Abstract
Background
From 2010 onward, a new leaflet about mammography screening for breast cancer, more informative than the preceding version, has been sent to women in Germany aged 50 to 69 with the invitation to undergo screening. The purpose of this study was to determine the effect of different informational content on the decision whether or not to be screened.
Methods
In a randomized and blinded design, 792 women aged 48 to 49 were sent either the old or the new leaflet. Questionnaires were sent together with the leaflets in order to assess the following: willingness to undergo mammography screening, knowledge, decisional confidence, personal experiences of breast cancer, and demographic data.
Results
370 (46.7%) of the questionnaires were returned, and 353 were evaluable. The two groups did not differ significantly in their willingness to be screened: 81.5% (95% confidence interval [CI] 75.8%–87.2%) versus 88.6% (95% CI 83.9%–91.3%, p = 0.060). A post-hoc analysis showed that women who reported having had personal experience of breast cancer (18.7%) were more willing to be screened if they were given the new leaflet, rather than the old one (interaction p = 0.014). The two groups did not differ in their knowledge about screening (p = 0.260). Women who received the old leaflet reported a higher decisional confidence (p = 0.017). The most commonly mentioned factors affecting the decision were experience of breast cancer in relatives and close acquaintances (26.5% of mentions) and a doctor’s recommendation (48.2%). Leaflets (3.6%) and all other factors played only a secondary role.
Conclusion
The greater or lesser informativeness of the leaflet affected neither the participants’ knowledge of mammography screening nor their willingness to undergo it. The leaflet was not seen as an aid to decision-making. The best way to assure an informed decision about screening may be for the patient to discuss the matter personally with a qualified professional.
The purpose of mammography screening for breast cancer is to diagnose the disease early and thereby reduce mortality. In Germany, screening is recommended for all women aged 50 to 69. The mortality from breast cancer in this age group is 4 to 6 deaths per 1000 women in 10 years (1, 2). It is thought that mammography screening once every two years in this age group can reduce mortality by 1 to 3 deaths per 1000 women in 10 years (3– 8).
This collective benefit—about which there has been increasing controversy of late (3– 7)—must be weighed against the collective harm that arises through false-positive findings and the resulting diagnostic testing, overdiagnosis, and overtreatment. Of 1000 women undergoing screening every two years for 10 years, 100 to 300 will obtain a primary false-positive result at least once, and 20 to 60 will undergo a biopsy because of a false-positive screening mammogram. This causes considerable mental distress, and 1 to 5 of these 1000 women will receive unnecessary oncologic treatment (3– 8).
There is an ethical and legal requirement for informed consent: women must be comprehensively informed of the benefits and risks of mammography screening so that they can make a well-founded decision to undergo it or not. It remains unclear whether, and to what extent, comprehensive information affects women’s willingness to be screened (8– 15). Any factor that lessens it would reduce the cost-effectiveness of screening, as the investment and procedural costs would remain largely the same while fewer women would reap its benefits (16). Health-care economics must, however, remain a secondary consideration in relation to the individual ethical perspective (17). This is explicitly stipulated in new legislation that took effect in Germany in 2013 (18).
In Germany, an information leaflet accompanies the official invitation to undergo mammography screening that is sent to all women in the relevant age group. One may well ask to what extent this leaflet promotes the two potentially conflicting goals alluded to above: adequate information on the one hand, and cost-effective screening on the other. The invitation permits the women to undergo mammography screening without any prior personal discussion with a physician. The leaflet in use up to 2010 was criticized for its low informational content (19); from 2010 onward, a new leaflet has been used that was developed in an atmosphere of growing criticism. Although neither leaflet was created in accordance with published criteria for evidence-based patient information (20), the new one contains much more information relevant to decision-making than the old one did (21). In this study, we asked whether the greater informativeness of the new leaflet raises or lowers women’s willingness to undergo mammography screening, and what effect the new leaflet has on these patients’ knowledge of screening and the definitiveness of their decisions about it.
Methods
Study design, sample, and recruitment
In a randomized controlled study, we compared the leaflet used up to 2010 with the one used from 2010 onward with respect to the recipients’ willingness to undergo mammography screening and their knowledge about it (22).
We recruited study participants aged 48 to 49 from 33 family practices in the German federal state of North Rhine–Westphalia. Women in this age group have not yet received their first invitation to be screened, but are just about to receive it. Their views on the importance of mammography screening are likely to be the same as those of 50-year-old women; unlike 50-year-old women, they have not yet been sent the information leaflet. The participating physicians gave us pseudonymized lists of all female patients in this age group whom they had seen in the preceding two years.
From these lists, we selected 24 women from each practice and divided them into two groups of 12 subjects each to whom we sent the new leaflet (group A) and the old one (group B). The 24 participants from each practice were selected by a computer-assisted random procedure, and the group allotment process was also random. The authors wrote each participant’s pseudonym on the envelope that she was to receive, and the practices put the actual names and addresses on the envelopes and sent them. The participants and their family physicians were blinded with respect to group allotment, but the study team was not. The participants were asked by letter to fill out the questionnaire after reading the leaflet and to send it back in an envelope that was also enclosed in the mailing.
Questionnaire
The questionnaire was developed on the model of previously published questionnaires, some of which have been validated (23, 24), and in keeping with accepted methodological standards for item construction and formulation (25). After a pretest on 15 women, further minor changes were made in wording and in the scales used in the questionnaire.
Willingness to participate
The primary endpoint was the yes-or-no question whether the participant would decide to undergo screening if invited to do so right now, at the time of questioning (eTable 2). We tested the non-directional hypothesis that the willingness to participate would differ between group A (recipients of the new leaflet) and group B (recipients of the old leaflet).
eTable 2. Overview of factors tested in the regression and covariance analyses.
| Independent factors | Knowledge score |
Knowledge about risks (metric) |
Knowledge about benefits (metric) |
Willingness to be screened |
Decisional confidence (metric) |
|---|---|---|---|---|---|
| Leaflet | x | x | x | x | + |
| Familiy status | x | x | x | x | x |
| Living circumstances | x | x | + | x | x |
| Educational level | + | + | x | + | x |
| Personal experience of breast cancer | + | + | + | Interaction with leaflet |
Interaction with willingness to be screened |
| Main factor in decision | x | Interaction with willingness to be screened |
|||
| Knowledge score (1–10) | x | x | |||
| Self-assessed knowledge (1– 4) …about risks …about benefits |
(x) + |
x + |
|||
| Willingness to be screened | + |
x: regressors in the model in question; +: significant regressors in the model in question
Knowledge
Five items directly measured the participants’ “objective knowledge” of the material benefits and risks of mammography screening (i.e., those that are relevant to decision-making), on a scale of 0 to 10 (eTable 1) (20, 22– 24).
eTable 1. Original questions about willingness to be screened. decisional confidence. and knowledge about screening. and distribution of answers.
| Question | Possible answers | Answers (%) | |
|---|---|---|---|
| Willingness to be screened | |||
| If you were invited to undergo mammography screening today. would you do so? (n = 353) | no yes |
15.0 85.0 |
|
| Decisional confidence | |||
| How sure are you about this decision? (n=353) | not sure at all | 1 | 3.1 |
| 2 | 1.4 | ||
| 3 | 4.0 | ||
| 4 | 6.5 | ||
| 5 | 20.7 | ||
| absolutely sure | 6 | 64.3 | |
| Knowledge | |||
| Imagine a group of 100 women undergoing mammography screening. About how many of these women will have a positive finding (in other words. a finding that might indicate cancer) and will therefore need further diagnostic testing? (n=346) | *1about 1 in 100 | 15.6 | |
| *2about 10 in 100 | 47.7 | ||
| about 20 in 100 | 31.8 | ||
| about 50 in 100 | 4.9 | ||
| Suppose 10 women are told they have a positive finding and then undergo further testing to see whether they really have breast cancer. About how many will receive a diagnosis of breast cancer? (n=348) | *1 1 in 10 | 41.4 | |
| *2 3 in 10 | 49.1 | ||
| 7 in 10 | 7.2 | ||
| all 10 | 2.3 | ||
| Imagine a group of 1000 women who are all 50 years old. About how many of them will have breast cancer in the next 10 years? (n=340) | *220 in 1000 | 33.8 | |
| *150 in 1000 | 37.4 | ||
| 100 in 1000 | 24.4 | ||
| 300 in 1000 | 4.4 | ||
| Now imagine a group of 1000 women who undergo mammography screening every two years for 10 years. How many of these women would otherwise have died of breast cancer. but will have their lives saved because they underwent mammography screening? (n=345) | *2about 2 in 1000 | 14.5 | |
| *1about 15 in 1000 | 45.2 | ||
| about 100 in 1000 | 23.5 | ||
| about 200 in 1000 | 16.8 | ||
|
Out of 1000 women who undergo mammography screening every two years between the ages of 50 and 60. 24 will receive a diagnosis of breast cancer at some time in this period. Some will receive the diagnosis from the screening itself. and others will receive it between two screening tests. About how many of these 24 women will receive the diagnosis of breast cancer between two screening tests? The possible answers are given at right. with a diagram for each. Pick the answer that you think is correct. (n = 345) |
●●●●●● ●●● ●●● ●●●●●● ●●●●●○675; *11 in 24 |
18.8 | |
| ●●●●●● ●● ●●●○675; ●●●●●○675; ●●●●●○675; *23 in 24 |
42.3 | ||
| ●●●●●○675; ●●●●●○675; ●●●●○675; ○675; ●●●●○675; ○675; 6 in 24 |
25.5 | ||
| ●●●●○675; ○675; ●●●●○675; ○675; ●●●●○675; ○675; ●●●○675; ○675; ○675; 9 in 24 |
13.3 | ||
*1one point for this answer;
*2two points for this answer; knowledge score from 0 to 10 (higher score = more knowledge)
In addition, the participants were asked to self-assess their knowledge („subjective knowledge“) in two items on a scale of 1 to 4 (1 = “I know very little about it,” 4 = “I am very well informed about it”).
Decisional confidence
The participants were asked to rate their decisional confidence regarding participation in mammography screening on a six-point scale, ranging from “not confident at all” to “very confident” (eTable 1).
Further questions and factors
We asked the participants which of the following factors was the most important determinant of their decision about screening:
a doctor’s recommendation
media reports
the information leaflet
friends and relatives
personal experience of breast cancer.
We also assessed the following potential factors: educational attainment, marital/familial status, living circumstances, native language, and type of personal experience of breast cancer (none vs. among acquaintances or distant relatives vs. in close relatives vs. in oneself).
Ethics committee approval and registration
This study was approved by the Ethics Committee of the Universitätsklinikum Düsseldorf (University Hospital Düsseldorf) on 22 February 2012 (study no. 3797) and was registered with TRIALS (DRKS00004271).
Statistical analysis
The power calculation proceeded on the assumption of a minimal relevant difference of 15% (absolute) between the two groups with respect to their willingness to be screened. To allow detection of such an effect with a power of 80%, 173 women per group are required (N = 346). Although the participants were recruited from family practices, we did not expect a cluster effect to be operative in the study, as counseling for mammography screening is usually not done by family physicians. Moreover, women in this age group rarely visit their family physicians, and the family physicians played no active role in this study. We expected that 50% of the questionnaires would be filled out and returned, and we therefore set the recruitment target at 692 participants.
In accordance with the protocol, group differences in the primary endpoint “willingness to participate: yes/no” were tested for significance using the likelihood ratio chi-square test with a two-tailed α of 5% (non-directional hypothesis). Univariate group differences of nominally scaled features were evaluated analogously with chi-square tests. Group comparisons of variables expressed on ranking scales (objective and subjective knowledge) and continuous scales (age) were performed with Mann-Whitney U tests and t tests, respectively. Associations between objective and subjective knowledge were measured with Spearman rank correlations. Factors affecting the willingness to participate were evaluated with multivariate logistic regression analysis, while factors affecting knowledge and decisional confidence were evaluated with multifactorial covariance analysis. These models were used to generate adjusted estimators of the effects of the two leaflets. An overview of the factors taken into account in each analysis, and the sequence of model adaptation for each model, is provided in eTable 2. Interactions were permitted only between the leaflets and the factors. These interactions represent possible modifications of the effect of the leaflet that depend on other factors; they were therefore tested systematically with backwards elimination (p <0.05). Only significant effect modifications are reported in this article.
Results
Return of questionnaires
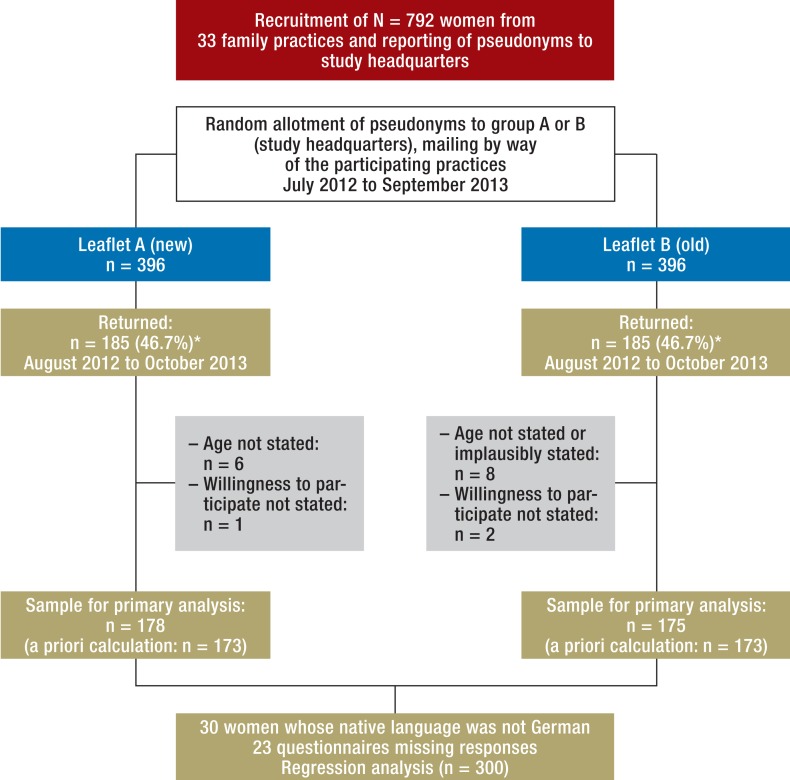
Questionnaires were sent to 792 women (396 per group) from July 2012 to September 2013. Women who did not respond after the first mailing were contacted a second time. 185 questionnaires were filled out and returned by each of the two groups (response rate, 46.7%); it was coincidental that this number was the same in both groups. 178 questionnaires from group A and 175 from group B were evaluable (total, 353; see Figure 1). The average number of questionnaires returned per practice was 8.2 after the first mailing (between 1 and 16) and 11.2 after the second mailing (between 5 and 19).
Figure 1.
Response and samples
*The exact same number of returned questionnaires in both groups was coincidental
Demographic features and previous experience
The two groups were comparable demographically and with respect to their prior experience of breast cancer; they differed only in their marital/familial status. One-fifth of the women overall did not know any other woman with breast cancer. One-fifth indicated having prior experience of breast cancer, either in themselves or in close relatives (Table 1).
Table 1. Description of study sample (from data provided by participants in response to the questionnaire).
| Leaflet A (new) | Leaflet B (old) | p*1 | ||
|---|---|---|---|---|
| Age (mean ± SD) |
48.67 ± 0.79 (n = 178) |
48.76 ± 0.80 (n = 175) |
n.s. | |
| Highest educational level attained | none or primary school | 35 (19.66%) | 32 (18.39%) | n.s. |
| middle school | 61 (34.27%) | 64 (36.78%) | ||
| high school | 49 (27.53%) | 55 (31.61%) | ||
| university | 33 (18.54%) | 23 (13.22%) | ||
| Family status | single | 19 (10.67%) | 14 (8.00%) | 0.025*2 |
| married | 119 (66.85%) | 141 (80.57%) | ||
| divorced | 37 (20.79%) | 19 (10.86%) | ||
| widowed | 3 (1.69%) | 1 (0.57%) | ||
| Living circumstances | alone | 24 (13.48%) | 14 (8.00%) | n.s. |
| with husband/life partner | 130 (73.03%) | 144 (82.29%) | ||
| with relatives | 22 (12.36%) | 13 (7.43%) | ||
| with others | 2 (1.12%) | 4 (2.29%) | ||
| Native language | German | 166 (93.26%) | 157 (89.71%) | n.s. |
| other | 12 (6.74%) | 18 (10.29%) | ||
| Personal experience of breast cancer | none | 40 (22.60%) | 35 (20.11%) | n.s. |
| in remote acquaintances | 102 (57.63%) | 108 (62.07%) | ||
| in relatives | 32 (18.08%) | 27 (15.52%) | ||
| I myself have had breast cancer | 3 (1.69%) | 4 (2.30%) | ||
*1Significance tests (all with a = 5%): t test for age. chi-square test for all frequencies.
*2Post hoc assessment of corrected standard residues: significantly more divorced and fewer married women in group A compared to group B.
n.s: difference not significant; SD. standard deviation
30 of the participating women (8.5%) were native speakers of a language other than German. Data from these women were included according to the protocol in the univariate analysis of primary and secondary endpoints, but not in the construction of the statistical model for the effects of the various influential factors. The reason for this was that analysis showed that these women react to the leaflet markedly differently from the native German-speakers. Further analysis of this subgroup seemed to be an unrewarding prospect for significant findings, as the subgroup was both too small to be representative of foreign-born women and too poorly characterized to permit any assessment of the severity of the communication deficit.
Willingness to undergo mammography screening (primary endpoint)
The women in the two groups did not differ in their willingness to be screened: 81.5% (95% confidence interval [CI], 75.8%–87.2%) of the group that received the new leaflet expressed their willingness to participate, as compared to 88.6% (95% CI 83.9%–91.3%) of the group that received the old leaflet (difference, 7.1%; 95% CI, -0.9%–14.3%; χ2; [df = 1] = 3.53; p = 0.060) (Table 2).
Table 2. Willingness to undergo mammography screening.
| Willing to be screened? | Overall | |||
|---|---|---|---|---|
| Yes | No | |||
| Group (leaflet) |
A (new) |
145 81.5% |
33 18.5% |
178 100.0% |
| B (old) |
155 88.6% |
20 11.4% |
175 100.0% |
|
| Overall | 300 85.0% |
53 15.0% |
353 100.0% |
|
Primary analysis without adjustment. including women whose native language was not German. Likelihood chi-square=3.53; df=1; p=0.060
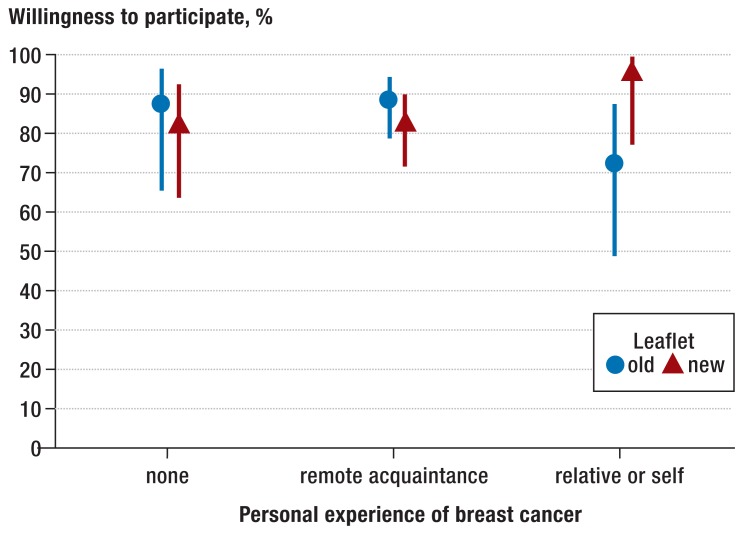
Regression analysis (eTable 3) revealed that women’s willingness to participate was negatively correlated with their educational level and positively correlated with the self-assessment of their own knowledge about the benefits of screening. Moreover, there was a significant interaction between prior experience of breast cancer and the leaflet (p = 0.014): in women who had had experience of breast cancer in themselves or in close relatives (18.7%), receipt of the new leaflet increased the likelihood that they would be willing to be screened (96.6% versus 72.5%; difference, 24.1%; p = 0.009) (Figure 2).
eTable 3. Factors affecting willingness to be screened.
| Independent factors | Estimated participation rate (willingness to be screened = yes). adjusted for all model variables (95% confidence interval) |
Odds ratio (95% confidence interval) |
p value |
|---|---|---|---|
| Leaflet | |||
| Old leaflet (reference) | 0.86 (0.77–0.92) | ||
| New leaflet | 0.85 (0.75–0.91) | 0.99 (0.92–1.07) | 0.814 |
| Marital status | |||
| Unmarried (reference) | 0.85 (0.71–0.93) | ||
| Married | 0.86 (0.78–0.91) | 1.11 (0.43–2.85) | 0.827 |
| Living circumstances | |||
| Living alone (reference) | 0.81 (0.58–0.93) | ||
| Not living alone | 0.86 (0.79–0.91) | 1.50 (0.45–4.94) | 0.506 |
| Highest educational attainment | 0.045 | ||
| None/primary school (reference) | 0.84 (0.68–0.93) | ||
| Middle school | 0.89 (0.80–0.95) | 1.68 (0.53–5.28) | 0.376 |
| High school | 0.88 (0.77–0.94) | 1.41 (0.44–4.46) | 0.563 |
| University | 0.72 (0.56–0.84) | 0.43 (0.14–1.33) | 0.143 |
| Main factor in decision | 0.227 | ||
| Personal experience (reference) | 0.83 (0.70–0.91) | ||
| Doctor’s recommendation | 0.89 (0.80–0.94) | 1.71 (0.65–4.47) | 0.278 |
| Other | 0.81 (0.69–0.89) | 0.83 (0.34–2.19) | 0.714 |
| Knowledge score (1–10). per point | 0.91 (0.75–1.10) | 0.327 | |
| Self-assessed knowledge (1–4) | |||
| …about risks Not at all informed A little bit informed Fairly well informed Very well informed |
0.98 (0.86–1.00) 0.86 (0.73–0.93) 0.74 (0.59–0.85) 0.91 (0.48–0.99) |
0.12 (0.02–0.74) 0.04 (0.01–0.40) 0.23 (0.01–5.16) |
0.059 0.022 0.045 0.128 |
| …about benefits Not at all informed A little bit informed Fairly well informed Very well informed |
0.59 (0.15–0.92) 0.68 (0.49–0.83) 0.91 (0.83–0.96) 0.88 (0.68–0.96) |
1.71 (0.20–14.42) 11.17 (1.05–118.5) 7.7 (0.55–108.6) |
0.007 0.621 0.045 0.128 |
| Personal experience of breast cancer (broken down by new vs. old leaflet) | 0.014 (between subgroups) |
||
| New leaflet: None (reference) In acquaintances In relatives or self |
0.82 (0.64–0.93) 0.83 (0.71–0.90) 0.97 (0.77–1.00) |
1.01 (0.33–3.13) 7.09 (0.70–71.83) |
0.983 0.097 |
| Old leaflet: None (reference) In acquaintances In relatives or self |
0.88 (0.66–0.96) 0.89 (0.79–0.94) 0.72 (0.49–0.88) |
1.12 (0.25–4.95) 0.31 (0.06–1.65) |
0.862 0.171 |
Multivariate logistic regression with the criterion “willingness to be screened” (no=0. yes=1); restricted to native German speakers (n = 300)
Figure 2.
Mammography screening: willingness of 48–49-year-old women to be screened as a function of personal experience after reading the old or new patient information leaflet (adjusted rates with 95% confidence intervals; calculated by inverse logit transformation, n = 300)
Knowledge
On a scale of 1 to 10, the mean objective knowledge score attained by the group that received the new leaflet was 5.49 (95% CI: 5.18–5.80; standard deviation [SD]: 1.99; n = 161), while that of the group that received the old leaflet was 5.23 (95% CI: 4.92–5.55; SD: 2.06; n = 168). This difference was insignificant (p = 0.260).
Nor did the two groups differ in their self-assessed knowledge of the benefits of screening (p = 0.874): on a scale of 1 to 4, the new-leaflet group attained a mean of 2.78 points (95% CI: 2.67–2.89; SD: 0.73; n = 178), while the old-leaflet group attained a mean of 2.78 points (95% CI: 2.66–2.90; SD: 0.77; n = 175). Their self-assessed knowledge of the risks of screening did not differ significantly either: mean in new-leaflet group, 2.45 points (95% CI: 2.33–2.57; SD: 0.82; n = 178); mean in old-leaflet group, 2.31 points (95% CI: 2.19–2.43; SD: 0.83; n = 174) on a scale of 1 to 4; p = 0.155.
The objective knowledge score and the self-assessment scores for knowledge of the benefits and risks of screening were not correlated with each other (insignificant correlations, rho <0.10). Regression analysis revealed that the objective knowledge score was positively correlated with educational attainment and negatively correlated with personal experience of breast cancer (data not shown).
Decisional confidence
Decisional confidence (on a scale of 1 to 6, from low to high) was high in both groups: mean score in new-leaflet group, 5.15 (95% CI: 4.95–5.35; SD: 1.36; n = 178); mean score in old-leaflet group, 5.52 (95% CI: 5.38–5.66; SD: 0.93; n = 175). The mean difference of 0.37 points (95% CI: 0.13–0.61) is statistically significant (p = 0.017), but the effect strength is low (r = 0.128).
Covariance analysis (eTable 4) revealed that the new leaflet lessened decisional confidence even after adjustment for other factors. Decisional confidence was positively associated with self-assessed knowledge; moreover, women who said they would undergo screening were more confident with their decision than those who said they would not.
eTable 4. Factors affecting decisional confidence.
| Independent factors | Mean score (adjusted for all model variables) | Difference from reference (95% confidence interval) | p value |
|---|---|---|---|
| Leaflet | 0.006 | ||
| Old leaflet (reference) New leaflet |
5.55 5.19 |
–0.36 (–0.62; 0.10) |
|
| Marital status | 0.373 | ||
| Married (reference) Unmarried |
5.47 5.33 |
–0.14 (–0.46; 0.17) |
|
| Living circumstances | 0.139 | ||
| Living alone (reference) Not living alone | 5.07 5.40 |
0.33 (–0.11; 0.80) |
|
| Highest educational attainment | 0.831 | ||
| None/primary school (reference) | 5.31 | ||
| Middle school | 5.34 | 0.04 (–0.33; 0.41) | 0.842 |
| High school | 5.46 | 0.15 (–0.24; 0.54) | 0.442 |
| University | 5.32 | 0.01 (–0.44; 0.46) | 0.958 |
| Knowledge score (1–10). per point | 0.00 (–0.06; 0.07) | 0.811 | |
| Self-assessed knowledge (1–4) | |||
| …about risks Not at all informed A little bit informed Fairly well informed Very well informed |
5.60 5.35 5.41 4.76 |
0.25 (–0.69; 0.19) –0.19 (–0.70; 0.33) –0.84 (–1.66; –0.02) |
0.184 0.258 0.475 0.044 |
| …about benefits Not at all informed A little bit informed Fairly well informed Very well informed |
4.83 5.02 5.47 5.85 |
0.18 (–0.54; 0.90) 0.64 (–0.13; 1.34) 1.02 (0.14; 1.90) |
0.016 0.617 0.102 0.023 |
| Willingness to participate | 0.002 | ||
| No (reference) Yes |
4.94 5.42 |
0.47 (0.11; 0.84) |
|
| Personal experience of breast cancer (broken down by willingness to be screened) | 0.042 (between subgroups) |
||
| If willing to be screened: None (reference) |
5.53 |
||
| In acquaintances | 5.33 | –0.13 (–0.46; 0.20) | 0.288 |
| In relatives or self | 5.6 | 0.01 (–0.41; 0.43) | 0.748 |
| If unwilling to be screened: None (reference) |
5.19 |
||
| In acquaintances | 5.1 | –0.09 (–0.90; 0.72) | 0.824 |
| In relatives or self | 4.1 | –1.09 (–2.17; 0.18) | 0.046 |
| Main factor in decision (broken down by willingness to be screened) |
0.004 (between subgroups) |
||
| If willing to be screeed: Personal experience (reference) |
5.57 |
||
| Doctor’s recommendation | 5.55 | –0.02 (–0.36; 0.31) | 0.891 |
| Other | 5.06 | –0.51 (–0.89; –0.14) | 0.008 |
| If unwilling to be screeed: Personal experience (reference) |
4.33 |
0.207 | |
| Doctor’s recommendation | 4.99 | 0.66 (–0.21; 1.54) | 0.138 |
| Other | 5.42 | 1.09 (0.22; 1.97) | 0.015 |
Multivariate covariance analysis with decisional confidence as the dependent variable (score ranging from 1=not confident at all to 6=absolutely confident); n=300
Regardless of the leaflet they received (old or new), women who were unwilling to be screened were less confident with their decision if they had prior experience of breast cancer (either in themselves or in a close relative) (eFigure).
eFigure.
Mammography screening: decisional confidence with regard to screening as a function of personal experience in 48- and 49-year-old women who were and were not willing to be screened (adjusted mean values on a scale of 1 = not confident at all to 6 = absolutely confident, with ANCOVA-based 95% confidence intervals; n = 300)
The role of the information leaflet
On being asked which among a list of factors was the most important in their decision to undergo or not to undergo mammography screening, the women most often said it was a doctor’s recommendation (48.2%); the information leaflet was named less often than any other factor on the list (3.6%). Groups A and B did not differ in this respect (p = 0.308) (Table 3).
Table 3. The most important factor in the decision whether to undergo mammography screening_(as stated in response to the questionnaire).
| Group | Total | ||||
|---|---|---|---|---|---|
| A. new | B. old | ||||
| Factor | Doctor’s recommendation | number | 75 | 87 | 162 |
| % in group | 44.1% | 52.4% | 48.2% | ||
| Media | number | 16 | 8 | 24 | |
| % in group | 9.4% | 4.8% | 7.1% | ||
| Leaflets | number | 7 | 5 | 12 | |
| % in group | 4.1% | 3.0% | 3.6% | ||
| Friends’ recommendation | number | 5 | 9 | 14 | |
| % in group | 2.9% | 5.4% | 4.2% | ||
| Personal experience of breast cancer | number | 47 | 42 | 89 | |
| % in group | 27.6% | 25.3% | 26.5% | ||
| Other | number | 20 | 15 | 35 | |
| % in group | 11.8% | 9.0% | 10.4% | ||
| Total | number | 170 | 166 | 336 | |
| % in group | 100.0% | 100.0% | 100.0% | ||
Only one answer was permitted. Difference between leaflets: chi-square test not significant (p = 0.308). Missing data: n=17
Discussion
Main findings
Among the women participating in this study, the receipt of a less informative leaflet or a more informative one made no difference to their willingness to undergo mammography screening (81.5% versus 88.6%, p = 0.060) or to their knowledge of its benefits and risks (5.23 versus 5.49 out of a maximum of 10 points, p = 0.260). On the other hand, a post-hoc analysis revealed that, in the subgroup of women with prior personal experience of breast cancer, the receipt of an old or new leaflet did indeed make a difference: those who received the new leaflet were more willing to be screened.
Willingness to be screened, knowledge, and decisional confidence
The demonstrated absence of an association between objective knowledge and willingness to be screened, and between objectively measured and subjectively (self-)assessed knowledge, challenges the ethical justification for the current mode of information for women in the German breast cancer screening program. It leads us to ask whether women are truly being enabled to thoroughly weigh the benefits and risks of mammography screening in order to arrive at a factually based decision whether to undergo it. The patient’s level of educational attainment was positively correlated both with objective knowledge and with (some aspects of) subjectively assessed knowledge; it thus seems that the information contained in the leaflet is not getting through as effectively to less educated women. This being the case, the fact that less educated women are actually more willing to participate than more educated ones, as also shown in previous studies (26), gives us yet another reason to doubt the ethical justification of patient information as currently practiced.
The exploratory analysis showed that the effect of the leaflet depended on the subjects’ personal experience of breast cancer (Figure 2). We consider this a meaningful provisional finding that should be empirically checked, and we are currently investigating the possible reasons for it in a qualitative study.
Women in both group A and group B felt highly confident with their decisions whether to undergo mammography screening. Apparently, either they did not realize their limited objective knowledge of the benefits and risks of screening, or else they were aware of it but nonetheless felt able to decide with confidence. This would indicate that there is a major emotional component in the decision whether to be screened, which would also help explain the effect of prior personal experience of breast cancer (eFigure): women who have lived through breast cancer in themselves or close relatives feel less confident with their decisions about screening than women who have not, and vice versa.
This study in the context of the literature
The question whether information leaflets actually increase patients’ knowledge about diagnostic tests for the early diagnosis of cancer has been studied previously, with mixed findings (23, 27). Studies of patients’ knowledge after reading an official information leaflet on breast cancer screening (28) or a leaflet on colon cancer screening prepared by the researchers themselves to be maximally clear and informative (13) have shown that patients knew more about risks and benefits after reading the leaflet. A study of an online decisional aid yielded a similar finding (23, 24). On the other hand, men who read an informational leaflet on prostate-specific antigen (PSA) testing did not have a better understanding of decisionally relevant facts after reading it than before (29).
The main finding of the present study, that the differing informativeness of two patient-education leaflets made no difference to women’s willingness to undergo screening, confirms a finding of the earlier study on colon cancer screening that was mentioned above (13).
Limitations
The screening participation rates and knowledge scores reported here may be biased in the positive direction, for a number of reasons: this study only included women who had a family physician; their willingness to undergo screening was only asked about theoretically, and not verified by actual participation; and they filled out the questionnaires at home, and thus may have consulted external references in order to answer the questions. The high willingness to undergo screening that we found in this study contrasts with the reported actual participation rate of 54% (30). The effects leading to artefactually high participation rates were presumably operative to a comparable extent in group A and group B of the present study.
The subjects were not asked about any mammographic examinations they might have had in the past. Prior mammography may well affect a woman’s decision whether to undergo screening.
The statistical analysis was predetermined only with respect to the primary analysis and the establishment of secondary endpoints. No correction for multiplicity was made in the model search (in accordance with the usual procedure). The interactions revealed by multivariate analysis can therefore only be considered exploratory; they must be confirmed by further, independent testing.
Overall assessment
The information leaflet on mammography screening is intended to give women the opportunity to make an independent, informed decision on the basis of a personal consideration of the risks and benefits. This study, however, in accordance with other ones (26, 31), implies that the leaflet does not achieve its purpose: most of the subjects considered the leaflet unimportant for their decision, and four out of five wanted to undergo screening regardless of whether they had received a more informative leaflet or a less informative one. Their understanding of the facts relevant to decision-making was independent of the leaflet they received. On the other hand, nearly half said their doctor’s recommendation was the most important factor in their decision. It may well be that women need to have a personal discussion with a qualified professional, supported by suitable materials (decision aids), in order for women to be enabled—as required by current German law—to make informed decisions for or against mammography screening (32).
Key Messages.
Two leaflets on mammography screening with differing informational content had no overall effect on women’s willingness to undergo mammography, or on their decisionally relevant knowledge about it.
Women with experience of breast cancer in themselves or close relatives were more willing to undergo mammography if they had read the more informative leaflet (96.6%) rather than the less informative one (72.5%) (post hoc analysis).
Less educated women have less decisionally relevant knowledge after reading the leaflet, but they are nevertheless more willing to undergo mammography than more educated women.
When asked to name the most important factor in their decision whether to undergo mammography, only 3.6% of women named the information leaflet, while 48.2% named their doctor’s recommendation.
The provision of an information leaflet alone apparently does not enable women to make an informed decision for or against mammography screening as required by current German law.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest.
References
- 1.Leitlinienprogramm Onkologie. Interdisziplinäre S3-Leitlinie für die Diagnostik, Therapie und Nachsorge des Mammakarzinoms. www.awmf.org/uploads/tx_szleitlinien/032_045OL_k_S3_Brustkrebs_Mammakarzinom_Diagnostik_Therapie_Nachsorge_2012-07.pdf. (last accessed on 19 May 2014)
- 2.Shapiro S, Coleman EA, Broeders M, et al. Breast cancer screening programmes in 22 countries: current policies, administration and guidelines. International Breast Cancer Screening Network (IBSN) and the European Network of Pilot Projects for Breast Cancer Screening. Int J Epidemiol. 1998;27:735–742. doi: 10.1093/ije/27.5.735. [DOI] [PubMed] [Google Scholar]
- 3.Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet. 2012;380:1778–1786. doi: 10.1016/S0140-6736(12)61611-0. [DOI] [PubMed] [Google Scholar]
- 4.Bleyler A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367:1998–2005. doi: 10.1056/NEJMoa1206809. [DOI] [PubMed] [Google Scholar]
- 5.Gøtzsche PC, Jørgensen KJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2013;6 doi: 10.1002/14651858.CD001877.pub5. CD001877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pace L, Keating N. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA. 2014;311:1327–1335. doi: 10.1001/jama.2014.1398. [DOI] [PubMed] [Google Scholar]
- 7.Miller A, Wall C, Baines C, Sun P, To T, Narod S. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study. BMJ. 2014;348 doi: 10.1136/bmj.g366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mühlhauser I, Höldke B. Information zum Mammographiescreening - vom Trugschluss zur Ent-Täuschung. Radiologe. 2002;42:299–304. doi: 10.1007/s00117-002-0737-y. [DOI] [PubMed] [Google Scholar]
- 9.Biller-Andorno N, Jüni P. Abolishing mammography screening programs? A view from the Swiss Medical Board. N Engl J Med. 2014:;370:1965–1967. doi: 10.1056/NEJMp1401875. [DOI] [PubMed] [Google Scholar]
- 10.Gigerenzer G. Breast cancer screening pamphlets mislead women. BMJ. 2014;348 doi: 10.1136/bmj.g2636. [DOI] [PubMed] [Google Scholar]
- 11.Baines C. Mammography screening: Are women really giving informed consent? J Natl Cancer Inst. 2003;95 doi: 10.1093/jnci/djg026. [DOI] [PubMed] [Google Scholar]
- 12.Loh A, Simon D. Patientenbeteilung bei medizinischen Entscheidungen [Shared Decision Making in Medicine] Dtsch Arztebl. 2007;104:A1484–A1488. [Google Scholar]
- 13.Steckelberg A, Hülfenhaus C, Haastert B, Mühlhauser I. Effect of evidence based risk information on “informed choice” in colorectal cancer screening: randomized controlled trial. BMJ. 2011;342 doi: 10.1136/bmj.d3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klemperer D, Lang B, Koch K, et al. Gute Praxis Gesundheitsinformation. Z Evid Fortbild Qual Gesundh.wesen (ZEFQ) 2010;144:66–68. [Google Scholar]
- 15.Rimer B, Briss P, Zeller P, et al. Informed decision making: what is the role in cancer screeening? Cancer. 2004;101:1214–1228. doi: 10.1002/cncr.20512. [DOI] [PubMed] [Google Scholar]
- 16.De Koning H. Breast cancer screening; cost effective in practice? Europ J Radiol. 2000;33:32–37. doi: 10.1016/s0720-048x(99)00105-9. [DOI] [PubMed] [Google Scholar]
- 17.Strech D. Participation rate or informed choice? Rethinking the European key performance indicators for mammography screening. Health Policy. 2014;115:100–103. doi: 10.1016/j.healthpol.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Helou A. Krebsfrüherkennung im Nationalen Krebsplan. Gesundheitspolitischer Rahmen und gesetzliche Neuregelungen. Bundesgesundheitsbl. 2014;57:288–293. doi: 10.1007/s00103-013-1902-3. [DOI] [PubMed] [Google Scholar]
- 19.Gummersbach E, Abholz HH. Info-Flyer “Mammographie-Screening” in Deutschland - Welche Informationen enthält er und welche sollte er enthalten? Z Allg Med. 2006;82:491–494. [Google Scholar]
- 20.Steckelberg A, Berger B, Köpke S, Heesen C, Mühlhauser I. Criteria for evidence-based patient information. Z ärztl Fortbild Qual Gesundh.wes. 2005;99:343–351. [PubMed] [Google Scholar]
- 21.Gummersbach E, Abholz HH. New leaflet for mammography screening in Germany: help for opinion making of invited persons. Z Allg Med. 2011;87:21–25. [Google Scholar]
- 22.Gummersbach E, in der Schmitten J, Abholz HH, Wegscheider K, Pentzek M. Effects of different information brochures on women’s decision-making regarding mammography screening: study protocol for a randomized controlled questionnaire study. Trials. 2013;14:319–324. doi: 10.1186/1745-6215-14-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Connor AM, Bennett CL, Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009;8 doi: 10.1002/14651858.CD001431.pub2. CD001431. [DOI] [PubMed] [Google Scholar]
- 24.Mathieu E, Barratt A, Davey HM, et al. Informed choice in mammography screening. A randomized trial of a decision aid for 70-year-old women. Arch Intern Med. 2007;67:2039–2046. doi: 10.1001/archinte.167.19.2039. [DOI] [PubMed] [Google Scholar]
- 25.Porst R. Ein Arbeitsbuch. 4th edition. Berlin: Springer; 2014. Fragebogen. [Google Scholar]
- 26.Naß-Griegoleit I, Schultz-Zehden B, Klusendick M, Diener J, Schulte H. Studie belegt hohe Akzeptanz des Mammographie-Screenings bei Frauen. Ergebnisse der ersten repräsentativen Studie in Deutschland. Frauenarzt. 2009;50:494–501. [Google Scholar]
- 27.Giordano L, Stefanini V, Senore C, et al. The effect of different communication and organizational strategies on mammography screening uptake in women aged 40-45 years. Europ J Pub Health. 2012;22:413–418. doi: 10.1093/eurpub/ckr090. [DOI] [PubMed] [Google Scholar]
- 28.Webster P, Austoker P. Women’s knowledge about breast cancer risk and their views of the purpose and implications of breast screening—a questionnaire survey. J Public Health. 2006;28:197–202. doi: 10.1093/pubmed/fdl030. [DOI] [PubMed] [Google Scholar]
- 29.Börgermann C, vom Dorp F, Rossi R, et al. Die Patientenaufklärung zur Prostatakarzinomfrüherkennung ist unzureichend. Der Urologe. 2009;48:997–1001. doi: 10.1007/s00120-009-2074-5. [DOI] [PubMed] [Google Scholar]
- 30.Malek A, Kääb-Sanyal V, Wegener B. Berlin: Kooperationsgemeinschaft Mammographie; 2014. Evaluationsbericht 2010 - Ergebnisse des Mammographie-Screening-Programms in Deutschland. [Google Scholar]
- 31.Dierks ML, Schmacke N. Mammographie-Screening und informierte Entscheidung-mehr Fragen als Antworten Gesundheitsmonitor 1/2014. Newsletter. www.bertelsmann-stiftung.de/cps/rde/xbcr/SID-35C1977B-FE483367/bst/xcms_bst_dms_39349_39350_2.pdf. (last accessed on 20 May 2014) [Google Scholar]
- 32.in der Schmitten J. Autonomie gewähren genügt nicht - Patienten-Selbstbestimmung bedarf aktiver Förderung durch Ärzte [Granting autonomy is not sufficient - patient self-determination needs active support by physicians] Zeitschr Allgemeinmed. 2014;6:20–24. [Google Scholar]