Abstract
Study Objectives:
School terms and vacations represent naturally occurring periods of restricted and extended sleep opportunities. A cognitive model of the relationships among objective sleep, subjective sleep, and negative mood was tested across these periods, with sleep-specific (i.e., dysfunctional beliefs and attitudes about sleep) and global (i.e., dysfunctional attitudes) cognitive vulnerabilities as moderators.
Design:
Longitudinal study over the last week of a school term (Time-E), the following 2-w vacation (Time-V), and the first week of the next term (Time-S).
Setting:
General community.
Participants:
146 adolescents, 47.3% male, mean age = 16.2 years (standard deviation ± 1 year).
Interventions:
N/A.
Measurements and Results:
Objective sleep was measured continuously by actigraphy. Sociodemographics and cognitive vulnerabilities were assessed at Time-E; subjective sleep, negative mood (anxiety and depressive symptoms), and academic stress were measured at each time point. Controlling for academic stress and sex, subjective sleep quality mediated the relationship between objective sleep and negative mood at all time points. During extended (Time-V), but not restricted (Time-E and Time-S) sleep opportunity, this mediation was moderated by global cognitive vulnerability, with the indirect effects stronger with higher vulnerability. Further, at Time-E and Time-V, but not Time-S, greater sleep-specific and global cognitive vulnerabilities were associated with poorer subjective sleep quality and mood, respectively.
Conclusions:
Results highlighted the importance of subjective sleep perception in the development of sleep related mood problems, and supported the role of cognitive vulnerabilities as potential mechanisms in the relationships between objective sleep, subjective sleep, and negative mood. Adolescents with higher cognitive vulnerability are more susceptible to perceived poor sleep and sleep related mood problems. These findings have practical implications for interventions.
Citation:
Bei B, Wiley JF, Allen NB, Trinder J. A cognitive vulnerability model of sleep and mood in adolescents under naturalistically restricted and extended sleep opportunities. SLEEP 2015;38(3):453–461.
Keywords: adolescents, anxiety, attitudes, beliefs, cognitive vulnerability, depression, mood, sleep, sleep restriction, vacation
INTRODUCTION
There is growing recognition that a significant number of adolescents obtain insufficient and poor quality sleep,1,2 especially during school weekdays.3 Major contributing factors include maturational processes that produce a progressive delay in the circadian timing of sleep and a reduction in homeostatic drive across adolescence,4 early school start times,3 and psychosocial factors such as less parental control over bedtime and the emergence of cultural social interests and obligations.4,5 Insufficient and poor sleep has been linked to psychosocial and physical consequences such as impaired cognitive performance,6 obesity,7 and increased risks for mood problems8 in adolescents.
The Sleep-Mood Relationship in Adolescents
The adolescent literature on the bidirectional relationship between sleep and negative mood has focused on two areas: sleep differences among adolescents with and without a mood/ anxiety disorder, and whether sleep restriction/deprivation affects mood. Sleep can be assessed objectively using polysomnography (PSG) or actigraphy, and subjectively using self-report questionnaires or sleep diary. Depressive9 or anxiety10,11 disorders have typically been associated with longer sleep onset latency (SOL), more awakenings, and shorter rapid eye movement latency. In adolescents, lower subjective sleep quality and quantity are cross-sectionally associated with negative mood,12–14 and longitudinally with increased risk of mood problems.15,16 Studies that have integrated objective with subjective measurements of sleep are rare, and results are somewhat inconsistent. For example, among community adolescents, subjective sleepiness, but not actigraphy-measured sleep duration or its variability, was related to anxiety/ depressive symptoms.8 Nevertheless, longer PSG-measured SOL during childhood/adolescence predicted adulthood depression,17 and experimentally restricting sleep in adolescents worsened mood and emotional regulation,18–21 suggesting an etiological role for sleep in negative mood.
A Cognitive Vulnerability Model of the Sleep-Mood Relationship
From a neurocognitive perspective the prefrontal cortex (PFC), which is important for cognitive control and affect regulation,22 undergoes ongoing development during adolescence.23 The negative effects of sleep deprivation on the functioning of the PFC24 has been proposed as a potential neurocognitive mechanism underlying the affective consequences of inadequate sleep.25,26
However, few studies have explored the mechanisms underlying the relationship between sleep and negative mood from a psychological perspective. The stronger relationship between subjective sleep and mood when compared to that between objective sleep and mood8,27,28 suggests that psychological factors that contribute to personal experiences of sleep might play important roles in the sleep-mood relationship. One such psychological factor is cognitive vulnerability—erroneous beliefs, cognitive biases, or patterns of thought that predispose individuals to a higher likelihood of psychopathology.29 The importance of these cognitive processes in the development and maintenance of mood problems is supported by strong empirical evidence in both adults30 and adolescents31–34 yet they are rarely applied to understand the sleep-mood relationship.
Sleep-Specific Cognitive Vulnerability
When dysfunctional beliefs and attitudes are related to sleep, they are sleep specific, and are most commonly assessed using the Dysfunctional Beliefs and Attitudes about Sleep (DBAS) Scale.35 The contribution of DBAS as a sleep-specific cognitive vulnerability to sleep complaints is elegantly illustrated in Harvey's cognitive model of insomnia,36 which proposes that individuals with insomnia tend to be preoccupied by sleep and the daytime consequences of poor sleep. This excessive, negatively toned, cognitive activity triggers selective attention and monitoring of sleep related threat cues, and can lead to overestimation of sleep deficit. Few studies have assessed DBAS among adolescents; however, those that did have found that higher DBAS scores were associated with longer actigraphy-assessed SOL,37 as well as shorter subjectively assessed nighttime sleep and more regular napping.38 These findings suggest a link between DBAS and poor sleep in adolescents, and a potential role of DBAS in sleep perception and sleep safety behaviors (e.g., napping).
Global Cognitive Vulnerability
When dysfunctional beliefs and attitudes are not focused on a specific behavioral or experiential domain, they are global. Based on Beck's widely studied cognitive model,39 early adverse events foster negative attitudes and biases about self, world, and future, that are integrated into the cognitive organization in the form of schemas, which become activated by later life stressors that impinge on the specific cognitive vulnerability, leading to systematic negative biases at the core of depression.40
There is some evidence that global cognitive vulnerabilities might play a role in the association between sleep complaints and negative mood. For example, in adolescents, sleep problems have been associated with cognitive factors (cognitive errors and control beliefs) that were closely linked to anxiety and depression.41 Among young female adults,42 insufficient sleep has been shown to be correlated with melancholic symptoms such as “I thought my life had been a failure” rather than “poor concentration” or “difficulty to get going”. Also, a recent study in older adults showed that hopelessness, an aspect of global cognitive vulnerability, partially mediated the effect of insomnia on depressive symptoms.43
Restricted and Extended Sleep Opportunities
In adolescents, school days are associated with restricted sleep opportunities12,44 and vacation periods with extended sleep opportunities.3 It is important to study the roles of cognitive vulnerability in the sleep-mood relationship during both school and vacation periods because (1) they represent two distinctive sleep-wake patterns common to most adolescents, (2) naturalistic changes in sleep opportunity over school terms and vacation are associated with changes in sleep quality such as SOL3 that are relevant to mood,17 and (3) this allows examination of cognitive vulnerabilities under two conditions in which school schedule, an exogenous nonpsychological factor, is the main contributing factor to differences in sleep opportunity.
The Current Study
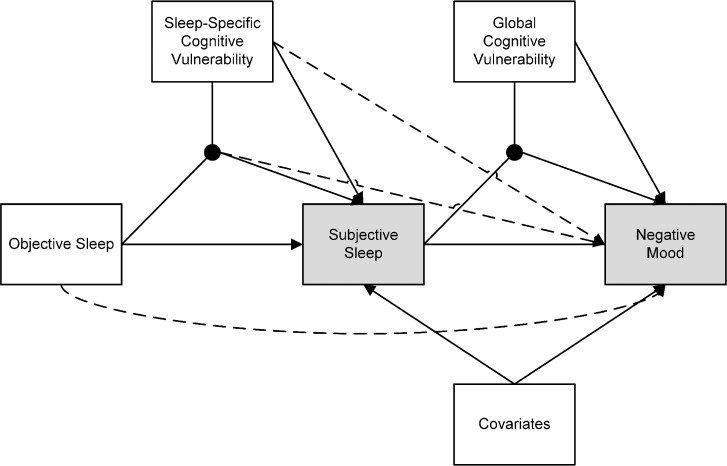
In this study, a cognitive vulnerability model of the relationships between objective sleep, subjective sleep, and negative mood (see Figure 1) was proposed and tested in a single model during both school terms and vacations. It was hypothesized that:
Subjective sleep perception would mediate the relationship between objective sleep and negative mood.
Based on the cognitive model of insomnia,36 higher sleep-specific cognitive vulnerability would be associated with worse subjective sleep, and that the relationship between objective sleep and subjective sleep would be moderated by sleep-specific cognitive vulnerability.
Based on the general cognitive model of depression,39 higher global cognitive vulnerability would be associated with worse mood, and that the relationship between subjective sleep and negative mood would be moderated by global cognitive vulnerability. This part of the model proposes that perceived poor sleep functions as a form of life stress and interacts with biased cognitions in vulnerable individuals to lead to negative mood.
Figure 1.
Analytic model of the relationships among objective sleep, subjective sleep, and cognitive vulnerabilities. Gray boxes indicate dependent variables, white boxes indicate independent variables, black dots represent the interaction of variables, lines with arrows represent directional regression paths from one variable to another, dotted lines represent paths that were not specifically hypothesized but were necessary to allow the possibility that effects were not mediated by subjective sleep but rather were direct effects on mood.
Academic stress and sex were included as covariates as the prior literature has shown that higher academic stress45,46 and being female47,48 were associated with mood problems in adolescents. Academic stress was controlled because it was theorized that it is a major non-sleep related contributor to the mood differences between the school and vacation periods.
METHODS
Participants
Participants were 146 adolescents (47.26% males, age mean ± standard deviation = 16.18 ± 1.00 y) enrolled in y 10–12 of Australian secondary colleges, and were primarily of Australian (59.6%) or Asian (26.7%) descent. One female was excluded because the presence of multiple sleep disorders with daily naps, and data from the first week were excluded from one female because of physical illness. A small number of participants reported having a depressive, anxiety, or attention deficit hyperactivity disorder (6.16%), or sleep conditions (11.64%) such as insomnia and bruxism at the time of recruitment (see Bei et al.3 for details). No significant differences in model fit or parameter estimates were found when the hypothesized model was estimated with or without these participants. Therefore, they were not excluded to retain the representativeness of a community sample.
Procedures
Procedures were approved by the Human Research Ethics Committee of the University of Melbourne. Participants were recruited via flyers in community centers and school e-newsletters with two movie vouchers as incentives. Informed consent was obtained from participants and guardians.
Data were collected over school terms and vacations (typically 2 w in Australia), excluding summer vacations, using an actigraph and online surveys. Participants were asked to register bedtimes and rise times using the actigraph's Event Marker and wear the actigraph on the non-dominant hand continuously for 4 w: the last school term week (Time-E [End]), through the 2-w vacation (Time-V [Vacation]), and the first week of the following term (Time-S [Start]). The measures of subjective sleep, negative mood, and academic stress referred to the preceding week, and were collected over Time-E, Time-V (within the second week of vacation), and Time-S. Demographics and cognitive vulnerability were assessed at Time-E.
Equipment and Materials
Actigraphy
Actigraphy is widely used to study sleep patterns in adolescents,49 and provides estimates of sleep duration and quality close to that of PSG.50 Actiwatch 2 and Actiwatch-64 (Mini Mitter, Bend, OR, USA) with comparable sleep statistics51 were used with data collected at 1-min epochs and analysed based on “medium” threshold for sleep/wake detection in Actiware 5.5. The following variables were generated using Actiware software (details on data processing see Bei et al.3): total sleep time (TSTacti), sleep onset latency (SOLacti), sleep efficiency (SEacti), and percentage of wake after sleep onset (%WASOacti). For Time-E and Time-S with restricted sleep opportunity, data from Monday to Thursday (24-h cycles that started and ended on a school day) were averaged; weekend days with extended sleep opportunity were not included. Data from the Saturdays at the start to the end of the vacation were averaged for Time-V variables.
Questionnaires
Subjective Sleep: The Pittsburgh Sleep Quality Index52 (PSQI) is well validated53 and has been applied in the adolescent population to assess sleep problems with good reliability.14,54 In this study, two subjective component scores were derived using PSQI raw values. First, TSTpsqi (min) was used as the subjective sleep duration variable. Second, raw values for SOLpsqi (min), SEpsqi (%), SDpsqi (sleep disturbance; sum of items 5b–5j), SQpsqi (sleep quality; item 9), and DDpsqi (sleep related daytime dysfunction; item 7) were standardized and summed to be the subjective sleep quality (SSQ) variable. Item 8, “how much of a problem was it for you to keep up enthusiasm to get things done?” was not included to reduce overlap with negative mood.
Negative Mood: Negative mood was assessed using two well-validated scales for depressive (Center for Epidemiological Studies Depression Scale; CES-D55) and anxiety (Spence Children's Anxiety Scale; SCAS56) symptoms. The CES-D has 20 items, and has been validated for use in adolescents57; the 44-item SCAS was designed for assessing various aspects of anxiety in children and adolescents. To reduce overlap between sleep and negative mood, scores on the item “my sleep was restless” was removed from the total score of CES-D. Both scales had excellent internal consistency reliability across all time points (all Cronbach α ≥ 0.89). Correlations between the total scores of CES-D and SCAS were high across time (r ranged 0.59–0.66). This is consistent with the notion that although depression and anxiety can be reliably distinguished, they have substantial overlap.58 In this study, overall negative mood was of interest, and scales of depression and anxiety were standardized and summed within each time point to make a composite score (MOOD) where higher values indicate greater negative mood.
Cognitive Vulnerability: Sleep-specific cognitive vulnerability was assessed using the Dysfunctional Beliefs and Attitudes about Sleep Scale-16 (DBAS-16), an abbreviated form of the DBAS Scale that is well validated.59 Global cognitive vulnerability was assessed using the Dysfunctional Attitude Scale (DAS), a 40-item questionnaire that assesses assumptions and beliefs based on Beck's cognitive model,60,61 and is validated for use in adolescents.62 Higher total scores on both the DBAS-16 and the DAS indicate higher endorsement of dysfunctional beliefs. In this study, Cronbach α was 0.86 for DBAS and 0.92 for DAS.
Academic Stress: Academic stress was measured using 18 academic-specific items (e.g., “struggling to meet your own standards of performance at school”) from the 41-item Inventory of High-School Students' Recent Life Experiences.63 Participants were asked to rate from 1 to 4 how each experience had been a part of his/her life, and the 18 items were summed to create a composite where higher total scores reflect greater academic stress. The academic stress composite had excellent internal consistency reliability across time points (all Cron-bach α ≥ 0.90).
Statistical Analysis
Analytic Plan
The hypothesized model in Figure 1 was tested as a single model in two steps. First, preliminary analyses were conducted using a series of linear regression analyses to determine the specific objective and subjective sleep variables that best represented the objective and subjective concepts. Second, primary model analyses were conducted at all three time points to test the hypothesized model in Figure 1. Sex and academic stress were included as covariates. Age was considered as a covariate, but was excluded after preliminary analyses showed that it shared minimal correlations at all time points (all r's < 0.11, all P > 0.05) with all variables included in the model.
Statistical Methods
Primary analyses were estimated in a Bayesian path analysis framework,64,65 which performs excellently for mediation analysis,66 using R 3.067 and Mplus 7.068 via Mplus-Automation 0.6-2.69 Missing data were handled by using all available data, which is more efficient than listwise deletion. Outliers and normality were assessed and one outlier was removed from SOLacti and SOLpsqi at Time-V. Further, the Bayesian inference is robust to non-normality. To facilitate interpretation, continuous variables were standardized to have a mean of zero and standard deviation of one.
Minimally informative priors were used for all parameters and convergence was determined using the Gelman scale reduction factor < 1.05 from two independent chains70 with at least 5,000 iterations. Model fit was assessed using posterior predictive checks,71 which give a P value for the difference between the estimated and observed covariance matrix. A non-significant value indicates good fit. Parameter estimates are reported as the posterior medians and 95% credible intervals. Two-tailed significance tests were used and P < 0.05 was considered statistically significant.
RESULTS
Descriptive Statistics
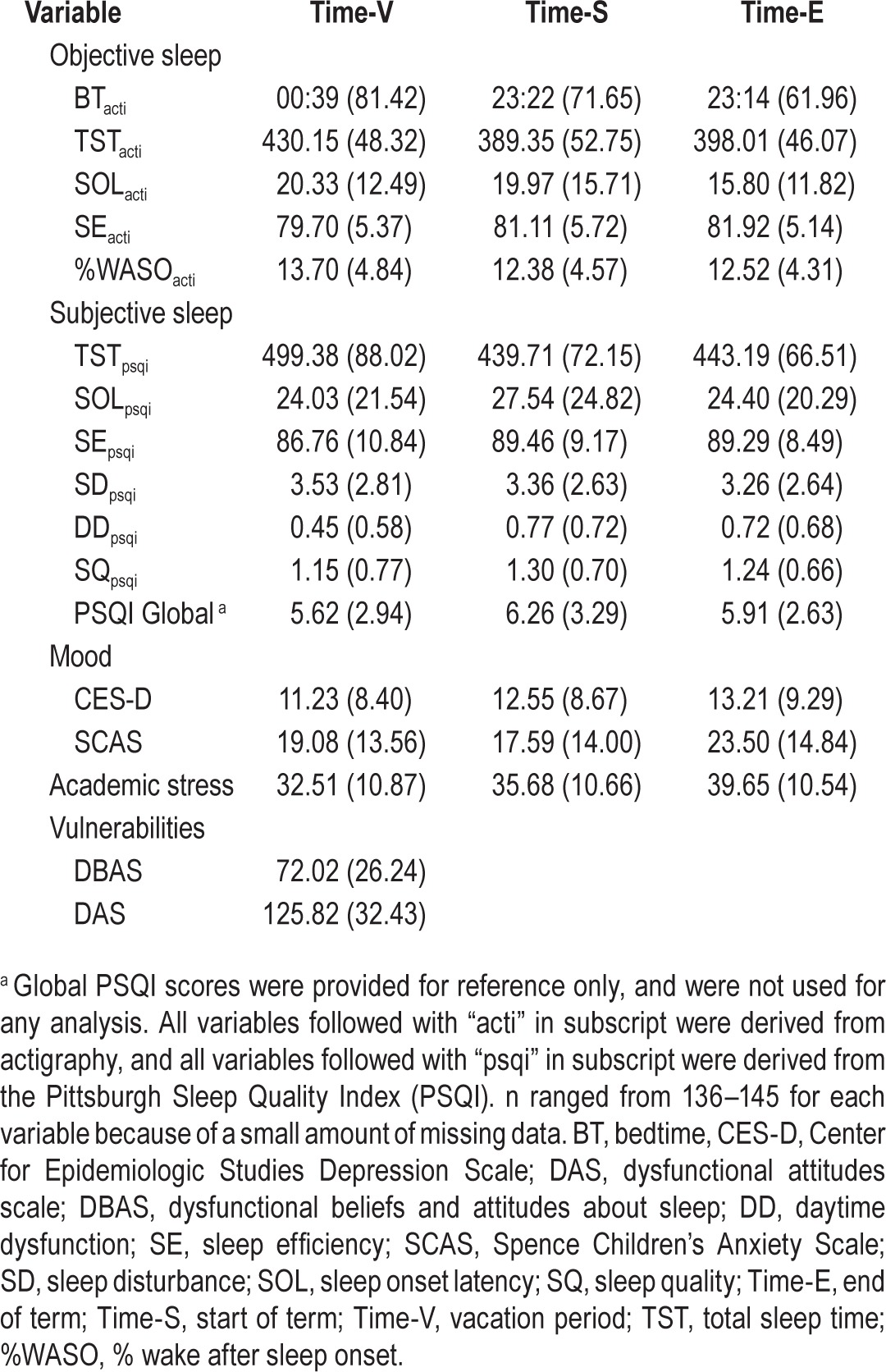
Descriptive statistics are shown in Table 1. Differences in objective sleep variables between time points have been reported previously.3 The data indicate that compared to Time-V with extended sleep opportunity, Time-S and Time-E were associated with substantial sleep restriction with significantly shorter sleep duration, shorter SOL, and more consolidated sleep as measured by actigraphy. Linear mixed models showed that compared to school term, Time-V was associated with significantly shorter TSTpsqi, higher DDpsqi, and lower SEpsqi; however, SDpsqi and SOLpsqi were not significantly different across time points. Depressive symptoms increased significantly from Time-V to Time-E, whereas anxiety symptoms decreased from Time-V to Time-S, but were highest at Time-E. Overall the sample was healthy, with 90.41%, 89.04%, and 84.25% scoring under the clinical cutoff on the CES-D,72 and 91.78%, 90.41%, and 81.51% within the normal range on the SCAS56 at Time-V, Time-S, and Time-E respectively.
Table 1.
Means (standard deviations) of objective sleep, subjective sleep, mood, academic stress, and cognitive vulnerability variables.
The rate of missing data on actigraphy was low (91.40% of all daily data were available) and was caused by technical faults, inconvenience of wearing the actigraph during certain activities, potential participant noncompliance, and a lost acti-graph. Objective sleep variables based on averaged actigraphy daily values had ≤ 6.20% missing at any time point. The rate of missing data for questionnaires was similarly low (≤ 4.14%) across all time points.
Preliminary Analyses
To identify which sleep variables uniquely explained negative mood at each time point, MOOD was simultaneously regressed on SSQ and TSTpsqi, and on BTacti, TSTacti, SOLacti, SEacti, and %WASOacti, controlling for sex and academic stress. SSQ was the only statistically significant subjective sleep variable (all P < 0.001), whereas no actigraphy variable was significant (all P > 0.08). Next, SSQ was simultaneously regressed on BTacti, TSTacti, SOLacti, SEacti, and %WASOacti to examine whether objective sleep variables uniquely explained SSQ. Across all time points, SOLacti was the only significant explanatory variable (all P < 0.05), with higher SOLacti being associated with worse SSQ. Therefore, SOLacti was used for objective sleep and SSQ for subjective sleep.
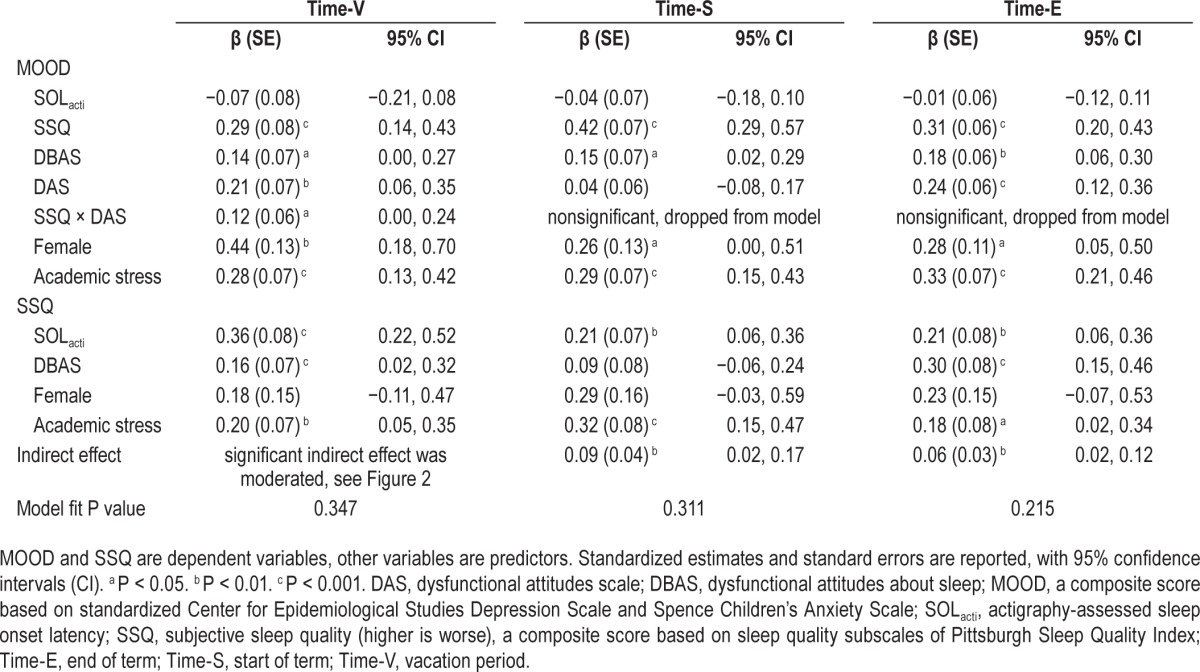
Primary Model Analyses
The full model shown in Figure 1 was tested at all three time points with good model fit (see results in Table 2). The interaction of SOLacti with DBAS was not a significant predictor of SSQ or MOOD at any time point (all P > 0.05) and was therefore dropped in the final models. The interaction of SSQ with DAS did not significantly predict MOOD at Time-S or Time-E, and this path was dropped from the model at Time-S and Time-E. No other paths from the model were dropped.
Table 2.
Results of the cognitive vulnerability model tested at Time-V, Time-S, and Time-E.
The Mediating Role of Subjective Sleep (Hypothesis 1)
Across all time points after controlling for academic stress and sex, SOLacti was significantly associated with SSQ, such that if SOLacti was longer by one standard deviation, SSQ was worse by 0.21 to 0.36 standard deviations (all P < 0.01). Although SOLacti was not significantly associated with MOOD, worse SSQ was significantly associated with more negative MOOD across all time points (all P < 0.001).
There was a significant indirect effect of SOLacti on MOOD via SSQ at Time-S (β = 0.09, P = 0.002) and Time-E (β = 0.06, P = 0.008), such that longer SOLacti was associated with higher SSQ, which in turn was associated with more negative MOOD. The indirect effect was also significant at Time-V; as this significant mediation effect was qualified by moderation, it is discussed under Hypothesis 3. Therefore, Hypothesis 1, that subjective sleep mediates the relationship between objective sleep and negative mood, was supported at all three time points.
The Role of DBAS (Hypothesis 2)
The direct effect of DBAS on SSQ was significant at Time-V (P = 0.028) and Time-E (P < 0.001), and higher DBAS was associated with worse SSQ. The direct effect of DBAS on SSQ was not significant at Time-S (P = 0.23). The interaction of DBAS and SOLacti on SSQ was not significant at all time points. These results suggest that DBAS did not moderate the relationship between objective and subjective sleep, but made significant direct contributions to subjective sleep at Time-V and Time-E. This partially confirms Hypothesis 2.
The Role of DAS (Hypothesis 3)
The direct effect of DAS on MOOD was significant at Time-V and Time-E (P < 0.01), and higher DAS was associated with more negative mood. The direct effect of DAS on MOOD was not significant at Time-S (P > 0.05).
At Time-V (but not Time-V or Time-E), there was a significant SSQ by DAS interaction, such that the association between SSQ and MOOD was stronger with higher DAS scores (more vulnerable). Also at Time-V, the significant mediating effect of SSQ between SOLacti and MOOD was moderated by DAS, such that the indirect effect was stronger for individuals with higher vulnerability (higher DAS scores). The indirect effects of SOLacti on MOOD via SSQ across a range of DAS values are shown in Figure 2. The indirect effect is statistically significant for DAS raw scores ≥ 98.22, when the 95% confidence interval does not include zero. In this sample, the range of DAS was from 60 to 221, with 115 participants falling above the 98.22 cutoff on DAS where the indirect effect is significant.
Figure 2.
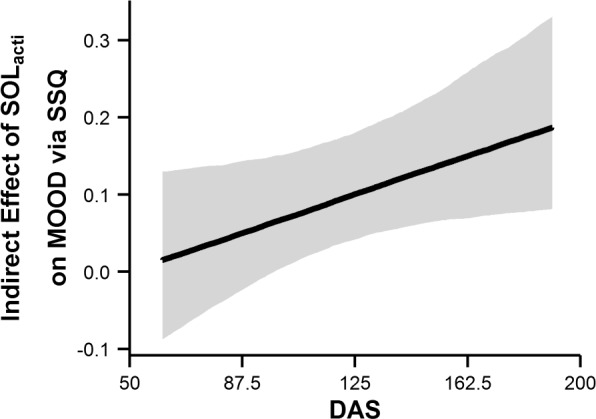
Line represents the indirect effect of SOLacti on MOOD via SSQ at each value of DAS. The shaded region represents 95% credible intervals. When the interval does not include 0, the indirect effect is statistically significant at P < 0.05. DAS, dysfunctional attitudes scale; MOOD, a composite score; SOLact, actigraphy-assessed sleep onset latency; SSQ, subjective sleep quality.
Thus, the hypothesis that global cognitive vulnerability (i.e., DAS) moderates the relationship between sleep perception and negative mood was supported for extended but not restricted sleep opportunity. DAS also made significant direct contributions to negative mood at Time-V and Time-E.
Covariates
At all time points, higher academic stress was significantly associated with worse SSQ (all P < 0.05), whereas the effect of sex on SSQ was not significant. Sex and academic stress had moderate and significant effects on MOOD across all time points, such that being female (all P < 0.05) and having higher academic stress (all P < 0.001) were associated with more negative MOOD.
DISCUSSION
Findings suggest that the cognitive vulnerability model proposed in Figure 1 can be useful in understanding the relationship between sleep and negative mood in adolescents over both restricted and extended sleep opportunities.
Subjective Sleep, Objective Sleep, and Mood
At all time points, actigraphy-measured SOL was the only objective variable that made significant, unique contributions to SSQ. This suggests that the presleep period and ease of sleep onset are key aspects of sleep experience upon which adolescents base their sleep perception, and are critical to their evaluation of overall sleep quality. The finding from the preliminary analysis that SSQ, but not objective sleep, was significantly associated with negative mood at all time points is consistent with the current understanding in both adolescent8 and adult27 literature. The finding that during both restricted and extended sleep opportunities, SSQ mediated the relationship between objective sleep and negative mood highlighted an important mechanistic role of perceived sleep quality in sleep related mood problems among adolescents.
Sleep-Specific Cognitive Vulnerability
In this study, DBAS as a sleep-specific cognitive vulnerability was not found to be a moderator between objective and subjective sleep, but a direct contributor to SSQ after controlling for academic stress and sex. The significant association between higher DBAS and worse SSQ at Time-E and Time-V is consistent with findings in adults that individuals with higher DBAS tend to have more sleep complaints.36,73 Findings in this study suggested that sleep-specific cognitive vulnerability might predispose adolescents to perceive poorer sleep quality during both restricted and extended sleep opportunities.
The effect of DBAS on SSQ was stronger at Time-E compared to Time-V. It is possible that although the effects of academic stress on SSQ was controlled, concerns regarding school-related sleep restriction and its daytime consequences at the end of a school term might have contributed to a stronger effect of DBAS compared to during vacation periods. The absence of a significant effect of DBAS on SSQ at Time-S can be interpreted in light of substantial changes in sleep-wake patterns at the start of a new school term: attitudes and beliefs might play a more important role at Time-V and Time-E when sleep-wake schedules were more stably established, compared to at Time-S when there was an abrupt advance in sleep timing and significant sleep restriction as adolescents transitioned from extended to restricted sleep opportunity.3 Thus, sleep parameters might be more strongly affected by changes in externally imposed sleep schedules.
Global Cognitive Vulnerability
Consistent with Beck's cognitive model,39 after controlling for SSQ and covariates, higher dysfunctional attitudes were associated with more negative mood at Time-E and Time-V. Similar to the findings for DBAS and SSQ, the absence of a significant effect of DAS on MOOD at Time-S might be caused by other factors associated with the transition from extended to restricted sleep opportunity having greater effect on mood than dysfunctional beliefs.
During extended (Time-V) but not restricted (Time-S or Time-E) sleep opportunity, DAS moderated the relationship between SSQ and negative mood. In addition, DAS moderated the significant indirect effects of SOLacti on negative mood via SSQ, such that greater endorsement on dysfunctional attitudes was associated with a significantly stronger relationship between SSQ and negative mood, as well as a stronger mediating effect of SSQ. In other words, when sleep opportunity is unconstrained, subjective sleep perception is of particular relevance to negative mood among cognitively vulnerable adolescents, and they were more likely to experience negative mood upon perceiving poor sleep. Adolescents with higher global cognitive vulnerability were more likely to engage in unhelpful thinking processes. Extended sleep opportunity may be permissive of these processes during time in bed, leading to perceived poor sleep, as well as facilitating associations amongst bedtime, poor sleep, and negative emotional experiences; in contrast, restricted sleep opportunity and subsequently shortened SOL during the school term3 might mitigate the effect of DAS on the sleep-mood association.
In this study, SSQ mediated the relationship between objective sleep and negative mood in nearly 80% of the sample with higher DAS, suggesting that for the majority of adolescents, global cognitive vulnerability might play a role in the etiology of sleep related mood problems.
Covariates
Consistent with the existing literature, at all time points higher academic stress45,46 and being female47,48 were associated with negative mood after controlling for SSQ; higher academic stress was also associated with poorer SSQ. These results highlight that multiple factors, including both sleep and non-sleep related factors, collectively contribute to adolescents' psychological well-being during school terms and vacations.
Limitations
First, the relations among variables within each time point were cross-sectional, limiting the strength of causal inference. Second, potential overestimation of wakefulness by actigraphy has recently been noted in adolescents.74 However, if this were to be present, it would contribute to the absolute values of some actigraphy variables, and be less likely to affect their association with other measures. Third, the lack of normative data in adolescents impeded the computation of a global score for PSQI that represented overall sleep quality. This was overcome by using self-report TST in minutes, and summing standardized raw subscale scores to quantify overall sleep quality. Fourth, only one aspect of global cognitive vulnerability, dys-functional attitudes, was assessed, and other factors, such as attributional style75 and coping strategies76 were not examined. In addition, other psychological factors that might be relevant to adolescents' sleep and mood, such as positive affect77 and presleep arousal78 were not examined. Fifth, participants being older adolescents who are relatively healthy raises the caveat that results might not be generalizable to younger adolescents or a clinical population.
Strengths
This is, to the best of our knowledge, the first study to have tested a cognitive vulnerability model of the relationships among objective sleep, subjective sleep, and negative mood in adolescents under both restricted and extended sleep conditions. Conceptually, the integration of theories and empirical evidence from both sleep and psychological sciences helped examine not just the association between sleep and negative mood, but also its underlying mechanisms. Methodologically, a naturalistic design and an unselected community sample suggest that findings in this study are likely to reflect adolescents' everyday experiences with good generalizability. Repeated measures conducted across school terms and vacations allowed for the examination of the cognitive vulnerability model in two main parts of an academic year with distinct sleep-wake patterns. Appropriate statistical modelling also strengthened testing of the hypothesized model.
Implications
By examining cognitive vulnerabilities as important moderators of the links between sleep and negative mood, this study helped better understand the psychological processes underlying sleep related mood problems. Findings raise the possibility that cognitive vulnerability might be a shared risk factor for the development of both sleep problems and emotional disorders.
There are several practical implications: (1) Compared to actual sleep duration, perceived sleep quality played a more important role in sleep related mood problems. A balanced attitude toward sleep, integrating the importance of adequate sleep, as well as normalizing some degrees of sleep restriction without depicting sleep loss as necessarily being a threat to well-being, might be helpful and appropriate in adolescents, particularly those who have sleep onset difficulties. (2) The mediating role of perceived sleep quality provides support to the notion that sleep complaints may be a risk factor,79 as well as play a maintaining role80 in the development of emotional disorders. Interventions that aim to improve sleep, particularly the subjective experience of sleep, might have beneficial effects on existing mood symptoms,14,81 as well as preventive effects on the development of future mood problems. (3) This study provides empirical support for therapeutically targeting cognitive vulnerability as a risk factor for sleep complaints and sleep related mood problems. Identifying and targeting individuals who are vulnerable to sleep related mood problems (e.g., existing sleep onset difficulties, high cognitive vulnerability) might enhance effectiveness of sleep interventions in adolescents.
DISCLOSURE STATEMENT
This was not an industry supported study. This work was supported by the Melbourne School of Psychological Sciences at the University of Melbourne, Australia. There is no off-label or investigational use in this study. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- BT
bedtime
- CES-D
Center for Epidemiologic Studies Depression Scale
- DAS
dysfunctional attitudes scale
- DBAS
Dysfunctional Beliefs and Attitudes about Sleep
- DD
daytime dysfunction
- MOOD
a composite score based on standardized Center for Epidemiological Studies Depression Scale and Spence Children's Anxiety Scale
- PFC
prefrontal cortex
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- SCAS
Spence Children's Anxiety Scale
- SD
sleep disturbance
- SE
sleep efficiency
- SOL
sleep onset latency
- SQ
sleep quality
- SSQ
subjective sleep quality
- Time-E
end of term
- Time-S
start of term
- Time-V
vacation period
- TST
total sleep time
- WASO
wake after sleep onset
REFERENCES
- 1.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12:110–8. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Roberts RE, Roberts CR, Xing Y. Restricted sleep among adolescents: prevalence, incidence, persistence, and associated factors. Behav Sleep Med. 2011;9:18–30. doi: 10.1080/15402002.2011.533991. [DOI] [PubMed] [Google Scholar]
- 3.Bei B, Allen NB, Nicholas CL, Dudgeon P, Murray G, Trinder J. Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents. J Sleep Res. 2014;23:107–17. doi: 10.1111/jsr.12080. [DOI] [PubMed] [Google Scholar]
- 4.Carskadon MA. Factors influencing sleep patterns of adolescents. In: Carskadon MA, editor. Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. New York: Cambridge University Press; 2002. pp. 4–26. [Google Scholar]
- 5.van den Bulck J. Adolescent use of mobile phones for calling and for sending text messages after lights out: results from a prospective cohort study with a one-year follow-up. Sleep. 2007;30:1220–3. doi: 10.1093/sleep/30.9.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 7.Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127:e345–52. doi: 10.1542/peds.2010-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore M, Kirchner HL, Drotar D, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34:1175–83. doi: 10.1093/jpepsy/jsp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rao U, Dahl RE, Ryan N, et al. Heterogeneity in EEG sleep findings in adolescent depression: unipolar versus bipolar clinical course. J Affect Disord. 2002;70:273–80. doi: 10.1016/s0165-0327(01)00396-2. [DOI] [PubMed] [Google Scholar]
- 10.Rapoport J, Elkins R, Langer DH, et al. Childhood obsessive-compulsive disorder. Am J Psychiatry. 1981;138:1545–54. doi: 10.1176/ajp.138.12.1545. [DOI] [PubMed] [Google Scholar]
- 11.Forbes EE, Bertocci MA, Gregory AM, et al. Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:148–55. doi: 10.1097/chi.0b013e31815cd9bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Short MA, Gradisar M, Lack LC, Wright HR, Dohnt H. The sleep patterns and well-being of Australian adolescents. J Adolesc. 2013;36:103–10. doi: 10.1016/j.adolescence.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep. 2010;33:97–106. doi: 10.1093/sleep/33.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bei B, Byrne ML, Ivens C, et al. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early Interv Psychiatry. 2013;7:213–20. doi: 10.1111/j.1751-7893.2012.00382.x. [DOI] [PubMed] [Google Scholar]
- 15.Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37:239–44. doi: 10.5665/sleep.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glozier N, Martiniuk A, Patton PG, et al. Short sleep duration in prevalent and persistent psychological distress in young adults: the DRIVE study. Sleep. 2010;33:1139–45. doi: 10.1093/sleep/33.9.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goetz RR, Wolk SI, Coplan JD, Ryan ND, Weissman MM. Premorbid polysomnographic signs in depressed adolescents: a reanalysis of EEG sleep after longitudinal follow-up in adulthood. Biol Psychiatry. 2001;49:930–42. doi: 10.1016/s0006-3223(00)01092-1. [DOI] [PubMed] [Google Scholar]
- 18.Dagys N, McGlinchey EL, Talbot LS, Kaplan KA, Dahl RE, Harvey AG. Double trouble? The effects of sleep deprivation and chronotype on adolescent affect. J Child Psychol Psychiatry. 2012;53:660–7. doi: 10.1111/j.1469-7610.2011.02502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGlinchey EL, Talbot LS, Chang K-H, Kaplan KA, Dahl RE, Harvey AG. The effect of sleep deprivation on vocal expression of emotion in adolescents and adults. Sleep. 2011;34:1233–41. doi: 10.5665/SLEEP.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10:831–41. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiatry. 2013;55:180–90. doi: 10.1111/jcpp.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davidson RJ. Anxiety and affective style: role of prefrontal cortex and amygdala. Biol Psychiatry. 2002;51:68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- 23.Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann N Y Acad Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- 24.Yoo S-S, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep — a prefrontal amygdala disconnect. Curr Biol. 2007;17:R877–8. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Telzer EH, Fuligni AJ, Lieberman MD, Galván A. The effects of poor quality sleep on brain function and risk taking in adolescence. Neuroimage. 2013;71:275–83. doi: 10.1016/j.neuroimage.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silk JS, Vanderbilt-Adriance E, Shaw DS, et al. Resilience among children and adolescents at risk for depression: mediation and moderation across social and neurobiological contexts. Dev Psychopathol. 2007;19:841–65. doi: 10.1017/S0954579407000417. [DOI] [PubMed] [Google Scholar]
- 27.Bei B, Milgrom J, Ericksen J, Trinder J. Subjective perception of sleep, but not its objective quality, is associated with immediate postpartum mood disturbances in healthy women. Sleep. 2010;33:531–8. doi: 10.1093/sleep/33.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baker FC, Sassoon SA, Kahan T, et al. Perceived poor sleep quality in the absence of polysomnographic sleep disturbance in women with severe premenstrual syndrome. J Sleep Res. 2012;21:535–45. doi: 10.1111/j.1365-2869.2012.01007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freeman A, Felgoise S. Encyclopedia of Cognitive Behavior Therapy. New York: Springer; 2005. [Google Scholar]
- 30.Scher CD, Scher CD, Ingram RE, Ingram RE, Segal ZV. Cognitive reactivity and vulnerability: empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clin Psychol Rev. 2005;25:487–510. doi: 10.1016/j.cpr.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33:809–18. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Lewinsohn PM, Joiner TE, Rohde P. Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. J Abnorm Psychol. 2001;110:203–15. doi: 10.1037//0021-843x.110.2.203. [DOI] [PubMed] [Google Scholar]
- 33.Abela JRZ, Sullivan C. A test of Beck's cognitive diathesis-stress theory of depression in early adolescents. J Early Adolesc. 2003;23:384–404. [Google Scholar]
- 34.Lakdawalla Z, Hankin BL, Mermelstein R. Cognitive theories of depression in children and adolescents: a conceptual and quantitative review. Clin Child Fam Psychol Rev. 2007;10:1–24. doi: 10.1007/s10567-006-0013-1. [DOI] [PubMed] [Google Scholar]
- 35.Morin CM. Dysfunctional beliefs and attitudes about sleep: preliminary scale development and description. The Behavior Therapist. 1994 Summer;:163–4. [Google Scholar]
- 36.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40:869–93. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 37.Ng AS, Ng AS, Dodd HF, et al. The relationship between parent and child dysfunctional beliefs about sleep and child sleep. J Child Fam Stud. 2012;22:827–35. [Google Scholar]
- 38.Gradisar M, Dohnt H, Wright H, et al. Adolescent napping behavior: dysfunctional cognitions and negative affect. Sleep Biol Rhythms. 2008;6:260–3. [Google Scholar]
- 39.Beck AT. Cognitive models of depression. J Cogn Psychother. 1987;1:5–37. [Google Scholar]
- 40.Beck AT. The evolution of the cognitive model of depression and its neurobiological correlates. Am J Psychiatry. 2008;165:969–77. doi: 10.1176/appi.ajp.2008.08050721. [DOI] [PubMed] [Google Scholar]
- 41.Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress Anxiety. 2009;26:503–12. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- 42.Regestein Q, Natarajan V, Pavlova M, Kawasaki S, Gleason R, Koff E. Sleep debt and depression in female college students. Psychiatry Res. 2010;176:34–9. doi: 10.1016/j.psychres.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 43.Sadler P, Sadler P, McLaren S, McLaren S, Jenkins M, Jenkins M. A psychological pathway from insomnia to depression among older adults. Int Psychogeriatr. 2013;25:1375–83. doi: 10.1017/S1041610213000616. [DOI] [PubMed] [Google Scholar]
- 44.Olds T, Maher C, Blunden S, Matricciani L. Normative data on the sleep habits of Australian children and adolescents. Sleep. 2010;33:1381–8. doi: 10.1093/sleep/33.10.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ang RP, Huan VS. Relationship between academic stress and suicidal ideation: testing for depression as a mediator using multiple regression. Child Psychiatry Hum Dev. 2006;37:133–43. doi: 10.1007/s10578-006-0023-8. [DOI] [PubMed] [Google Scholar]
- 46.Spangler G, Pekrun R, Kramer K, Hofmann H. Students' emotions, physiological reactions, and coping in academic exams. Anxiety Stress Coping. 2002;15:413–32. [Google Scholar]
- 47.Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB. Gender differences in anxiety disorders and anxiety symptoms in adolescents. J Abnorm Psychol. 1998;107:109–17. doi: 10.1037//0021-843x.107.1.109. [DOI] [PubMed] [Google Scholar]
- 48.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–43. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 49.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15:259–67. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 50.Meltzer L, Walsh C, Traylor J. Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep. 2012;35:159–66. doi: 10.5665/sleep.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Philips Respironics. Equivalence of activity recordings and derived sleep statistics [Internet]. minimitter.com. 2008. [cited 2012 Apr 8]. Available from: http://www.minimitter.com/downloads/researchreports.pdf.
- 52.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 53.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 54.Zhou H-Q, Shi W-B, Wang X-F, et al. An epidemiological study of sleep quality in adolescents in South China: a school-based study. Child Care Health Dev. 2012;38:581–7. doi: 10.1111/j.1365-2214.2011.01300.x. [DOI] [PubMed] [Google Scholar]
- 55.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psyc Meas. 1977;1:385–401. [Google Scholar]
- 56.Spence SH. A measure of anxiety symptoms among children. Behav Res Ther. 1998;36:545–66. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- 57.Radloff LS. The use of the center for epidemiologic studies depression scale in adolescent and young adults. J Youth Adolesc. 1991;20:149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 58.Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–36. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 59.Morin CM, Vallières A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16) Sleep. 2007;30:1547–54. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weissman AN, Beck AT. Development and validation of the Dysfunctional Attitude Scale: a preliminary investigation. Paper presented at the meeting of the Association for the Advancement of Behavior Therapy; 1978; Chicago. [Google Scholar]
- 61.Weissman AN. The Dysfunctional Attitude Scale: a validation study. Diss Abstr Int. 1979;40:1389B–90B. [Google Scholar]
- 62.Prenoveau JM, Zinbarg RE, Craske MG, Mineka S, Griffith JW, Rose RD. Evaluating the invariance and validity of the structure of dysfunctional attitudes in an adolescent population. Assessment. 2009;16:258–73. doi: 10.1177/1073191108324519. [DOI] [PubMed] [Google Scholar]
- 63.Kohn PM, Milrose JA. The inventory of high-school students recent life experiences: a decontaminated measure of adolescents hassles. J Youth Adolesc. 1993;22:43–55. [Google Scholar]
- 64.Christensen R, Johnson W, Branscum A, Hanson TE. Bayesian Ideas and Data Analysis. Boca Raton, FL: Chapman & Hall/CRC Press; 2011. [Google Scholar]
- 65.Muthén BO, Asparouhov T. Bayesian structural equation modeling: a more flexible representation of substantive theory. Psychol Methods. 2012;17:313–35. doi: 10.1037/a0026802. [DOI] [PubMed] [Google Scholar]
- 66.Yuan Y, MacKinnon DP. Bayesian mediation analysis. Psychol Methods. 2009;14:301. doi: 10.1037/a0016972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. Retrieved from http://www.R-project.org/ [Google Scholar]
- 68.Muthén LK, Muthén BO. Mplus User's Guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 2013. [Google Scholar]
- 69.Hallquist M, Wiley JF. MplusAutomation: Automating Mplus Model Estimation and Interpretation (Version 0.6-2) 2013. Retrieved from http://cran.r project.org/package=MplusAutomation.
- 70.Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. 1998;7:434–55. [Google Scholar]
- 71.Gelman A, Meng X-L, Stern H. Posterior predictive assessment of model fitness via realized discrepancies. Statistica Sinica. 1996;6:733–60. [Google Scholar]
- 72.Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. J Am Acad Child Adolesc Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 73.Morin CM, Stone J, Stone J, et al. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993;8:463–7. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- 74.Short MA, Gradisar M, Lack LC, Wright H, Carskadon MA. The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Med. 2012;13:378–84. doi: 10.1016/j.sleep.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 75.Calvete E, Villardón L, Estévez A. Attributional style and depressive symptoms in adolescents: an examination of the role of various indicators of cognitive vulnerability. Behav Res Ther. 2008;46:944–53. doi: 10.1016/j.brat.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 76.Sadeh A, Keinan G, Daon K. Effects of stress on sleep: the moderating role of coping style. Health Psychol. 2004;23:542–5. doi: 10.1037/0278-6133.23.5.542. [DOI] [PubMed] [Google Scholar]
- 77.Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64:409–15. doi: 10.1016/j.jpsychores.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 78.Gregory AM, Willis TA, Wiggs L, Harvey AG STEPS Team. Presleep arousal and sleep disturbances in children. Sleep. 2008;31:1745–7. doi: 10.1093/sleep/31.12.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 80.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36:1059–68. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]