Abstract
Bilateral re-expansion pulmonary edema (RPE) is an extremely rare entity. We report the unique case of bilateral RPE following a traumatic, unilateral hemopneumothorax in a young healthy male. Bilateral RPE occurred only one hour after drainage of a unilateral hemopneumothorax. The patient was treated with diuretics and supplemental oxygen. Diagnosis was confirmed by excluding other causes, using laboratory findings, chest radiography, pulmonary and cardiac ultrasound and high resolution computed tomography. His recovery was uneventful. The pathophysiology of bilateral RPE is not well known. Treatment is mainly supportive and consists of diuretics, mechanical ventilation, inotropes and steroids. In case of a pulmonary deterioration after the drainage of a traumatic pneumothorax, bilateral RPE should be considered after exclusion of more common causes of dyspnea.
Keywords: Re-expansion pulmonary edema, bilateral, hemothorax, pneumothorax, trauma
Introduction
We report here on a unique case of bilateral re-expansion pulmonary edema (RPE). First described in 1958, RPE is a rare, but well known complication of thoracocentesis 1. RPE usually occurs unilaterally after expansion of the ipsilateral collapsed lung caused by either spontaneous pneumothorax or various types of pleural effusion 2. However, in this case, RPE occurred bilaterall y, following expansion of a unilateral hemopneumothorax in the setting of trauma.
Case
A 31-year old caucasian male with no significant past medical history was brought to our emergency department after falling 1.5 meters down from a platform. He was fully conscious and both respiratory and hemodynamically stable. Secondary survey findings included a fractured left olecranon and fractures of costae 7 to 9 on the left side, without clinical or radiological signs of a pneumothorax.
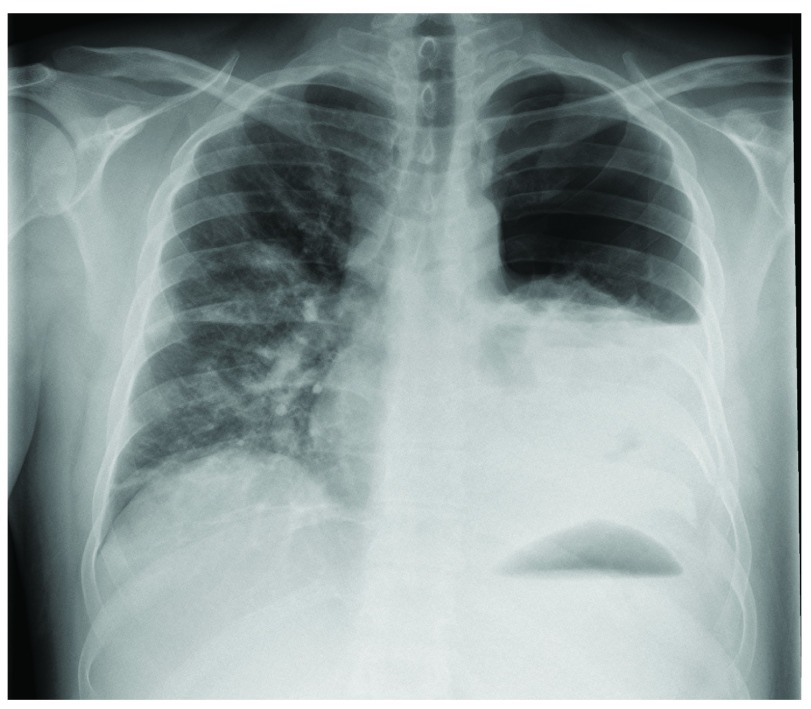
After two days in the hospital, he underwent tension band wiring of his olecranon under general anaesthesia. There were no difficulties during mechanical ventilation. However, on the first postoperative day, his peripheral oxygen saturation was noted to be 93% without supplemental oxygen. Auscultation yielded decreased breath sounds on the left side and a chest radiograph showed a fully collapsed left lung with pleural effusion ( Figure 1). A chest tube was placed which immediately drained air and 250 mL of blood.
Figure 1. Chest radiograph showing a hemopneumothorax of the left lung.
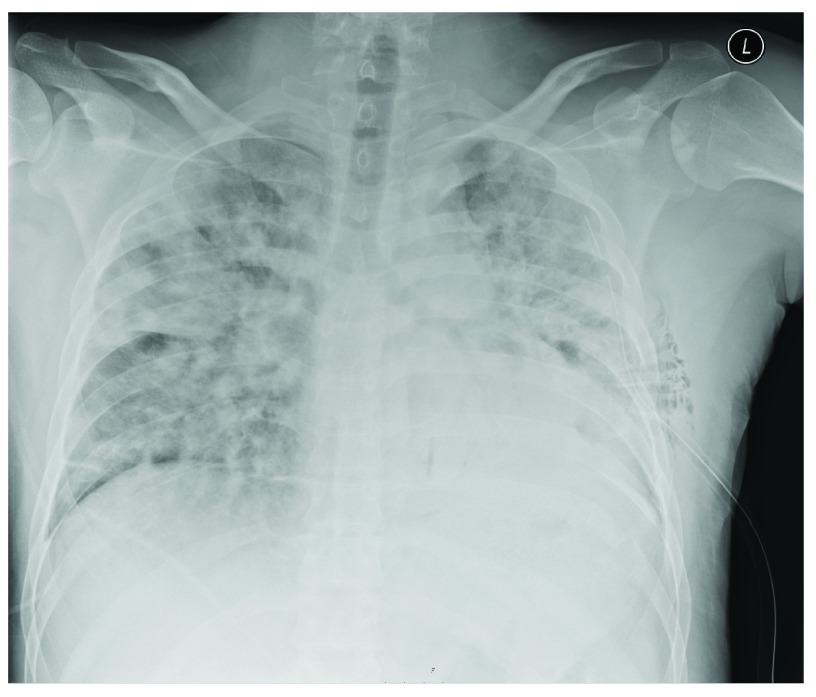
To our surprise, follow-up chest radiography one hour after drainage, demonstrated diffuse bilateral airspace opacification, peribronchial cuffing and Kerley-B lines, indicating bilateral pulmonary edema ( Figure 2). The chest tube was in a good position. In the course of several hours our patient became increasingly dyspnoeic, requiring 15 liters of oxygen via a non-rebreathing mask. He was transferred to the intensive care unit.
Figure 2. Chest radiograph one hour after drainage of the left hemopneumothorax showing bilateral pulmonary edema.
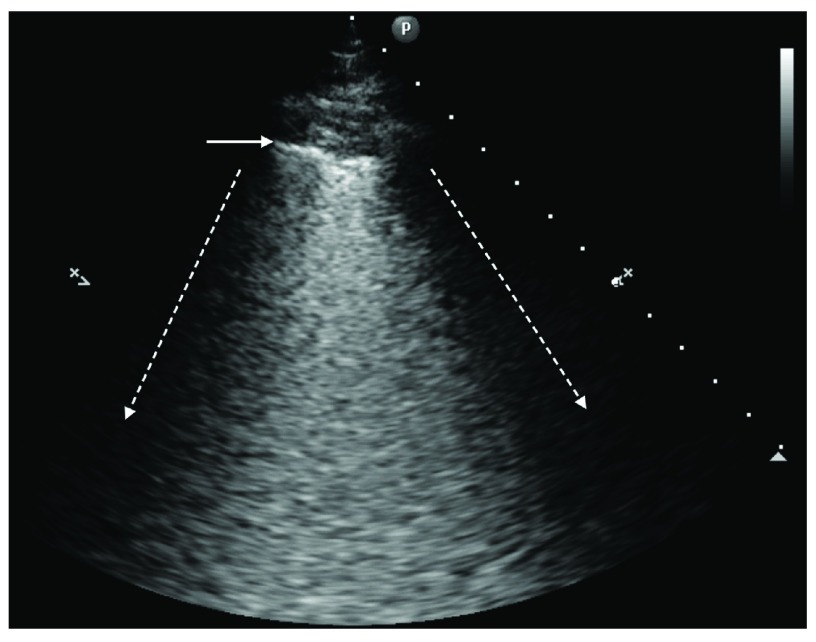
Intensive care ultrasound showed bilateral B-lines in all lung fields ( Figure 3), normal left and right ventricular function, no valvular dysfunction, normal atrial and caval vein dimensions and no pericardial effusion. These findings are consistent with non-cardiogenic pulmonary edema. Our patient did not receive excessive fluid therapy or blood transfusions and N-terminal-pro-B-type natriuretic peptide was normal (430ng/L), as were white cell count (9,6×10 9s/L) and C-reactive protein (23mg/L). Through this process of exclusion, and consistent with recent lung re-expansion, our patient was diagnosed with bilateral RPE.
Figure 3. Ultrasound image of the upper right lobe.
The dotted arrows indicate the rib shadows. The horizontal arrow indicates the pleura. Between the dotted arrows B-lines can be seen in a pattern called ground-glass rockets, showing an interstitial syndrome.
Aggressive diuretic therapy markedly improved his dyspnea without the need for mechanical ventilation and our patient was transferred back to the ward after 24 hours. Because of a persisting dependency of supplemental oxygen, high resolution computed tomography was performed two days later. This confirmed our diagnosis of bilateral pulmonary edema and revealed two additional rib fractures on the left side. Diuretics and oxygen suppletion were discontinued after a few days, and twelve days after the initial trauma our patient was discharged to home.
Discussion
To the best of our knowledge, this is the first report of bilateral RPE following thoracocentesis of a unilateral traumatic hemopneumothorax. A few cases of bilateral RPE have been described in literature 3– 11. However, none of these cases were preceded by a traumatic injury. In fact, most reported cases of either unilateral or bilateral RPE followed non-traumatic pneumothorax, pleural empyema or pleural effusion. The incidence of unilateral RPE is between 0 and 6,5% whereas bilateral RPE is extremely rare 11– 14.
The pathophysiology of bilateral RPE is not well known. Increased levels of the pro-inflammatory cytokine interleukin-8 and monocyte chemo-attractant protein 1 might be involved in the inflammatory process that characterizes RPE 15. In addition, re-expansion of the lung may lead to reperfusion injury and increased permeability of the endovascular cells 16. A prolonged collapse seems to result in an increased risk for RPE 4, 11. Other risk factors include the extent of lung collapse, young age 17 and fast re-expansion using suction 4. Treatment is still mainly supportive and relies mostly on diuretics but may necessitate mechanical ventilation, inotropes and steroids 11, 17.
In conclusion, bilateral re-expansion pulmonary edema is an extremely rare but fascinating phenomenon following treatment of a unilateral traumatic hemopneumothorax. In case of a pulmonary deterioration after the drainage of a traumatic pneumothorax, bilateral RPE should be considered, after exclusion of more common causes of dyspnea.
Consent
Written informed consent for publication of clinical details and clinical images was obtained from the patient.
Funding Statement
The author(s) declared that no grants were involved in the funding of this work.
v1; ref status: indexed
References
- 1.Carlson RI, Classen KL, Gollan F, et al. : Pulmonary edema following the rapid reexpansion of a totally collapsed lung due to a pneumothorax: a clinical and experimental study. Surg Forum. 1958;9:367–371. [PubMed] [Google Scholar]
- 2.Neustein SM: Reexpansion pulmonary edema. J Cardiothorac Vasc Anesth. 2007;21(6):887–891. 10.1053/j.jvca.2007.01.014 [DOI] [PubMed] [Google Scholar]
- 3.Henderson AF, Banham SW, Moran F: Re-expansion pulmonary oedema: a potentially serious complication of delayed diagnosis of pneumothorax. Br Med J (Clin Res Ed). 1985;291(6495):593–594. 10.1136/bmj.291.6495.593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahfood S, Hix WR, Aaron BL, et al. : Reexpansion pulmonary edema. Ann Thorac Surg. 1988;45(3):340–345. 10.1016/S0003-4975(10)62480-0 [DOI] [PubMed] [Google Scholar]
- 5.Ragozzino MW, Green R: Bilateral reexpansion pulmonary edema following unilateral pleurocentesis. Chest. 1991;99(2):506–508. 10.1378/chest.99.2.506 [DOI] [PubMed] [Google Scholar]
- 6.Özlü O, Kilic A, Cengizlier R: Bilateral re-expansion pulmonary edema in a child: a reminder. Acta Anaesthesiol Scand. 2000;44(7):884–885. 10.1034/j.1399-6576.2000.440717.x [DOI] [PubMed] [Google Scholar]
- 7.Dubose J, Perciballi J, Timmer S, et al. : Bilateral reexpansion pulmonary edema after treatment of spontaneous pneumothorax. Curr Surg. 2004;61(4):376–379. [DOI] [PubMed] [Google Scholar]
- 8.Baik JH, Ahn MI, Park YH, et al. : High-resolution CT findings of re-expansion pulmonary edema. Korean J Radiol. 2010;11(2):164–168. 10.3348/kjr.2010.11.2.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paksu MS, Paksu S, Akgün M, et al. : Bilateral reexpansion pulmonary edema associated with pleural empyema: a case report. Eur J Pediatr. 2011;170(9):1205–1207. 10.1007/s00431-011-1441-6 [DOI] [PubMed] [Google Scholar]
- 10.Gleeson T, Thiessen R, Müller N: Reexpansion Pulmonary edema computed tomography findings in 22 patients. J Thorac Imaging. 2011;26(1):36–41. 10.1097/RTI.0b013e3181ced052 [DOI] [PubMed] [Google Scholar]
- 11.Haga T, Kurihara M, Kataoka H: The risk for re-expansion pulmonary edema following spontaneous pneumothorax. Surg Today. 2013;44(10):1823–7. 10.1007/s00595-013-0726-y [DOI] [PubMed] [Google Scholar]
- 12.Mills M, Balsch BF: Spontaneous pneumothorax: A series of 400 cases. Ann Thorac Surg. 1965;122:286–297. 10.1016/S0003-4975(10)66756-2 [DOI] [PubMed] [Google Scholar]
- 13.Brooks JW: Open thoracotomy in the management of spontaneous pneumothorax. Ann Surg. 1973;177(6):798–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rozenman J, Yellin A, Simansky DA, et al. : Re-expansion pulmonary oedema following spontaneous pneumothorax. Respir Med. 1996;90(4):235–238. 10.1016/S0954-6111(96)90293-0 [DOI] [PubMed] [Google Scholar]
- 15.Sakao Y, Kajikawa O, Martin TR, et al. : Association of IL-8 and MCP-1 with the development of reexpansion pulmonary edema in rabbits. Ann Thorac Surg. 2001;71(6):1825–1832. 10.1016/S0003-4975(01)02489-4 [DOI] [PubMed] [Google Scholar]
- 16.Sivrikoz MC, Tunçözgür B, Cekmen M, et al. : The role of tissue reperfusion in the reexpansion injury of the lungs. Eur J Cardiothorac Surg. 2002;22(5):721–727. 10.1016/S1010-7940(02)00447-5 [DOI] [PubMed] [Google Scholar]
- 17.Matsuura Y, Nomimura T, Murakami H, et al. : Clinical analysis of reexpansion pulmonary edema. Chest. 1991;100(6):1562–1566. 10.1378/chest.100.6.1562 [DOI] [PubMed] [Google Scholar]