoplasma positive; EA & T+: People without epilepsy and Toxoplasma positive; OR: Odds ratio; SSA: Sub-saharan Africa
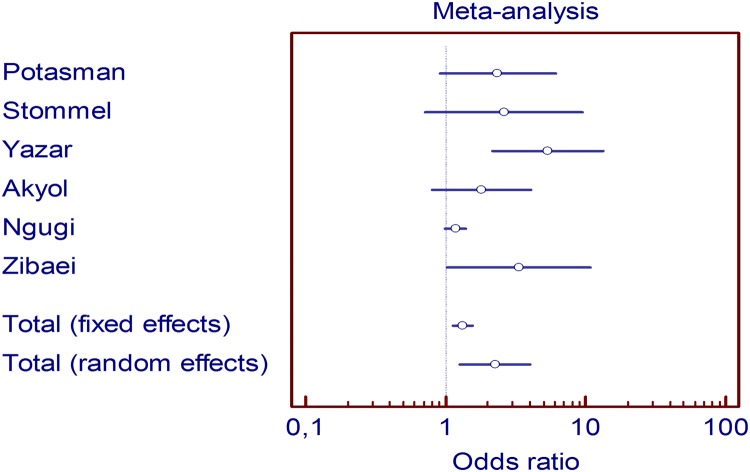
The total number of subjects in all included studies was 2888, of whom 1280 had epilepsy and 1608 did not (table 2). As summarized in table 2, the frequency of patients with epilepsy who were Toxoplasma-positive varied from 14.1% to 75.0%. Among subjects without epilepsy, the proportion of Toxoplasma positivity varied between 4.70% and 56.50%. Seroprevalence for T. gondii was therefore higher among those who had epilepsy than those who did not. The ORs of included studies varied from 1.17 (95% CI 0.99–1.39) to 5.35 (95% CI 2.15–13.30) but only two of these results were significant (table 2). Scatter plots of the six studies are presented in Fig. 2. The common OR (fixed effects model) was 1.32 (95% CI 1.13–1.55), p<0.001. The heterogeneity was statistically significant, p = 0.006. Therefore, we estimated a common OR by a random effects model at 2.25 (95% CI 1.27–3.98), p = 0.05. The test of homogeneity was clearly not significant in this case, p = 0.6.
Fig 2. Scatter plot of odds ratios for epidemiological correlation between toxoplasmosis and epilepsy.
Discussion
We conducted a systematic review and meta-analysis of literature primarily to estimate the relationship between chronic toxoplasmosis and epilepsy. Our literature search was comprehensive as different databases and specific journals were searched, including those in the French language to avoid any publication bias. However, this search might have excluded important studies published exclusively in other languages. The last meta-analysis on this subject, conducted in 2007, [10] included only three studies, whereas ours identified six, table 1.
One of the foremost lessons from our work is that despite the fact that T.gondii infection affects nearly one-third of the world’s population and is likely to be epileptogenic, few data exist on the subject. This certainly calls for more studies. Interestingly, none of the studies found were from Latin America, or Europe, and most of Asia remains unaddressed sparing two countries from Western Asia (Israel and Turkey) and one from Southern Asia (Iran), another important limitation. Toxoplasmosis in Asia is reportedly a silent threat [19], and epilepsy is far less well addressed in Asia than elsewhere. As seen in table 2, the OR was lower in African studies than those conducted elsewhere, whereas in Turkey OR was higher than elsewhere [11] [15]. Significant differences in the virulence and host response to strains are reported[20]. The extent to which these strain differences affect epileptogenic potential is not yet studied. Differences in strains can also be important in elucidating regional differences in the burden of toxoplasma-related epilepsy as there is a spatial distribution [20] [21] [22] [23] [24]. Strains circulating in Africa and South America are genetically quite different from those circulating in Europe or North America, and are responsible for more severe and frequent retinochoroiditis. It cannot be excluded that this higher pathogenicity observed in retinal tissue is also observed in brain tissue [20,24–26]. Very recently, a study conducted in Sub-Saharan Africa demonstrated that combinations of parasites can have additive effects on consequential conditions such as toxoplasmosis and onchocerciasis on active convulsive epilepsy [27].
Toxoplasmosis was found to be a risk factor for epilepsy; however the degree of risk differed between that reported in an earlier meta-analysis (OR 4.80, 95% CI 2.60–7.80) [10] and the one estimated by us (OR 2.25, 95% CI 1.15–3.93). The previous meta-analysis was, however based on only three studies [10].
Moreover, there were important differences in data extraction between the earlier meta-analysis [10] and ours. For instance, in one study [17], the number of patients with epilepsy was erroneously considered to be 95. The actual number was 52, as we calculated from the OR given in the study and the data recorded in the results [17]. A similar case relates to the estimated number of seropositives and seronegatives in another study [18]. The previous meta-analysis [10] estimated 18 seropositive cases and five seronegative controls, but this would give an OR of 12.24, higher than the 2.63 reported [18] However, we performed a calculation by approximation that permitted us to obtain, from the OR, the respective values of 10 and 13, which yielded an OR of 2.62, just about same as the original OR reported in that study.
Four studies out of six had non-significant results, table 2. Most had small sample sizes, with the exception of one by Ngugi et al [3]. This later study [3] yielded significant risk of epilepsy only in subjects >18 years of age, and not those <18 years old, table 2. Nevertheless, five out of six studies concluded that toxoplasmosis was a risk factor for epilepsy, while only one of our studies [11] failed to find any association between toxoplasmosis and epilepsy. However, this study had several limitations in its design and data analysis [28]. It is often contended that the burden of epilepsy moves proportionately with that of toxoplasmosis (e.g. more toxoplasmosis, more epilepsy) [10], but this may not be logically correct. Because of the large number of causes of epilepsy, one single factor like toxoplasmosis, about the epileptogenicity of which little is known, cannot explain such epidemiological shifts of a disease like epilepsy in any given population.
Also, there is always a possibility of an influence of variables such as 24 hour EEGs supervised by an epileptologist or diagnosis by simple history-taking by a family physician, etc., that may cause some influence on the diagnosis of epilepsy, hence on the results of some of these studies.
Various cellular, anatomical, immunological, and neurotransmitter-related changes occur as a result of infection with T. gondii, which plays a role in the development of various neurological conditions [29]. In general, the neuropathology of chronic latent infection differs from acute cerebral toxoplasmosis, in which necrosis and inflammation are generally widespread. For epilepsy, the neuropathology of T. gondii infection is yet to be fully elucidated and is speculative at best. Epileptogenic mechanisms of toxoplasmosis are probably multifactorial. Brain is one of the primary targets for the formation of T. gondii cysts and a variety of brain cells, particularly neurons, but microglia and astrocytes, can also get infected [30,31]. Neurons are predominantly infected because both astrocytes and microglia may protect themselves as a result of their ability to inhibit parasitic replication upon activation [32]. Once a chronic infection is established, T. gondii is found in tissue cysts containing the bradyzoite stage. Brain tissue cysts mature slowly; their wall may eventually rupture in immunocompetent hosts, liberating numerous bradyzoites that are capable of infecting new cells and inducing localized inflammation. This process may produce microglial scars (glial nodules). It has been suggested that scar tissue formation is one of the main causes of epilepsy in toxoplasmosis patients [10]. The likelihood of seizures would also depend on the location and numbers of cysts. Most cysts occur in the grey matter, a more epileptogenic area than white matter [33]. Other epilepsy-relevant areas such as the cerebral cortex, hippocampus, amygdala, and basal ganglia are also reported to be invaded by tissue cysts; while the greatest impact is reportedly on the hippocampus and amygdala [34]. In addition, the size of a cyst may also influence how it functionally impairs neuronal activity [35].
Neurotransmitters such as serotonin, glutamate, and gamma aminobutyric acid (GABA) need to be considered in T. gondii-induced neuropathological changes, and the host immune response to T. gondii infection can lead to altered neurotransmitter levels [36]. Chronic infection with T. gondii may also cause localized changes in serotonin levels [37]. The inhibitory neurotransmitter GABA is also important. In cases of infection with T. gondii, secretion of GABA increases as a response by dendritic cells to the invading parasite [38].
Data from animal studies show the following: intraneuronal T. gondii cysts directly modulate neuronal function, leading to either hypo- or hyper-responsive neurons [39,40] [41]. Tachyzoite infection of neurons results in dysregulation of calcium influx upon stimulation with glutamate [39], the major excitatory amino acid in the brain, which inevitably plays an important role in the initiation and spread of seizure activity. Another hypothesis concerns the importance of Ca+ ions in key aspects of the T. gondii life cycle, including motility, invasion and exit from the host cell [42]. Neuronal excitability can be influenced through depletion of calcium stores in the endoplasmic reticulum of the host cell. Uninfected neurons display a sustained calcium response, whereas infected neurons display either a short calcium response or complete failure. This indicates that T. gondii infected neurons exhibit depletion of calcium stores in the endoplasmic reticulum, and therefore influence the excitability of the neurons [43].
Desirable criteria for good-quality studies on this subject
Good-quality epidemiological research will further help to draw broad conclusions on this important subject. These good-quality studies may at least be population-based with samples representative of all age-groups, and taking cases-controls from the same source population with at least 70% power. These studies should also use standard criteria to define various parameters and taking active epilepsy into account with clear description of procedures followed in the article.
Conclusions
Few studies evaluating the risk of epilepsy following toxoplasmosis are available, and none cover Europe and Latin American regions. Most Asian countries also remain unaddressed except Israel, Turkey and Iran. Based on the currently available data, and their obvious limitations, it is still good to consider toxoplasmosis as a possible epilepsy risk factor, at least epidemiologically. However, many questions remain to be addressed in future studies. Combinations of parasites may have additive effects on consequential conditions such as toxoplasmosis and onchocerciasis on active epilepsy [27].
Key learning points
If one-third of the global human population carries a toxoplasma infection, and if a fraction of these toxoplasma carriers eventually develop epilepsy, then a huge number of people worldwide is at risk of developing toxoplasma-related epilepsy;
Good quality studies are needed to correctly determine whether or not there is a risk/causal relationship between toxoplasmosis and epilepsy;
Interestingly, there is no data from South America, Europe, or most of Asia, where more virulent Toxoplasma strains circulate;
Based on current data, the risk of epilepsy with toxoplasmosis stands at 2.2-fold, but the confidence interval ranges between 1.27 and 3.9-fold;
Epileptogenic mechanisms of toxoplasmosis are probably multifactorial (direct lodgment of parasite, direct modulation of neuronal functions, abnormalities in GABA, role of calcium, etc.);
Many unanswered issues remain, including the role of different strains, defining suitable prevention strategies, defining epileptogenic mechanisms, etc.;
Combinations of parasites may have additive effects on consequential conditions such as toxoplasmosis and onchocerciasis on active convulsive epilepsy.
Key papers in the field
Palmer BS (2007) Meta-analysis of three case controlled studies and an ecological study into the link between cryptogenic epilepsy and chronic toxoplasmosis infection. Seizure 16: 657–663.
Stommel EW, Seguin, R., Thadani, V. M. et al. (2001) Cryptogenic epilepsy: an infectious aetiology?. Epilepsia 42: 436–438.
Veeranoot N (2007) Toxoplasmosis: A silent threat in Southeast Asia. Res J Parasitol 2: 1–12.
Fuks JM, Arrighi RB, Weidner JM, Kumar Mendu S, Jin Z, et al. (2012) GABAergic signaling is linked to a hypermigratory phenotype in dendritic cells infected by Toxoplasma gondii. PLoS Pathog 8: e1003051.
Haroon F, Händel U, Angenstein F, Goldschmidt J, Kreutzmann P, Lison H, Fischer KD, Scheich H, Wetzel W, Schlüter D, Budinger E. Toxoplasma gondii actively inhibits neuronal function in chronically infected mice. PLoS One. 2012;7(4):e35516.
Fischer HG, Nitzgen B, Reichmann G, Gross U, Hadding U (1997) Host cells of Toxoplasma gondii encystation in infected primary culture from mouse brain. Parasitol Res 83: 637–641.
Kamuyu G, Bottomley C, Mageto J, Lowe B, Wilkins PP, et al. (2014) Exposure to multiple parasites is associated with the prevalence of active convulsive epilepsy in sub-saharan Africa. PLoS Negl Trop Dis 8: e2908.
Supporting Information
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
BGFI-Bank Foundation (www.bgfi.com) funded EA-NEMIT headed by EBN (1st author). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR (2010) Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia 51: 883–890. 10.1111/j.1528-1167.2009.02481.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Komolafe MA, Sunmonu TA, Afolabi OT, Komolafe EO, Fabusiwa FO, et al. (2012) The social and economic impacts of epilepsy on women in Nigeria. Epilepsy Behav 24: 97–101. 10.1016/j.yebeh.2011.11.019 [DOI] [PubMed] [Google Scholar]
- 3. Ngugi AK, Bottomley C, Kleinschmidt I, Wagner RG, Kakooza-Mwesige A, et al. (2013) Prevalence of active convulsive epilepsy in sub-Saharan Africa and associated risk factors: cross-sectional and case-control studies. Lancet Neurol 12: 253–263. 10.1016/S1474-4422(13)70003-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burneo JG, Tellez-Zenteno J, Wiebe S (2005) Understanding the burden of epilepsy in Latin America: a systematic review of its prevalence and incidence. Epilepsy Res 66: 63–74. [DOI] [PubMed] [Google Scholar]
- 5. Preux PM, Druet-Cabanac M (2005) Epidemiology and aetiology of epilepsy in sub-Saharan Africa. Lancet Neurol 4: 21–31. [DOI] [PubMed] [Google Scholar]
- 6. de Bittencourt PR, Adamolekum B, Bharucha N, Carpio A, Cossio OH, et al. (1996) Epilepsy in the tropics: I. Epidemiology, socioeconomic risk factors, and etiology. Epilepsia 37: 1121–1127. [DOI] [PubMed] [Google Scholar]
- 7. Tenter AM, Heckeroth AR, Weiss LM (2000) Toxoplasma gondii: from animals to humans. Int J Parasitol 30: 1217–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pappas G, Roussos N, Falagas ME (2009) Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol 39: 1385–1394. 10.1016/j.ijpara.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 9. Torgerson PR, Mastroiacovo P (2013) The global burden of congenital toxoplasmosis: a systematic review. Bull World Health Organ 91: 501–508. 10.2471/BLT.12.111732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Palmer BS (2007) Meta-analysis of three case controlled studies and an ecological study into the link between cryptogenic epilepsy and chronic toxoplasmosis infection. Seizure 16: 657–663. [DOI] [PubMed] [Google Scholar]
- 11. Akyol A, Bicerol B, Ertug S, Ertabaklar H, Kiylioglu N (2007) Epilepsy and seropositivity rates of Toxocara canis and Toxoplasma gondii. Seizure 16: 233–237. [DOI] [PubMed] [Google Scholar]
- 12. Dalimi A, Abdoli A (2012) Latent toxoplasmosis and human. Iran J Parasitol 7: 1–17. [PMC free article] [PubMed] [Google Scholar]
- 13. Finsterer J, Auer H (2013) Parasitoses of the human central nervous system. J Helminthol 87: 257–270. 10.1017/S0022149X12000600 [DOI] [PubMed] [Google Scholar]
- 14. Critchley EM, Vakil SD, Hutchinson DN, Taylor P (1982) Toxoplasma, Toxocara, and epilepsy. Epilepsia 23: 315–321. [DOI] [PubMed] [Google Scholar]
- 15. Yazar S, Fehim A, Saban Y, Funda D (2003) Investigation of probable relationship between toxoplasma gondii and cryptogenic epilepsy. Seizure 12: 107–109. [DOI] [PubMed] [Google Scholar]
- 16. Zibaei M, Zamani Z, Esfahani AC, Anbari K, Nazer MR (2011) Toxoplasma infection and epilepsy: A case-control study in Iran. Neurol Asia 16: 299–302. [Google Scholar]
- 17. Potasman I, Davidovitch M, Tal Y, Tal J, Zelnik N, et al. (1995) Congenital toxoplasmosis: a significant cause of neurological morbidity in Israel? Clin Infect Dis 20: 259–262. [DOI] [PubMed] [Google Scholar]
- 18. Stommel EW, Seguin R, Thadani VM, Schwartzman JD, Gilbert K, et al. (2001) Cryptogenic epilepsy: an infectious etiology? Epilepsia 42: 436–438. [DOI] [PubMed] [Google Scholar]
- 19. Veeranoot N (2007) Toxoplasmosis: A silent threat in Southeast Asia. Res J Parasitol 2: 1–12. [Google Scholar]
- 20. Darde ML (2008) Toxoplasma gondii, “new” genotypes and virulence. Parasite 15: 366–371. [DOI] [PubMed] [Google Scholar]
- 21. Doskaya M, Caner A, Ajzenberg D, Degirmenci A, Darde ML, et al. (2013) Isolation of Toxoplasma gondii strains similar to Africa 1 genotype in Turkey. Parasitol Int 62: 471–474. 10.1016/j.parint.2013.06.008 [DOI] [PubMed] [Google Scholar]
- 22. Stajner T, Vasiljevic Z, Vujic D, Markovic M, Ristic G, et al. (2013) Atypical strain of Toxoplasma gondii causing fatal reactivation after hematopoietic stem cell transplantion in a patient with an underlying immunological deficiency. J Clin Microbiol 51: 2686–2690. 10.1128/JCM.01077-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pereira-Chioccola VL, Vidal JE, Su C (2009) Toxoplasma gondii infection and cerebral toxoplasmosis in HIV-infected patients. Future Microbiol 4: 1363–1379. 10.2217/fmb.09.89 [DOI] [PubMed] [Google Scholar]
- 24. Mercier A, Devillard S, Ngoubangoye B, Bonnabau H, Banuls AL, et al. (2010) Additional haplogroups of Toxoplasma gondii out of Africa: population structure and mouse-virulence of strains from Gabon. PLoS Negl Trop Dis 4: e876 10.1371/journal.pntd.0000876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gilbert RE, Stanford MR, Jackson H, Holliman RE, Sanders MD (1995) Incidence of acute symptomatic toxoplasma retinochoroiditis in south London according to country of birth. BMJ 310: 1037–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pfaff AW, de-la-Torre A, Rochet E, Brunet J, Sabou M, et al. (2014) New clinical and experimental insights into Old World and neotropical ocular toxoplasmosis. Int J Parasitol 44: 99–107. 10.1016/j.ijpara.2013.09.007 [DOI] [PubMed] [Google Scholar]
- 27. Kamuyu G, Bottomley C, Mageto J, Lowe B, Wilkins PP, et al. (2014) Exposure to multiple parasites is associated with the prevalence of active convulsive epilepsy in sub-saharan Africa. PLoS Negl Trop Dis 8: e2908 10.1371/journal.pntd.0002908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Quet F, Preux PM, Nicoletti A (2008) Comment on “Epilepsy and seropositivity rates of Toxocara canis and Toxoplasma gondii”. Seizure 17: 296 [DOI] [PubMed] [Google Scholar]
- 29. Hermes G, Ajioka JW, Kelly KA, Mui E, Roberts F, et al. (2008) Neurological and behavioral abnormalities, ventricular dilatation, altered cellular functions, inflammation, and neuronal injury in brains of mice due to common, persistent, parasitic infection. J Neuroinflammation 5: 48 10.1186/1742-2094-5-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carruthers VB, Suzuki Y (2007) Effects of Toxoplasma gondii infection on the brain. Schizophr Bull 33: 745–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fischer HG, Nitzgen B, Reichmann G, Gross U, Hadding U (1997) Host cells of Toxoplasma gondii encystation in infected primary culture from mouse brain. Parasitol Res 83: 637–641. [DOI] [PubMed] [Google Scholar]
- 32. Halonen SK, Lyman WD, Chiu FC (1996) Growth and development of Toxoplasma gondii in human neurons and astrocytes. J Neuropathol Exp Neurol 55: 1150–1156. [DOI] [PubMed] [Google Scholar]
- 33. Ferguson DJ, Hutchison WM (1987) The host-parasite relationship of Toxoplasma gondii in the brains of chronically infected mice. Virchows Arch A Pathol Anat Histopathol 411: 39–43. [DOI] [PubMed] [Google Scholar]
- 34. Vyas A, Kim SK, Giacomini N, Boothroyd JC, Sapolsky RM (2007) Behavioral changes induced by Toxoplasma infection of rodents are highly specific to aversion of cat odors. Proc Natl Acad Sci U S A 104: 6442–6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ferguson DJ, Hutchison WM (1987) An ultrastructural study of the early development and tissue cyst formation of Toxoplasma gondii in the brains of mice. Parasitol Res 73: 483–491. [DOI] [PubMed] [Google Scholar]
- 36. Webster JP (2001) Rats, cats, people and parasites: the impact of latent toxoplasmosis on behaviour. Microbes Infect 3: 1037–1045. [DOI] [PubMed] [Google Scholar]
- 37. Stibbs HH (1985) Changes in brain concentrations of catecholamines and indoleamines in Toxoplasma gondii infected mice. Ann Trop Med Parasitol 79: 153–157. [DOI] [PubMed] [Google Scholar]
- 38. Fuks JM, Arrighi RB, Weidner JM, Kumar Mendu S, Jin Z, et al. (2012) GABAergic signaling is linked to a hypermigratory phenotype in dendritic cells infected by Toxoplasma gondii. PLoS Pathog 8: e1003051 10.1371/journal.ppat.1003051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Haroon F, Handel U, Angenstein F, Goldschmidt J, Kreutzmann P, et al. (2012) Toxoplasma gondii actively inhibits neuronal function in chronically infected mice. PLoS One 7: e35516 10.1371/journal.pone.0035516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kaushik M, Lamberton PH, Webster JP (2012) The role of parasites and pathogens in influencing generalised anxiety and predation-related fear in the mammalian central nervous system. Horm Behav 62: 191–201. 10.1016/j.yhbeh.2012.04.002 [DOI] [PubMed] [Google Scholar]
- 41. Webster JP, McConkey GA (2010) Toxoplasma gondii-altered host behaviour: clues as to mechanism of action. Folia Parasitol (Praha) 57: 95–104. [DOI] [PubMed] [Google Scholar]
- 42. Arrizabalaga G, Ruiz F, Moreno S, Boothroyd JC (2004) Ionophore-resistant mutant of Toxoplasma gondii reveals involvement of a sodium/hydrogen exchanger in calcium regulation. J Cell Biol 165: 653–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kim JY, Ahn HJ, Ryu KJ, Nam HW (2008) Interaction between parasitophorous vacuolar membrane-associated GRA3 and calcium modulating ligand of host cell endoplasmic reticulum in the parasitism of Toxoplasma gondii. Korean J Parasitol 46: 209–216. 10.3347/kjp.2008.46.4.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.