A 28-year-old woman with multiple sclerosis (MS) presented to the emergency department (ED) at University Hospital in Newark, NJ on March 10, 2011 with epigastric abdominal pain, a low-grade fever, chills, shortness of breath, pleuritic pain, and impaired balance of 2 days' duration. She also reported right arm numbness and dizziness, consistent with her previous symptoms of MS. She had 3 episodes of nonbloody, nonbilious vomiting while in the ED. The patient had had a root canal procedure 2 weeks earlier.
The patient was diagnosed with aggressive relapsing-remitting MS in February 2003. Her past MS exacerbations numbered more than 10, and she had been treated previously with interferon β-1b, glatiramer acetate, cladribine, prednisone, and cyclophosphamide. She started monthly natalizumab (NTZ) infusions in May 2009 and tolerated the drug without any side effects until March 2011. She received a total of 22 monthly infusions. Her most recent visit, for a lab draw, occurred 3 days prior to presentation, and her lab test that day, arranged post hoc, demonstrated positive immunoglobulin M (IgM) anti–hepatitis B core antibody (anti-HBc) and negative anti–hepatitis B surface antibody (anti-HBs). The patient did not smoke, use alcohol, or take IV drugs. She was sexually active with one partner. She had never been vaccinated with hepatitis B. Hepatitis B viral markers in 2006 were negative for hepatitis B surface antigen (HBsAg), IgM anti-HBc, and anti-HBs.
On examination, her blood pressure was 107/68 mm Hg, pulse was 108 bpm, respiratory rate was 18, and temperature was 99.6°F. She was awake, alert, and oriented to time, place, and person. Her pupils were equal, round, and reactive. Strength was 4/5 in both upper extremities and 5/5 in both lower extremities. Sensation to light touch, deep touch, and pinprick was diminished in the right arm and hand. Reflexes were brisk throughout and plantar responses were flexor. Fine finger movements were slow. There was no dysmetria on finger-to-nose or heel-to-shin testing. She had an unsteady gait.
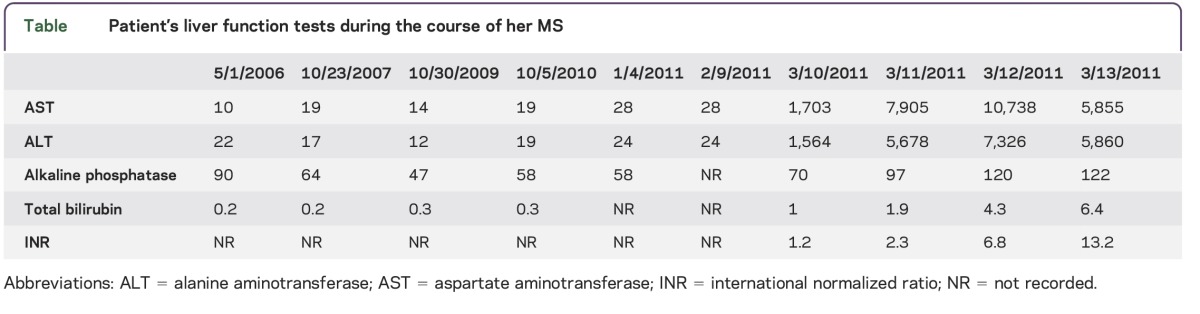
Initial workup showed a leukocyte count of 5,400/uL, hemoglobin of 12.5 g/dL, and platelet count of 123,000. Liver function tests were as follows: aspartate aminotransferase (AST): 1,203 U/L; alanine aminotransferase (ALT): 1,564 U/L; total bilirubin: 1.0 mg/dL; alkaline phosphatase: 70 U/L. International normalized ratio (INR) was 1.2 (table). On the night of her admission, she spiked a temperature of 103°F. Blood and urine cultures were negative. She was started empirically on vancomycin and piperacillin/tazobactam. Subsequent complete blood count with differential demonstrated neutropenia. Steroids were not administered. On March 12, her AST rose to 10,730 U/L, ALT was 7,226 U/L, alkaline phosphatase was 120 U/L, total bilirubin was 4.2 mg/dL, and INR was 3.4. Viral hepatitis markers (March 11) were as follows: HBsAg, anti-HBs, and IgM anti-HBc were positive, while hepatitis C antibody and anti–hepatitis A virus IgM were negative. She had 7,973,400 copies/mL of hepatitis B virus (HBV) DNA. She was transferred to the hepatology service and started on entecavir, N-acetylcysteine, lactulose, and vitamin K. Her transaminase levels continued to worsen. On March 13th, she developed hepatic encephalopathy with behavioral changes. Treatment with liver transplant was entertained, but the patient and her family refused. She died on March 14, 2011.
Table.
Patient's liver function tests during the course of her MS
Discussion.
NTZ is a recombinant monoclonal antibody approved for the treatment of patients with MS and Crohn disease. Because of its immune suppressive effects, it has been associated with various opportunistic CNS viral infections, including progressive multifocal leukoencephalopathy, herpes simplex virus encephalitis and varicella-zoster virus encephalitis, meningitis, and myelitis.1 Serious hepatic injury and hepatitis have been reported with NTZ use.2,3
To our knowledge, we present the first case report of acute HBV infection leading to fulminant liver failure and death in a patient treated with NTZ for MS. Our patient's hepatitis markers were confirmed to be HBV-negative in 2006. Liver function tests were normal until her presentation in 2011 (table). She was positive for both HBsAg and anti-HBs and she had shown seroconversion to positive anti-HBs within 3 days. Concurrent positivity to HBsAg and anti-HBs can be seen in about 25% of patients with fulminant hepatitis from HBV infection.4 Patients with fulminant hepatitis related to HBV have early appearance of anti-HBs due to heightened immune response to the viral antigen, the mechanism of which is poorly understood.4,5 We cannot be sure whether our patient had an acute HBV infection, possibly related to a dental procedure, or reactivation from a chronic HBV carrier state.
In conclusion, while her HBV infection may be unrelated to NTZ treatment, NTZ treatment could have contributed to the fulminant course of her illness. These findings emphasize the need for pretreatment hepatitis screening and regular monitoring of hepatic function of patients taking NTZ.
Footnotes
Author contributions: Machteld Hillen, Stuart Cook, Arun Samantha, and Jamuna Rajasingham contributed to drafting and conceptualizing of the manuscript for intellectual content. Machteld Hillen, Stuart Cook, Arun Samantha, James Quinless, and Jamuna Rajasingham analyzed and interpreted the data. Evan Grant and James Quinless collected clinical data.
Study funding: No targeted funding reported.
Disclosure: M.E. Hillen received research support from Roche, Biogen Idec, Novartis, NIH/National Institute of Neurological Disorders and Stroke, and CDHI Foundation. S.D. Cook is on the scientific advisory board for Bayer, Merck Serono, Actinobac Biomed, Teva, and Biogen Idec; is an editor for Neurology Reviews; has consulted for Merck Serono; and has received research support from Merck Serono, Bayer Healthcare, Biogen Idec, Roche, and Novartis. A. Samanta has received speaker honorarium from Vertex Pharmaceuticals and Gilead Pharmaceuticals and is on the speakers' bureau for Vertex Pharmaceuticals and Gilead Pharmaceuticals. E. Grant reports no disclosures. J.R. Quinless received research support from Merck Serono, Bayer, Roche, Biogen, Novartis, and National Multiple Sclerosis Society. J.K. Rajasingham reports no disclosures. Go to Neurology.org/nn for full disclosures. The Article Processing Charge was paid by the authors.
References
- 1.Fine AJ, Sobello A, Kortepeter C, Scarazzini L. Central nervous system herpes encephalitis and varicella zoster virus infections in natalizumab-treated patients. Clin Infect Dis 2013;57:849–52. [DOI] [PubMed] [Google Scholar]
- 2.Bezabeh S, Flowers CM, Kortepeter C, Avigan M. Clinically significant liver injury in patients treated with natalizumab. Aliment Pharmacol Ther 2010;31:1028–1035. [DOI] [PubMed] [Google Scholar]
- 3.Lisotti A, Azzaroli F, Brillanti S, Mazzella G. Severe acute autoimmune hepatitis after natalizumab treatment. Dig Liver Dis 2012;44:356–357. [DOI] [PubMed] [Google Scholar]
- 4.Trepo CG, Robert D, Motin j, Trepo D, Sepetjian M, Prince AM. Hepatitis B antigen (HBsAg) and/or antibodies (ant-HBs and anti-HBc) in fulminant hepatitis: pathogenic and prognostic significance. Gut 1976;17:10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gimson AES, Tedder RS, White YS, Eddleston AL, Williams R. Serologic markers in fulminant hepatitis B. Gut 1983;24:615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]


