Abstract
Background
Despite the wide application of open reduction and internal fixation with locking plates for the treatment of proximal humeral fractures, the surgical invasive approach remains controversial. This study aimed to evaluate the pros and cons of the minimally invasive lateral approach for the treatment of proximal humeral fracture (PHF) in comparison with the deltopectoral approach.
Material/Methods
All patients who sustained a PHF and received open reduction and internal fixation (ORIF) surgery with locking plate through either minimally invasive subacromial approach or conventional deltopectoral approach between January 2008 and February 2012 were retrospectively analyzed. Patients were divided into the conventional group and min-group according to the surgical incision. Surgery-related information, postoperative radiography, complications, and shoulder functional measurement scores in a 2-year follow-up were collected and evaluated.
Results
Ninety-one patients meeting the inclusion criteria were included in this study. We observed a significant difference in both surgery time (81.8±18.3 vs. 91.0±18.4) (p=0.021) and blood loss (172±54.2 vs. 205±73.6) (p=0.016) between the min-group and conventional group. Compared to the conventional group, the min-group had significantly better Constant-Murley score and DASH score at early follow-up (p<0.05) and higher patients satisfaction rate (8.1±1.1 vs. 7.6±1.2) (p= 0.019). The multiple linear regression analysis indicated that age, PHF types, surgical groups, surgery time, and blood loss have significant effect on the activity of affected shoulder in both abduction and forward flexion (p<0.05) except for gender factor. While larger range of movement of the affected shoulder, mainly in the 2-part and 3-part fractures, was observed in the min-group, the conventional group obtained better movement in the 4-part fractures.
Conclusions
The minimally invasive lateral approach is the optimal alternative for the treatment of Neer’s type 2 and 3 proximal humerus fractures.
MeSH Keywords: Internal Fixators; Retrospective Studies; Shoulder Fractures; Surgical Procedures, Minimally Invasive
Background
Except for distal radius fractures and those adjacent to the hip joint, proximal humerus fractures (PHF) are the most common fractures of the extremity, accounting for 4–5% of all fractures, with a rising incidence rate in recent years [1,2]. However, the therapeutic option of PHF is still controversial. A large number of interventions are applied routinely, ranging from conservative treatment to shoulder joint arthroplasty [3]. In the last decade, locking plate technology has been developed and heralded as a breakthrough for the treatment of PHF, especially in osteoporotic patients [4]. We therefore hypothesized that open reduction and internal fixation (ORIF) with a locking plate, which leads to a good clinical and functional outcome for even the most complex fractures [5], is a helpful option in treatment of PHF.
In addition to a reliable fixation system to stabilize fractures and an adequate incision facilitating the exposure of all fracture fragments, limited soft tissue damage is another important factor for the recovery of postoperative shoulder function and for decreasing the complication rate. Given its satisfactory clinical outcome, the deltopectoral approach remains the most widely used treatment for these injuries [6,7]. Using this approach, surgeons benefit from the excellent exposure of the anterior structures, including the humeral head and lesser tuberosity, with limited concern about injuring axillary nerve branches. In addition, it facilitates an easy intraoperative conversion to arthroplasty [8]. However, this approach provides limited exposure of the posterior aspect of the proximal humerus due to the pull of the cuff muscles and the lateral aspect where the plate is placed [9]. Furthermore, excessive soft tissue stripping destroys the local blood supply and integrity of the deltoid, which may increase the risk of avascular necrosis and restrict postoperative functional recovery [7,8,10]. These limiting factors have triggered the exploration of a minimally invasive approach. A recent study showed that minimally invasive surgery (MIS) or minimally invasive plate osteosynthesis (MIPPO) for anterior ring fracture combined with pubic symphysis separation has the advantages of short operation time and less blood loss [11]. Percutaneous vertebroplasty (PV) and kyphoplasty (PK) are 2 vertebral augmentation procedures that have emerged as minimally invasive surgical options to treat painful vertebral compression fractures (VCF) during the last 2 decades. This review consists of a discussion of current research on clinical outcome of these 2 procedures, and it also sheds light on ongoing and future research to maximize the efficacy and safety of vertebral augmentation procedures [12]. This clinical operation is safe and feasible, with good therapeutic efficacy. According to the anatomic characteristics of the proximal humerus, a sub-acromial lateral minimal incision that distinctly exposes the fracture sites and facilitates reduction during surgery with limited soft issue trauma has been utilized.
This retrospective study aimed to investigate the advantages and disadvantages of the sub-acromial lateral minimally invasive approach in comparison with the conventional deltopectoral approach. We hope our results lead to the identification of a more suitable surgery incision for the treatment of PHF.
Material and Methods
Patients and inclusion criteria
We included patients aged 18 or older who had PHF and received ORIF surgery with locking plate through either the minimally invasive subacromial approach or the conventional deltopectoral approach between January 2008 and February 2012. The diagnosis and severity of PHF were determined by preoperative radiographs, including standard anteroposterior, lateral X-ray film of the shoulder, and CT scan with 3-dimensional reconstruction. Fracture type was defined according to the Neer classification system [13]. Biochemical and other medical technological reports were employed to evaluate the physical condition of the patients. The indications for surgery were defined according to the modified Neer criteria (displacement of the tuberosity of >5 mm and angulation of the head fragment of >45°) [13]. All patients had data available on preoperative and postoperative evaluations (including radiographic and biochemical assessment), statistical data of series marking system, and basic information. All the patients involved in this study had 4 follow-up evaluations during the first 2 years after surgery. This retrospective study was approved by the Institutional Review Board and was performed based on the understanding and agreement from the patients. Patients with the following situations were excluded: open, pathological fractures or refractures; pseudarthrosis; 1-part-fracture (displacement less than 30° and 5 mm); concomitant ipsilateral fractures of the distal part of the humerus or the elbow joint; time from the injury more than 4 weeks; having been treated with other therapy instead of ORIF; no prior treatment through either the minimal-invasive lateral approach or conventional deltopectoral incision; and follow-up frequency less than 4 times or a follow-up time shorter than 2 years.
Surgical techniques and physiotherapy
All the operations were performed by professor Wu X either with deltopectoral approach or with subacromial minimally invasive lateral approach. Patients were divided into 2 different groups based on their incisions, the min-group (minimally invasive surgery group) and the conventional group. Both groups of patients were placed in a beach-chair position with the affected extremity draped free and the image intensifier included in the sterile surgical field. In the conventional group, a standard deltopectoral incision (Figure 1A) starting from the lateral edge of the coracoid and 8–10 cm length along the deltopectoral groove was performed. The definitive operative procedure has been well described previously [10,14,6].
Figure 1.
The different surgical incision, locking plate placement, and the internal fixation during the operation between the 2 groups. (A) The conventional deltopectoral approach. (B) The lateral minimally invasive approach. (C) The placement of a locking plate through the minimally invasive approach. (D) The anatomic reduction, plate position, fixation, and screw length were verified as satisfactory under the C-arm image-intensified fluorocopy before the operation was finished. (E) Suture of the incision after the operation.
In the min-group, subacromial lateral laterigrade incision was used as an invasive approach, and the locking plan and incision are shown in Figure 1B. The crosscut incision was 4–5 cm in length and 1 finger below the acromion. Muscle fiber was split bluntly and carefully along the deltoid, and excessive splitting of the deltoid muscle was avoided to protect the anterior motor branch of the axillary nerve from injury. A longitudinal split was made in the deltoid and was retracted to identify the subdeltoid bursa, and the greater tuberosity and humeral fracture sites were identified. Anatomic reduction was maximally achieved via manipulation of pulling traction and leverage using a periosteal elevator. Kirschner wires were also used to facilitate reduction and to temporarily fix the fracture. After reduction and fixation were verified with C-arm image-intensified fluoroscopy, an appropriate-length locking plate (Synthes, Johnson & Johnson, USA) was safely inserted along the submuscular tunnel to prevent the axillary nerve from being trapped under the plate (Figure 1C). The plate was placed laterally between the greater and lesser tuberosity, and proximally below the apex of the greater tuberosity. Another longitudinal incision below the branch of the axillary nerve was made to visualize the distal part of the plate. Multiple-angle locking screws were used to fix the distal part of the fracture. C-arm image-intensified fluoroscopy was used again to verify the reduction, plate position, and screw length (Figure 1D). The incision was closed after irrigating the wound and hemostasis was achieved (Figure 1E).
Physiotherapy was initiated within the first week post-surgery, which is important for the recovery of shoulder function. We requested all the patients to flex their elbow joint to 90°and to use a sling for 3–4 weeks. Passive pendulum exercise of the affected shoulder was initiated 2–3 days after the operation, and the range of activity was gradually increased. After 2 weeks, positive shoulder exercise was executed and much higher strength of exercise, including superduction, abduction, post-stretch, and ante-flexion, was initiated. The time and method of all the postoperative exercises were strictly monitored by a physiotherapist.
Intraoperative and postoperative assessment method
The surgery duration and amount of bleeding during the operation were recorded. Patients were followed up radiographically and clinically with a detailed clinical evaluation and shoulder function assessed during the visit at 3, 6, 12, and 24 months post-surgery, respectively. All the patients were examined by the same surgeon in a blinded manner. At each follow-up, anteroposterior and lateral view radiographies were performed to monitor fracture healing, and the recovery of shoulder function was evaluated by measuring the shoulder functional score and range of motion of the affected shoulder. The Constant-Murley score (CMS) [15], graded as poor (0–64), moderate (65–74), good (75–85), or excellent (86–100), was used to evaluate the functional outcome of the affected shoulder in comparison with the uninjured contralateral joint. A questionnaire on disabilities of arm, shoulder, and hand (DASH) [16] score was used to evaluate any limitations in the activities of daily living. The satisfaction of the patients associated with pain, cosmetic appearance, and ability to return to work, as well as overall outcome of the affected shoulder after the operation, were investigated and graded as unsatisfied (0–6), satisfied (6–8), or very satisfied (8–10). Complications related to the operation were recorded and analyzed at the time they occurred.
Statistical analysis
SPSS 11.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The 2 independent-sample T test, chi-square test, and Mann-Whitney U test were used for examining the statistical difference in preoperative and postoperative evaluation between the 2 groups. Multiple linear regression analysis was used to evaluate the strength of associations between surgical approaches and clinical end result. The level of significance was set at 0.05.
Results
We analyzed 91 patients with PHF who met the inclusion criteria. These patients were divided into 2 groups: 39 in the min-group and 52 in the conventional group. According to the Neer classification [13], 33 patients had 2-part fractures, 43 had 3-part fractures, and 15 had 4-part fractures (Table 1). The majority of fractures were united in an average of 10 weeks (range 8–15 weeks). Statistical analysis indicated no significant difference in age, gender, or fracture type between the 2 groups (p>0.05, Table 1). The surgery duration and blood loss during the operation were 81.8±18.3 vs. 91.0±18.4 minutes and 172±54.2 vs. 205±73.6 ml, respectively, between the min-group and conventional group, and the differences were statistically significant (P values were 0.021 and 0.016 for surgery time and blood loss, respectively) (Table 1). Moreover, a significantly higher satisfaction rate was obtained from the min-group than from the conventional group (8.1±1.1 vs. 7.6±1.2, p=0.019).
Table 1.
Comprehensive general patient information and operative information in each group.
| Min-group | Traditional-group | Statistical data | |
|---|---|---|---|
| Gender | |||
| Male | 17 (43.6%) | 25 (48.1%) | χ2=0.181, P=0.695 |
| Femal | 22 (56.4%) | 27 (51.9%) | |
| Age/years | 60.2±14.4 | 61.7±13.7 | t=−0.501, P=0.617 |
| Fracture types | – | – | Z=−3.93, P=0.694 |
| 2 parts | 15 (38.5%) | 18 (34.6%) | |
| 3 parts | 18 (46.2%) | 25 (48.1%) | |
| 4 parts | 6 (15.4%) | 9 (17.3%) | |
| Operation time/min | 81.8±18.3 | 91.0±18.4 | t=−2.36, P=0.021 |
| Blood loss/ml | 172±54.2 | 205±73.6 | t=−2.46, P=0.016 |
| Satisfaction | 8.1±1.1 | 7.6±1.2 | t=2.39, P=0.019 |
| Complication rate | 2.6% | 7.7% | χ2=1.129, P=0.288 |
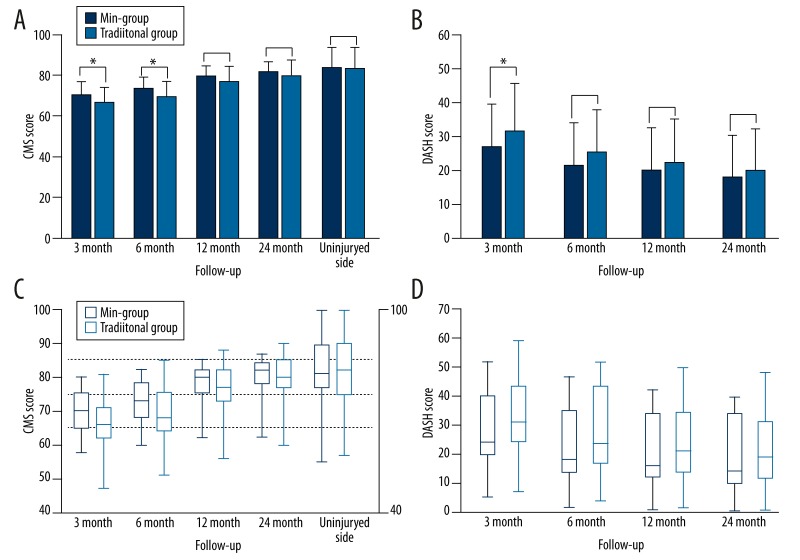
We found a statistically significant difference between the groups in the early follow-up (CMS score at 3- and 6-month follow-up, with p values of 0.015 and 0.023, respectively; DASH score at 3 months with a p value of 0.032) (Table 2, Figure 2). For most patients, we found functional recovery of the affected shoulders in a time-dependent manner (Figure 2). At the last follow-up, the mean Constant-Murley score was 80.0±6.6, and average DASH Score was 18.8±12.2. Compared with the uninjured side, no significant difference in the Constant-Murley scores of the affected shoulders was observed in the min-group (P=0.321) and conventional group (P=0.063). According to constant score, 17.6% had excellent outcome, 64.7% had good functional outcome, 13.2% had moderate outcome, and 4.4% had poor outcome.
Table 2.
Comparison of absolutely Constant-Murle score and DASH score of the injured shoulder at the variousfFollow-up visits between two groups.
| Follow-up | Min-group (M±SD) | traditional-group (M±SD) | Statistical data | |
|---|---|---|---|---|
| CMS | 3 month | 69.8±6.2 | 65.6±7.6 | Z=−2.43, P=0.015 |
| 6 month | 72.6±6.0 | 68.9±7.8 | Z=−2.27, P−0.023 | |
| 12 month | 78.6±5.0 | 75.9±7.7 | Z=−1.33, P=0.18 | |
| 24 month | 81.0±5.0 | 79.2±7.6 | Z=−0.80, P=0.43 | |
| Uninjuryed side | 83.0±10.0 | 82.4±10.5 | Z=−0.06, P=0.96 | |
| DSAH | 3 month | 26.2±12.9 | 31.1±13.8 | Z=−2.15, P=0.032 |
| 6 month | 20.9±12.7 | 24.7±12.8 | Z=−1.80, P=0.072 | |
| 12 month | 19.4±12.7 | 22.1±12.6 | Z=−1.32, P=0.19 | |
| 24 month | 17.6±12.4 | 19.6±12.0 | Z=−1.08, P=0.28 |
M±SD – mean ± standard deviation. CMS – Constant-Murle score; DASH – disabilities of arm, shoulder, and hand questionnaire score. The Mann-Whitney U test was applied to evaluate the statistical difference between two groups.
Figure 2.
(A–D) The Constant-Murley score and DASH score of the injured shoulder at the various follow-up (FU) visits between the 2 groups.
Regarding the activity of the affected shoulder, the average abduction was 135° degrees (range 58°–166°) and forward flexion was 142° (range 89°–175°) at the last follow-up (data not shown). Multiple linear regression analysis indicated that age, PHF types, surgical groups, surgery duration, and blood loss have significant impact on the activity of the affected shoulder in both abduction and forward flexion (P<0.05, Table 3). In addition, larger range of movement of the affected shoulder mainly in the 2-part and 3-part fractures was observed in the min-group, implying a better postoperative functional recovery of the affected shoulder in the min-group (Table 4). However, patients with 4-part PHF in the conventional group obtained much better postoperative range of movement of the affected shoulder in both abduction and forward flexion when compared to the min-group (108.8±14.6° vs. 120.0±11.8° in forward flexion, 105.0±14.9° vs. 112.3±17.3° in abduction).
Table 3.
The factors affecting the range of motion of affected shoulder postoperatively in both forward flexion and abduction activity.
| Gender | Age | Surgery time | Blood loss | Groups | Fracture types | |
|---|---|---|---|---|---|---|
| Forward flexion | t=0.441 p=0.66 | t=−4.47 p<0.001 | t=−2.08 p=0.041 | t=−2.14 p=0.038 | t=−2.94 p=0.004 | t=−3.19 p=0.002 |
| Abduction | t=0.345 p=0.731 | t=−3.05 p=0.003 | t=−2.03 p=0.045 | t=−2.20 p=0.028 | t=−2.50 p=0.014 | t=−2.89 p=0.005 |
The groups means of min-group and conventional group. The multiple linear regression analysis was applied to examine the statistical difference.
Table 4.
The range of movement of affected shoulder after the operation.
| Min-group (M±SD) | Conventional group (M±SD) | |
|---|---|---|
| Forward flexion | 148.7±23.3° | 136.2±16.0° |
| Type 2 | 163.7±8.2° | 147.1±9.6° |
| Type 3 | 149.4±18.4° | 134.2±15.5° |
| Type 4 | 108.8±14.6° | 120.0±11.8° |
| Abduction | 142.9±22.0° | 129.2±18.2° |
| Type 2 | 156.5±6.7° | 140.1±8.0° |
| Type 3 | 144.2±17.7° | 127.4±19.0° |
| Type 4 | 105.0±14.9° | 112.3±17.3° |
M±SD – mean ± standard deviation.
Postoperative complications occurred in 7 patients (7.7%), including 2 (5.1%) in the min-group and 5 (9.6%) in the conventional group, with no significant difference in the complication rate between the 2 groups (p=0.29) (Table 5). In the min-group, 1 patient (2.6%) had malreduction and 1 (2.6%) had internal fixation loosening, but none of the patients had axillary nerve branch damage. In the conventional group, 4 postoperative complications occurred in 5 patients, including 1 case (1.9%) of avascular necrosis, 1 case (1.9%) of nonunion, 1 case (1.9%) of internal fixation loosing, and 2 cases of limited abduction activity (3.8%). The patient who had avascular necrosis received shoulder arthroplasty surgery later on.
Table 5.
Postoperative complications and relative shoulder functional evaluation scores.
| Complications | Group | Gender | Age | Fracture type | CMS score | DASH score | Forward flexion | Abduction | Union time |
|---|---|---|---|---|---|---|---|---|---|
| Malreduction | Min- | Male | 65 | 4-part | 62 | 40 | 97° | 88° | 16w |
| IF loosening | Min- | Female | 66 | 4-part | 70 | 39 | 102° | 103° | 12 w |
| AN | Conv- | Female | 72 | 4-part | 60 | 48 | 90° | 108° | 22 w |
| IF loosening | Conv- | Male | 72 | 3-part | 81 | 29 | 115° | 114° | 14 w |
| Delay union | Conv- | Male | 68 | 4-part | 60 | 33 | 128° | 118° | 18 w |
| Limited AD | Conv- | Male | 60 | 3-part | 63 | 40 | 89° | 60° | 12 w |
| Limited AD | Conv- | Male | 48 | 4-part | 65 | 40 | 97° | 70° | 11 w |
The group means the minimal invasive group and conventional group. IF loosening means the internal fixation loosening. The AN is the abbreviation of avascular necrosis. Limited AD means limited abduction of shoulder.
Discussion
Anatomic structure of proximal humerus
To decrease the complication rate and promote functional recovery, a thorough understanding of the neurovascular, musculotendinous, and bony anatomy of the proximal humerus is required for a surgeon. The humeral head, greater tuberosity, lesser tuberosity, rotator cuff, posterior humeral circumflex artery (PCA), and axillary nerve branch are the most important anatomic structures to which attention should be paid. The greater and lesser tuberosities with intertubercular groove of the humerus are the significant anatomic landmarks facilitating the reduction of proximal humeral fragments. PCA providing affluent nutrition to the proximal humerus is usually injured by preoperative or intraoperative trauma [17,18]. The branches of the axillary nerve lie in the anterolateral deltoid and are located an average of 3.5 cm from the lateral prominence of the greater tuberosity and 6 cm from the anterolateral border [19]. Careless surgery often results in injury to the nerve branches and the subsequent atrophy of the muscle it dominates. The rotator cuff, with other tendons and muscles, as well as their complex interaction among the proximal humeral, constitute the articulation humeri, which is the most mobile joint in the body. Rotator cuff injury is a critical factor in limited postoperative functional recovery of the affected shoulder [20]. The traction of muscle and tendon often lends to rotated and separated displacement of the fracture fragment. For example, the humeral head is often internally rotated by the pull of the subscapularis and a tuberosity fragment is pulled upwards and posteriorly [18,19].
The strength and weakness of minimal-invasive lateral approach
Other minimally invasive approaches are also available for the treatment of PHF, such as the deltoid insertion approach, deltoid-splitting approach, and combination (both deltopectoral incision and lateral incision) [9]. However, all these approaches have limitations. The deltoid insertion approach prevents the use of longer plates to stabilize fractures that extend into the shaft [21]. The deltoid-splitting approach has the potential risk of causing injury to the anterior branch of the axillary nerve during the muscle splitting [6]. The 2-incision approach has proven to be the most reliable method to distinctly expose each fracture fragment of the PHF and to effectively stabilize the fractures, but at the cost of larger trauma [8]. In the present study, a special minimally invasive lateral approach was applied. An average of 1-finger lower than the subacromial and 4–5-cm length laterigrade incision was made to cut-off the skin and the subcutaneous tissues, so as to expose deltoid muscles, but the muscle fiber was split lengthways along the deltoid. This technique was designed to facilitate the extension of the incision in case the fracture is too complex to reduce and fix. Moreover, the lateral incision is able to distinctly expose laterally fractured structures, especially the displaced greater tuberosity, thereby facilitating reduction and fixation with a locking plate. Anatomic reduction of the greater tuberosity is important for the recovery of shoulder function [22]. As the locking plate is positioned on the greater tuberosity and lateral proximal humeral, this technique offers direct access to the laterally fractured planes for the placement of a locking plate, which is considered a difficult procedure with the deltopectoral approach [8]. Explicit exposure and convenient surgery result in decreased surgery duration and blood loss, as shown in our study (Table 1). In addition, the distinct exposure of the rotator cuff is another advantage, making it easier to find the injury and repair the tears. The rotator cuff surrounding the proximal humerus is at high risk of being simultaneously injured by the fracture, which is a critical factor that leads to pain, engorgement, and limitation of motion of the shoulder after the operation [20]. Despite the advantages described above, the most outstanding advantage of the minimally invasive approach is the limited soft tissue damage around the proximal humerus. Decreased soft tissue stripping favors the blood supply of local tissue, which is also critical for successful clinical outcome [23]. Moreover, it is more suitable for the restless patient to receive surgery with the minimally invasive approach given the finding that the min-group had a significantly higher patient satisfaction rating (p=0.019). In addition, decreased soft tissue injury may facilitate quicker shoulder function recovery, as proven in our study (p<0.05, Table 2). However, there is a concern that injury to the anterior branch of the axillary nerve may occur when the deltoid is split. Indeed, previous studies have shown that splitting the deltoid lengthways along the raphe can be safe as long as the splitting length is less than 6 cm [19,24,25]. In our study, 39 patients received the minimally invasive approach, with no cases of intraoperative axillary nerve branch injury or atrophy of correlative muscles.
Although satisfactory operative results and low complication rate (5.1% vs. 9.6%) were achieved with the minimally invasive lateral approach, it should be noted that not all PHFs are suited for this incision, as indicated by the malreduction that occurred in the min-group in the present study. The displacement and separation of lesser tuberosities and medial cortex usually occur in the 4-part fracture according to the Neer classification, which results in loss of medial cortical buttress [26–28]. The medial cortical of the proximal humerus has the highest bone strength and provides mechanical support during the reduction [29]. The loss of medial support is a critical factor leading to bone- and fracture-related complications, such as malreduction and Varus fracture collapse, particularly in elderly patients with osteoporosis [28]. Autologous fibular or iliac graft augmentation and medial endosteal implant have been used to restore the integrity of the medial column [39–41]. However, the minimally invasive approach is unable to distinctly expose the anteromedial region of the proximal humerus, making it inconvenient to restore the medial column. Therefore, the minimally invasive approach is considered unsuitable for 4-part or loss of medial support fractures, although it has a significant advantage in the treatment of patients with 2-part or 3-part PHF. In contrast, patients with 4-part PHF in the conventional group obtained much better postoperative range of movement of the affected should, suggesting that the conventional approach is more suitable for the treatment of 4-part PHF. For the patients with complex 4-part PHF or serious osteoporotic, other techniques or humeral head replacement should be considered. If a surgeon is not able to achieve satisfactory reduction and stable internal fixation, primary arthroplasty should be considered [30].
Conclusions
Compared to the conventional deltopectoral approach in the ORIF of a PHF, the minimally invasive lateral approach has significant advantages in terms of lesser intra-operational surgery duration and blood loss, shorter hospitalization, lower postoperative complication rate, and quicker shoulder functional recovery. Our study suggests that the minimally invasive lateral approach may be a good alternative to the deltopectoral approach for patients with PHF and being treated with ORIF, especially for those with 2- or 3-part fractures. Close attention should be paid to the related complications, including loss of medial support, internal fixation loosening, and malreduction. For patients with severe, complex 4-part PHF, other invasive approaches or primary arthroplasty should be considered.
Acknowledgements
We express our deepest gratitude to the other supervisors of our department for their introductions and kind help.
Footnotes
Conflict of interest
No benefits in any form have been received or will be received from any commercial party related directly or indirectly to the subject of this article.
Source of support: Departmental sources
References
- 1.Norouzi M, Naderi MN, Komasi MH, et al. Clinical results of using the proximal humeral internal locking system plate for internal fixation of displaced proximal humeral fractures. Am J Orthop. 2012;41:E64–68. [PubMed] [Google Scholar]
- 2.Bartonicek J, Dzupa V, Fric V, et al. [Epidemiology and economic implications of fractures of proximal femur, proximal humerus, distal radius and fracture-dislocation of ankle]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 2008;87:213–19. [in German] [PubMed] [Google Scholar]
- 3.Khmelnitskaya E, Lamont LE, Taylor SA, et al. Evaluation and management of proximal humerus fractures. Adv Orthop. 2012;2012:861598. doi: 10.1155/2012/861598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 5.Verdano MA, Lunini E, Pellegrini A, et al. Can the osteosynthesis with locking plates be a better treatment for unstable fractures of the proximal humerus? Musculoskelet Surg. 2014;98(1):27–33. doi: 10.1007/s12306-013-0267-y. [DOI] [PubMed] [Google Scholar]
- 6.Buecking B, Mohr J, Bockmann B, et al. Deltoid-split or Deltopectoral Approaches for the Treatment of Displaced Proximal Humeral Fractures? Clin Orthop Relat Res. 2014;472(5):1576–85. doi: 10.1007/s11999-013-3415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23:163–72. doi: 10.1097/BOT.0b013e3181920e5b. [DOI] [PubMed] [Google Scholar]
- 8.Gallo RA, Zeiders GJ, Altman GT. Two-incision technique for treatment of complex proximal humerus fractures. J Orthop Trauma. 2005;19:734–40. doi: 10.1097/01.bot.0000174708.88108.da. [DOI] [PubMed] [Google Scholar]
- 9.Robinson CM, Murray IR. The extended deltoid-splitting approach to the proximal humerus: variations and extensions. J Bone J Surg Br. 2011;93:387–92. doi: 10.1302/0301-620X.93B3.25818. [DOI] [PubMed] [Google Scholar]
- 10.Zlotolow DA, Catalano LW, III, Barron OA, et al. Surgical exposures of the humerus. J Am Acad Orthop Surg. 2006;14:754–65. doi: 10.5435/00124635-200612000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Liu Z, Wang K, Zhang K, et al. Minimally invasive surgery (MIS) of anterior ring fracture combined with pubic symphysis separation. Med Sci Monit. 2014;20:1913–17. doi: 10.12659/MSM.892358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yimin Y, Zhiwei R, Wei M, et al. Current status of percutaneous vertebroplasty and percutaneous kyphoplasty – a review. Med Sci Monit. 2013;19:826–36. doi: 10.12659/MSM.889479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neer CS., II Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–89. [PubMed] [Google Scholar]
- 14.Wu CH, Ma CH, Yeh JJ, et al. Locked plating for proximal humeral fractures: differences between the deltopectoral and deltoid-splitting approaches. J Trauma. 2011;71:1364–70. doi: 10.1097/TA.0b013e31820d165d. [DOI] [PubMed] [Google Scholar]
- 15.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–64. [PubMed] [Google Scholar]
- 16.Offenbaecher M, Ewert T, Sangha O, et al. Validation of a German version of the disabilities of arm, shoulder, and hand questionnaire (DASH-G) J Rheumatol. 2002;29:401–2. [PubMed] [Google Scholar]
- 17.Cornell CN, Levine D, Pagnani MJ. Internal fixation of proximal humerus fractures using the screw-tension band technique. J Orthop Trauma. 1994;8:23–27. doi: 10.1097/00005131-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Terry GC, Chopp TM. Functional anatomy of the shoulder. J Athl Train. 2000;35:248–55. [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner MJ, Griffith MH, Dines JS, et al. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;(434):123–29. doi: 10.1097/01.blo.0000152872.95806.09. [DOI] [PubMed] [Google Scholar]
- 20.Aksu N, Aslan O, Kara AN, et al. Simultaneous repair of chronic full-thickness rotator cuff tears during fixation of proximal humerus fractures and clinical results. Acta Orthop Traumatol Turc. 2010;44:173–79. doi: 10.3944/AOTT.2010.2295. [DOI] [PubMed] [Google Scholar]
- 21.Rispoli DM, Athwal GS, Sperling JW, et al. The anatomy of the deltoid insertion. J Shoulder Elbow Surg. 2009;18(3):386–90. doi: 10.1016/j.jse.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Demirhan M, Kilicoglu O, Altinel L, et al. Prognostic factors in prosthetic replacement for acute proximal humerus fractures. J Orthop Trauma. 2003;17:181–88. doi: 10.1097/00005131-200303000-00004. discussion 188–89. [DOI] [PubMed] [Google Scholar]
- 23.Gardner MJ, Griffith MH, Dines JS, et al. A minimally invasive approach for plate fixation of the proximal humerus. Bulletin. 2004;62:18–23. [PubMed] [Google Scholar]
- 24.Smith J, Berry G, Laflamme Y, et al. Percutaneous insertion of a proximal humeral locking plate: an anatomic study. Injury. 2007;38:206–11. doi: 10.1016/j.injury.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 25.Saran N, Bergeron SG, Benoit B, et al. Risk of axillary nerve injury during percutaneous proximal humerus locking plate insertion using an external aiming guide. Injury. 2010;41:1037–40. doi: 10.1016/j.injury.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 26.Kennedy J, Feerick E, McGarry P, et al. Effect of calcium triphosphate cement on proximal humeral fracture osteosynthesis: a finite element analysis. J Orthop Surg (Hong Kong) 2013;21:167–72. doi: 10.1177/230949901302100210. [DOI] [PubMed] [Google Scholar]
- 27.Weeks CA, Begum F, Beaupre LA, et al. Locking plate fixation of proximal humeral fractures with impaction of the fracture site to restore medial column support: a biomechanical study. J Shoulder Elbow Surg. 2013;22:1552–57. doi: 10.1016/j.jse.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Jung WB, Moon ES, Kim SK, et al. Does medial support decrease major complications of unstable proximal humerus fractures treated with locking plate? BMC Musculoskelet Disord. 2013;14:102. doi: 10.1186/1471-2474-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burke NG, Kennedy J, Green C, et al. Locking plate fixation for proximal humerus fractures. Orthopedics. 2012;35:e250–54. doi: 10.3928/01477447-20120123-41. [DOI] [PubMed] [Google Scholar]
- 30.Krappinger D, Bizzotto N, Riedmann S, et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–88. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]