Abstract
The aim of this study was to evaluate the combination of daptomycin and fosfomycin in experimental chronic implant-associated osteomyelitis due to methicillin-resistant Staphylococcus aureus (MRSA). Infection was induced in the tibiae of rats by the insertion of a bacterial inoculum (1 to 5 × 108 CFU/ml) of a clinical MRSA isolate and a titanium wire. Four weeks after infection, each animal was assigned to a treatment group: daptomycin monotherapy at 60 mg/kg of body weight once daily (n = 10), fosfomycin monotherapy at 40 mg/kg once daily (n = 10), or daptomycin and fosfomycin combined at 60 mg/kg and 40 mg/kg, respectively, once daily (n = 9). Ten animals were left untreated. After a 3-week treatment period, the animals were euthanized, and the infected tibiae and implants were processed for quantitative bacterial cultures. The bacterial cultures from bones were positive for MRSA in all animals in the untreated group, the daptomycin group, and the fosfomycin group, with median bacterial counts of 2.34 × 106 CFU/g bone, 1.57 × 106 CFU/g bone, and 3.48 × 102 CFU/g bone, respectively. In the daptomycin-fosfomycin group, 6 out of 9 animals were positive for MRSA, with a median count of 7.92 CFU/g bone. Bacterial cultures derived from the titanium wires were negative in the fosfomycin- and daptomycin-fosfomycin-treated groups. Based on bacterial counts in bones, treatment with daptomycin-fosfomycin was statistically significantly superior to all that of the other groups (P ≤ 0.003). Fosfomycin was superior to daptomycin and no treatment (P < 0.0001). No development of resistance was observed in any treatment arm. The combination of daptomycin and fosfomycin demonstrated synergism against MRSA in experimental implant-associated osteomyelitis.
INTRODUCTION
Implant-associated osteomyelitis is considered an infection that is difficult to treat. Bacteria adhering to implants may organize in biofilms; this special formation of bacteria initiates specific gene expression patterns enabling bacteria to enter a stationary phase. This in turn alters the bacterial metabolism, making it less susceptible to antibiotic agents. Furthermore, biofilm-organized bacteria impair the diffusion of antimicrobial agents to the bacterial cells due to the production of an extracellular polymeric matrix. Due to these special circumstances, treatment of implant-associated osteomyelitis requires long-term antibiotic treatment along with surgical interventions. As cases differ to a great extent in clinical routine, evidence-based guidelines advising the use of distinct antibiotic agents on the basis of randomized clinical trials do not exist (1–3).
Staphylococcus aureus is frequently isolated in patients with implant-associated osteomyelitis (1, 4). The rising number of methicillin-resistant Staphylococcus aureus (MRSA) isolates, however, reduces the antimicrobial treatment options. Additionally, as long-term antibiotic regimens are standard for osteomyelitis, applied antibiotics need to have a favorable adverse effect profile at preferably low economic costs (5).
Daptomycin is a relatively new antibiotic agent with rapid bactericidal activity against Gram-positive bacteria, including MRSA. It is approved for the treatment of Staphylococcus aureus bacteremia and endocarditis. Further, daptomycin has been shown to be effective in the treatment of osteomyelitis in experimental animal studies and in clinical studies (6–8). Little information, however, is available on the effectiveness of daptomycin for the treatment of implant-associated osteomyelitis and biofilms.
Fosfomycin is a bactericidal agent that has been in clinical use for several decades. Fosfomycin shows antibacterial activity against various Gram-positive and Gram-negative bacteria, including multidrug-resistant strains. In addition, high antibacterial activity in biofilms and the enhancement of efficacies of other agents when combined are attributed to fosfomycin (9, 10). Due to concerns about the rapid emergence of resistance against fosfomycin observed in vitro, fosfomycin is usually combined with other antibiotics of other classes in clinical practice (11), although several studies recently questioned the clinical relevance of this finding (8, 12).
As we demonstrated previously, fosfomycin is effective in experimental implant- and non-implant-associated MRSA osteomyelitis (12, 13). The combination with daptomycin proved highly efficacious in experimental non-implant-associated osteomyelitis, yet synergism was not identifiable due to the high efficacy observed for fosfomycin when applied in standard doses (8).
Therefore, the aim of the present study was to evaluate the effectiveness of daptomycin and fosfomycin combined and a possible synergistic effect in experimental chronic implant-associated MRSA osteomyelitis in rats by applying lower doses of fosfomycin and standard doses of daptomycin (12, 13).
MATERIALS AND METHODS
The study protocol was approved by the local Animal Welfare Committee and was performed in the level 2 biohazard area of the Institute of Biomedical Research, Medical University of Vienna.
Bacteria and preparation of inocula.
A clinical strain of MRSA (4409/07) isolated from a patient with chronic osteomyelitis was used in this study. For in vivo testing, bacteria in the exponential growth phase were used as follows: bacteria grown overnight in Trypticase soy broth (TSB) were diluted 1:100 in TSB and incubated for 5 h at 37°C. The bacterial count of the prepared inoculum was confirmed from plate counts made before and after the surgical procedures at 1 to 5 × 108 CFU/ml.
In vitro susceptibility testing.
The MICs of daptomycin and fosfomycin for MRSA were determined by using a broth microdilution method with cation-adjusted Mueller-Hinton broth (CAMHB) (75 mg/liter Ca2+, 25 mg/liter Mg2+) according to CLSI guidelines (14). For the testing of fosfomycin activity, CAMHB was supplemented with glucose-6-phosphate (Sigma-Aldrich) at a final concentration of 25 mg/liter (15).
Experimental osteomyelitis.
Bone infection was established using an implant-associated osteomyelitis model as described previously (13). The overall study period was 7 weeks, comprising an incubation period of 4 weeks and a treatment phase of 3 weeks. In short, male Sprague-Dawley CD rats (Charles River WIGA GmbH, Sulzfeld, Germany) weighing 400 ± 30 g were used. Each animal was anesthetized with ketamine and xylazine, and the left hind leg was shaved and disinfected with polyvinyl pyrrolidine iodine. The proximal medial surface of the tibia was surgically exposed, and a hole (0.1-cm diameter) was drilled into the medullary cavity using a high-speed drill (Multipro; Dremel, Racine, WI). A 15-μl sample of the MRSA inoculum containing 1 × 108 to 5 × 108 CFU/ml was injected into the bone. Subsequently, a sterile 1-cm-long titanium Kirschner wire (0.8-mm diameter) was inserted into the medullary cavity. No sclerosing agent was administered. The drill holes were sealed with sterile bone wax (Ethicon Sutures Ltd., Peterborough, Ontario, Canada). The incisions were closed with sutures. All animals received postoperative analgesia in the form of subcutaneous and oral piritramide.
Antibiotic treatment regimens.
Four weeks after infection, animals with radiographically confirmed osteomyelitis of the tibia were randomly assigned to one of the following four groups: (i) daptomycin alone (n = 10), (ii) fosfomycin alone (n = 10), (iii) daptomycin and fosfomycin in combination (n = 9), or (iv) no treatment (n = 10). Daptomycin powder (Cubist Pharmaceuticals, Lexington, MA) was dissolved in sterile water and administered intraperitoneally at a dose of 60 mg/kg of body weight once daily. Fosfomycin powder (Sandoz, Kundl, Austria) was dissolved in sterile water and administered intraperitoneally at a dose of 40 mg/kg of body weight once daily. The combined treatment group received daptomycin and fosfomycin at doses of 60 mg/kg of body weight once daily and 40 mg/kg of body weight once daily, respectively. All the treatment regimens were administered for 21 to 23 days.
Bacterial counting.
Twelve hours after the completion of antimicrobial therapy, each rat was euthanized with a lethal dose of thiopental. The infected tibiae were aseptically removed and weighed. The Kirschner wires were aseptically removed from the medullar cavity. The bones were then pulverized by using a liquid-nitrogen-cooled cryo-mill (6770 Freezer Mill; Spex SamplePrep, Metuchen, NJ). Sterile physiological saline (10 ml) was added to each bone specimen, and bone suspensions were vigorously vortexed. Serial 10-fold dilutions were prepared, and bacterial counts were made by plating 20 μl of each dilution onto sheep blood agar plates. Additionally, 100 μl of each bone suspension was plated on blood agar. After incubation for 24 h at 37°C, the MRSA colonies were counted, and the results were expressed as CFU/g of bone. The remaining specimens were placed into 10 ml TSB and incubated for 48 h in 5% CO2 at 37°C. Sterile cultures were assigned a value of 1 log10 CFU/g of bone.
The removed Kirschner wires were processed as follows: the wires were put into 2 ml of sterile physiological saline, vortexed for 30 s, sonicated at 35 kHz for 5 min, and vortexed again for 30 s. Quantitative bacterial cultures were performed out of the suspension as described above. For qualitative cultures, 500 μl of the remaining 2 ml of saline was plated onto sheep blood agar plates; furthermore, the Kirschner wires were rolled and placed onto sheep blood agar plates. Sterile cultures were assigned a value of 1 log10 CFU/g of bone.
To detect the emergence of resistance, the MICs of fosfomycin and daptomycin for MRSA recovered from bones and implants were determined using the standard methods described above.
Statistics.
Experimental results were plotted and analyzed by using GraphPad Prism version 6. Pairwise comparisons between bacterial counts of the bones and those of the implants, as well as the median weight gains in the four groups, were performed using the Mann-Whitney U test followed by Bonferroni's correction for multiple comparison testing. Therefore, P values of <0.008 were considered statistically significant to adjust for six pairwise comparisons.
RESULTS
Experimental osteomyelitis.
All the infected rats displayed implant-associated osteomyelitis in radiographical evaluations 4 weeks after incubation.
The results of the antibiotic treatment regimens are shown in Fig. 1. Bacterial cultures from bones were positive for MRSA in 10 out of 10 (100%) animals in the untreated group, in 10 out of 10 (100%) animals in the daptomycin-treated group, in 10 out of 10 (100%) animals in the fosfomycin-treated group, and in 6 out of 9 (66.6%) animals in the daptomycin-fosfomycin combination group. The median bacterial count (minimum to maximum) in the untreated group was 2.34 × 106 CFU/g of bone (6.28 × 103 to 1.57 × 107 CFU/g). Treatment with daptomycin yielded a median bacterial count of 1.57 × 106 CFU/g of bone (2.25 × 105 to 8.73 × 106 CFU/g); treatment with daptomycin was not statistically superior to no treatment (P = 0.519). Bacterial cultures from bones of the fosfomycin-treated group yielded a median bacterial count of 3.48 × 102 CFU/g of bone (1.17 × 102 to 4.16 × 103 CFU/g). Treatment with daptomycin and fosfomycin combined resulted in a median bacterial count of 7.92 CFU/g of bone (0 to 1.65 × 103 CFU/g). Daptomycin and fosfomycin combined showed statistical superiority to fosfomycin alone (P = 0.003), daptomycin alone (P < 0.0001), and no treatment (P < 0.0001), while treatment with fosfomycin alone was superior to daptomycin (P < 0.0001) and no treatment (P < 0.0001).
FIG 1.
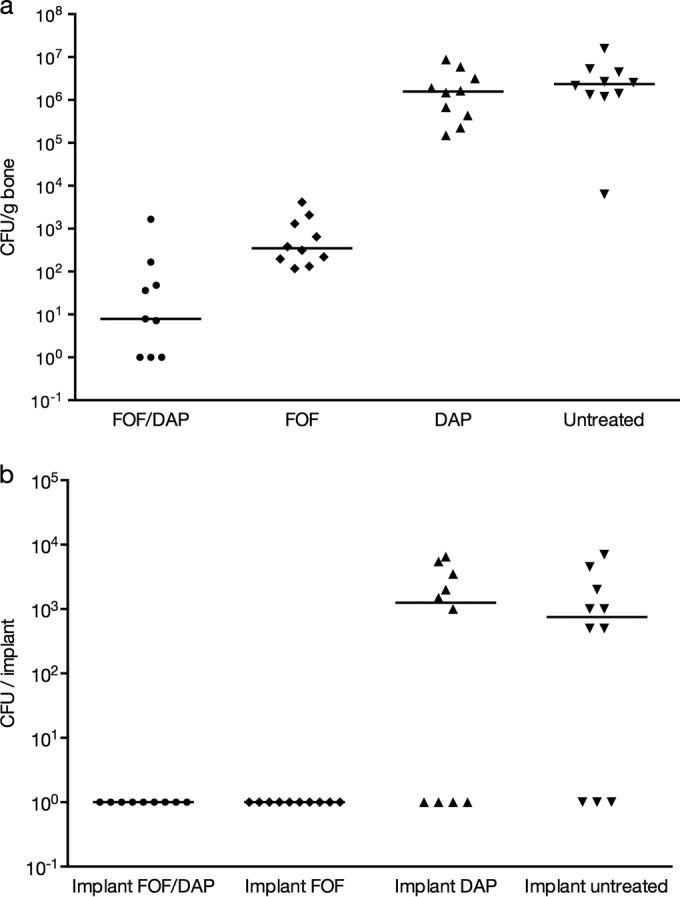
Bacterial counts in osseous tissue (a) and on implants (b) after a 3-week treatment period with daptomycin (DAP), fosfomycin (FOF), the daptomycin-fosfomycin combination, and no treatment in rats with experimental implant-associated MRSA osteomyelitis. Each symbol represents the value retained for an individual animal. Horizontal bars indicate median values.
Bacterial cultures derived from the Kirschner wires after the microbiological workup were positive for MRSA in 7 out of 10 (70%) animals in the untreated group and in 6 out of 10 animals in the daptomycin-treated group (60%). The bacterial cultures derived from the Kirschner wires were all negative in the groups treated with fosfomycin and with daptomycin-fosfomycin. The median bacterial counts were 7.50 × 102 (0 to 7.00 × 103) and 1.25 × 103 (0 to 6.50 × 103) in the untreated and daptomycin-treated groups, respectively. In a statistical assessment based on the bacterial counts obtained from implant suspensions, daptomycin-fosfomycin and fosfomycin alone were statistically superior to no treatment (P = 0.0031), yet they were not superior to daptomycin (P = 0.0108).
MICs, drug interactions, and development of drug resistance.
The MICs of fosfomycin and daptomycin against MRSA 4409/07 were 0.5 ml/liter and 0.25 ml/liter, respectively, and thus were not resistant in terms of the EUCAST clinical breakpoints database (15). The MICs of MRSA isolates obtained from all the animals still infected at the end of the treatment period were within 1 dilution of the pretreatment MIC, indicating no emergence of resistance.
Adverse events.
None of the animals developed diarrhea; however, body weight gains differed between the treatment arms. The median weight gain in the combination group was significantly lower than those in the other groups (P ≤ 0.0057).
DISCUSSION
In this study, treatment with daptomycin yielded no difference compared to no treatment, indicating a low efficacy of daptomycin in the treatment of implant-associated infections when used as monotherapy. This, however, stands in contrast to previous studies. Vaudaux et al. and Schaad et al. demonstrated decreased bacterial counts in tissue cage models of infection due to Staphylococcus aureus after 7 days of treatment with daptomycin at 30 mg/kg once and twice daily, respectively (16, 17). Likewise, Rouse et al. found decreased colony counts in experimental osteomyelitis after a 21-day treatment period with a dose of 60 mg/kg twice daily (18). Of interest to note is that daptomycin applied as monotherapy has been shown to be effective in an non-implant-associated osteomyelitis model using the same MRSA strain used in the present study (8). Thus, for implant-associated osteomyelitis, higher doses might be necessary. However, Sakoulas et al. found that a dosage of 40 mg/kg in rats is comparable to a dosage of 6 mg/kg in humans (19). Hence, the dosage of 60 mg/kg in rats used in the present study appears comparable to the increasingly higher doses of daptomycin applied in humans currently (20).
In this study, a fosfomycin monotherapy of 40 mg/kg of body weight once daily was superior to daptomycin or no treatment. Regimens with fosfomycin in treatment of systemic infections usually apply doses from 4 g up to 8 g three times daily (21). It was recently shown that in rats, a fosfomycin dosage of 200 to 500 mg/kg three times daily is most suitable in order to obtain a drug exposure comparable to a dosage of 8 g three times daily in humans (22). Thus, the exposure obtained in the present study is easily achieved with all fosfomycin regimens currently applied in humans. An even higher effectiveness of fosfomycin monotherapy in the treatment of implant-associated and non-implant-associated osteomyelitis was already shown when fosfomycin was used in a dosage of 75 mg/kg (8, 13). However, in this study, the particular low dosage was used in order to identify a possible synergistic interaction between daptomycin and fosfomycin in vivo.
Yet, in this study, the combination of daptomycin and fosfomycin was superior to all compared monotherapies and no treatment. Moreover, daptomycin and fosfomycin were synergistic in the treatment of experimental implant-associated osteomyelitis.
The combination of daptomycin and fosfomycin has been evaluated in different experimental settings. Garrigós et al. studied daptomycin plus fosfomycin using a MRSA tissue cage model and demonstrated high bactericidal activity of this combination (23). Likewise, high efficacy and a synergistic effect for this combination were also shown in experimental MRSA endocarditis (24). Thus, this combination has been shown to be effective against different strains of MRSA in different experimental settings. Most importantly, the combination does not seem to display any antagonistic features. Furthermore, Garrigós et al. (23) and a recently published study by Mihailescu et al. (25) compared combined daptomycin plus fosfomycin with daptomycin plus rifampin in MRSA biofilms. In both studies, combined daptomycin and rifampin proved to be statistically more effective than daptomycin plus fosfomycin in experimental MRSA tissue cage infection models (23, 25). Yet, the latter study showed the overall best cure rates in another treatment group with combined fosfomycin and rifampin. In line with these findings, rifampin is currently recommended for combinations with other antibiotics in the treatment of implant-associated osteoarticular infections (26); however, enhanced bacterial activity with other antibiotics was also shown for fosfomycin. Mihailescu et al. reasoned that fosfomycin may be a useful combination partner to rifampin, but it cannot replace rifampin as an antibiofilm agent (25). In contrast, an in vitro study demonstrated enhanced antibacterial activity of linezolid, minocycline, vancomycin, and teicoplanin against planktonic or biofilm-embedded isolates of MRSA after the addition of fosfomycin. Moreover, the combination with fosfomycin demonstrated better results than those of the same combinations with rifampin (10). Hence, the role of fosfomycin in implant-associated infections and in biofilms due to Gram-positive cocci is under controversial scientific discussion. Likewise, daptomycin is under thorough investigation concerning implant- or biofilm-associated infections. As mentioned above, daptomycin displays certain efficacy in foreign body models, especially when combined with another antibiotic agent. Furthermore, daptomycin is increasingly in use in implant-associated infections (27). The penetration into biofilms, however, was recently shown to be moderate (28), as was clinical success (29). In this study, implants were cleared of all bacteria in the fosfomycin-containing treatment groups, underlining the capability of fosfomycin to penetrate into adherent bacteria or biofilm formations and augment the activity of daptomycin.
The mechanism of the synergism remains unclear. Fosfomycin acts as an inhibitor of the first phase in the synthesis of peptidoglycan by blocking the formation of N-acetylmuramic acid (30). Daptomycin acts bactericidally by oligomerization and disruption of the functional integrity of the bacterial membrane. However, it also induces certain bacterial cell wall gene products, including MurA, the protein that fosfomycin is inhibiting (31). Thus, these two agents show fields of interaction, yet the exact mechanisms of the observed synergism need to be investigated further.
In our study, no emergence of resistance against fosfomycin or daptomycin was observed in any MRSA isolate after the cessation of treatment. As already shown previously, fosfomycin monotherapy did not induce resistance (13). The present results, however, have to be interpreted with care, as the MRSA isolate applied in this study displays a relatively low MIC against fosfomycin, resulting in a higher efficacy of fosfomycin and consequently a lower chance of resistance induction (32). Moreover, the low number of included animals limits the strength of evidence of this finding.
Regarding tolerance of the applied treatment regimens, animal weights differed between the treatment groups. Although no adverse events, such as diarrhea, were observed, animals in the combination group gained significantly less weight than animals in all the other groups. However, in humans, the combination of daptomycin and fosfomycin has been well tolerated with no evident side effects (33).
In conclusion, we demonstrated antibacterial synergism between daptomycin and fosfomycin against MRSA in implant-associated infection in bone. Further studies are needed to estimate the relevance of this finding for the management of implant-associated osteomyelitis in humans.
ACKNOWLEDGMENTS
We thank Heidelinde Schranz from the Department of Internal Medicine I, Division of Infectious Diseases and Tropical Medicine, Medical University of Vienna, for valuable suggestions, excellent technical assistance, and support in the microbiological workup.
This study was supported by an unrestricted educational grant from Novartis.
REFERENCES
- 1.Trampuz A, Zimmerli W. 2008. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr Infect Dis Rep 10:394–403. doi: 10.1007/s11908-008-0064-1. [DOI] [PubMed] [Google Scholar]
- 2.Zimmerli W, Trampuz A, Ochsner PE. 2004. Prosthetic-joint infections. N Engl J Med 351:1645–1654. doi: 10.1056/NEJMra040181. [DOI] [PubMed] [Google Scholar]
- 3.Walter G, Kemmerer M, Kappler C, Hoffmann R. 2012. Treatment algorithms for chronic osteomyelitis. Dtsch Arztebl Int 109:257–264. doi: 10.3238/arztebl.2012.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright JA, Nair SP. 2010. Interaction of staphylococci with bone. Int J Med Microbiol 300:193–204. doi: 10.1016/j.ijmm.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spellberg B, Lipsky BA. 2012. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis 54:393–407. doi: 10.1093/cid/cir842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byren I, Rege S, Campanaro E, Yankelev S, Anastasiou D, Kuropatkin G, Evans R. 2012. Randomized controlled trial of the safety and efficacy of daptomycin versus standard-of-care therapy for management of patients with osteomyelitis associated with prosthetic devices undergoing two-stage revision arthroplasty. Antimicrob Agents Chemother 56:5626–5632. doi: 10.1128/AAC.00038-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallagher JC, Huntington JA, Culshaw D, McConnell SA, Yoon M, Berbari E. 2012. Daptomycin therapy for osteomyelitis: a retrospective study. BMC Infect Dis 12:133. doi: 10.1186/1471-2334-12-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poeppl W, Tobudic S, Lingscheid T, Plasenzotti R, Kozakowski N, Lagler H, Georgopoulos A, Burgmann H. 2011. Daptomycin, fosfomycin, or both for treatment of methicillin-resistant Staphylococcus aureus osteomyelitis in an experimental rat model. Antimicrob Agents Chemother 55:4999–5003. doi: 10.1128/AAC.00584-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang HJ, Chen CC, Cheng KC, Wu KY, Lin YC, Zhang CC, Weng TC, Yu WL, Chiu YH, Toh HS, Chiang SR, Su BA, Ko WC, Chuang YC. 2013. In vitro efficacies and resistance profiles of rifampin-based combination regimens for biofilm-embedded methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 57:5717–5720. doi: 10.1128/AAC.01236-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang HJ, Chen CC, Cheng KC, Toh HS, Su BA, Chiang SR, Ko WC, Chuang YC. 2012. In vitro efficacy of fosfomycin-containing regimens against methicillin-resistant Staphylococcus aureus in biofilms. J Antimicrob Chemother 67:944–950. doi: 10.1093/jac/dkr535. [DOI] [PubMed] [Google Scholar]
- 11.Falagas ME, Roussos N, Gkegkes ID, Rafailidis PI, Karageorgopoulos DE. 2009. Fosfomycin for the treatment of infections caused by Gram-positive cocci with advanced antimicrobial drug resistance: a review of microbiological, animal and clinical studies. Expert Opin Investig Drugs 18:921–944. doi: 10.1517/13543780902967624. [DOI] [PubMed] [Google Scholar]
- 12.Poeppl W, Tobudic S, Lingscheid T, Plasenzotti R, Kozakowski N, Georgopoulos A, Burgmann H. 2011. Efficacy of fosfomycin in experimental osteomyelitis due to methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 55:931–933. doi: 10.1128/AAC.00881-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poeppl W, Lingscheid T, Bernitzky D, Schwarze UY, Donath O, Perkmann T, Kozakowski N, Plasenzotti R, Reznicek G, Burgmann H. 2014. Efficacy of fosfomycin compared to vancomycin in treatment of implant-associated chronic methicillin-resistant Staphylococcus aureus osteomyelitis in rats. Antimicrob Agents Chemother 58:5111–5116. doi: 10.1128/AAC.02720-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clinical and Laboratory Standards Institute. January 2014. Performance standards for antimicrobial susceptibility testing, 24th informational supplement. Approved standard M100-S24 Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 15.The European Committee on Antimicrobial Susceptibility Testing. 2013. Fosfomycin: rationale for the EUCAST clinical breakpoints, version 1.0, 2013. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Rationale_documents/Fosfomycin_rationale_1.0_20130203.pdf.
- 16.Vaudaux P, Francois P, Bisognano C, Li D, Lew DP, Schrenzel J. 2003. Comparative efficacy of daptomycin and vancomycin in the therapy of experimental foreign body infection due to Staphylococcus aureus. J Antimicrob Chemother 52:89–95. doi: 10.1093/jac/dkg277. [DOI] [PubMed] [Google Scholar]
- 17.Schaad HJ, Bento M, Lew DP, Vaudaux P. 2006. Evaluation of high-dose daptomycin for therapy of experimental Staphylococcus aureus foreign body infection. BMC Infect Dis 6:74. doi: 10.1186/1471-2334-6-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rouse MS, Piper KE, Jacobson M, Jacofsky DJ, Steckelberg JM, Patel R. 2006. Daptomycin treatment of Staphylococcus aureus experimental chronic osteomyelitis. J Antimicrob Chemother 57:301–305. doi: 10.1093/jac/dki435. [DOI] [PubMed] [Google Scholar]
- 19.Sakoulas G, Eliopoulos GM, Alder J, Eliopoulos CT. 2003. Efficacy of daptomycin in experimental endocarditis due to methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 47:1714–1718. doi: 10.1128/AAC.47.5.1714-1718.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai CC, Sheng WH, Wang JT, Cheng A, Chuang YC, Chen YC, Chang SC. 2013. Safety and efficacy of high-dose daptomycin as salvage therapy for severe Gram-positive bacterial sepsis in hospitalized adult patients. BMC Infect Dis 13:66. doi: 10.1186/1471-2334-13-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker S, Lipman J, Koulenti D, Dimopoulos G, Roberts JA. 2013. What is the relevance of fosfomycin pharmacokinetics in the treatment of serious infections in critically ill patients? A systematic review. Int J Antimicrob Agents 42:289–293. doi: 10.1016/j.ijantimicag.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 22.Poeppl W, Lingscheid T, Bernitzky D, Donath O, Reznicek G, Zeitlinger M, Burgmann H. 2014. Assessing pharmacokinetics of different doses of fosfomycin in laboratory rats enables adequate exposure for pharmacodynamic models. Pharmacology 93:65–68. doi: 10.1159/000357569. [DOI] [PubMed] [Google Scholar]
- 23.Garrigós C, Murillo O, Lora-Tamayo J, Verdaguer R, Tubau F, Cabellos C, Cabo J, Ariza J. 2013. Fosfomycin-daptomycin and other fosfomycin combinations as alternative therapies in experimental foreign-body infection by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 57:606–610. doi: 10.1128/AAC.01570-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miro JM, Garcia de la Maria C, Pericas JM, Armero Y, Soy D, Cervera C, Mestres CA, Falces C, Marco F, Moreno A. 2014. Combination of daptomycin plus fosfomycin has synergistic, potent, and rapid bactericidal activity against methicillin-resistant Staphylococcus aureus (MRSA) in a rabbit model of experimental endocarditis (EE), poster 0088 European Congress of Clinical Microbiology and Infectious Diseases, Barcelona, Spain, 10 to 13 May 2014. [Google Scholar]
- 25.Mihailescu R, Furustrand Tafin U, Corvec S, Oliva A, Betrisey B, Borens O, Trampuz A. 2014. High activity of fosfomycin and rifampin against methicillin-resistant Staphylococcus aureus biofilm in vitro and in an experimental foreign-body infection model. Antimicrob Agents Chemother 58:2547–2553. doi: 10.1128/AAC.02420-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR. 2013. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 27.Seaton RA, Malizos KN, Viale P, Gargalianos-Kakolyris P, Santantonio T, Petrelli E, Pathan R, Heep M, Chaves RL. 2013. Daptomycin use in patients with osteomyelitis: a preliminary report from the EU-CORE database. J Antimicrob Chemother 68:1642–1649. doi: 10.1093/jac/dkt067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siala W, Mingeot-Leclercq MP, Tulkens PM, Hallin M, Denis O, Van Bambeke F. 2014. Comparison of the antibiotic activities of daptomycin, vancomycin, and the investigational fluoroquinolone delafloxacin against biofilms from Staphylococcus aureus clinical isolates. Antimicrob Agents Chemother 58:6385–6397. doi: 10.1128/AAC.03482-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lora-Tamayo J, Parra-Ruiz J, Rodríguez-Pardo D, Barberán J, Ribera A, Tornero E, Pigrau C, Mensa J, Ariza J, Soriano A. 2014. High doses of daptomycin (10 mg/kg/d) plus rifampin for the treatment of staphylococcal prosthetic joint infection managed with implant retention: a comparative study. Diagn Microbiol Infect Dis 80:66–71. doi: 10.1016/j.diagmicrobio.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 30.Popovic M, Steinort D, Pillai S, Joukhadar C. 2010. Fosfomycin: an old, new friend? Eur J Clin Microbiol Infect Dis 29:127–142. doi: 10.1007/s10096-009-0833-2. [DOI] [PubMed] [Google Scholar]
- 31.Muthaiyan A, Silverman JA, Jayaswal RK, Wilkinson BJ. 2008. Transcriptional profiling reveals that daptomycin induces the Staphylococcus aureus cell wall stress stimulon and genes responsive to membrane depolarization. Antimicrob Agents Chemother 52:980–990. doi: 10.1128/AAC.01121-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roussos N, Karageorgopoulos DE, Samonis G, Falagas ME. 2009. Clinical significance of the pharmacokinetic and pharmacodynamic characteristics of fosfomycin for the treatment of patients with systemic infections. Int J Antimicrob Agents 34:506–515. doi: 10.1016/j.ijantimicag.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Miró JM, Entenza JM, Del Río A, Velasco M, Castañeda X, Garcia de la Mària C, Giddey M, Armero Y, Pericàs JM, Cervera C, Mestres CA, Almela M, Falces C, Marco F, Moreillon P, Moreno A, Hospital Clinic Experimental Endocarditis Study Group. 2012. High-dose daptomycin plus fosfomycin is safe and effective in treating methicillin-susceptible and methicillin-resistant Staphylococcus aureus endocarditis. Antimicrob Agents Chemother 56:4511–4515. doi: 10.1128/AAC.06449-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


