Abstract
Background
Cardiac stress testing, particularly with imaging, has been the focus of debates about rising health care costs, inappropriate use, and patient safety in the context of radiation exposure.
Objective
To determine whether U.S. trends in cardiac stress test use may be attributable to population shifts in demographics, risk factors, and provider characteristics and evaluate whether racial/ethnic disparities exist in physician decision making.
Design
Analyses of repeated cross-sectional data.
Setting
National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey (1993 to 2010).
Patients
Adults without coronary heart disease.
Measurements
Cardiac stress test referrals and inappropriate use.
Results
Between 1993 to 1995 and 2008 to 2010, the annual number of U.S. ambulatory visits in which a cardiac stress test was ordered or performed increased from 28 per 10 000 visits to 45 per 10 000 visits. No trend was found toward more frequent testing after adjustment for patient characteristics, risk factors, and provider characteristics (P = 0.134). Cardiac stress tests with imaging comprised a growing portion of all tests, increasing from 59% in 1993 to 1995 to 87% in 2008 to 2010. At least 34.6% were probably inappropriate, with associated annual costs and harms of $501 million and 491 future cases of cancer. Authors found no evidence of a lower likelihood of black patients receiving a cardiac stress test (odds ratio, 0.91 [95% CI, 0.69 to 1.21]) than white patients, although some evidence of disparity in Hispanic patients was found (odds ratio, 0.75 [CI, 0.55 to 1.02]).
Limitations
Cross-sectional design with limited clinical data.
Conclusion
National growth in cardiac stress test use can largely be explained by population and provider characteristics, but use of imaging cannot. Physician decision making about cardiac stress test use does not seem to contribute to racial/ethnic disparities in cardiovascular disease.
Introduction
Advances in cardiovascular testing have enhanced physicians’ ability to diagnose and treat coronary heart disease (CHD), but growth in use of these technologies—particularly those involving radiological imaging—has been at the epicenter of debates over rising healthcare costs,(1) inappropriate utilization,(2) and patient safety in the context of radiation exposure.(3) The controversy has also spurred public and private action, with recent years witnessing reductions in Medicare reimbursement for cardiac imaging studies,(4) adoption of prior authorization policies,(5) and promotion of professional society campaigns aimed at reducing wasteful healthcare services.(6, 7) Cardiac stress testing—particularly when performed with imaging—has been a focal point of these debates.(6, 8–11) However, little is known about national patterns of cardiac stress test use in the United States(12); the extent to which test growth may be attributable to changing population demographics, risk factors, and provider characteristics; or whether racial/ethnic disparities exist in its use.
Prior studies examining temporal trends in cardiac stress testing have generally focused on patients enrolled in Medicare or other selective populations that may not be representative of the US population.(13–15) To the best of our knowledge, studies of disparities in cardiac stress testing have primarily explored differences in care between men and women,(16–19) and the potential influence of race or ethnicity has received little attention.(20) Examining disparities in this context is important because differences in the use (underuse) of diagnostic testing could contribute to poorer cardiovascular health outcomes observed in black patients, or worsen health in Hispanic patients; these may both be exacerbated by efforts to reduce testing use.(21, 22) To answer these questions, we used nationally representative data to (1) explore trends in cardiac stress test use in the United States among patients evaluated for CHD; (2) determine whether these trends may be attributable to population shifts in demographic and clinical risk factors and provider characteristics; and (3) evaluate whether racial/ethnic disparities exist in the use of cardiac stress testing.
Methods
Data, Study Population, and Primary Outcome
We analyzed data collected in the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1993–2010.(23) We included all visits to office-based physicians and hospital-based outpatient clinics by adults (≥18 years old) without a visit diagnosis of CHD. Performance or referral to cardiac stress testing was the primary outcome, and we identified these visits using International Classification of Diseases procedure codes 89.41 (treadmill stress test), 89.43 (bicycle ergometer stress test), and 89.44 (stress test with imaging).(24) The survey specifically asks about tests that were “ordered or provided at this visit.” Details of our methods are provided in the Appendix.
Primary Measures
We used visit diagnoses and reasons for visit to identify patients with established risk factors for CHD based on the Framingham Heart Study, including hypertension, dyslipidemia, cigarette smoking, obesity, and diabetes/glucose intolerance. We also identified patients who visited the physician for chest pain (Reason for Visit Classification codes 1050.0 and 1265.0).(24) In addition, we created a measure for low-risk visits, defined by patients who had no clinical risk factors and did not visit the physician because of chest pain.
Race and ethnicity were determined, per NAMCS and NHAMCS instructions, according to the office or clinic’s “usual practice, based on your knowledge of the patient, or from information in the medical record.” We categorized patients as non-Hispanic white, non-Hispanic black, Hispanic, other race, and unknown race/ethnicity, when information on ethnicity was missing.
Other Measures
To further assess whether cardiac stress testing was associated with characteristics of patients or providers, we extracted information on patient age, sex, insurance (private, Medicare, Medicaid, self-pay/no charge, and other/unknown), US census region (Northeast, Midwest, South, and West), urban or rural setting, and physician type (primary care, cardiology, and other), which was only available in the NAMCS. Census measures for percent living in poverty, median household income, and percent of adults with a bachelor’s degree were provided in the 2006–2010 NAMCS and NHAMCS using each patient’s ZIP code. We included these measures in sub-analyses of ethnic/racial disparities.
Appropriateness of Imaging Use
We also assessed the appropriateness of cardiac stress testing with and without imaging using appropriate use criteria developed collaboratively by several medical specialty societies, including the American College of Cardiology, American Society of Nuclear Cardiology, and American Society of Echocardiography.(25) Adapting these criteria to our population, we generally considered a test rarely appropriate if it was ordered or performed in a patient without chest pain/angina as a reason for visiting their physician, ischemic equivalents (including jaw or shoulder pain, palpitations, and dyspnea), CHD risk equivalents, electrocardiogram (ECG) abnormalities, or syncope. The NAMCS/NHAMCS provide a sufficient amount of clinical data to identify cardiac stress tests that are rarely appropriate because they collect detailed information about patients’ complaints/symptoms and physicians’ visit diagnoses. In order to maximize the specificity of our approach and minimize the risk of incorrectly categorizing an appropriate test as inappropriate, we also generally excluded studies that were done in patients with congestive heart failure (see Appendix Table 9 for detailed description of methods). Our assessment of appropriateness was limited to 2005–2010, the years after which appropriate use criteria were adopted.
We also estimated the potential economic and health impact of inappropriate testing in the United States. To perform our economic analysis, we used average national Medicare reimbursement rates as a proxy for economic costs.(26) Because Medicare reimbursement for nonimaging and imaging cardiac stress tests fell from 2005 to 2010, we calculated the mean reimbursement levels in these two years and converted these amounts to 2013 US dollars using the Consumer Price Index ($114 for stress ECG, $284 for stress echocardiogram, and $644 for stress myocardial perfusion imaging [MPI]). We also assumed that 62% of imaging stress tests in patients undergoing initial outpatient evaluation for CHD were performed with myocardial perfusion imaging, with the remainder performed with echocardiography.(27) Similarly, the population attributable cancer risk from stress MPI-related ionizing radiation (mean effective dose 16.9 millisieverts per exam) was estimated to be 1 radiation-related cancer per 1,230 MPI exams, based on a prior study which adjusted for exam technique, type of cardiac radiopharmaceutical used, and population characteristics.(28) Finally, we assumed that patients were unlikely to receive more than one cardiac stress test with imaging each year.(29)
Statistical Analysis
All analyses accounted for the complex sampling design of the NAMCS and NHAMCS.(30) We used simple and multivariate logistic regressions with year included as a continuous linear predictor to examine time trends. Multivariable logistic regression models also adjusted for patients’ clinical risk factors and demographic characteristics, insurance, region, setting, and physician specialty. To determine which specific patient and provider characteristics accounted for the overall trends we observed, we constructed simple logistic regression models that assessed whether factors that were statistically significant in our primary model also rose in prevalence over the duration of our study period. The specifications of our models are further described in the Appendix. Analyses were performed using Stata version 12 (College Station, Texas).
Role of the Funding Source
The study was funded in part by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. The funding sources had no role in the design, conduct, or reporting of this study or in the decision to submit the manuscript for publication.
Results
Cardiac Stress Tests
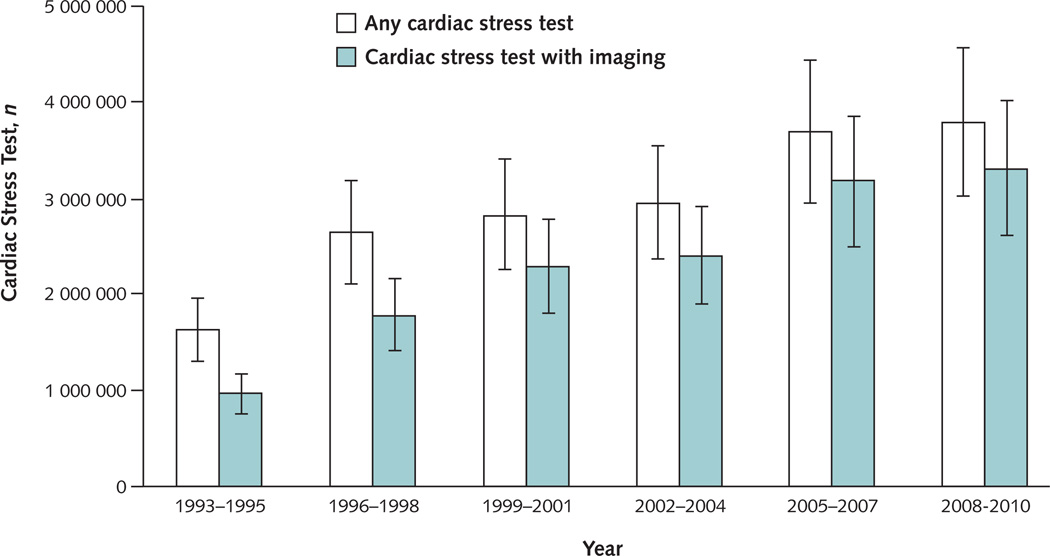
Over the 18-year period, the average annual rate of ambulatory visits in the US resulting in a cardiac stress test being ordered or performed increased from 28 per 10,000 visits among adults without CHD in 1993–1995, to 42 per 10,000 visits in 2001–2003, to 45 per 10,000 visits in 2008–2010 (Table 1). Using the NAMCS and NHAMCS survey weights, these rates correspond to a total of 1.6 million (95% CI, 1.3–2.0) visits per year in 1993–1995, 3.2 million (95% CI, 2.6–3.8) visits per year in 2001–2003, and 3.8 million (95% CI, 3.0–4.6) visits per year in 2008–2010 (Table 1 and Figure 1). Overall, there was a trend toward more frequent testing over time in unadjusted analyses (P<0.01) but this finding was not significant after adjusting for patient characteristics, clinical risk factors, and provider characteristics (P=0.134). In particular, an increase over time in the proportion of patients who were men, between the age of 45 and 64, privately insured or insured by Medicare, seeing cardiologists or other non-primary care physicians, or diagnosed with hypertension, dyslipidemia, diabetes, or obesity, accounted for the trend.
Table 1.
U.S. Ambulatory Care Visits Resulting in Cardiac Stress Test Order or Performance, by Demographic and Clinical Characteristics, 1993–2010*
| Annual Average, 1993–1995¶ | Annual Average, 2001–2003‖ | Annual Average, 2008–2010‡ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Weighted No. in Thous.§ |
Test Rate per 10,000† |
95% CI | Weighted No. in Thous.§ |
Test Rate per 10,000† |
95% CI | Weighted No. in Thous.§ |
Test Rate per 10,000† |
95% CI | P for trend, unadj. |
P for trend, adj. |
OR, trend |
aOR, trend |
| All visits | 1,635 | 28 | (23 to 33) | 3,205 | 42 | (35 to 50) | 3,805 | 45 | (36 to 53) | 0.004 | 0.134 | 1.02 | 1.01 |
| Age, yrs | |||||||||||||
| 18–44 | 309 | 12 | (7 to 17) | 788 | 29 | (18 to 40) | 527 | 19 | (12 to 25) | 0.012 | 0.27 | 1.03 | 1.02 |
| 45–64 | 833 | 50 | (38 to 63) | 1,594 | 61 | (48 to 74) | 1,964 | 62 | (49 to 75) | 0.89 | 0.69 | 1.00 | 1.00 |
| 65–79 | 462 | 36 | (24 to 48) | 705 | 44 | (31 to 57) | 1,114 | 62 | (44 to 79) | 0.013 | 0.008 | 1.03 | 1.04 |
| >80 | 67 | 15 | (7 to 24) | 111 | 19 | (8 to 29) | 174 | 25 | (16 to 34) | 0.031 | 0.143 | 1.06 | 1.04 |
| Sex | |||||||||||||
| Female | 820 | 22 | (16 to 28) | 1,390 | 29 | (23 to 35) | 1,974 | 37 | (29 to 45) | 0.003 | 0.045 | 1.03 | 1.02 |
| Male | 815 | 38 | (30 to 47) | 1,815 | 64 | (49 to 79) | 1,831 | 58 | (45 to 71) | 0.078 | 0.61 | 1.02 | 1.01 |
| Race/ethnicity | |||||||||||||
| Non-Hispanic white | 1,218 | 30 | (23 to 37) | 2,012 | 44 | (34 to 53) | 1,964 | 44 | (34 to 53) | 0.056 | 0.89 | 1.02 | 1.00 |
| Non-Hispanic black | 128 | 25 | (10 to 40) | 306 | 54 | (26 to 83) | 216 | 30 | (15 to 45) | 0.20 | 0.41 | 1.03 | 1.02 |
| Hispanic | 77 | 19 | (8 to 30) | 209 | 36 | (17 to 54) | 305 | 44 | (26 to 63) | 0.04 | 0.141 | 1.05 | 1.04 |
| Other/unknown | 211 | 23 | (11 to 36) | 678 | 37 | (24 to 49) | 1,319 | 51 | (31 to 70) | 0.073 | 0.123 | 1.03 | 1.03 |
| Insurance | |||||||||||||
| Private | 742 | 35 | (26 to 44) | 2,127 | 51 | (40 to 63) | 2,171 | 49 | (38 to 59) | 0.186 | 0.81 | 1.01 | 1.00 |
| Medicare | 436 | 31 | (20 to 42) | 663 | 34 | (24 to 45) | 1,136 | 48 | (35 to 61) | 0.016 | 0.024 | 1.03 | 1.03 |
| Medicaid/Other | 421 | 26 | (16 to 35) | 287 | 26 | (13 to 39) | 404 | 33 | (16 to 50) | 0.76 | 0.46 | 1.01 | 1.01 |
| Uninsured | 65 | 11 | (6 to 16) | - | - | (- to -) | 86 | 19 | (10 to 28) | 0.012 | 0.058 | 1.06 | 1.05 |
| Region | |||||||||||||
| Northeast | 399 | 29 | (16 to 43) | 892 | 53 | (34 to 72) | 523 | 32 | (20 to 44) | 0.80 | 0.60 | 1.00 | 0.99 |
| Midwest | 292 | 22 | (12 to 32) | 801 | 49 | (33 to 65) | 722 | 38 | (25 to 51) | 0.027 | 0.193 | 1.03 | 1.01 |
| South | 503 | 28 | (18 to 39) | 926 | 35 | (22 to 48) | 1,531 | 47 | (35 to 59) | 0.05 | 0.43 | ||
| West | 442 | 32 | (22 to 42) | 586 | 36 | (23 to 48) | 1,029 | 59 | (28 to 90) | 0.22 | 0.21 | 1.03 | 1.03 |
| Office/clinic setting | |||||||||||||
| Urban | 1,244 | 26 | (21 to 32) | 2,991 | 46 | (37 to 54) | 3,555 | 47 | (38 to 57) | <0.001 | 0.027 | 1.03 | 1.02 |
| Rural | 391 | 35 | (18 to 52) | 214 | 20 | (11 to 29) | 269 | 26 | (11 to 41) | 0.31 | 0.126 | 0.98 | 0.96 |
| Physician specialty** | |||||||||||||
| Primary care | 806 | 28 | (19 to 38) | 1,614 | 41 | (30 to 53) | 1,160 | 28 | (20 to 36) | 0.93 | 0.99 | 1.00 | 1.00 |
| Cardiology | 617 | 693 | (510 to 876) | 1,264 | 767 | (568 to 966) | 2,210 | 1,089 | (841 to 1337) | 0.006 | 0.043 | 1.03 | 1.03 |
| Reason for visit | |||||||||||||
| Chest pain | 494 | 572 | (408 to 735) | 997 | 912 | (605 to 1219) | 1,085 | 1,075 | (846 to 1303) | 0.004 | 0.033 | 1.03 | 1.02 |
| Other | 1,141 | 20 | (15 to 25) | 2,209 | 29 | (23 to 36) | 2,721 | 32 | (25 to 40) | 0.006 | 0.40 | 1.03 | 1.01 |
| Smoker | |||||||||||||
| Yes | 185 | 28 | (16 to 39) | 451 | 51 | (33 to 69) | 515 | 55 | (38 to 72) | 0.059 | 0.27 | 1.03 | 1.02 |
| Unknown | 474 | 21 | (14 to 28) | 828 | 32 | (21 to 43) | 1,057 | 35 | (19 to 51) | 0.42 | 0.80 | 1.01 | 1.00 |
| No | 1,015 | 35 | (27 to 43) | 1,926 | 46 | (37 to 56) | 2,233 | 49 | (39 to 59) | 0.006 | 0.051 | 1.03 | 1.02 |
| Visit diagnosis | |||||||||||||
| Hypertension | 273 | 55 | (32 to 78) | 831 | 98 | (66 to 130) | 1,133 | 107 | (75 to 139) | 0.006 | 0.004 | 1.04 | 1.04 |
| Dyslipidemia | 141 | 121 | (73 to 169) | 397 | 123 | (60 to 186) | 620 | 120 | (81 to 159) | 0.38 | 0.74 | 0.98 | 0.99 |
| Diabetes | 117 | 36 | (18 to 53) | - | - | (- to -) | 253 | 49 | (33 to 65) | 0.30 | 0.51 | 1.03 | 1.02 |
| Obesity | 51 | 62 | (31 to 93) | - | - | (- to -) | 116 | 99 | (60 to 138) | 0.30 | 0.35 | 1.03 | 1.03 |
| Low risk visit€ | |||||||||||||
| Yes | 802 | 18 | (13 to 23) | 1,169 | 22 | (16 to 27) | 1,286 | 21 | (15 to 28) | 0.50 | 0.82 | 1.01 | 1.00 |
| No | 833 | 60 | (46 to 73) | 2,036 | 94 | (74 to 114) | 2,519 | 101 | (80 to 121) | 0.172 | 0.009 | 1.01 | 1.03 |
Abbreviations: CI, confidence interval; Avg., average; No., number; CHD, coronary heart disease; Thous., thousands; unadj., unadjusted; adj., adjusted
Includes only adults without a diagnosis of CHD. Trend analyses based on logistic regression models using all years of data, with adjustment for patient and provider characteristics. Time intervals exceed 3 years for some subgroups in order to construct reliable confidence intervals.
Cardiac stress test rate among all visits of adults without a diagnosis of CHD and falling within subgroup
Total no. of weighted visits resulting in a cardiac stress test order or performance
Time interval extends from 1993–1996 for non-Hispanic black and smoker; 1993–1997 for Hispanic and dyslipidemia; 1993–1998 for age>80 years; 1993–2001 for uninsured, diabetes, and obesity
Time interval extends from 1999–2004 for age>80 years. Data for uninsured, diabetes, and obesity captured in first and third time intervals.
Time interval extends from 2005–2010 for age>80 years; 2007–2010 for rural; 2002–2010 for uninsured, diabetes, and obesity.
Adult visits categorized as low-risk if patient was not a smoker, did not have chest pain, and had no diagnosis for hypertension, dyslipidemia, diabetes, or obesity.
Physician specialty available in NAMCS only
Figure 1.
Number of Cardiac Stress Tests Ordered or Performed for Adults Without Coronary Heart Disease in U.S. Ambulatory Care Visits, 1993–2010
Use of Imaging with Cardiac Stress Tests
Cardiac stress tests with imaging comprised an increasing portion of all stress tests ordered or performed over the 18-year period, rising from 59% (95% CI, 50%–69%) in 1993–1995 to 87% (95% CI, 82%–92%) in 2001–2003 and 87% (95% CI, 82%–93%) in 2008–2010 (Appendix Table 1). This trend was not explained by changes in population demographics, risk factors, or provider characteristics (P<0.001 for time trend after adjustment).
In our assessment of appropriateness, we found that 30% of cardiac stress tests with imaging (a total of approximately 972,500 tests annually in 2005–2010) and 14% of cardiac stress tests without imaging (a total of approximately 67,500 tests annually in 2005–2010) were performed in patients for whom these studies were rarely appropriate. The most common principal diagnosis in visits with inappropriate testing was hypertension. These imaging and nonimaging tests were associated with annual healthcare costs of $494 and $7.7 million, respectively, or total costs of $501 million. Based on these estimates, patients were exposed to up to 10.2 million mSv of unnecessary radiation each year from stress MPI—an amount that would result in 491 patients annually later developing cancer in their lifetime because of that test.
Time Trends in Subgroups
While trends in cardiac stress test rates were not significant after adjustment in the overall population, they remained significant in the following important subgroups: women (P=0.045), age between 65–79 years-old (P=0.008), enrolled in Medicare (P=0.024), presented with chest pain (P=0.033), saw a cardiologist (P=0.043), or had a non-low-risk visit (P<0.01) (Table 1). In contrast, in our analysis of imaging use, upward trends were present overall and in nearly every subgroup, but the trend was only significant after adjustment in white patients and in patients of other or unknown race/ethnicity (Appendix Table 1). In addition, the portion of cardiac stress tests that were performed or ordered with imaging was higher in visits with women (73%, 95% CI 61%–84%) than men (46%, 95% CI 34%–58%) in 1993–1995, but this gap was absent in 2001–2003 and afterward.
Racial/Ethnic Disparities
Over the 18-year study period, the mean number of cardiac stress tests per 10,000 visits was 41 for white patients, 38 for black patients, 33 for Hispanic patients, and 42 for patients of another or unknown race/ethnicity (Table 2). We observed a general upward trend in cardiac stress test use and use of imaging in all racial/ethnic groups (Figures 2). There was no evidence of a lower likelihood of receiving a cardiac stress test in black patients (adjusted odds ratio, aOR 0.91, 95% CI 0.69 to 1.21). Cardiac stress test rates were lower in Hispanics patients, but this finding did not reach statistical significance at the 5% level (aOR 0.75, 95% CI 0.55 to 1.02). In a sensitivity analysis, we included census data on poverty, education, and income from 2006–2010; limited our model to only patients whose race/ethnicity were known; and used the imputed ethnicity in each year the NAMCS and NHAMCS provided these data. These changes did not alter our results.
Table 2.
Prevalence and Adjusted Odds of Cardiac Stress Test Order or Performance in U.S. Ambulatory Care Visits, 1993–2010
| All Ambulatory Visits | Office-based Visits Only | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted No. |
Test Rate per 10,000† |
Adjusted OR | 95% CI | P value |
Unweighted No. |
Test Rate per 10,000† |
Adjusted OR | 95% CI | P value | |
| Age, yrs | ||||||||||
| 18–44 | 582 | 19 | 1.00 | 353 | 20 | 1.00 | ||||
| 45–64 | 1,593 | 61 | 2.43 | 2.02 to 2.93 | <0.001 | 1,035 | 62 | 2.29 | 1.86 to 2.81 | <0.001 |
| 65–79 | 833 | 52 | 2.31 | 1.79 to 2.99 | <0.001 | 570 | 53 | 1.94 | 1.45 to 2.59 | <0.001 |
| >80 | 146 | 31 | 0.95 | 0.66 to 1.37 | 0.80 | 107 | 32 | 0.69 | 0.46 to 1.02 | 0.064 |
| Gender | ||||||||||
| Female | 1,592 | 31 | 0.61 | 0.54 to 0.69 | <0.001 | 1,020 | 32 | 0.60 | 0.52 to 0.68 | <0.001 |
| Male | 1,562 | 56 | 1.00 | 1,045 | 58 | 1.00 | ||||
| Ethnicity | ||||||||||
| White | 1,855 | 41 | 1.00 | 1,256 | 42 | 1.00 | ||||
| Black | 278 | 38 | 0.91 | 0.69 to 1.21 | 0.52 | 140 | 41 | 0.95 | 0.68 to 1.33 | 0.76 |
| Hispanic | 254 | 33 | 0.75 | 0.55 to 1.02 | 0.064 | 126 | 34 | 0.70 | 0.52 to 0.94 | 0.017 |
| Other/unknown | 767 | 42 | 0.97 | 0.82 to 1.15 | 0.70 | 543 | 44.0 | 0.96 | 0.80 to 1.15 | 0.63 |
| Insurance | ||||||||||
| Private | 1,626 | 47 | 1.00 | 1,186 | 48 | 1.00 | ||||
| Medicare | 876 | 43 | 0.8 | 0.65 to 0.98 | 0.036 | 606 | 44 | 0.81 | 0.64 to 1.02 | 0.07 |
| Medicaid | 228 | 22 | 0.59 | 0.41 to 0.84 | 0.004 | 65 | 24 | 0.52 | 0.33 to 0.82 | 0.005 |
| Uninsured | 161 | 15 | 0.39 | 0.28 to 0.56 | <0.001 | 49 | 14 | 0.47 | 0.31 to 0.71 | <0.001 |
| Other/unknown | 263 | 32 | 0.79 | 0.57 to 1.09 | 0.156 | 159 | 34.0 | 0.87 | 0.60 to 1.25 | 0.45 |
| Region | ||||||||||
| Northeast | 679 | 37 | 1.00 | 396 | 39 | 1.00 | ||||
| Midwest | 691 | 39 | 1.07 | 0.86 to 1.34 | 0.53 | 428 | 40 | 1.18 | 0.92 to 1.51 | 0.196 |
| South | 1,135 | 40 | 1.11 | 0.88 to 1.40 | 0.36 | 745 | 41 | 1.15 | 0.89 to 1.49 | 0.27 |
| West | 649 | 45 | 1.29 | 1.00 to 1.67 | 0.047 | 496 | 46 | 1.37 | 1.04 to 1.81 | 0.026 |
| Metropolitan statistical area | ||||||||||
| Urban | 2,857 | 41 | 1.00 | 1,869 | 43 | 1.00 | ||||
| Rural | 297 | 34 | 0.83 | 0.64 to 1.07 | 0.157 | 196 | 35 | 0.99 | 0.74 to 1.32 | 0.94 |
| Physician specialty | ||||||||||
| Primary care | - | - | 454 | 36 | 1.00 | |||||
| Cardiology | - | - | 1,494 | 901 | 14.2 | 11.3 to 17.7 | <0.001 | |||
| Other | - | - | 117 | 6 | 0.17 | 0.11 to 0.27 | <0.001 | |||
| Reason for visit | ||||||||||
| Chest pain | 1,123 | 958 | 36.3 | 31.2 to 42.25 | <0.001 | 691 | 975 | 12.2 | 9.75 to 15.24 | <0.001 |
| Other | 2,031 | 28.0 | 1.00 | 1,374 | 29.0 | 1.00 | ||||
| Smoker | ||||||||||
| Yes | 343 | 42 | 0.93 | 0.77 to 1.13 | 0.49 | 217 | 44 | 0.97 | 0.78 to 1.21 | 0.81 |
| Unknown | 1,466 | 36 | 0.94 | 0.80 to 1.12 | 0.49 | 860 | 38 | 0.99 | 0.82 to 1.2 | 0.92 |
| No | 1,345 | 45 | 1.00 | 988 | 45 | 1.00 | ||||
| Visit diagnosis¶ | ||||||||||
| Hypertension | 822 | 103 | 2.08 | 1.76 to 2.47 | <0.001 | 544 | 106 | 1.19 | 0.99 to 1.44 | 0.061 |
| Dyslipidemia | 374 | 149 | 2.50 | 1.98 to 3.15 | <0.001 | 285 | 151 | 1.69 | 1.32 to 2.17 | <0.001 |
| Diabetes | 213 | 44 | 0.69 | 0.51 to 0.92 | 0.011 | 103 | 44 | 0.76 | 0.55 to 1.05 | 0.095 |
| Obesity | 101 | 84 | 1.97 | 1.43 to 2.69 | <0.001 | 68 | 87 | 1.39 | 0.94 to 2.06 | 0.097 |
Abbreviations: CI, confidence interval; OR, odds ration; No., number; CHD, coronary heart disease
Includes only adults without a diagnosis of CHD. Logistic regression models adjusted for patient and provider characteristics.
Cardiac stress test rate among all visits of adults without a diagnosis of CHD and falling within subgroup
Reference for each diagnosis category includes all visits without the diagnosis category
Figure 2.
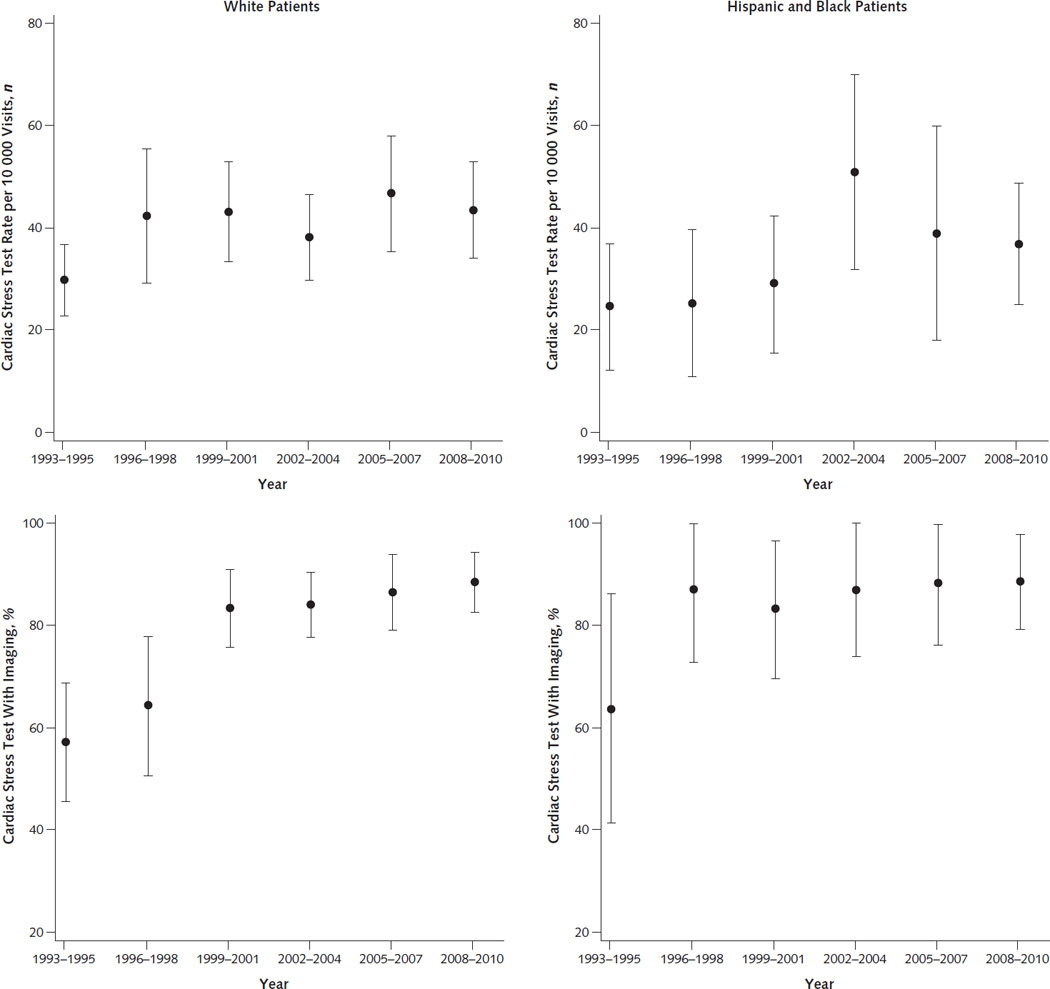
Rate of Cardiac Stress Tests Ordered or Performed for Adults Without Coronary Heart Disease and Percentage of Cardiac Stress Tests Ordered or Performed with Imaging in U.S in U.S. Ambulatory Care Visits, by Race/Ethnicity, 1993–2010
Error bars represent 95% CIs. Top. Rate of tests ordered or performed for adults without coronary heart disease. Bottom. Percentage of tests ordered or performed with imaging.
Other factors associated with the likelihood of undergoing or being referred for cardiac stress testing included being a woman (aOR 0.61 compared to men, 95% CI 0.54 to 0.69), being uninsured (aOR 0.39 compared to patients with private insurance, 95% CI 0.28 to 0.56) having Medicaid (aOR 0.59, 95% CI 0.41 to 0.84), presenting with chest pain (aOR 36.3, 95% CI 31.2 to 42.2), seeing a cardiologist (aOR 14.2, 95% CI 11.3 to 17.7), or having hypertension, dyslipidemia, or obesity. Factors associated with patients receiving imaging versus nonimaging cardiac stress tests included being a woman (aOR 1.43 compared to men, 95% CI 1.04 to 1.97) and having hypertension (aOR 1.95, 95% CI 1.27 to 2.99), among others (Appendix Table 2).
Discussion
In this analysis of national trends in cardiac stress tests performed or ordered among adults without a visit diagnosis of CHD, we provide novel evidence that national growth in cardiac stress test use can largely be explained by changes in population demographics, clinical risk factors, and provider characteristics rather than changes in physician ordering behavior. In contrast to overall growth, the brisk increase in the use of imaging in cardiac stress tests was largely unexplained by these factors, and a substantial portion of these tests were for patients for whom imaging is rarely appropriate. Our examination of racial/ethnic disparities in cardiac stress testing uncovered little evidence for a difference in the likelihood of physicians using cardiac stress tests in black or Hispanic patients compared to white patients. This suggests that physician decision-making around cardiac stress test use does not contribute to health disparities in cardiovascular disease, though our study cannot assess the burden of unmet need among at-risk patients not visiting physicians.
Concerns about overutilization or cost-ineffective use of cardiac stress testing, particularly when performed with imaging, are widespread,(1) and they have spurred intense research,(13–15, 31, 32) payer policy changes,(4, 5) and professional society action.(6, 7) The diagnostic performance and positive predictive value of cardiac stress testing have also been questioned.(33) As part of the Choosing Wisely campaign, cardiac stress testing is specifically mentioned in statements issued by the American College of Physicians,(11) American Academy of Family Physicians,(10) American College of Cardiology,(6) and American Society of Nuclear Cardiology.(9) Because of limitations in the clinical data reported in the NAMCS and NHAMCS, we are constrained in our ability to determine whether national cardiac stress test patterns at any time in our study represent underuse, optimal use, or overuse, based on appropriateness guidelines.(34) However, we can conclude that growth in cardiac stress test use in several patient populations, including women, Medicare enrollees, patients between 65–79 years old, and patients with at least one clinical risk factor for CHD, cannot be fully explained by changes over time in population demographics, risk factors, or provider characteristics. This finding in women may reflect growing recognition of and remediation for gender disparities in cardiac testing and procedures, a controversial issue that has received substantial attention over the past 20 years.(16–19, 35, 36) Our findings in Medicare enrollees are consistent with other studies that have reported rapid growth in cardiac stress test use in this population.(13, 14) Furthermore, among the factors that accounted for the increasing overall trends, many were patient/clinical characteristics associated with a higher risk of CHD, but the independent contributions of private insurance and Medicare insurance do suggest that trends in cardiac stress test use are at least partially driven by nonclinical—and possibly, economic—motivations.
Our findings clearly demonstrate that the use of cardiac stress tests with imaging has grown rapidly over the past 18 years nationally and in nearly every subgroup. However, it is important to note that, in light of our overall findings, this largely represents a substitution of imaging for non-imaging tests. Therefore, tracking cardiac stress imaging alone may be a misleading metric for utilization. However, because the majority of cardiac stress tests with imaging are performed with nuclear imaging,(27, 37, 38) which is both expensive and exposes patients to radiation, this trend may be a legitimate quality concern. Moreover, we found that nearly one-third of cardiac imaging stress tests were ordered or performed for patients in whom it is rarely appropriate. In addition to increasing population cancer risk, their associated cost of $494 million annually is important because, in the long run, it reduces society’s ability to provide other health services or expand access to care for uninsured and underserved populations. Our results therefore support and further refine concerns voiced by professional societies and insurers about utilization.
Currently, robust efforts are underway to reduce inappropriate testing and radiation exposure from necessary tests, with leadership from several professional organizations, including the American College of Cardiology, American Society of Nuclear Cardiology, and American College of Radiology.(9, 39) These organizations are actively working to reduce risks and harms related to radiological technologies.
Racial and ethnic disparities in the diagnosis and treatment of cardiovascular disease and its risk factors are widely recognized, and reducing the burden of these disparities was a major focus of Healthy People 2010.(40) Our findings suggest that racial/ethnic disparities that have previously been reported in the utilization of preventive and therapeutic cardiovascular interventions, such as cholesterol screening,(41) hypertension treatment,(42, 43) and cardiac revascularization,(44, 45) do not appear to extend to cardiac stress testing. However, reducing disparities in the burden of cardiovascular disease remains an important concern.
Our study has several imitations. The NAMCS and NHAMCS provide only a limited amount of clinical information on each patient visit, and we were often unable to characterize a patient’s chest pain as typical or atypical, nor were we able to distinguish cardiac imaging stress tests performed with echocardiography from those performed with cardiac magnetic resonance perfusion scanning or nuclear imaging. Our estimates of attributable cancers and costs could also be erroneously inflated if double counting of cardiac stress tests occurred due to tests that were ordered at one office visit and then provided at another office visit (instead of being provided separately from an office visit, such as in a stress test lab), with both visits counted in the survey. To help address this concern, we estimated the portion of stress tests ordered by cardiologists (since primary care doctors are less likely to perform a stress test in the office) seeing patients who had been seen within the past 12 months. This portion was 27.8% in 2005–2010, and we believe that visits specifically meeting the requirements for double counting within this subset are uncommon and do not contribute significantly to error in our study. In addition, patients who decide not to complete ordered tests would also inflate our estimates. However, our approach to identifying inappropriate tests was conservative and most likely underestimated their overall frequency. Related to this, our findings could be sensitive to errors or anomalies in data collection or reporting, though our focus on trends may reduce the effect of these artifacts, provided they remained relatively stable over time. Because our study is cross-sectional, we also do not have information on patient outcomes. In addition, visits only allow three diagnoses, so risk factors are likely underreported for many patients and conditions. As previously noted, race/ethnicity were missing for many patients, and were determined by an observer instead of the patient. However, our findings did not change substantially after using multiple approaches to address this limitation. In addition, our assessment of appropriateness used stringent criteria to identify cardiac stress tests that were rarely appropriate and may have therefore underestimated the prevalence of inappropriate testing.
In conclusion, growth in cardiac stress testing can largely be explained by changes in population demographics, risk factors, and provider characteristics, but growth in the use of imaging cannot. Cardiac stress test use should continue to be examined, and understanding the incremental value of this widely disseminated technology may uncover insights into optimal approaches to further reduce the morbidity and mortality from coronary heart disease.
Supplementary Material
Acknowledgments
Dr. Joseph Ladapo had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Ladapo's work is supported by a K23 Career Development Award (1 K23 HL116787-01A1) from the National Heart, Lung, and Blood Institute (NHLBI) and he serves as a consultant to CardioDx, Inc. Dr. Blecker’s work is supported by National Center for Advancing Translational Sciences (NCATS) grant KL2 TR000053. This study was not supported by any other external funding sources.
Footnotes
Reproducible Research Statement
Study protocol: Not available. Statistical code: Available from Dr. Ladapo (joseph.ladapo@nyumc.org) with written use agreement. Data: freely available at http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm
There are no other conflicts of interest to report.
References
- 1.Shaw LJ, Marwick TH, Zoghbi WA, Hundley WG, Kramer CM, Achenbach S, et al. Why all the focus on cardiac imaging? JACC Cardiovasc Imaging. 2010;3(7):789–794. doi: 10.1016/j.jcmg.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Gibbons RJ, Miller TD, Hodge D, Urban L, Araoz PA, Pellikka P, et al. Application of appropriateness criteria to stress single-photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol. 2008;51(13):1283–1289. doi: 10.1016/j.jacc.2007.10.064. [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ. Medical imaging in the 21st century--getting the best bang for the rad. The New England journal of medicine. 2010;362(10):943–945. doi: 10.1056/NEJMe1000802. [DOI] [PubMed] [Google Scholar]
- 4.Levin DC, Rao VM, Parker L, Frangos AJ, Sunshine JH. Bending the curve: the recent marked slowdown in growth of noninvasive diagnostic imaging. AJR. American journal of roentgenology. 2011;196(1):W25–W29. doi: 10.2214/AJR.10.4835. [DOI] [PubMed] [Google Scholar]
- 5.Iglehart JK. Health insurers and medical-imaging policy--a work in progress. N Engl J Med. 2009;360(10):1030–1037. doi: 10.1056/NEJMhpr0808703. [DOI] [PubMed] [Google Scholar]
- 6.Choosing Wisely. American College of Cardiology: Imaging tests for heart disease: when you need them--and when you don't. ABIM Foundation. [Accessed July 8, 2013]; http://www.choosingwisely.org/doctor-patient-lists/imaging-tests-for-heart-disease/. [Google Scholar]
- 7.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 8.Rao VM, Levin DC. The overuse of diagnostic imaging and the Choosing Wisely initiative. Ann Intern Med. 2012;157(8):574–576. doi: 10.7326/0003-4819-157-8-201210160-00535. [DOI] [PubMed] [Google Scholar]
- 9.Choosing Wisely. American Society of Nuclear Cardiology: Stress tests for chest pain: When you need an imaging test--and when you don't. ABIM Foundation. [Accessed July 8, 2013]; http://www.choosingwisely.org/doctor-patient-lists/stress-tests-for-chest-pain/. [Google Scholar]
- 10.Choosing Wisely. American Academy of Family Physicians: EKGs and exercise stress tests: When you need them for heart disease--and when you don't. ABIM Foundation. [Accessed July 8, 2013]; http://www.choosingwisely.org/doctor-patient-lists/ekgs-and-exercise-stress-tests/. [Google Scholar]
- 11.Choosing Wisely. American College of Physicians: Stress tests for chest pain: When you need an imaging test--and when you don't. ABIM Foundation. [Accessed July 8, 2013]; http://www.choosingwisely.org/doctor-patient-lists/american-college-of-physicians/. [Google Scholar]
- 12.Will JC, Loustalot F, Hong Y. National Trends in Visits to Physician Offices and Outpatient Clinics for Angina 1995 to 2010. Circulation: Cardiovascular Quality and Outcomes. 2014;7(1):110–117. doi: 10.1161/CIRCOUTCOMES.113.000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113(3):374–379. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circulation. Cardiovascular quality and outcomes. 2012;5(1):31–36. doi: 10.1161/CIRCOUTCOMES.111.961813. [DOI] [PubMed] [Google Scholar]
- 15.Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE, et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. Journal of the American College of Cardiology. 2013;61(10):1054–1065. doi: 10.1016/j.jacc.2012.11.056. [DOI] [PubMed] [Google Scholar]
- 16.Shaw LJ, Miller DD, Romeis JC, Kargl D, Younis LT, Chaitman BR. Gender differences in the noninvasive evaluation and management of patients with suspected coronary artery disease. Annals of internal medicine. 1994;120(7):559–566. doi: 10.7326/0003-4819-120-7-199404010-00005. [DOI] [PubMed] [Google Scholar]
- 17.Miller TD, Roger VL, Hodge DO, Hopfenspirger MR, Bailey KR, Gibbons RJ. Gender differences and temporal trends in clinical characteristics, stress test results and use of invasive procedures in patients undergoing evaluation for coronary artery disease. Journal of the American College of Cardiology. 2001;38(3):690–697. doi: 10.1016/s0735-1097(01)01413-9. [DOI] [PubMed] [Google Scholar]
- 18.Roger VL, Jacobsen SJ, Pellikka PA, Miller TD, Bailey KR, Gersh BJ. Gender differences in use of stress testing and coronary heart disease mortality: a population-based study in Olmsted County, Minnesota. Journal of the American College of Cardiology. 1998;32(2):345–352. doi: 10.1016/s0735-1097(98)00229-0. [DOI] [PubMed] [Google Scholar]
- 19.Chang AM, Mumma B, Sease KL, Robey JL, Shofer FS, Hollander JE. Gender bias in cardiovascular testing persists after adjustment for presenting characteristics and cardiac risk. Academic Emergency Medicine. 2007;14(7):599–605. doi: 10.1197/j.aem.2007.03.1355. [DOI] [PubMed] [Google Scholar]
- 20.Cohen MC, Stafford RS, Misra B. Stress testing: national patterns and predictors of test ordering. American heart journal. 1999;138(6 Pt 1):1019–1024. doi: 10.1016/s0002-8703(99)70065-7. [DOI] [PubMed] [Google Scholar]
- 21.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feinstein M, Ning H, Kang J, Bertoni A, Carnethon M, Lloyd-Jones DM. Racial differences in risks for first cardiovascular events and noncardiovascular death: the Atherosclerosis Risk in Communities study, the Cardiovascular Health Study, and the Multi-Ethnic Study of Atherosclerosis. Circulation. 2012;126(1):50–59. doi: 10.1161/CIRCULATIONAHA.111.057232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics (U.S.) Ambulatory Health Care Data: NAMCS and NHAMCS description. [Accessed June 4, 2013];Centers for Disease Control and Prevention. 2013 http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 24.National Center for Health Statistics (U.S.) NAMCS Public-use Data File Documentation. Centers for Disease Control and Prevention; 2009. [Accessed June 4, 2013];2009 ftp://ftp.cdc.gov/pub/health_statistics/NCHS/Dataset_Documentation/NAMCS/doc09pdf.
- 25.Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 Multimodality Appropriate Use Criteria for the Detection and Risk Assessment of Stable Ischemic Heart DiseaseA Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2014;63(4):380–406. doi: 10.1016/j.jacc.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Hsiao WC, Braun P, Dunn D, Becker ER. Resource-based relative values. An overview. JAMA. 1988;260(16):2347–2353. [PubMed] [Google Scholar]
- 27.Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA. 2011;306(19):2128–2136. doi: 10.1001/jama.2011.1652. [DOI] [PubMed] [Google Scholar]
- 28.Berrington de Gonzalez A, Kim KP, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: projected population cancer risks from current levels of use in the United States. Circulation. 2010;122(23):2403–2410. doi: 10.1161/CIRCULATIONAHA.110.941625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Einstein AJ, Weiner SD, Bernheim A, Kulon M, Bokhari S, Johnson LL, et al. Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA. 2010;304(19):2137–2144. doi: 10.1001/jama.2010.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Center for Health Statistics (U.S.) Ambulatory Health Care Data: NAMCS and NHAMCS, Reliability of Estimates. Centers for Disease Control and Prevention. [Accessed June 4, 2013];2013 http://www.cdc.gov/nchs/ahcd/ahcd_estimation_reliability.htm.
- 31.Ladapo JA, Hoffmann U, Bamberg F, Nagurney JT, Cutler DM, Weinstein MC, et al. Cost-effectiveness of coronary MDCT in the triage of patients with acute chest pain. AJR. Am. J. Roentgenol. 2008;191(2):455–463. doi: 10.2214/AJR.07.3611. [DOI] [PubMed] [Google Scholar]
- 32.Ladapo JA, Jaffer FA, Hoffmann U, Thomson CC, Bamberg F, Dec W, et al. Clinical outcomes and cost-effectiveness of coronary computed tomography angiography in the evaluation of patients with chest pain. Journal of the American College of Cardiology. 2009;54(25):2409–2422. doi: 10.1016/j.jacc.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 33.Ladapo JA, Blecker S, Elashoff MR, Federspiel JJ, Vieira DL, Sharma G, et al. Clinical implications of referral bias in the diagnostic performance of exercise testing for coronary artery disease. J Am Heart Assoc. 2013;2(6):e000505. doi: 10.1161/JAHA.113.000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brindis RG, Douglas PS, Hendel RC, Peterson ED, Wolk MJ, Allen JM, et al. ACCF/ASNC appropriateness criteria for single-photon emission computed tomography myocardial perfusion imaging (SPECT MPI): a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group and the American Society of Nuclear Cardiology endorsed by the American Heart Association. Journal of the American College of Cardiology. 2005;46(8):1587–1605. doi: 10.1016/j.jacc.2005.08.029. [DOI] [PubMed] [Google Scholar]
- 35.Lauer MS, Pashkow FJ, Snader CE, Harvey SA, Thomas JD, Marwick TH. Gender and referral for coronary angiography after treadmill thallium testing. American Journal of Cardiology. 1996;78(3):278–283. doi: 10.1016/s0002-9149(96)00277-9. [DOI] [PubMed] [Google Scholar]
- 36.Shaw LJ, Vasey C, Sawada S, Rimmerman C, Marwick TH. Impact of gender on risk stratification by exercise and dobutamine stress echocardiography: long-term mortality in 4234 women and 6898 men. Eur Heart J. 2005;26(5):447–456. doi: 10.1093/eurheartj/ehi102. [DOI] [PubMed] [Google Scholar]
- 37.The Myocardial Perfusion Imaging Market Guide (U.S.). Supplement to the U.S. Imaging Market Guide. Malvern, PA: Arlington Medical Resources, Inc; 2007. [Google Scholar]
- 38.The Echocardiography Market Guide (U.S.). Supplement to the U.S. Imaging Market Guide. Malvern, PA: Arlington Medical Resources, Inc; 2009. [Google Scholar]
- 39.ACR Appropriateness Criteria. Reston VA: American College of Radiology; 2014. [Accessed January 28, 2014]. http://www.acr.org/Quality-Safety/Appropriateness-Criteria. [Google Scholar]
- 40.Centers for Disease Control and Prevention. Healthy People. [Accessed July 10, 2013];2010 http://www.cdc.gov/nchs/healthy_people/hp2010.htm.
- 41.Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162(8):929–935. doi: 10.1001/archinte.162.8.929. [DOI] [PubMed] [Google Scholar]
- 42.Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113(5):647–656. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 43.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 44.Lillie-Blanton M, Maddox TM, Rushing O, Mensah GA. Disparities in cardiac care: rising to the challenge of Healthy People 2010. Journal of the American College of Cardiology. 2004;44(3):503–508. doi: 10.1016/j.jacc.2004.04.043. [DOI] [PubMed] [Google Scholar]
- 45.Bradley EH, Herrin J, Wang Y, McNamara RL, Webster TR, Magid DJ, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292(13):1563–1572. doi: 10.1001/jama.292.13.1563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.